Victoza prior authorization resources
Most recent state uniform prior authorization forms
Brand Resources
Victoza patient education
Patient toolkit
Dosage & administration
DOSAGE AND ADMINISTRATION
- Adult Patients : Initiate at 0.6 mg injected subcutaneously once daily for one week then increase to 1.2 mg daily. If additional glycemic control is required, increase the dose to 1.8 mg daily after one week of treatment with the 1.2 mg daily dose. (2.1 )
- Pediatric Patients : Initiate at 0.6 mg injected subcutaneously once daily for at least one week. If additional glycemic control is required increase the dose to 1.2 mg daily and if additional glycemic control is still required, increase the dose to 1.8 mg daily after at least one week of treatment with the 1.2 mg daily dose. (2.1 )
- Inspect visually prior to each injection. Only use if solution is clear, colorless, and contains no particles. (2.3 )
- Inject VICTOZA subcutaneously once-daily at any time of day, independently of meals, in the abdomen, thigh or upper arm. (2.3 )
- When using VICTOZA with insulin, administer as separate injections. Never mix. (2.3 )
Recommended Dosage
Adult Patients
- The recommended starting dosage of VICTOZA is 0.6 mg injected subcutaneously once daily for one week. The 0.6 mg once daily dosage is intended to reduce the risk of gastrointestinal adverse reactions [see Warnings and Precautions (5.6 ), Adverse Reactions (6.1 )] during initial titration and is not effective for glycemic control in adults.
- After one week at the 0.6 mg once daily dosage, increase the dosage to 1.2 mg injected subcutaneously once daily.
- If additional glycemic control is required, increase the dosage to the maximum recommended dosage of 1.8 mg injected subcutaneously once daily after at least one week of treatment with the 1.2 mg once daily dosage.
Pediatric Patients Aged 10 Years and Older
- The recommended starting dosage of VICTOZA is 0.6 mg injected subcutaneously once daily.
- If additional glycemic control is required, increase the dosage in 0.6 mg increments after at least one week on the current dosage, to reduce the risk of gastrointestinal adverse reactions [see Warnings and Precautions (5.6 ), Adverse Reactions (6.1 )] .
- The maximum recommended dosage is 1.8 mg injected subcutaneously once daily.
Recommendations Regarding Missed Dose
- Instruct patients who miss a dose of VICTOZA to resume the once daily dosage regimen as prescribed with the next scheduled dose. Do not administer an extra dose or increase the dose to make up for the missed dose.
- If more than 3 days have elapsed since the last VICTOZA dose, reinitiate VICTOZA at 0.6 mg once daily to reduce the risk of gastrointestinal adverse reactions associated with reinitiation of treatment. Upon reinitiation, VICTOZA should be titrated at the discretion of the healthcare provider.
Important Administration Instructions
- Inspect visually prior to each injection. Only use if solution is clear, colorless, and contains no particles.
- Inject VICTOZA subcutaneously once daily at any time of day, independently of meals.
- Inject VICTOZA subcutaneously in the abdomen, thigh or upper arm. No dosage adjustment is needed if changing the injection site and/or timing.
- Rotate injection sites within the same region in order to reduce the risk of cutaneous amyloidosis [see Adverse Reactions (6.2 )].
- When using VICTOZA with insulin, administer as separate injections. Never mix. It is acceptable to inject VICTOZA and insulin in the same body region but the injections should not be adjacent to each other.

By using PrescriberAI, you agree to the AI Terms of Use.
Victoza prescribing information
WARNING: RISK OF THYROID C-CELL TUMORS
- Liraglutide causes dose-dependent and treatment-duration-dependent thyroid C-cell tumors at clinically relevant exposures in both genders of rats and mice. It is unknown whether VICTOZA causes thyroid C-cell tumors, including medullary thyroid carcinoma (MTC), in humans, as the human relevance of liraglutide-induced rodent thyroid C-cell tumors has not been determined [see Warnings and Precautions (5.1 ), Nonclinical Toxicology (13.1 )].
- VICTOZA is contraindicated in patients with a personal or family history of MTC and in patients with Multiple Endocrine Neoplasia syndrome type 2 (MEN 2). Counsel patients regarding the potential risk for MTC with the use of VICTOZA and inform them of symptoms of thyroid tumors (e.g., a mass in the neck, dysphagia, dyspnea, persistent hoarseness). Routine monitoring of serum calcitonin or using thyroid ultrasound is of uncertain value for early detection of MTC in patients treated with VICTOZA [see Contraindications (4 ), Warnings and Precautions (5.1 )].
INDICATIONS AND USAGE
VICTOZA is indicated:
- as an adjunct to diet and exercise to improve glycemic control in adults and pediatric patients aged 10 years and older with type 2 diabetes mellitus,
- to reduce the risk of major adverse cardiovascular events (cardiovascular death, non-fatal myocardial infarction, or non-fatal stroke) in adults with type 2 diabetes mellitus and established cardiovascular disease.
Limitations of Use:
VICTOZA contains liraglutide. Coadministration with other liraglutide-containing products is not recommended.
DOSAGE AND ADMINISTRATION
- Adult Patients : Initiate at 0.6 mg injected subcutaneously once daily for one week then increase to 1.2 mg daily. If additional glycemic control is required, increase the dose to 1.8 mg daily after one week of treatment with the 1.2 mg daily dose. (2.1 )
- Pediatric Patients : Initiate at 0.6 mg injected subcutaneously once daily for at least one week. If additional glycemic control is required increase the dose to 1.2 mg daily and if additional glycemic control is still required, increase the dose to 1.8 mg daily after at least one week of treatment with the 1.2 mg daily dose. (2.1 )
- Inspect visually prior to each injection. Only use if solution is clear, colorless, and contains no particles. (2.3 )
- Inject VICTOZA subcutaneously once-daily at any time of day, independently of meals, in the abdomen, thigh or upper arm. (2.3 )
- When using VICTOZA with insulin, administer as separate injections. Never mix. (2.3 )
Recommended Dosage
Adult Patients
- The recommended starting dosage of VICTOZA is 0.6 mg injected subcutaneously once daily for one week. The 0.6 mg once daily dosage is intended to reduce the risk of gastrointestinal adverse reactions [see Warnings and Precautions (5.6 ), Adverse Reactions (6.1 )] during initial titration and is not effective for glycemic control in adults.
- After one week at the 0.6 mg once daily dosage, increase the dosage to 1.2 mg injected subcutaneously once daily.
- If additional glycemic control is required, increase the dosage to the maximum recommended dosage of 1.8 mg injected subcutaneously once daily after at least one week of treatment with the 1.2 mg once daily dosage.
Pediatric Patients Aged 10 Years and Older
- The recommended starting dosage of VICTOZA is 0.6 mg injected subcutaneously once daily.
- If additional glycemic control is required, increase the dosage in 0.6 mg increments after at least one week on the current dosage, to reduce the risk of gastrointestinal adverse reactions [see Warnings and Precautions (5.6 ), Adverse Reactions (6.1 )] .
- The maximum recommended dosage is 1.8 mg injected subcutaneously once daily.
Recommendations Regarding Missed Dose
- Instruct patients who miss a dose of VICTOZA to resume the once daily dosage regimen as prescribed with the next scheduled dose. Do not administer an extra dose or increase the dose to make up for the missed dose.
- If more than 3 days have elapsed since the last VICTOZA dose, reinitiate VICTOZA at 0.6 mg once daily to reduce the risk of gastrointestinal adverse reactions associated with reinitiation of treatment. Upon reinitiation, VICTOZA should be titrated at the discretion of the healthcare provider.
Important Administration Instructions
- Inspect visually prior to each injection. Only use if solution is clear, colorless, and contains no particles.
- Inject VICTOZA subcutaneously once daily at any time of day, independently of meals.
- Inject VICTOZA subcutaneously in the abdomen, thigh or upper arm. No dosage adjustment is needed if changing the injection site and/or timing.
- Rotate injection sites within the same region in order to reduce the risk of cutaneous amyloidosis [see Adverse Reactions (6.2 )].
- When using VICTOZA with insulin, administer as separate injections. Never mix. It is acceptable to inject VICTOZA and insulin in the same body region but the injections should not be adjacent to each other.
DOSAGE FORMS AND STRENGTHS
Injection: 18 mg/3 mL (6 mg/mL) clear, colorless solution in a prefilled, single-patient-use pen that delivers doses of 0.6 mg, 1.2 mg, or 1.8 mg.
USE IN SPECIFIC POPULATIONS
Pregnancy: VICTOZA should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. (8.1 )
Pregnancy
Risk Summary
Based on animal reproduction studies, there may be risks to the fetus from exposure to VICTOZA during pregnancy. VICTOZA should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Animal reproduction studies identified increased adverse developmental outcomes from exposure during pregnancy. Liraglutide exposure was associated with early embryonic deaths and an imbalance in some fetal abnormalities in pregnant rats administered liraglutide during organogenesis at doses that approximate clinical exposures at the maximum recommended human dose (MRHD) of 1.8 mg/day. In pregnant rabbits administered liraglutide during organogenesis, decreased fetal weight and an increased incidence of major fetal abnormalities were seen at exposures below the human exposures at the MRHD (see Animal Data) .
The estimated background risk of major birth defects for women with uncontrolled pre-gestational diabetes (Hemoglobin A 1c >7) is 6 to 10%. The major birth defect rate has been reported to be as high as 20 to 25% in women with a Hemoglobin A 1c >10. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Clinical Considerations
Disease-associated maternal and/or embryo/fetal risk
Poorly controlled diabetes in pregnancy increases the maternal risk for diabetic ketoacidosis, pre-eclampsia, spontaneous abortions, preterm delivery, and delivery complications. Poorly controlled diabetes increases the fetal risk for major birth defects, still birth, and macrosomia related morbidity.
Animal Data
Female rats given subcutaneous doses of 0.1, 0.25 and 1 mg/kg/day liraglutide beginning 2 weeks before mating through gestation day 17 had estimated systemic exposures 0.8-, 3-, and 11-times the human exposure at the MRHD based on plasma AUC comparison. The number of early embryonic deaths in the 1 mg/kg/day group increased slightly. Fetal abnormalities and variations in kidneys and blood vessels, irregular ossification of the skull, and a more complete state of ossification occurred at all doses. Mottled liver and minimally kinked ribs occurred at the highest dose. The incidence of fetal malformations in liraglutide-treated groups exceeding concurrent and historical controls were misshapen oropharynx and/or narrowed opening into larynx at 0.1 mg/kg/day and umbilical hernia at 0.1 and 0.25 mg/kg/day.
Pregnant rabbits given subcutaneous doses of 0.01, 0.025 and 0.05 mg/kg/day liraglutide from gestation day 6 through day 18 inclusive, had estimated systemic exposures less than the human exposure at the MRHD of 1.8 mg/day at all doses, based on plasma AUC. Liraglutide decreased fetal weight and dose-dependently increased the incidence of total major fetal abnormalities at all doses. The incidence of malformations exceeded concurrent and historical controls at 0.01 mg/kg/day (kidneys, scapula), ≥0.01 mg/kg/day (eyes, forelimb), 0.025 mg/kg/day (brain, tail and sacral vertebrae, major blood vessels and heart, umbilicus), ≥0.025 mg/kg/day (sternum) and at 0.05 mg/kg/day (parietal bones, major blood vessels). Irregular ossification and/or skeletal abnormalities occurred in the skull and jaw, vertebrae and ribs, sternum, pelvis, tail, and scapula; and dose-dependent minor skeletal variations were observed. Visceral abnormalities occurred in blood vessels, lung, liver, and esophagus. Bilobed or bifurcated gallbladder was seen in all treatment groups, but not in the control group.
In pregnant female rats given subcutaneous doses of 0.1, 0.25 and 1 mg/kg/day liraglutide from gestation day 6 through weaning or termination of nursing on lactation day 24, estimated systemic exposures were 0.8-, 3-, and 11-times human exposure at the MRHD of 1.8 mg/day, based on plasma AUC. A slight delay in parturition was observed in the majority of treated rats. Group mean body weight of neonatal rats from liraglutide-treated dams was lower than neonatal rats from control group dams. Bloody scabs and agitated behavior occurred in male rats descended from dams treated with 1 mg/kg/day liraglutide. Group mean body weight from birth to postpartum day 14 trended lower in F 2 generation rats descended from liraglutide-treated rats compared to F 2 generation rats descended from controls, but differences did not reach statistical significance for any group.
Lactation
Risk Summary
There are no data on the presence of VICTOZA in human milk, the effects on the breastfed infant, or the effects on milk production. Liraglutide was present in milk of lactating rats (see Data) .
Developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for VICTOZA and any potential adverse effects on the breastfed infant from VICTOZA or from the underlying maternal condition.
Data
In lactating rats, liraglutide was present unchanged in milk at concentrations approximately 50% of maternal plasma concentrations.
Pediatric Use
The safety and effectiveness of VICTOZA as an adjunct to diet and exercise to improve glycemic control in type 2 diabetes mellitus have been established in pediatric patients 10 years of age and older. Use of VICTOZA for this indication is supported by a 26-week placebo-controlled clinical trial and a 26-week open-label extension in 134 pediatric patients 10 to 17 years of age with type 2 diabetes mellitus, a pediatric pharmacokinetic study, and studies in adults with type 2 diabetes mellitus [see Clinical Pharmacology (12.3 ) and Clinical Studies (14.1 , 14.2 )] . The risk of hypoglycemia was higher with VICTOZA in pediatric patients regardless of insulin and/or metformin use [see Adverse Reactions (6.1 )] .
The safety and effectiveness of VICTOZA have not been established in pediatric patients less than 10 years of age.
Geriatric Use
In the VICTOZA treatment arms of the glycemic control trials, a total of 832 (19.3%) of the patients were 65 to 74 years of age and 145 (3.4%) were 75 years of age and over [see Clinical Studies (14.1 )] . In the VICTOZA treatment arm of the LEADER trial [see Clinical Studies (14.3 )] , a total of 1738 (37.2%) patients were 65 to 74 years of age, 401 (8.6%) were 75 to 84 years of age, and 17 (0.4%) were 85 years of age or older at baseline.
No overall differences in safety or effectiveness for VICTOZA have been observed between patients 65 years of age and older and younger patients.
Renal Impairment
No dose adjustment of VICTOZA is recommended for patients with renal impairment [see Clinical Pharmacology (12.3 )]. The safety and efficacy of VICTOZA was evaluated in a 26-week clinical study that included patients with moderate renal impairment (eGFR 30 to 60 mL/min/1.73 m 2 ) [see Clinical Studies (14.1 )].
In the VICTOZA treatment arm of the LEADER trial [see Clinical Studies (14.3 )] , 1,932 (41.4%) patients had mild renal impairment, 999 (21.4%) patients had moderate renal impairment and 117 (2.5%) patients had severe renal impairment at baseline. No overall differences in safety or efficacy were seen in these patients compared to patients with normal renal function.
There is limited experience with VICTOZA in patients with end stage renal disease.
Hepatic Impairment
There is limited experience in patients with mild, moderate or severe hepatic impairment. Therefore, VICTOZA should be used with caution in this patient population. No dose adjustment of VICTOZA is recommended for patients with hepatic impairment [see Clinical Pharmacology (12.3 )] .
CONTRAINDICATIONS
VICTOZA is contraindicated in patients with a:
- personal or family history of medullary thyroid carcinoma (MTC) or in patients with Multiple Endocrine Neoplasia syndrome type 2 (MEN 2) [see Warnings and Precautions (5.1 )] .
- serious hypersensitivity reaction to liraglutide or to any of the excipients in VICTOZA. Serious hypersensitivity reactions including anaphylactic reactions and angioedema have been reported with VICTOZA [see Warnings and Precautions (5.7 )].
WARNINGS AND PRECAUTIONS
- Acute Pancreatitis : Has been observed in patients treated with GLP-1 receptor agonists, including VICTOZA. Discontinue if pancreatitis is suspected. (5.2 )
- Never Share a VICTOZA Pen Between Patients , even if the needle is changed. (5.3)
- Hypoglycemia : Adult patients taking an insulin secretagogue or insulin may have an increased risk of hypoglycemia, including severe hypoglycemia. In pediatric patients 10 years of age and older, the risk of hypoglycemia was higher with VICTOZA regardless of insulin and/or metformin use. Reduction in the dose of insulin secretagogues or insulin may be necessary. (5.4)
- Acute Kidney Injury Due to Volume Depletion : Monitor renal function in patients reporting adverse reactions that could lead to volume depletion. (5.5)
- Severe Gastrointestinal Adverse Reactions: Use has been associated with gastrointestinal adverse reactions, sometimes severe. VICTOZA is not recommended in patients with severe gastroparesis. (5.6 )
- Hypersensitivity Reactions : Postmarketing reports of serious hypersensitivity reactions (e.g., anaphylactic reactions and angioedema). Discontinue VICTOZA and promptly seek medical advice. (5.7)
- Acute Gallbladder Disease : If cholelithiasis or cholecystitis are suspected, gallbladder studies are indicated. (5.8)
- Pulmonary Aspiration During General Anesthesia or Deep Sedation : Has been reported in patients receiving GLP-1 receptor agonists undergoing elective surgeries or procedures. Instruct patients to inform healthcare providers of any planned surgeries or procedures. (5.9 )
Risk of Thyroid C-cell Tumors
Liraglutide causes dose-dependent and treatment-duration-dependent thyroid C-cell tumors (adenomas and/or carcinomas) at clinically relevant exposures in both genders of rats and mice [see Nonclinical Toxicology (13.1 )] . Malignant thyroid C-cell carcinomas were detected in rats and mice. It is unknown whether VICTOZA will cause thyroid C-cell tumors, including medullary thyroid carcinoma (MTC), in humans, as the human relevance of liraglutide-induced rodent thyroid C-cell tumors has not been determined.
Cases of MTC in patients treated with VICTOZA have been reported in the postmarketing period; the data in these reports are insufficient to establish or exclude a causal relationship between MTC and VICTOZA use in humans.
VICTOZA is contraindicated in patients with a personal or family history of MTC or in patients with MEN 2. Counsel patients regarding the potential risk for MTC with the use of VICTOZA and inform them of symptoms of thyroid tumors (e.g., a mass in the neck, dysphagia, dyspnea, persistent hoarseness).
Routine monitoring of serum calcitonin or using thyroid ultrasound is of uncertain value for early detection of MTC in patients treated with VICTOZA. Such monitoring may increase the risk of unnecessary procedures, due to low test specificity for serum calcitonin and a high background incidence of thyroid disease. Significantly elevated serum calcitonin may indicate MTC and patients with MTC usually have calcitonin values >50 ng/L. If serum calcitonin is measured and found to be elevated, the patient should be further evaluated. Patients with thyroid nodules noted on physical examination or neck imaging should also be further evaluated.
Acute Pancreatitis
Acute pancreatitis, including fatal and non-fatal hemorrhagic or necrotizing pancreatitis, has been observed in patients treated with GLP-1 receptor agonists, including liraglutide [see Adverse Reactions (6 )] .
After initiation of VICTOZA, observe patients carefully for signs and symptoms of acute pancreatitis which may include persistent or severe abdominal pain (sometimes radiating to the back) and which may or may not be accompanied by nausea or vomiting. If pancreatitis is suspected, discontinue VICTOZA and initiate appropriate management.
Never Share a VICTOZA Pen Between Patients
VICTOZA pens must never be shared between patients, even if the needle is changed. Pen-sharing poses a risk for transmission of blood-borne pathogens.
Hypoglycemia
Adult patients receiving VICTOZA in combination with an insulin secretagogue (e.g., sulfonylurea) or insulin may have an increased risk of hypoglycemia, including severe hypoglycemia. In pediatric patients 10 years of age and older, the risk of hypoglycemia was higher with VICTOZA regardless of insulin and/or metformin use. [see Adverse Reactions (6.1) , Drug Interactions (7.2) ].
The risk of hypoglycemia may be lowered by a reduction in the dose of sulfonylurea (or other concomitantly administered insulin secretagogues) or insulin. Inform patients using these concomitant medications and pediatric patients of the risk of hypoglycemia and educate them on the signs and symptoms of hypoglycemia.
Acute Kidney Injury Due to Volume Depletion
There have been postmarketing reports of acute kidney injury, in some cases requiring hemodialysis, in patients treated with VICTOZA [see Adverse Reactions (6.2)] . The majority of the reported events occurred in patients who experienced gastrointestinal reactions leading to dehydration such as nausea, vomiting, or diarrhea [see Adverse Reactions (6.1)] . Monitor renal function in patients reporting adverse reactions to VICTOZA that could lead to volume depletion, especially during dosage initiation and escalation of VICTOZA. [see Use in Specific Populations (8.6)] .
Severe Gastrointestinal Adverse Reactions
Use of GLP-1 receptor agonists, including liraglutide, has been associated with gastrointestinal adverse reactions, sometimes severe [see Adverse Reactions (6 )] . In VICTOZA clinical trials, severe gastrointestinal adverse reactions were reported more frequently among patients receiving VICTOZA (1.2 mg 4.4%, 1.8 mg 4.2%) than placebo (1.1%). Severe gastrointestinal adverse reactions have also been reported postmarketing with GLP-1 receptor agonists. VICTOZA is not recommended in patients with severe gastroparesis.
Hypersensitivity Reactions
There have been postmarketing reports of serious hypersensitivity reactions (e.g., anaphylactic reactions and angioedema) in patients treated with VICTOZA [see Adverse Reactions (6.2 )] . If a hypersensitivity reaction occurs, discontinue VICTOZA; treat promptly per standard of care, and monitor until signs and symptoms resolve.
Anaphylaxis and angioedema have been reported with other GLP-1 receptor agonists. Use caution in a patient with a history of anaphylaxis or angioedema with another GLP-receptor agonist because it is unknown whether such patients will be predisposed to these reactions with VICTOZA. VICTOZA is contraindicated in patients who have had a serious hypersensitivity reaction to liraglutide or any of the excipients in VICTOZA [see Contraindications (4 )].
Acute Gallbladder Disease
Acute events of gallbladder disease such as cholelithiasis or cholecystitis have been reported in GLP-1 receptor agonist trials and postmarketing. In the LEADER trial [see Clinical Studies (14.3 )] , 3.1% of VICTOZA-treated patients versus 1.9% of placebo-treated patients reported an acute event of gallbladder disease, such as cholelithiasis or cholecystitis
[see Adverse Reactions (6.1 )] . If cholelithiasis is suspected, gallbladder studies and appropriate clinical follow-up are indicated.
Pulmonary Aspiration During General Anesthesia or Deep Sedation
VICTOZA delays gastric emptying [see Clinical Pharmacology (12.2 )] . There have been rare postmarketing reports of pulmonary aspiration in patients receiving GLP-1 receptor agonists undergoing elective surgeries or procedures requiring general anesthesia or deep sedation who had residual gastric contents despite reported adherence to preoperative fasting recommendations.
Available data are insufficient to inform recommendations to mitigate the risk of pulmonary aspiration during general anesthesia or deep sedation in patients taking VICTOZA, including whether modifying preoperative fasting recommendations or temporarily discontinuing VICTOZA could reduce the incidence of retained gastric contents. Instruct patients to inform healthcare providers prior to any planned surgeries or procedures if they are taking VICTOZA.
ADVERSE REACTIONS
The following serious adverse reactions are described below or elsewhere in the prescribing information:
- Risk of Thyroid C-cell Tumors [see Warnings and Precautions (5.1 )]
- Acute Pancreatitis [see Warnings and Precautions (5.2 )]
- Hypoglycemia [see Warnings and Precautions (5.4 )]
- Acute Kidney Injury Due to Volume Depletion [see Warnings and Precautions (5.5 )]
- Severe Gastrointestinal Adverse Reactions [see Warnings and Precautions (5.6 )]
- Hypersensitivity Reactions [see Warnings and Precautions (5.6 )]
- Acute Gallbladder Disease [see Warnings and Precautions (5.8 )]
- Pulmonary Aspiration During General Anesthesia or Deep Sedation [see Warnings and Precautions (5.9 )]
Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Common Adverse Reactions
The safety of VICTOZA in patients with type 2 diabetes mellitus was evaluated in 5 glycemic control, placebo-controlled trials in adults and one trial of 52 weeks duration in pediatric patients 10 years of age and older [see Clinical Studies (14.1 )] . The data in Table 1 reflect exposure of 1,673 adult patients to VICTOZA and a mean duration of exposure to VICTOZA of 37.3 weeks. The mean age of adult patients was 58 years, 4% were 75 years or older and 54% were male. The population was 79% White, 6% Black or African American, 13% Asian; 4% were of Hispanic or Latino ethnicity. At baseline the population had diabetes for an average of 9 years and a mean HbA 1c of 8.4%. Baseline estimated renal function was normal or mildly impaired in 88% and moderately impaired in 12% of the pooled population.
Table 1 shows common adverse reactions in adults, excluding hypoglycemia, associated with the use of VICTOZA for the treatment of type 2 diabetes mellitus. These adverse reactions occurred more commonly on VICTOZA than on placebo and occurred in at least 5% of patients treated with VICTOZA. Overall, the type, and severity of adverse reactions in pediatric patients 10 years of age and older and above were comparable to that observed in the adult population.
Table 1. Adverse reactions reported in ≥5% of Adult Patients Treated with VICTOZA for Type 2 Diabetes Mellitus
Placebo N=661 | Liraglutide 1.2 mg N= 645 | Liraglutide 1.8 mg N= 1024 | |
Adverse Reaction | (%) | (%) | (%) |
Nausea | 5 | 18 | 20 |
Diarrhea | 4 | 10 | 12 |
Headache | 7 | 11 | 10 |
Nasopharyngitis | 8 | 9 | 10 |
Vomiting | 2 | 6 | 9 |
Decreased appetite | 1 | 10 | 9 |
Dyspepsia | 1 | 4 | 7 |
Upper Respiratory Tract Infection | 6 | 7 | 6 |
Constipation | 1 | 5 | 5 |
Back Pain | 3 | 4 | 5 |
Cumulative proportions were calculated combining studies using Cochran-Mantel-Haenszel weights.
In an analysis of placebo- and active-controlled trials, the types and frequency of common adverse reactions, excluding hypoglycemia, were similar to those listed in Table 1 .
Other Adverse Reactions
Gastrointestinal Adverse Reactions
In the pool of 5 glycemic control, placebo-controlled adult clinical trials, withdrawals due to gastrointestinal adverse reactions, occurred in 4.3% of VICTOZA-treated patients and 0.5% of placebo-treated patients. Severe gastrointestinal adverse reactions were reported more frequently among patients receiving VICTOZA (1.2 mg 4.4%, 1.8 mg 4.2%) than placebo (1.1%). Withdrawal due to gastrointestinal adverse events mainly occurred during the first 2 to 3 months of the trials.
Injection site reactions
Injection site reactions (e.g., injection site rash, erythema) were reported in approximately 2% of VICTOZA-treated adult patients in the five double-blind, glycemic control trials of at least 26 weeks duration. Less than 0.2% of VICTOZA-treated patients discontinued due to injection site reactions.
Hypoglycemia
In 5 adult glycemic control, placebo-controlled clinical trials of at least 26 weeks duration, hypoglycemia requiring the assistance of another person for treatment occurred in 8 VICTOZA-treated patients (7.5 events per 1,000 patient-years). Of these 8 VICTOZA-treated patients, 7 patients were concomitantly using a sulfonylurea.
|
| |
Add-on to Metformin | Placebo + Metformin (N=121) | VICTOZA + Metformin
|
Patient not able to self-treat |
|
|
Patient able to self-treat |
|
|
Add-on to Glimepiride |
|
|
Patient not able to self-treat |
|
|
Patient able to self-treat |
|
|
Not classified |
|
|
Add-on to Metformin + Rosiglitazone |
(N=175) | VICTOZA + Metformin + Rosiglitazone
|
Patient not able to self-treat |
|
|
Patient able to self-treat |
|
|
Not classified |
|
|
Add-on to Metformin + Glimepiride |
(N=114) | VICTOZA + Metformin + Glimepiride
|
Patient not able to self-treat |
|
|
Patient able to self-treat |
|
|
Not classified |
|
|
“Patient not able to self-treat” is defined as an event requiring the assistance of another person for treatment.
In a 26-week placebo-controlled clinical trial in pediatric patients 10 years of age and older with a 26-week open-label extension, 21.2% of VICTOZA-treated patients (mean age 14.6 years) with type 2 diabetes mellitus, had hypoglycemia with a blood glucose <54 mg/dL with or without symptoms (335 events per 1,000 patient years). No severe hypoglycemic episodes occurred in the VICTOZA treatment group (severe hypoglycemia was defined as an episode requiring assistance of another person to actively administer carbohydrate, glucagon, or other resuscitative actions).
Papillary thyroid carcinoma
In adult glycemic control trials of VICTOZA, there were 7 reported cases of papillary thyroid carcinoma in patients treated with VICTOZA and 1 case in a comparator-treated patient (1.5 vs. 0.5 cases per 1,000 patient-years). Most of these papillary thyroid carcinomas were <1 cm in greatest diameter and were diagnosed in surgical pathology specimens after thyroidectomy prompted by findings on protocol-specified screening with serum calcitonin or thyroid ultrasound.
Pancreatitis
In glycemic control trials of VICTOZA, there have been 13 cases of pancreatitis among VICTOZA-treated patients and 1 case in a comparator (glimepiride) treated patient (2.7 vs. 0.5 cases per 1,000 patient-years). Nine of the 13 cases with VICTOZA were reported as acute pancreatitis and four were reported as chronic pancreatitis. In one case in a VICTOZA-treated patient, pancreatitis, with necrosis, was observed and led to death; however clinical causality could not be established. Some patients had other risk factors for pancreatitis, such as a history of cholelithiasis or alcohol abuse.
Cholelithiasis and cholecystitis
In adult glycemic control trials of VICTOZA, the incidence of cholelithiasis was 0.3% in both VICTOZA-treated and placebo-treated patients. The incidence of cholecystitis was 0.2% in both VICTOZA-treated and placebo-treated patients.
In the LEADER trial [see Clinical Studies (14.3 )] , the incidence of cholelithiasis was 1.5% (3.9 cases per 1,000 patient years of observation) in adult VICTOZA-treated and 1.1% (2.8 cases per 1,000 patient years of observation) in placebo-treated patients, both on a background of standard of care. The incidence of acute cholecystitis was 1.1% (2.9 cases per 1,000 patient years of observation) in adult VICTOZA-treated and 0.7% (1.9 cases per 1,000 patient years of observation) in placebo-treated patients. The majority of events required hospitalization or cholecystectomy.
Laboratory Tests
Bilirubin
In the five adult glycemic control trials of at least 26 weeks duration, mildly elevated serum bilirubin concentrations (elevations to no more than twice the upper limit of the reference range) occurred in 4% of VICTOZA-treated patients, 2.1% of placebo-treated patients and 3.5% of active-comparator-treated patients. This finding was not accompanied by abnormalities in other liver tests. The significance of this isolated finding is unknown.
Calcitonin
Calcitonin, a biological marker of MTC, was measured throughout the clinical development program. At the end of the adult glycemic control trials, adjusted mean serum calcitonin concentrations were higher in VICTOZA-treated patients compared to placebo-treated patients but not compared to patients receiving active comparator. Between group differences in adjusted mean serum calcitonin values were approximately 0.1 ng/L or less. Among adult patients with pretreatment calcitonin <20 ng/L, calcitonin elevations to >20 ng/L occurred in 0.7% of VICTOZA-treated patients, 0.3% of placebo-treated patients, and 0.5% of active-comparator-treated patients. The clinical significance of these findings is unknown.
Lipase and Amylase
In one adult glycemic control trial in renal impairment patients, a mean increase of 33% for lipase and 15% for amylase from baseline was observed for VICTOZA-treated patients while placebo-treated patients had a mean decrease in lipase of 3% and a mean increase in amylase of 1%.
In the LEADER trial, serum lipase and amylase were routinely measured. Among adult VICTOZA-treated patients, 7.9% had a lipase value at any time during treatment of greater than or equal to 3 times the upper limit of normal compared with 4.5% of placebo-treated patients, and 1% of VICTOZA-treated patients had an amylase value at any time during treatment of greater than or equal to 3 times the upper limit of normal versus 0.7% of placebo-treated patients.
The clinical significance of elevations in lipase or amylase with VICTOZA is unknown in the absence of other signs and symptoms of pancreatitis [see Warnings and Precautions (5.2 )].
Vital signs
VICTOZA did not have adverse effects on blood pressure. Mean increases from baseline in heart rate of 2 to 3 beats per minute have been observed in adult patients treated with VICTOZA compared to placebo.
Postmarketing Experience
The following additional adverse reactions have been reported during post-approval use of VICTOZA. Because these events are reported voluntarily from a population of uncertain size, it is generally not possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
- Gastrointestinal: Acute pancreatitis; hemorrhagic and necrotizing pancreatitis sometimes resulting in death; ileus, intestinal obstruction, severe constipation including fecal impaction, nausea, vomiting and diarrhea leading to dehydration
- Hepatobiliary: Elevations of liver enzymes, hyperbilirubinemia, cholestasis, cholecystitis, cholelithiasis requiring cholecystectomy, hepatitis
- Hypersensitivity: Angioedema, anaphylactic reactions, pruritus
- Neoplasms: Medullary thyroid carcinoma
- Neurologic: Dysgeusia, dizziness, dysesthesia
- Pulmonary: Pulmonary aspiration has occurred in patients receiving GLP-1 receptor agonists undergoing elective surgeries or procedures requiring general anesthesia or deep sedation.
- Renal: Acute renal failure or worsening of chronic renal failure, sometimes requiring hemodialysis; and increased serum creatinine
- Skin and subcutaneous tissue: Cutaneous amyloidosis, alopecia
DRUG INTERACTIONS
- Effects of delayed gastric emptying on oral medications: VICTOZA delays gastric emptying and may impact absorption of concomitantly administered oral medications. (7 )
Effects of Delayed Gastric Emptying on Oral Medications
VICTOZA causes a delay of gastric emptying, and thereby has the potential to impact the absorption of concomitantly administered oral medications. In clinical pharmacology trials, VICTOZA did not affect the absorption of the tested orally administered medications to any clinically relevant degree [see Clinical Pharmacology (12.3 )] . Nonetheless, caution should be exercised when oral medications are concomitantly administered with VICTOZA.
Concomitant Use with an Insulin Secretagogue (e.g., Sulfonylurea) or with Insulin
VICTOZA stimulates insulin release in the presence of elevated blood glucose concentrations. Patients receiving VICTOZA in combination with an insulin secretagogue (e.g., sulfonylurea) or insulin may have an increased risk of hypoglycemia, including severe hypoglycemia. When initiating VICTOZA, consider reducing the dose of concomitantly administered insulin secretagogues (such as sulfonylureas) or insulin to reduce the risk of hypoglycemia [see Warnings and Precautions (5.4 ), Adverse Reactions (6.1 )].
DESCRIPTION
VICTOZA contains liraglutide, an analog of human GLP-1 and acts as a GLP-1 receptor agonist. The peptide precursor of liraglutide, produced by a process that includes expression of recombinant DNA in Saccharomyces cerevisiae, has been engineered to be 97% homologous to native human GLP-1 by substituting arginine for lysine at position 34. Liraglutide is made by attaching a C-16 fatty acid (palmitic acid) with a glutamic acid spacer on the remaining lysine residue at position 26 of the peptide precursor. The molecular formula of liraglutide is C 172 H 265 N 43 O 51 and the molecular weight is 3751.2 Daltons. The structural formula ( Figure 1 ) is:

Figure 1. Structural Formula of liraglutide
VICTOZA injection is a sterile, aqueous, clear, colorless or almost colorless solution for subcutaneous use. Each 1 mL of VICTOZA solution contains 6 mg of liraglutide and the following inactive ingredients: disodium phosphate dihydrate, 1.42 mg; propylene glycol, 14 mg; phenol, 5.5 mg; and water for injection. VICTOZA has a pH of approximately 8.15, hydrochloric acid or sodium hydroxide may be added to adjust pH. Each prefilled pen contains a 3 mL solution of VICTOZA equivalent to 18 mg liraglutide (free-base, anhydrous).
CLINICAL PHARMACOLOGY
Mechanism of Action
Liraglutide is an acylated human GLP-1 receptor agonist with 97% amino acid sequence homology to endogenous human GLP-1(7-37). GLP-1(7-37) represents <20% of total circulating endogenous GLP-1. Like GLP-1(7-37), liraglutide activates the GLP-1 receptor, a membrane-bound cell-surface receptor coupled to adenylyl cyclase by the stimulatory G-protein, Gs, in pancreatic beta cells. Liraglutide increases intracellular cyclic AMP (cAMP) leading to insulin release in the presence of elevated glucose concentrations. This insulin secretion subsides as blood glucose concentrations decrease and approach euglycemia. Liraglutide also decreases glucagon secretion in a glucose-dependent manner. The mechanism of blood glucose lowering also involves a delay in gastric emptying.
GLP-1(7-37) has a half-life of 1.5 to 2 minutes due to degradation by the ubiquitous endogenous enzymes, dipeptidyl peptidase 4 (DPP-4) and neutral endopeptidases (NEP). Unlike native GLP-1, liraglutide is stable against metabolic degradation by both peptidases and has a plasma half-life of 13 hours after subcutaneous administration. The pharmacokinetic profile of liraglutide, which makes it suitable for once daily administration, is a result of self-association that delays absorption, plasma protein binding and stability against metabolic degradation by DPP-4 and NEP.
Pharmacodynamics
VICTOZA’s pharmacodynamic profile is consistent with its pharmacokinetic profile observed after single subcutaneous administration as VICTOZA lowered fasting, premeal and postprandial glucose throughout the day [see Clinical Pharmacology (12.3 )] .
Fasting and postprandial glucose was measured before and up to 5 hours after a standardized meal after treatment to steady state with 0.6, 1.2 and 1.8 mg VICTOZA or placebo. Compared to placebo, the postprandial plasma glucose AUC 0-300min was 35% lower after VICTOZA 1.2 mg and 38% lower after VICTOZA 1.8 mg.
Glucose-dependent insulin secretion
The effect of a single dose of 7.5 mcg/kg (~0.7 mg) VICTOZA on insulin secretion rates (ISR) was investigated in 10 patients with type 2 diabetes mellitus during graded glucose infusion. In these patients, on average, the ISR response was increased in a glucose-dependent manner ( Figure 2 ).

Figure 2. Mean Insulin Secretion Rate (ISR) versus Glucose Concentration Following Single-Dose VICTOZA 7.5 mcg/kg (~ 0.7 mg) or Placebo in Patients with Type 2 Diabetes Mellitus (N=10) During Graded Glucose Infusion
Glucagon secretion
VICTOZA lowered blood glucose by stimulating insulin secretion and lowering glucagon secretion. A single dose of VICTOZA 7.5 mcg/kg (~0.7 mg) did not impair glucagon response to low glucose concentrations.
Gastric emptying
VICTOZA causes a delay of gastric emptying, thereby reducing the rate at which postprandial glucose appears in the circulation.
Cardiac Electrophysiology (QTc)
The effect of VICTOZA on cardiac repolarization was tested in a QTc study. VICTOZA at steady state concentrations with daily doses up to 1.8 mg did not produce QTc prolongation.
Pharmacokinetics
Absorption
Following subcutaneous administration, maximum concentrations of liraglutide are achieved at 8 to 12 hours post dosing. The mean peak (C max ) and total (AUC) exposures of liraglutide were 35 ng/mL and 960 ng·h/mL, respectively, for a subcutaneous single dose of 0.6 mg. After subcutaneous single dose administrations, C max and AUC of liraglutide increased proportionally over the therapeutic dose range of 0.6 mg to 1.8 mg. At 1.8 mg VICTOZA, the average steady state concentration of liraglutide over 24 hours was approximately 128 ng/mL. AUC 0-∞ was equivalent between upper arm and abdomen, and between upper arm and thigh. AUC 0-∞ from thigh was 22% lower than that from abdomen. However, liraglutide exposures were considered comparable among these three subcutaneous injection sites. Absolute bioavailability of liraglutide following subcutaneous administration is approximately 55%.
Distribution
The mean apparent volume of distribution after subcutaneous administration of VICTOZA 0.6 mg is approximately 13 L. The mean volume of distribution after intravenous administration of VICTOZA is 0.07 L/kg. Liraglutide is extensively bound to plasma protein (>98%).
Elimination
The mean apparent clearance following subcutaneous administration of a single dose of liraglutide is approximately 1.2 L/h with an elimination half-life of approximately 13 hours.
Metabolism
During the initial 24 hours following administration of a single [ 3 H]-liraglutide dose to healthy subjects, the major component in plasma was intact liraglutide. Liraglutide is endogenously metabolized in a similar manner to large proteins without a specific organ as a major route of elimination.
Excretion
Following a [ 3 H]-liraglutide dose, intact liraglutide was not detected in urine or feces. Only a minor part of the administered radioactivity was excreted as liraglutide-related metabolites in urine or feces (6% and 5%, respectively). The majority of urine and feces radioactivity was excreted during the first 6 to 8 days.
Specific Populations
Geriatric Patients
Age had no effect on the pharmacokinetics of VICTOZA based on a pharmacokinetic study in healthy elderly subjects (65 to 83 years) and population pharmacokinetic analyses of patients 18 to 80 years of age [see Use in Specific Populations (8.5 )] .
Pediatric Patients
A population pharmacokinetic analysis was conducted for VICTOZA using data from 72 pediatric patients (10 to 17 years of age) with type 2 diabetes mellitus. The pharmacokinetic profile of VICTOZA in pediatric patients was consistent with that in adults.
Male and Female Patients
Based on the results of population pharmacokinetic analyses, females have 25% lower weight-adjusted clearance of VICTOZA compared to males.
Race or Ethnic Groups
Race and ethnicity had no effect on the pharmacokinetics of VICTOZA based on the results of population pharmacokinetic analyses that included White, Black or African American, Asian and Hispanic or Latino/Non-Hispanic or Latino subjects.
Body Weight
Body weight significantly affects the pharmacokinetics of VICTOZA based on results of population pharmacokinetic analyses. The exposure of liraglutide decreases with an increase in baseline body weight. However, the 1.2 mg and 1.8 mg daily doses of VICTOZA provided adequate systemic exposures over the body weight range of 40 kg to 160 kg evaluated in the clinical trials. Liraglutide was not studied in patients with body weight >160 kg.
Patients with Renal Impairment
The single-dose pharmacokinetics of VICTOZA were evaluated in patients with varying degrees of renal impairment. Patients with mild (estimated creatinine clearance 50-80 mL/min) to severe (estimated creatinine clearance <30 mL/min) renal impairment and subjects with end-stage renal disease requiring dialysis were included in the trial. Compared to healthy subjects, liraglutide AUC in mild, moderate, and severe renal impairment and in end-stage renal disease was on average 35%, 19%, 29% and 30% lower, respectively [see Use in Specific Populations (8.6 )] .
Patients with Hepatic Impairment
The single-dose pharmacokinetics of VICTOZA were evaluated in patients with varying degrees of hepatic impairment. Patients with mild (Child Pugh score 5-6) to severe (Child Pugh score >9) hepatic impairment were included in the trial. Compared to healthy subjects, liraglutide AUC in patients with mild, moderate and severe hepatic impairment was on average 11%, 14% and 42% lower, respectively [see Use in Specific Populations (8.7 )] .
Drug Interaction Studies
In vitro assessment of drug-drug interactions
VICTOZA has low potential for pharmacokinetic drug-drug interactions related to cytochrome P450 (CYP450) and plasma protein binding.
In vivo assessment of drug-drug interactions
The drug-drug interaction studies were performed at steady state with VICTOZA 1.8 mg/day. Before administration of concomitant treatment, subjects underwent a 0.6 mg weekly dose increase to reach the maximum dose of 1.8 mg/day. Administration of the interacting drugs was timed so that C max of VICTOZA (8 h to 12 h) would coincide with the absorption peak of the co-administered drugs.
Digoxin
A single dose of digoxin 1 mg was administered 7 hours after the dose of VICTOZA at steady state. The concomitant administration with VICTOZA resulted in a reduction of digoxin AUC by 16%; C max decreased by 31%. Digoxin median time to maximal concentration (T max ) was delayed from 1 h to 1.5 h.
Lisinopril
A single dose of lisinopril 20 mg was administered 5 minutes after the dose of VICTOZA at steady state. The coadministration with VICTOZA resulted in a reduction of lisinopril AUC by 15%; C max decreased by 27%. Lisinopril median T max was delayed from 6 h to 8 h with VICTOZA.
Atorvastatin
VICTOZA did not change the overall exposure (AUC) of atorvastatin following a single dose of atorvastatin 40 mg, administered 5 hours after the dose of VICTOZA at steady state. Atorvastatin C max was decreased by 38% and median T max was delayed from 1 h to 3 h with VICTOZA.
Acetaminophen
VICTOZA did not change the overall exposure (AUC) of acetaminophen following a single dose of acetaminophen 1000 mg, administered 8 hours after the dose of VICTOZA at steady state. Acetaminophen C max was decreased by 31% and median T max was delayed up to 15 minutes.
Griseofulvin
VICTOZA did not change the overall exposure (AUC) of griseofulvin following coadministration of a single dose of griseofulvin 500 mg with VICTOZA at steady state. Griseofulvin C max increased by 37% while median T max did not change.
Oral Contraceptives
A single dose of an oral contraceptive combination product containing 0.03 mg ethinylestradiol and 0.15 mg levonorgestrel was administered under fed conditions and 7 hours after the dose of VICTOZA at steady state. VICTOZA lowered ethinylestradiol and levonorgestrel C max by 12% and 13%, respectively. There was no effect of VICTOZA on the overall exposure (AUC) of ethinylestradiol. VICTOZA increased the levonorgestrel AUC 0-∞ by 18%. VICTOZA delayed T max for both ethinylestradiol and levonorgestrel by 1.5 h.
Insulin Detemir
No pharmacokinetic interaction was observed between VICTOZA and insulin detemir when separate subcutaneous injections of insulin detemir 0.5 Unit/kg (single-dose) and VICTOZA 1.8 mg (steady state) were administered in patients with type 2 diabetes mellitus.
Immunogenicity
The observed incidence of anti-drug antibodies is highly dependent on the sensitivity and specificity of the assay. Differences in assay methods preclude meaningful comparisons of the incidence of anti-drug antibodies in the studies described below with the incidence of anti-drug antibodies in other studies, including those with VICTOZA or other liraglutide products.
A subset of VICTOZA-treated patients (1,104 of 2,501, 44%) in five adult double-blind clinical trials of 26 weeks duration or longer were tested for the presence of anti-liraglutide antibodies at the end of treatment [see Clinical Studies (14.1 )] and 102/1,104 (9%) of VICTOZA-treated patients developed anti-liraglutide antibodies. Of these 102 VICTOZA-treated patients, 56 (5%) patients developed antibodies that cross-reacted with native GLP-1. These cross-reacting antibodies were not tested for neutralizing effect against native GLP-1, and thus the potential for clinically significant neutralization of native GLP-1 was not assessed. Antibodies that had a neutralizing effect on liraglutide in an in vitro assay occurred in 12 (1%) of the VICTOZA-treated patients. There was no identified clinically significant effect of anti-liraglutide antibodies on effectiveness of VICTOZA.
In five double-blind adult glycemic control trials of VICTOZA, events from a composite of adverse events potentially related to immunogenicity (e.g., urticaria, angioedema) occurred among 0.8% of VICTOZA-treated patients and among 0.4% of comparator-treated patients. Urticaria accounted for approximately one-half of the events in this composite for VICTOZA-treated patients. Patients who developed anti-liraglutide antibodies were not more likely to develop events from the immunogenicity events composite than were patients who did not develop anti-liraglutide antibodies.
In the LEADER trial [see Clinical Studies (14.3 )] , anti-liraglutide antibodies were detected in 11 out of the 1247 (0.9%) adult VICTOZA-treated patients with antibody measurements. Of the 11 adult VICTOZA-treated patients who developed anti-liraglutide antibodies, none were observed to develop neutralizing antibodies to liraglutide, and 5 patients (0.4%) developed cross-reacting antibodies against native GLP-1.
In a clinical trial with pediatric patients aged 10 years and older [see Clinical Studies (14.2 )], anti-liraglutide antibodies were detected in 1 (2%) VICTOZA treated patient at week 26 and 5 (9%) VICTOZA treated patients at week 53. None of the 5 patients had antibodies cross reactive to native GLP-1 or had neutralizing antibodies.
NONCLINICAL TOXICOLOGY
Carcinogenesis, Mutagenesis, Impairment of Fertility
A 104-week carcinogenicity study was conducted in male and female CD-1 mice at doses of 0.03, 0.2, 1, and 3 mg/kg/day liraglutide administered by bolus subcutaneous injection yielding systemic exposures 0.2-, 2-, 10- and 45-times the human exposure, respectively, at the MRHD of 1.8 mg/day based on plasma AUC comparison. A dose-related increase in benign thyroid C-cell adenomas was seen in the 1 and the 3 mg/kg/day groups with incidences of 13% and 19% in males and 6% and 20% in females, respectively. C-cell adenomas did not occur in control groups or 0.03 and 0.2 mg/kg/day groups. Treatment-related malignant C-cell carcinomas occurred in 3% of females in the 3 mg/kg/day group. Thyroid C-cell tumors are rare findings during carcinogenicity testing in mice. A treatment-related increase in fibrosarcomas was seen on the dorsal skin and subcutis, the body surface used for drug injection, in males in the 3 mg/kg/day group. These fibrosarcomas were attributed to the high local concentration of drug near the injection site. The liraglutide concentration in the clinical formulation (6 mg/mL) is 10-times higher than the concentration in the formulation used to administer 3 mg/kg/day liraglutide to mice in the carcinogenicity study (0.6 mg/mL).
A 104-week carcinogenicity study was conducted in male and female Sprague Dawley rats at doses of 0.075, 0.25 and 0.75 mg/kg/day liraglutide administered by bolus subcutaneous injection with exposures 0.5-, 2- and 8-times the human exposure, respectively, resulting from the MRHD based on plasma AUC comparison. A treatment-related increase in benign thyroid C-cell adenomas was seen in males in 0.25 and 0.75 mg/kg/day liraglutide groups with incidences of 12%, 16%, 42%, and 46% and in all female liraglutide-treated groups with incidences of 10%, 27%, 33%, and 56% in 0 (control), 0.075, 0.25, and 0.75 mg/kg/day groups, respectively. A treatment-related increase in malignant thyroid C-cell carcinomas was observed in all male liraglutide-treated groups with incidences of 2%, 8%, 6%, and 14% and in females at 0.25 and 0.75 mg/kg/day with incidences of 0%, 0%, 4%, and 6% in 0 (control), 0.075, 0.25, and 0.75 mg/kg/day groups, respectively. Thyroid C-cell carcinomas are rare findings during carcinogenicity testing in rats.
Studies in mice demonstrated that liraglutide-induced C-cell proliferation was dependent on the GLP-1 receptor and that liraglutide did not cause activation of the REarranged during Transfection (RET) proto-oncogene in thyroid C-cells.
Human relevance of thyroid C-cell tumors in mice and rats is unknown and has not been determined by clinical studies or nonclinical studies [see Boxed Warning , Warnings and Precautions (5.1 )] .
Liraglutide was negative with and without metabolic activation in the Ames test for mutagenicity and in a human peripheral blood lymphocyte chromosome aberration test for clastogenicity. Liraglutide was negative in repeat-dose in vivo micronucleus tests in rats.
In rat fertility studies using subcutaneous doses of 0.1, 0.25 and 1 mg/kg/day liraglutide, males were treated for 4 weeks prior to and throughout mating and females were treated 2 weeks prior to and throughout mating until gestation day 17. No direct adverse effects on male fertility was observed at doses up to 1 mg/kg/day, a high dose yielding an estimated systemic exposure 11- times the human exposure at the MRHD, based on plasma AUC. In female rats, an increase in early embryonic deaths occurred at 1 mg/kg/day. Reduced body weight gain and food consumption were observed in females at the 1 mg/kg/day dose.
CLINICAL STUDIES
Glycemic Control Trials in Adults with Type 2 Diabetes Mellitus
In glycemic control trials in adults, VICTOZA has been studied as monotherapy and in combination with one or two oral anti-diabetic medications or basal insulin. VICTOZA was also studied in a cardiovascular outcomes trial (LEADER trial).
In each of the placebo controlled trials, treatment with VICTOZA produced clinically and statistically significant improvements in hemoglobin A 1c and fasting plasma glucose (FPG) compared to placebo.
All VICTOZA-treated patients started at 0.6 mg/day. The dose was increased in weekly intervals by 0.6 mg to reach 1.2 mg or 1.8 mg for patients randomized to these higher doses. VICTOZA 0.6 mg is not effective for glycemic control and is intended only as a starting dose to reduce gastrointestinal intolerance [see Dosage and Administration (2 )] .
Monotherapy
In this 52-week trial, 746 adult patients with type 2 diabetes mellitus were randomized to VICTOZA 1.2 mg, VICTOZA 1.8 mg, or glimepiride 8 mg. Patients who were randomized to glimepiride were initially treated with 2 mg daily for two weeks, increasing to 4 mg daily for another two weeks, and finally increasing to 8 mg daily. Treatment with VICTOZA 1.8 mg and 1.2 mg resulted in a statistically significant reduction in HbA 1c compared to glimepiride ( Table 3 ). The percentage of patients who discontinued due to ineffective therapy was 3.6% in the VICTOZA 1.8 mg treatment group, 6% in the VICTOZA 1.2 mg treatment group, and 10.1% in the glimepiride-treatment group.
The mean age of participants was 53 years, and the mean duration of diabetes was 5 years. Participants were 49.7% male, 77.5% White, 12.6% Black or African American and 35% of Hispanic or Latino ethnicity. The mean BMI was 33.1 kg/m 2 .
Table 3. Results of a 52-week Monotherapy Trial in Adults with Type 2 Diabetes Mellitus a
VICTOZA 1.8 mg | VICTOZA 1.2 mg |
| |
Intent-to-Treat Population (N) | 246 | 251 |
|
HbA 1c (%) (Mean) | |||
Baseline | 8.2 | 8.2 |
|
Change from baseline (adjusted mean) b | -1.1 | -0.8 |
|
Difference from glimepiride arm (adjusted mean) b | -0.6•• | -0.3• | |
95% Confidence Interval | (-0.8, -0.4) | (-0.5, -0.1) | |
Percentage of patients achieving HbA 1c <7% | 51 | 43 |
|
Fasting Plasma Glucose (mg/dL) (Mean) | |||
Baseline | 172 | 168 |
|
Change from baseline (adjusted mean) b | -26 | -15 |
|
Difference from glimepiride arm (adjusted mean) b | -20•• | -10• | |
95% Confidence Interval | (-29, -12) | (-19, -1) | |
Body Weight (kg) (Mean) | |||
Baseline | 92.6 | 92.1 |
|
Change from baseline (adjusted mean) b | -2.5 | -2.1 |
|
Difference from glimepiride arm (adjusted mean) b | -3.6•• | -3.2•• | |
95% Confidence Interval | (-4.3, -2.9) | (-3.9, -2.5) |
a Intent-to-treat population using last observation on study
b Least squares mean adjusted for baseline value
• p-value <0.05
•• p-value <0.0001

Figure 3. Mean HbA 1c for Adult Patients with Type 2 Diabetes Mellitus who Completed the 52-week Trial and for the Last Observation Carried Forward (LOCF, intent-to-treat) data at Week 52 (Monotherapy)
Combination Therapy
Add-on to Metformin
In this 26-week trial, 1,091 adult patients with type 2 diabetes mellitus were randomized to VICTOZA 0.6 mg, VICTOZA 1.2 mg, VICTOZA 1.8 mg, placebo, or glimepiride 4 mg (one-half of the maximal approved dose in the United States), all as add-on to metformin. Randomization occurred after a 6-week run-in period consisting of a 3-week initial forced metformin titration period followed by a maintenance period of another 3 weeks. During the titration period, doses of metformin were increased up to 2,000 mg/day. Treatment with VICTOZA 1.2 mg and 1.8 mg as add-on to metformin resulted in a significant mean HbA 1c reduction relative to placebo add-on to metformin and resulted in a similar mean HbA 1c reduction relative to glimepiride 4 mg add-on to metformin ( Table 4 ). The percentage of patients who discontinued due to ineffective therapy was 5.4% in the VICTOZA 1.8 mg + metformin treatment group, 3.3% in the VICTOZA 1.2 mg + metformin treatment group, 23.8% in the placebo + metformin treatment group, and 3.7% in the glimepiride + metformin treated group.
The mean age of participants was 57 years, and the mean duration of diabetes was 7 years. Participants were 58.2% male, 87.1% White and 2.4% Black or African American. The mean BMI was 31.0 kg/m 2 .
Table 4. Results of a 26-week Trial of VICTOZA as Add-on to Metformin in Adults with Type 2 Diabetes Mellitus a
VICTOZA 1.8 mg + Metformin | VICTOZA 1.2 mg + Metformin |
|
| |
Intent-to-Treat Population (N) | 242 | 240 |
|
|
HbA 1c (%) (Mean) | ||||
Baseline | 8.4 | 8.3 |
|
|
Change from baseline (adjusted mean) b | -1 | -1 |
|
|
Difference from placebo + metformin arm (adjusted mean) b | -1.1•• | -1.1•• | ||
95% Confidence Interval | (-1.3, -0.9) | (-1.3, -0.9) | ||
Difference from glimepiride + metformin arm (adjusted mean) b | 0 | 0 | ||
95% Confidence Interval | (-0.2, 0.2) | (-0.2, 0.2) | ||
Percentage of patients achieving HbA 1c <7% | 42 | 35 |
|
|
Fasting Plasma Glucose (mg/dL) (Mean) | ||||
Baseline | 181 | 179 |
|
|
Change from baseline (adjusted mean) b | -30 | -30 |
|
|
Difference from placebo + metformin arm (adjusted mean) b | -38•• | -37•• | ||
95% Confidence Interval | (-48, -27) | (-47, -26) | ||
Difference from glimepiride + metformin arm (adjusted mean) b | -7 | -6 | ||
95% Confidence Interval | (-16, 2) | (-15, 3) | ||
Body Weight (kg) (Mean) | ||||
Baseline | 88 | 88.5 |
|
|
Change from baseline (adjusted mean) b | -2.8 | -2.6 |
|
|
Difference from placebo + metformin arm (adjusted mean) b 95% Confidence Interval | -1.3• (-2.2, -0.4) | -1.1• (-2, -0.2) | ||
Difference from glimepiride + metformin arm (adjusted mean) b | -3.8•• | -3.5•• | ||
95% Confidence Interval | (-4.5, -3.0) | (-4.3, -2.8) | ||
a Intent-to-treat population using last observation on study b Least squares mean adjusted for baseline value † For glimepiride, one-half of the maximal approved United States dose. • p-value <0.05 •• p-value <0.0001 | ||||
VICTOZA Compared to Sitagliptin, Both as Add-on to Metformin
In this 26–week, open-label trial, 665 adult patients with type 2 diabetes mellitus on a background of metformin ≥1,500 mg per day were randomized to VICTOZA 1.2 mg once daily, VICTOZA 1.8 mg once daily or sitagliptin 100 mg once daily, all dosed according to approved labeling. Patients were to continue their current treatment on metformin at a stable, pre-trial dose level and dosing frequency.
The mean age of participants was 56 years, and the mean duration of diabetes was 6 years. Participants were 52.9% male, 86.6% White, 7.2% Black or African American and 16.2% of Hispanic or Latino ethnicity. The mean BMI was 32.8 kg/m 2 .
The primary endpoint was the change in HbA 1c from baseline to Week 26. Treatment with VICTOZA 1.2 mg and VICTOZA 1.8 mg resulted in statistically significant reductions in HbA 1c relative to sitagliptin 100 mg ( Table 5 ). The percentage of patients who discontinued due to ineffective therapy was 3.1% in the VICTOZA 1.2 mg group, 0.5% in the VICTOZA 1.8 mg treatment group, and 4.1% in the sitagliptin 100 mg treatment group. From a mean baseline body weight of 94 kg, there was a mean reduction of 2.7 kg for VICTOZA 1.2 mg, 3.3 kg for VICTOZA 1.8 mg, and 0.8 kg for sitagliptin 100 mg.
Table 5. Results of a 26-week Open-label Trial of VICTOZA Compared to Sitagliptin (both in combination with metformin) in Adults with Type 2 Diabetes Mellitus a
VICTOZA 1.8 mg + Metformin | VICTOZA 1.2 mg + Metformin | Sitagliptin 100 mg + Metformin | |
Intent-to-Treat Population (N) | 218 | 221 |
|
HbA 1c (%) (Mean) | |||
Baseline | 8.4 | 8.4 |
|
Change from baseline (adjusted mean) | -1.5 | -1.2 |
|
Difference from sitagliptin arm (adjusted mean) b 95% Confidence Interval | -0.6•• (-0.8, -0.4) | -0.3•• (-0.5, -0.2) | |
Percentage of patients achieving HbA 1c <7% | 56 | 44 |
|
Fasting Plasma Glucose (mg/dL) (Mean) | |||
Baseline | 179 | 182 |
|
Change from baseline (adjusted mean) | -39 | -34 |
|
Difference from sitagliptin arm (adjusted mean) b 95% Confidence Interval | -24•• (-31, -16) | -19•• (-26, -12) |
a Intent-to-treat population using last observation on study
b Least squares mean adjusted for baseline value
•• p-value <0.0001

Figure 4. Mean HbA 1c for Adult Patients with Type 2 Diabetes Mellitus who Completed the 26-week Trial and for the Last Observation Carried Forward (LOCF, intent-to-treat) data at Week 26
Combination Therapy with Metformin and Insulin
This 26-week open-label trial enrolled 988 adult patients with type 2 diabetes mellitus with inadequate glycemic control (HbA 1c 7% to 10%) on metformin (≥1,500 mg/day) alone or inadequate glycemic control (HbA 1c 7% to 8.5%) on metformin (≥1,500 mg/day) and a sulfonylurea. Patients who were on metformin and a sulfonylurea discontinued the sulfonylurea then all patients entered a 12-week run-in period during which they received add-on therapy with VICTOZA titrated to 1.8 mg once-daily. At the end of the run-in period, 498 patients (50%) achieved HbA 1c <7% with VICTOZA 1.8 mg and metformin and continued treatment in a non-randomized, observational arm. Another 167 patients (17%) withdrew from the trial during the run-in period with approximately one-half of these patients doing so because of gastrointestinal adverse reactions [see Adverse Reactions (6.1 )] . The remaining 323 patients with HbA 1c ≥7% (33% of those who entered the run-in period) were randomized to 26 weeks of once-daily insulin detemir administered in the evening as add-on therapy (N=162) or to continued, unchanged treatment with VICTOZA 1.8 mg and metformin (N=161). The starting dose of insulin detemir was 10 units/day and the mean dose at the end of the 26-week randomized period was 39 units/day. During the 26 week randomized treatment period, the percentage of patients who discontinued due to ineffective therapy was 11.2% in the group randomized to continued treatment with VICTOZA 1.8 mg and metformin and 1.2% in the group randomized to add-on therapy with insulin detemir.
The mean age of participants was 57 years, and the mean duration of diabetes was 8 years. Participants were 55.7% male, 91.3% White, 5.6% Black or African American and 12.5% of Hispanic or Latino ethnicity. The mean BMI was 34 kg/m 2 .
Treatment with insulin detemir as add-on to VICTOZA 1.8 mg + metformin resulted in statistically significant reductions in HbA 1c and FPG compared to continued, unchanged treatment with VICTOZA 1.8 mg + metformin alone ( Table 6 ). From a mean baseline body weight of 96 kg after randomization, there was a mean reduction of 0.3 kg in the patients who received insulin detemir add-on therapy compared to a mean reduction of 1.1 kg in the patients who continued on unchanged treatment with VICTOZA 1.8 mg + metformin alone.
Table 6. Results of a 26-week Open-label Trial of Insulin detemir as add on to VICTOZA + Metformin Compared to Continued Treatment with VICTOZA + Metformin alone in Adult Patients with Type 2 Diabetes Mellitus not Achieving HbA 1c <7% after 12 weeks of Metformin and VICTOZA a
Insulin detemir + VICTOZA + Metformin | VICTOZA + Metformin | |
Intent-to-Treat Population (N) | 162 | 157 |
HbA 1c (%) (Mean) | ||
Baseline (week 0) | 7.6 | 7.6 |
Change from baseline (adjusted mean) | -0.5 | 0 |
| -0.5•• | |
| (-0.7, -0.4) | |
Percentage of patients achieving HbA 1c <7% | 43 | 17 |
Fasting Plasma Glucose (mg/dL) (Mean) | ||
Baseline (week 0) | 166 | 159 |
Change from baseline (adjusted mean) | -39 | -7 |
| -31•• | |
| (-39, -23) |
a Intent-to-treat population using last observation on study
b Least squares mean adjusted for baseline value
•• p-value <0.0001
Add-on to Sulfonylurea
In this 26-week trial, 1,041 adult patients with type 2 diabetes mellitus were randomized to VICTOZA 0.6 mg, VICTOZA 1.2 mg, VICTOZA 1.8 mg, placebo, or rosiglitazone 4 mg (one-half of the maximal approved dose in the United States), all as add-on to glimepiride. Randomization occurred after a 4-week run-in period consisting of an initial, 2-week, forced-glimepiride titration period followed by a maintenance period of another 2 weeks. During the titration period, doses of glimepiride were increased to 4 mg/day. The doses of glimepiride could be reduced (at the discretion of the investigator) from 4 mg/day to 3 mg/day or 2 mg/day (minimum) after randomization, in the event of unacceptable hypoglycemia or other adverse events.
The mean age of participants was 56 years, and the mean duration of diabetes was 8 years. Participants were 49.4% male, 64.4% White and 2.8% Black or African American. The mean BMI was 29.9 kg/m 2 .
Treatment with VICTOZA 1.2 mg and 1.8 mg as add-on to glimepiride resulted in a statistically significant reduction in mean HbA 1c compared to placebo add-on to glimepiride ( Table 7 ). The percentage of patients who discontinued due to ineffective therapy was 3% in the VICTOZA 1.8 mg + glimepiride treatment group, 3.5% in the VICTOZA 1.2 mg + glimepiride treatment group, 17.5% in the placebo + glimepiride treatment group, and 6.9% in the rosiglitazone + glimepiride treatment group.
Table 7. Results of a 26-week Trial of VICTOZA as add-on to Sulfonylurea in Adult Patients with Type 2 Diabetes Mellitus a
VICTOZA 1.8 mg + Glimepiride | VICTOZA 1.2 mg + Glimepiride |
|
| |
Intent-to-Treat Population (N) | 234 | 228 |
|
|
HbA 1c (%) (Mean) | ||||
| 8.5 | 8.5 |
|
|
| -1.1 | -1.1 |
|
|
| -1.4•• | -1.3•• | ||
| (-1.6, -1.1) | (-1.5, -1.1) | ||
Percentage of patients achieving HbA 1c <7% | 42 | 35 |
|
|
Fasting Plasma Glucose (mg/dL) (Mean) | ||||
| 174 | 177 |
|
|
| -29 | -28 |
|
|
| -47•• | -46•• | ||
| (-58, -35) | (-58, -35) | ||
| ||||
| 83 | 80 |
|
|
| -0.2 | +0.3 |
|
|
| -0.1 | 0.4 | ||
| (-0.9, 0.6) | (-0.4, 1.2) |
a Intent-to-treat population using last observation on study
b Least squares mean adjusted for baseline value
† For rosiglitazone, one-half of the maximal approved United States dose.
•• p-value <0.0001
Add-on to Metformin and Sulfonylurea
In this 26-week trial, 581 adult patients with type 2 diabetes mellitus were randomized to VICTOZA 1.8 mg, placebo, or insulin glargine, all as add-on to metformin and glimepiride. Randomization took place after a 6-week run-in period consisting of a 3-week forced metformin and glimepiride titration period followed by a maintenance period of another 3 weeks. During the titration period, doses of metformin and glimepiride were to be increased up to 2,000 mg/day and 4 mg/day, respectively. After randomization, patients randomized to VICTOZA 1.8 mg underwent a 2 week period of titration with VICTOZA. During the trial, the VICTOZA and metformin doses were fixed, although glimepiride and insulin glargine doses could be adjusted. Patients titrated glargine twice-weekly during the first 8 weeks of treatment based on self-measured fasting plasma glucose on the day of titration. After Week 8, the frequency of insulin glargine titration was left to the discretion of the investigator, but, at a minimum, the glargine dose was to be revised, if necessary, at Weeks 12 and 18. Only 20% of glargine-treated patients achieved the pre-specified target fasting plasma glucose of ≤100 mg/dL. Therefore, optimal titration of the insulin glargine dose was not achieved in most patients.
The mean age of participants was 58 years, and the mean duration of diabetes was 9 years. Participants were 56.5% male, 75.0% White and 3.6% Black or African American. The mean BMI was 30.5 kg/m 2 .
Treatment with VICTOZA as add-on to glimepiride and metformin resulted in a statistically significant mean reduction in HbA 1c compared to placebo add-on to glimepiride and metformin ( Table 8 ). The percentage of patients who discontinued due to ineffective therapy was 0.9% in the VICTOZA 1.8 mg + metformin + glimepiride treatment group, 0.4% in the insulin glargine + metformin + glimepiride treatment group, and 11.3% in the placebo + metformin + glimepiride treatment group.
Table 8. Results of a 26-week Trial of VICTOZA as Add-on to Metformin and Sulfonylurea in Adult Patients with Type 2 Diabetes Mellitus a
VICTOZA 1.8 mg + Metformin + Glimepiride | Placebo + Metformin + Glimepiride | Insulin glargine † + Metformin + Glimepiride | |
Intent-to-Treat Population (N) | 230 | 114 |
|
HbA 1c (%) (Mean) | |||
Baseline | 8.3 | 8.3 |
|
Change from baseline (adjusted mean) b | -1.3 | -0.2 |
|
| -1.1•• | ||
| (-1.3, -0.9) | ||
Percentage of patients achieving HbA 1c <7% | 53 | 15 |
|
Fasting Plasma Glucose (mg/dL) (Mean) | |||
Baseline | 165 | 170 |
|
Change from baseline (adjusted mean) b | -28 | +10 |
|
| -38•• | ||
| (-46, -30) | ||
Body Weight (kg) (Mean) | |||
Baseline | 85.8 | 85.4 |
|
Change from baseline (adjusted mean) b | -1.8 | -0.4 |
|
| -1.4• | ||
| (-2.1, -0.7) |
a Intent-to-treat population using last observation on study
b Least squares mean adjusted for baseline value
† For insulin glargine, optimal titration regimen was not achieved for 80% of patients.
• p-value <0.05
•• p-value <0.0001
VICTOZA Compared to Exenatide, Both as Add-on to Metformin and/or Sulfonylurea Therapy
In this 26-week, open-label trial, 464 adult patients with type 2 diabetes mellitus on a background of metformin monotherapy, sulfonylurea monotherapy or a combination of metformin and sulfonylurea were randomized to once daily VICTOZA 1.8 mg or exenatide 10 mcg twice daily. Maximally tolerated doses of background therapy were to remain unchanged for the duration of the trial. Patients randomized to exenatide started on a dose of 5 mcg twice-daily for 4 weeks and then were escalated to 10 mcg twice-daily.
The mean age of participants was 57 years, and the mean duration of diabetes was 8 years. Participants were 51.9% male, 91.8% White, 5.4% Black or African American and 12.3% of Hispanic or Latino ethnicity. The mean BMI was 32.9 kg/m 2 .
Treatment with VICTOZA 1.8 mg resulted in statistically significant reductions in HbA 1c and FPG relative to exenatide ( Table 9 ). The percentage of patients who discontinued for ineffective therapy was 0.4% in the VICTOZA treatment group and 0% in the exenatide treatment group. Both treatment groups had a mean decrease from baseline in body weight of approximately 3 kg.
Table 9. Results of a 26-week Open-label trial of VICTOZA versus Exenatide (both in combination with metformin and/or sulfonylurea) in Adult Patients with Type 2 Diabetes Mellitus a
VICTOZA 1.8 mg once daily + metformin and/or sulfonylurea | Exenatide 10 mcg twice daily + metformin and/or sulfonylurea | |
Intent-to-Treat Population (N) | 233 | 231 |
HbA 1c (%) (Mean) | ||
Baseline | 8.2 | 8.1 |
Change from baseline (adjusted mean) b | -1.1 | -0.8 |
Difference from exenatide arm (adjusted mean) b 95% Confidence Interval | -0.3•• (-0.5, -0.2) | |
Percentage of patients achieving HbA 1c <7% | 54 | 43 |
Fasting Plasma Glucose (mg/dL) (Mean) | ||
Baseline | 176 | 171 |
Change from baseline (adjusted mean) b | -29 | -11 |
Difference from exenatide arm (adjusted mean) b 95% Confidence Interval | -18•• (-25, -12) |
a Intent-to-treat population using last observation carried forward
b Least squares mean adjusted for baseline value
•• p-value <0.0001
Add-on to Metformin and Thiazolidinedione
In this 26-week trial, 533 adult patients with type 2 diabetes mellitus were randomized to VICTOZA 1.2 mg, VICTOZA 1.8 mg or placebo, all as add-on to rosiglitazone (8 mg) plus metformin (2,000 mg). Patients underwent a 9 week run-in period (3-week forced dose escalation followed by a 6-week dose maintenance phase) with rosiglitazone (starting at 4 mg and increasing to 8 mg/day within 2 weeks) and metformin (starting at 500 mg with increasing weekly increments of 500 mg to a final dose of 2,000 mg/day). Only patients who tolerated the final dose of rosiglitazone (8 mg/day) and metformin (2000 mg/day) and completed the 6-week dose maintenance phase were eligible for randomization into the trial.
The mean age of participants was 55 years, and the mean duration of diabetes was 9 years. Participants were 61.6% male, 84.2% White, 10.2% Black or African American and 16.4% of Hispanic or Latino ethnicity. The mean BMI was 33.9 kg/m 2 .
Treatment with VICTOZA as add-on to metformin and rosiglitazone produced a statistically significant reduction in mean HbA 1c compared to placebo add-on to metformin and rosiglitazone ( Table 10 ). The percentage of patients who discontinued due to ineffective therapy was 1.7% in the VICTOZA 1.8 mg + metformin + rosiglitazone treatment group, 1.7% in the VICTOZA 1.2 mg + metformin + rosiglitazone treatment group, and 16.4% in the placebo + metformin + rosiglitazone treatment group.
Table 10. Results of a 26-week Trial of VICTOZA as Add-on to Metformin and Thiazolidinedione in Adult Patients with Type 2 Diabetes Mellitus a
VICTOZA 1.8 mg + Metformin + Rosiglitazone | VICTOZA 1.2 mg + Metformin + Rosiglitazone | Placebo + Metformin +
| |
Intent-to-Treat Population (N) | 178 | 177 |
|
HbA 1c (%) (Mean) | |||
Baseline | 8.6 | 8.5 |
|
Change from baseline (adjusted mean) b | -1.5 | -1.5 |
|
| -0.9•• | -0.9•• | |
| (-1.1, -0.8) | (-1.1, -0.8) | |
Percentage of patients achieving HbA 1c <7% | 54 | 57 |
|
Fasting Plasma Glucose (mg/dL) (Mean) | |||
Baseline | 185 | 181 |
|
Change from baseline (adjusted mean) b | -44 | -40 |
|
| -36•• | -32•• | |
| (-44, -27) | (-41, -23) | |
Body Weight (kg) (Mean) | |||
Baseline | 94.9 | 95.3 |
|
Change from baseline (adjusted mean) b | -2 | -1 |
|
| -2.6•• | -1.6•• | |
| (-3.4, -1.8) | (-2.4, -1.0) |
a Intent-to-treat population using last observation on study
b Least squares mean adjusted for baseline value
•• p-value <0.0001
VICTOZA Compared to Placebo Both With or Without metformin and/or Sulfonylurea and/or Pioglitazone and/or Basal or Premix insulin in Patients with Type 2 Diabetes Mellitus and Moderate Renal Impairment
In this 26-week, double-blind, randomized, placebo-controlled, parallel-group trial in adult patients with type 2 diabetes mellitus, 279 patients with moderate renal impairment, as per MDRD formula (eGFR 30-59 mL/min/1.73 m 2 ), were randomized to VICTOZA or placebo once daily. VICTOZA was added to the patient’s stable pre-trial antidiabetic regimen (insulin therapy and/or metformin, pioglitazone, or sulfonylurea). The dose of VICTOZA was escalated according to approved labeling to achieve a dose of 1.8 mg per day. The insulin dose was reduced by 20% at randomization for patients with baseline HbA 1c ≤8% and fixed until liraglutide dose escalation was complete. Dose reduction of insulin and SU was allowed in case of hypoglycemia; up titration of insulin was allowed but not beyond the pre-trial dose.
The mean age of participants was 67 years, and the mean duration of diabetes was 15 years. Participants were 50.5% male, 92.3% White, 6.6% Black or African American, and 7.2% of Hispanic or Latino ethnicity. The mean BMI was 33.9 kg/m 2 . Approximately half of patients had an eGFR between 30 and <45 mL/min/1.73 m 2 .
Treatment with VICTOZA resulted in a statistically significant reduction in HbA 1c from baseline at Week 26 compared to placebo (see Table 11 ). 123 patients reached the 1.8 mg dose of VICTOZA.
Table 11. Results of a 26-week Trial of VICTOZA Compared to Placebo in Adult Patients with Type 2 Diabetes Mellitus and Moderate Renal Impairment a
VICTOZA 1.8 mg + insulin and/or OAD | Placebo + insulin and/or OAD | |
Intent to Treat Population (N) | 140 | 137 |
HbA 1c (%) | ||
Baseline (mean) | 8.1 | 8.0 |
Change from baseline (estimated mean) b, c | -0.9 | -0.4 |
Difference from placebo b, c 95% Confidence Interval | -0.6• (-0.8, -0.3) | |
Proportion achieving HbA 1c < 7% d | 39.3 | 19.7 |
FPG (mg/dL) | ||
Baseline (mean) | 171 | 167 |
Change from baseline (estimated mean) e | -22 | -10 |
Difference from placebo e 95% Confidence Interval | -12•• (-23, -0.8) |
a Intent-to-treat population
b Estimated using a mixed model for repeated measurement with treatment, country, stratification groups as factors and baseline as a covariate, all nested within visit. Multiple imputation method modeled “wash out” of the treatment effect for patients having missing data who discontinued treatment.
c Early treatment discontinuation, before week 26, occurred in 25% and 22% of VICTOZA and placebo patients, respectively.
d Based on the known number of subjects achieving HbA 1c < 7%. When applying the multiple imputation method described in b) above, the estimated percents achieving HbA 1c < 7% are 47.6% and 24.9% for VICTOZA and placebo, respectively.
e Estimated using a mixed model for repeated measurement with treatment, country, stratification groups as factors and baseline as a covariate, all nested within visit.
• p-value <0.0001
•• p-value <0.05
Glycemic Control Trial in Pediatric Patients Aged 10 Years and Older with Type 2 Diabetes Mellitus
VICTOZA was evaluated in a 26-week, double-blind, randomized, parallel group, placebo controlled multi-center trial (NCT01541215), in 134 pediatric patients with type 2 diabetes mellitus aged 10 years and older . Patients were randomized to VICTOZA once-daily or placebo once-daily in combination with metformin with or without basal insulin treatment. All patients were on a metformin dose of 1000 to 2000 mg prior to randomization. The basal insulin dose was decreased by 20% at randomization and VICTOZA was titrated weekly by 0.6 mg for 2 to 3 weeks based on tolerability and an average fasting plasma glucose goal of ≤110 mg/dL.
The mean age was 14.6 years: 29.9% were ages 10-14 years, and 70.1% were greater than 14 years of age. 38.1% were male, 64.9% were White, 13.4% were Asian, 11.9% were Black or African American; 29.1% were of Hispanic or Latino ethnicity. The mean BMI was 33.9 kg/m 2 and the mean BMI SDS was 2.9. 18.7% of patients were using basal insulin at baseline. The mean duration of diabetes was 1.9 years and the mean HbA 1c was 7.8%.
At week 26, treatment with VICTOZA was superior in reducing HbA 1c from baseline versus placebo. The estimated treatment difference in HbA 1c reduction from baseline between VICTOZA and placebo was -1.06% with a 95% confidence interval of [-1.65%; -0.46%] (see Table 12 ).
Table 12. Results at week 26 in a trial comparing VICTOZA in combination with metformin with or without basal insulin versus Placebo in combination with metformin with or without basal insulin in Pediatric Patients Aged 10 Years and Older with Type 2 Diabetes Mellitus
VICTOZA+metformin±basal insulin | Placebo+metformin±basal insulin | |
N | 66 | 68 |
HbA 1c (%) | ||
Baseline | 7.9 | 7.7 |
End of 26 weeks | 7.1 | 8.2 |
Adjusted mean change from baseline after 26 weeks a | -0.64 | 0.42 |
Treatment difference [95% CI] VICTOZA vs Placebo | -1.06 [-1.65; -0.46]• | |
Percentage of patients achieving HbA 1c <7% b | 63.7 | 36.5 |
FPG (mg/dL) | ||
Baseline | 157 | 147 |
End of 26 weeks | 132 | 166 |
Adjusted mean change from baseline after 26 weeks a | -19.4 | 14.4 |
Treatment difference [95% CI] VICTOZA vs Placebo | -33.83 [-55.74; -11.92] | |
a The change from baseline to end of treatment visit in HbA 1c and FPG was analyzed using a pattern mixture model with multiple imputation. Missing observations (10.6% in the VICTOZA, 14.5% in the placebo) were imputed from the placebo arm based on multiple (x10,000) imputations. The data for week 26 was then analyzed with an ANCOVA model containing treatment, sex and age group as fixed effects and baseline value as covariate.
b Categories are derived from continuous measurements of HbA 1c using a pattern mixture model with multiple imputation for missing observations.
• p-value <0.001
Cardiovascular Outcomes Trial in Adult Patients with Type 2 Diabetes Mellitus and Atherosclerotic Cardiovascular Disease
The LEADER trial (NCT01179048) was a multi-national, multi-center, placebo-controlled, double-blind trial. In this study, 9,340 adult patients with inadequately controlled type 2 diabetes mellitus and atherosclerotic cardiovascular disease (CVD) were randomized to VICTOZA 1.8 mg or placebo for a median duration of 3.5 years. The study compared the risk of major adverse cardiovascular events between VICTOZA and placebo when these were added to, and used concomitantly with, background standard of care treatments for type 2 diabetes mellitus. The primary endpoint, major adverse cardiac events (MACE), was the time to first occurrence of a three part composite outcome which included; cardiovascular death, non-fatal myocardial infarction and non-fatal stroke.
Patients eligible to enter the trial were; 50 years of age or older and had established, stable, cardiovascular, cerebrovascular, peripheral artery disease, chronic kidney disease or New York Heart Association (NYHA) class II and III heart failure (80% of the enrolled population) or were 60 years of age or older and had other specified risk factors for cardiovascular disease (20% of the enrolled population).
At baseline, demographic and disease characteristics were balanced. The mean age was 64 years and the population was 64.3% male, 77.5% White, 10.0% Asian, and 8.3% Black or African American. In the study, 12.1% of the population identified as Hispanic or Latino ethnicity. The mean duration of type 2 diabetes mellitus was 12.8 years, the mean HbA 1c was 8.7% and the mean BMI was 32.5 kg/m 2 . A history of previous myocardial infarction was reported in 31% of randomized individuals, a prior revascularization procedure in 39%, a prior ischemic stroke in 11%, documented symptomatic coronary disease in 9%, documented asymptomatic cardiac ischemia in 26%, and a diagnosis of NYHA class II to III heart failure in 14%. The mean eGFR at baseline was 79 mL/min/1.73 m 2 and 41.8% of patients had mild renal impairment (eGFR 60 to 90 mL/min/1.73m 2 ) , 20.7% had moderate renal impairment (eGFR 30 to 60 mL/min/1.73 m 2 ) and 2.4% of patients had severe renal impairment (eGFR <30 mL/min/1.73 m 2 ).
At baseline, patients treated their diabetes with; diet and exercise only (3.9%), oral antidiabetic drugs only (51.5%), oral antidiabetic drugs and insulin (36.7%) or insulin only (7.9%). The most common background antidiabetic drugs used at baseline and in the trial were metformin, sulfonylurea and insulin. Use of DPP-4 inhibitors and other GLP-1 receptor agonists was excluded by protocol and sodium-glucose cotransporter-2 (SGLT-2) inhibitors were either not approved or not widely available. At baseline, cardiovascular disease and risk factors were managed with; non-diuretic antihypertensives (92.4%), diuretics (41.8%), statin therapy (72.1%) and platelet aggregation inhibitors (66.8%). During the trial, investigators could modify anti-diabetic and cardiovascular medications to achieve local standard of care treatment targets with respect to blood glucose, lipid, and blood pressure, and manage patients recovering from an acute coronary syndrome or stroke event per local treatment guidelines.
For the primary analysis, a Cox proportional hazards model was used to test for non-inferiority against the pre-specified risk margin of 1.3 for the hazard ratio of MACE and to test for superiority on MACE if non-inferiority was demonstrated. Type 1 error was controlled across multiple tests.
VICTOZA significantly reduced the occurrence of MACE. The estimated hazard ratio (95% CI) for time to first MACE was 0.87 (0.78, 0.97). Refer to Figure 5 and Table 13 .
Vital status was available for 99.7% of subjects in the trial. A total of 828 deaths were recorded during the LEADER trial. A majority of the deaths in the trial were categorized as cardiovascular deaths and non-cardiovascular deaths were balanced between the treatment groups (3.5% in patients treated with VICTOZA and 3.6% in patients treated with placebo). The estimated hazard ratio of time to all-cause death for VICTOZA compared to placebo was 0.85 (0.74, 0.97).

Figure 5. Kaplan-Meier: Time to First Occurrence of a MACE in the LEADER Trial (Patients with Type 2 Diabetes Mellitus and Atherosclerotic CVD)
Table 13. Treatment Effect for the Primary Composite Endpoint, MACE, and its Components in the LEADER Trial (Patients with Type 2 Diabetes Mellitus and Atherosclerotic CVD) a
VICTOZA N=4668 | Placebo N=4672 | Hazard Ratio (95% CI) b | |
Composite of cardiovascular death, non-fatal myocardial infarction, non-fatal stroke (MACE) (time to first occurrence) c | 608 (13.0%) | 694 (14.9%) | 0.87 (0.78; 0.97) |
Non-fatal myocardial infarction d | 281 (6.0%) | 317 (6.8%) | 0.88 (0.75;1.03) |
Non-fatal stroke d | 159 (3.4%) | 177 (3.8%) | 0.89 (0.72;1.11) |
Cardiovascular death d | 219 (4.7%) | 278 (6%) | 0.78 (0.66;0.93) |
a Full analysis set (all randomized patients)
b Cox-proportional hazards model with treatment as a factor
c p-value for superiority (2-sided) 0.011
d Number and percentage of first events
HOW SUPPLIED/STORAGE AND HANDLING
How Supplied
VICTOZA Injection: 18 mg/3 mL (6 mg/mL) clear, colorless solution in a prefilled, single-patient-use pen that delivers doses of 0.6 mg, 1.2 mg, or 1.8 mg is available in the following package sizes:
2 x VICTOZA pen NDC 0169-4060-12
3 x VICTOZA pen NDC 0169-4060-13
Recommended Storage
Prior to first use, VICTOZA should be stored in a refrigerator between 36ºF to 46ºF (2ºC to 8ºC). Do not store in the freezer or directly adjacent to the refrigerator cooling element. Do not freeze VICTOZA and do not use VICTOZA if it has been frozen.
After first use of the VICTOZA pen, the pen can be stored for 30 days at controlled room temperature 59°F to 86°F (15°C to 30°C) or in a refrigerator 36°F to 46°F (2°C to 8°C). Keep the pen cap on when not in use. Protect VICTOZA from excessive heat and sunlight. Always remove and safely discard the needle after each injection and store the VICTOZA pen without an injection needle attached. This will reduce the potential for contamination, infection, and leakage while also ensuring dosing accuracy. Always use a new needle for each injection to prevent contamination.
Instructions for Use
Victoza (liraglutide) injection
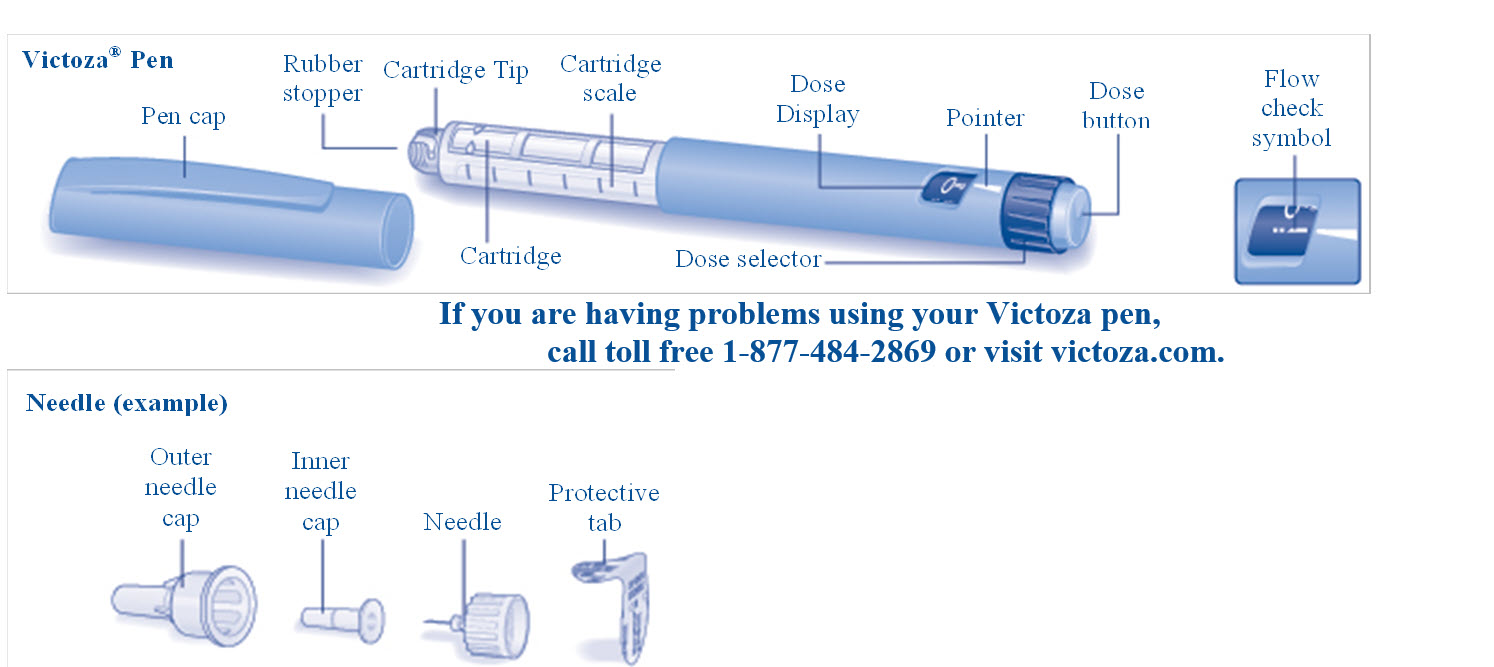 | |
First read the Medication Guide that comes with your Victoza single-patient use pen and then read this Instructions for Use for information about how to use your Victoza pen the right way. These instructions do not take the place of talking with your healthcare provider about your medical condition or your treatment. Do not share your Victoza Pen with other people, even if the needle has been changed. You may give other people a serious infection, or get a serious infection from them. Your Victoza pen is a disposable single-patient-use prefilled pen injector that contains 3 mL of Victoza and will deliver doses of 0.6 mg, 1.2 mg or 1.8 mg. The number of doses that you can take with a Victoza pen depends on the dose of medicine that is prescribed for you. Your healthcare provider will tell you how much Victoza to take. Talk to your healthcare provider or pharmacist for more information about needles for your Victoza pen. Important Information
Supplies you will need to give your Victoza injection:
See “Remove and Dispose of the Needle” at the end of these instructions. | |
First Time Use for Each New Pen | |
Step A. Check the Pen
| 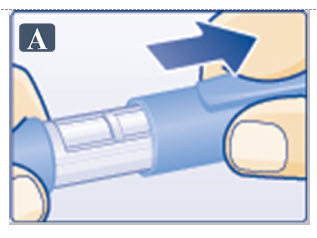 |
Step B. Attach the Needle
| 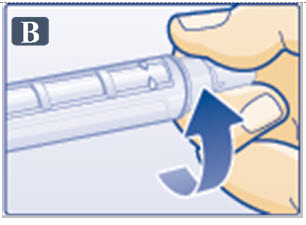 |
| 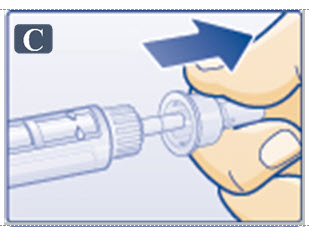 |
| 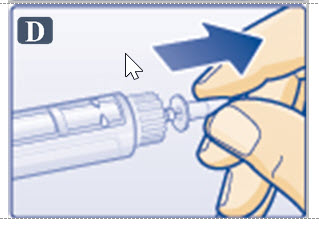 |
Step C. Dial to the Flow Check Symbol This step is done only One Time for each new pen and is Only required the first time you use a new pen.
|  |
Step D. Prepare the Pen
|  |
If you still see no drop of Victoza, use a new pen and contact Novo Nordisk at 1-877-484-2869. Continue to Step G under “Routine Use” | 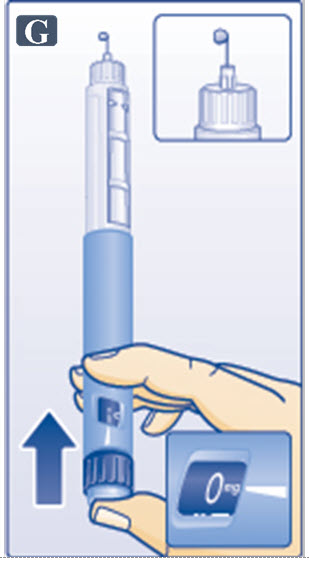 |
Routine Use | |
Step E. Check the Pen
| 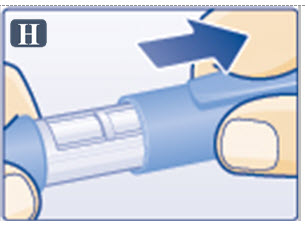 |
Step F. Attach the Needle
| 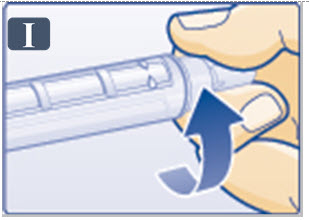 |
| 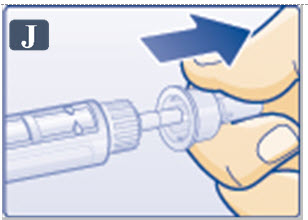 |
|  |
Step G. Dial the Dose | |
| 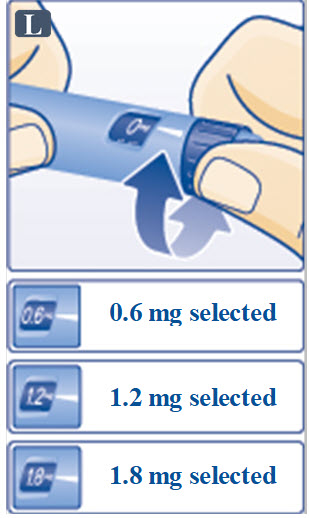 |
| |
| |
Step H. Injecting the Dose | |
| 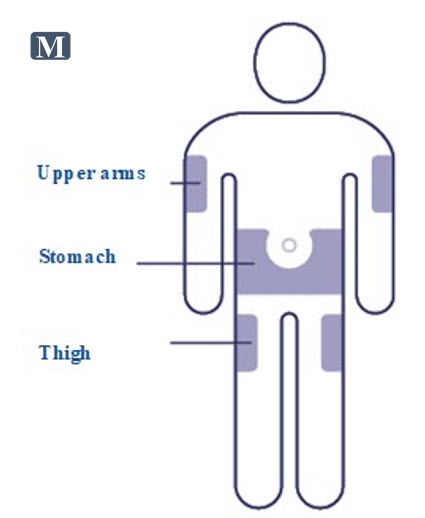 |
|  |
| |
|  |
Step I. Withdraw Needle | |
| 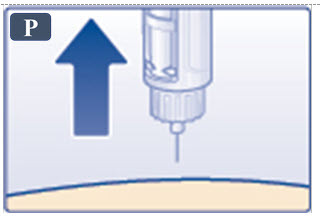 |
Step J. Remove and Dispose of the Needle | |
| 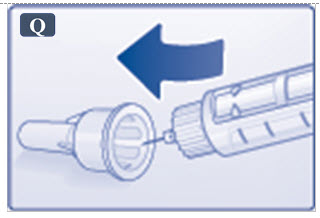 |
| |
Caring for your Victoza pen | |
| 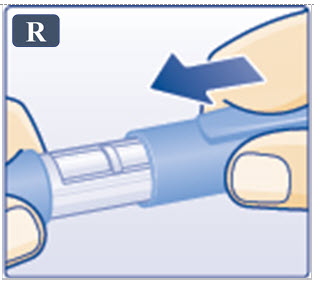 |
How should I store Victoza?
| |
| |
Mechanism of Action
Liraglutide is an acylated human GLP-1 receptor agonist with 97% amino acid sequence homology to endogenous human GLP-1(7-37). GLP-1(7-37) represents <20% of total circulating endogenous GLP-1. Like GLP-1(7-37), liraglutide activates the GLP-1 receptor, a membrane-bound cell-surface receptor coupled to adenylyl cyclase by the stimulatory G-protein, Gs, in pancreatic beta cells. Liraglutide increases intracellular cyclic AMP (cAMP) leading to insulin release in the presence of elevated glucose concentrations. This insulin secretion subsides as blood glucose concentrations decrease and approach euglycemia. Liraglutide also decreases glucagon secretion in a glucose-dependent manner. The mechanism of blood glucose lowering also involves a delay in gastric emptying.
GLP-1(7-37) has a half-life of 1.5 to 2 minutes due to degradation by the ubiquitous endogenous enzymes, dipeptidyl peptidase 4 (DPP-4) and neutral endopeptidases (NEP). Unlike native GLP-1, liraglutide is stable against metabolic degradation by both peptidases and has a plasma half-life of 13 hours after subcutaneous administration. The pharmacokinetic profile of liraglutide, which makes it suitable for once daily administration, is a result of self-association that delays absorption, plasma protein binding and stability against metabolic degradation by DPP-4 and NEP.
 Always use a new needle for each injection to prevent contamination.
Always use a new needle for each injection to prevent contamination.  Always remove the needle after each injection, and store your pen without the needle attached. This reduces the risk of contamination, infection, leakage of liraglutide, blocked needles and inaccurate dosing.
Always remove the needle after each injection, and store your pen without the needle attached. This reduces the risk of contamination, infection, leakage of liraglutide, blocked needles and inaccurate dosing.  Keep your Victoza pen and all medicines out of the reach of children.
Keep your Victoza pen and all medicines out of the reach of children.  If you drop your Victoza pen, repeat “ First Time Use for Each New Pen ” (steps A through D).
If you drop your Victoza pen, repeat “ First Time Use for Each New Pen ” (steps A through D).  Be careful not to bend or damage the needle.
Be careful not to bend or damage the needle.  Do not use the cartridge scale to measure how much Victoza to inject.
Do not use the cartridge scale to measure how much Victoza to inject.  Be careful when handling used needles to avoid needle stick injuries.
Be careful when handling used needles to avoid needle stick injuries.  You can use your Victoza pen for up to 30 days after you use it the first time.
You can use your Victoza pen for up to 30 days after you use it the first time. 