Get your patient on Darzalex Faspro (Daratumumab And Hyaluronidase-Fihj (Human Recombinant))
Darzalex Faspro prior authorization resources
Most recent state uniform prior authorization forms
Brand Resources
Darzalex Faspro patient education
Patient toolkit
Dosage & administration
DOSAGE AND ADMINISTRATION
For subcutaneous use only.
- Pre-medicate with a corticosteroid, acetaminophen and a histamine-1 receptor antagonist. (2.6 )
- The recommended dosage of DARZALEX FASPRO is (1,800 mg daratumumab and 30,000 units hyaluronidase) administered subcutaneously into the abdomen over approximately 3 to 5 minutes according to recommended schedule. (2.2 , 2.3 , 2.4 )
- Administer post-medications as recommended. (2.6 )
Important Dosing Information
- DARZALEX FASPRO is for subcutaneous use only.
- Administer medications before and after administration of DARZALEX FASPRO to minimize administration-related reactions [see Dosage and Administration (2.6) ] .
- Type and screen patients prior to starting DARZALEX FASPRO.
Recommended Dosage for Multiple Myeloma
The recommended dose of DARZALEX FASPRO is 1,800 mg/30,000 units (1,800 mg daratumumab and 30,000 units hyaluronidase) administered subcutaneously over approximately 3 to 5 minutes. Tables 1, 2, 3, 4, 5, and 6 provide the recommended dosing schedule when DARZALEX FASPRO is administered as monotherapy or as part of a combination therapy.
Monotherapy and In Combination with Lenalidomide and Dexamethasone (DARZALEX FASPRO-Rd), Pomalidomide and Dexamethasone (DARZALEX FASPRO-Pd) or Carfilzomib and Dexamethasone (DARZALEX FASPRO-Kd)
Use the dosing schedule provided in Table 1 when DARZALEX FASPRO is administered:
- in combination with lenalidomide and dexamethasone (4-week cycle) OR
- in combination with pomalidomide and dexamethasone (4-week cycle) OR
- in combination with carfilzomib and dexamethasone (4-week cycle) OR
- as monotherapy.
| Weeks | Schedule |
|---|---|
| Weeks 1 to 8 | weekly (total of 8 doses) |
| Weeks 9 to 24 First dose of the every-2-week dosing schedule is given at Week 9 | every two weeks (total of 8 doses) |
| Week 25 onwards until disease progression First dose of the every-4-week dosing schedule is given at Week 25 | every four weeks |
When DARZALEX FASPRO is administered as part of a combination therapy, see Clinical Studies (14.2) and the prescribing information for dosage recommendations for the other drugs.
In Combination with Bortezomib, Melphalan and Prednisone (DARZALEX FASPRO-VMP)
Use the dosing schedule provided in Table 2 when DARZALEX FASPRO is administered in combination with bortezomib, melphalan and prednisone (6-week cycle).
| Weeks | Schedule |
|---|---|
| Weeks 1 to 6 | weekly (total of 6 doses) |
| Weeks 7 to 54 First dose of the every-3-week dosing schedule is given at Week 7 | every three weeks (total of 16 doses) |
| Week 55 onwards until disease progression First dose of the every-4-week dosing schedule is given at Week 55 | every four weeks |
When DARZALEX FASPRO is administered as part of a combination therapy, see Clinical Studies (14.1) and the prescribing information for dosage recommendations for the other drugs.
In Combination with Bortezomib, Thalidomide, and Dexamethasone (DARZALEX FASPRO-VTd)
Use the dosing schedule in Table 3 when DARZALEX FASPRO is administered in combination with bortezomib, thalidomide, and dexamethasone (4-week cycle).
| Treatment phase | Weeks | Schedule |
|---|---|---|
| Induction | Weeks 1 to 8 | weekly (total of 8 doses) |
| Weeks 9 to 16 First dose of the every-2-week dosing schedule is given at Week 9 | every two weeks (total of 4 doses) | |
| Stop for high dose chemotherapy and ASCT | ||
| Consolidation | Weeks 1 to 8 First dose of the every-2-week dosing schedule is given at Week 1 upon re-initiation of treatment following ASCT | every two weeks (total of 4 doses) |
When DARZALEX FASPRO is administered as part of a combination therapy, see the prescribing information for dosage recommendations for the other drugs.
In Combination with Bortezomib, Lenalidomide, and Dexamethasone (DARZALEX FASPRO-VRd) for Patients Eligible for Autologous Stem Cell Transplant (ASCT)
Use the dosing schedule in Table 4 when DARZALEX FASPRO is administered in combination with bortezomib, lenalidomide, and dexamethasone (4-week cycle) for treatment of newly diagnosed multiple myeloma patients eligible for ASCT.
| Treatment phase | Weeks | Schedule |
|---|---|---|
| Induction | Weeks 1 to 8 | weekly (total of 8 doses) |
| Weeks 9 to 16 First dose of the every-2-week dosing schedule is given at Week 9 | every two weeks (total of 4 doses) | |
| Stop for high dose chemotherapy and ASCT | ||
| Consolidation | Weeks 1 to 8 First dose of the every-2-week dosing schedule is given at Week 1 upon re-initiation of treatment following ASCT | every two weeks (total of 4 doses) |
When DARZALEX FASPRO is administered as part of a combination therapy, see Clinical Studies (14.1) and the prescribing information for dosage recommendations for the other drugs.
In Combination with Bortezomib, Lenalidomide, and Dexamethasone (DARZALEX FASPRO-VRd) for Patients Who Are Ineligible for ASCT
Use the dosing schedule in Table 5 when DARZALEX FASPRO is administered in combination with bortezomib, lenalidomide, and dexamethasone (3-week cycle) for treatment of newly diagnosed multiple myeloma patients who are ineligible for ASCT.
| Weeks | Schedule |
|---|---|
| Weeks 1 to 6 | weekly (total of 6 doses) |
| Weeks 7 to 24 First dose of the every-3-week dosing schedule is given at Week 7 | every three weeks (total of 6 doses) |
| Week 25 onwards until disease progression First dose of the every-4-week dosing schedule is given at Week 25 | every four weeks |
When DARZALEX FASPRO is administered as part of a combination therapy, see Clinical Studies (14.1) and the prescribing information for dosage recommendations for the other drugs.
In Combination with Bortezomib and Dexamethasone (DARZALEX FASPRO-Vd)
Use the dosing schedule in Table 6 when DARZALEX FASPRO is administered in combination with bortezomib and dexamethasone (3-week cycle).
| Weeks | Schedule |
|---|---|
| Weeks 1 to 9 | weekly (total of 9 doses) |
| Weeks 10 to 24 First dose of the every-3-week dosing schedule is given at Week 10 | every three weeks (total of 5 doses) |
| Week 25 onwards until disease progression First dose of the every-4-week dosing schedule is given at Week 25 | every four weeks |
When DARZALEX FASPRO is administered as part of a combination therapy, see the prescribing information for dosage recommendations for the other drugs.
Recommended Dosage for High-Risk Smoldering Multiple Myeloma
The recommended dose of DARZALEX FASPRO is 1,800 mg/30,000 units (1,800 mg daratumumab and 30,000 units hyaluronidase) administered subcutaneously over approximately 3 to 5 minutes.
Use the dosing schedule provided in Table 7 when DARZALEX FASPRO is administered as monotherapy in high-risk smoldering multiple myeloma patients (4-week cycle).
| Weeks | Schedule |
|---|---|
| Weeks 1 to 8 | weekly (total of 8 doses) |
| Weeks 9 to 24 First dose of the every-2-week dosing schedule is given at Week 9 | every two weeks (total of 8 doses) |
| Week 25 onwards until diagnosis of multiple myeloma or a maximum of 3 years First dose of the every-4-week dosing schedule is given at Week 25 | every four weeks |
Recommended Dosage for Light Chain Amyloidosis
In Combination with Bortezomib, Cyclophosphamide and Dexamethasone (DARZALEX FASPRO-VCd)
The recommended dose of DARZALEX FASPRO is 1,800 mg/30,000 units (1,800 mg daratumumab and 30,000 units hyaluronidase) administered subcutaneously over approximately 3 to 5 minutes.
Use the dosing schedule provided in Table 8 when DARZALEX FASPRO is administered in combination with bortezomib, cyclophosphamide and dexamethasone (4-week cycle).
| Weeks | Schedule |
|---|---|
| Weeks 1 to 8 | weekly (total of 8 doses) |
| Weeks 9 to 24 First dose of the every-2-week dosing schedule is given at Week 9 | every two weeks (total of 8 doses) |
| Week 25 onwards until disease progression or a maximum of 2 years First dose of the every-4-week dosing schedule is given at Week 25 | every four weeks |
When DARZALEX FASPRO is administered as part of a combination therapy, see Clinical Studies (14.4) and the prescribing information for dosage recommendations for the other drugs.
Missed DARZALEX FASPRO Doses
If a dose of DARZALEX FASPRO is missed, administer the dose as soon as possible and adjust the dosing schedule to maintain the dosing interval.
Recommended Concomitant Medications
Pre-medication
Administer the following pre-medications 1 to 3 hours before each dose of DARZALEX FASPRO:
- Acetaminophen 650 mg to 1,000 mg orally
- Diphenhydramine 25 mg to 50 mg (or equivalent) orally or intravenously
- Corticosteroid (long- or intermediate-acting)
- Monotherapy
- Administer methylprednisolone 100 mg (or equivalent) orally or intravenously. Consider reducing the dose of methylprednisolone to 60 mg (or equivalent) following the second dose of DARZALEX FASPRO.
- In Combination
- Administer dexamethasone 20 mg (or equivalent) orally or intravenously prior to every DARZALEX FASPRO administration.
- When dexamethasone is the background regimen-specific corticosteroid, the dexamethasone dose that is part of the background regimen will serve as pre-medication on DARZALEX FASPRO administration days [see Clinical Studies (14) ] .
- Do not administer background regimen-specific corticosteroids (e.g., prednisone) on DARZALEX FASPRO administration days when patients have received dexamethasone (or equivalent) as a pre-medication.
Post-medication
Administer the following post-medications:
- Monotherapy
Administer methylprednisolone 20 mg (or an equivalent dose of an intermediate- or long-acting corticosteroid) orally for 2 days starting the day after the administration of DARZALEX FASPRO. - In Combination
Consider administering oral methylprednisolone at a dose of less than or equal to 20 mg (or an equivalent dose of an intermediate- or long-acting corticosteroid) on the day after administration of DARZALEX FASPRO.
If a background regimen-specific corticosteroid (e.g., dexamethasone, prednisone) is administered the day after the administration of DARZALEX FASPRO, additional corticosteroids may not be needed [see Clinical Studies (14) ] .
If the patient does not experience a major systemic administration-related reaction after the first 3 doses of DARZALEX FASPRO, consider discontinuing the administration of corticosteroids (excluding any background regimen-specific corticosteroid).
For patients with a history of chronic obstructive pulmonary disease, consider prescribing short and long-acting bronchodilators and inhaled corticosteroids. Following the first 4 doses of DARZALEX FASPRO, consider discontinuing these additional post-medications, if the patient does not experience a major systemic administration-related reaction.
Prophylaxis for Herpes Zoster Reactivation
Initiate antiviral prophylaxis to prevent herpes zoster reactivation within 1 week after starting DARZALEX FASPRO and continue for 3 months following the end of treatment [see Adverse Reactions (6.1) ].
Dosage Modifications for Adverse Reactions
No dose reductions of DARZALEX FASPRO are recommended. Consider withholding DARZALEX FASPRO to allow recovery of blood cell counts in the event of myelosuppression [see Warnings and Precautions (5.4 , 5.5) ] .
Preparation and Administration
DARZALEX FASPRO should be administered by a healthcare provider.
To prevent medication errors, check the vial labels to ensure that the drug being prepared and administered is DARZALEX FASPRO for subcutaneous use. Do not administer DARZALEX FASPRO intravenously .
DARZALEX FASPRO is ready to use.
Preparation
- Remove the DARZALEX FASPRO vial from refrigerated storage [2°C to 8°C (36°F to 46°F)] and equilibrate to ambient temperature [15°C to 30°C (59°F to 86°F)]. Store the unpunctured vial at ambient temperature and ambient light for a maximum of 24 hours. Keep out of direct sunlight. Do not shake.
- Withdraw 15 mL from the vial into a syringe using an 18G to 22G transfer needle with a regular bevel. Insert the needle into the vial at a 90° angle within the ring of the stopper.
- Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. Do not use if opaque particles, discoloration or other foreign particles are present.
- DARZALEX FASPRO is compatible with polypropylene or polyethylene syringe material; polypropylene, polyethylene, or polyvinyl chloride (PVC) subcutaneous infusion sets; and stainless steel transfer and injection needles. Use the product immediately.
- After the solution of DARZALEX FASPRO is withdrawn into the syringe, replace the transfer needle with a syringe closing cap. Label the syringe appropriately to include the route of administration per institutional standards. Label the syringe with the peel-off label.
- To avoid needle clogging, attach the hypodermic injection needle or subcutaneous infusion set to the syringe immediately prior to injection.
Storage
- If the syringe containing DARZALEX FASPRO is not used immediately, store refrigerated at 2°C to 8°C (36°F to 46°F) for up to 24 hours and/or at room temperature at 15°C to 25°C (59°F to 77°F) for up to 12 hours under ambient light.
- Discard if storage time exceeds these limits.
- If stored in the refrigerator, allow the solution to come to room temperature before administration.
Administration
- Inject 15 mL of DARZALEX FASPRO into the subcutaneous tissue of the abdomen approximately 3 inches [7.5 cm] to the right or left of the navel over approximately 3 to 5 minutes. No data are available on performing the injection at other sites of the body.
- Rotate injection sites for successive injections.
- Never inject DARZALEX FASPRO into areas where the skin is red, bruised, tender, hard or areas where there are scars.
- Pause or slow down delivery rate if the patient experiences pain. In the event pain is not alleviated by pausing or slowing down delivery rate, a second injection site may be chosen on the opposite side of the abdomen to deliver the remainder of the dose.
- During treatment with DARZALEX FASPRO, do not administer other medications for subcutaneous use at the same site as DARZALEX FASPRO.

By using PrescriberAI, you agree to the AI Terms of Use.
Darzalex Faspro prescribing information
INDICATIONS AND USAGE
DARZALEX FASPRO is a combination of daratumumab, a CD38-directed cytolytic antibody, and hyaluronidase, an endoglycosidase, indicated for the treatment of adult patients with:
- multiple myeloma in combination with bortezomib, lenalidomide, and dexamethasone for induction and consolidation in newly diagnosed patients who are eligible for autologous stem cell transplant
- multiple myeloma in combination with bortezomib, lenalidomide, and dexamethasone in newly diagnosed patients who are ineligible for autologous stem cell transplant
- multiple myeloma in combination with bortezomib, melphalan and prednisone in newly diagnosed patients who are ineligible for autologous stem cell transplant
- multiple myeloma in combination with lenalidomide and dexamethasone in newly diagnosed patients who are ineligible for autologous stem cell transplant and in patients with relapsed or refractory multiple myeloma who have received at least one prior therapy
- multiple myeloma in combination with bortezomib, thalidomide, and dexamethasone in newly diagnosed patients who are eligible for autologous stem cell transplant
- multiple myeloma in combination with bortezomib and dexamethasone in patients who have received at least one prior therapy
- multiple myeloma in combination with pomalidomide and dexamethasone in patients who have received at least one prior line of therapy including lenalidomide and a proteasome inhibitor
- multiple myeloma in combination with carfilzomib and dexamethasone in patients with relapsed or refractory multiple myeloma who have received one to three prior lines of therapy
- multiple myeloma as monotherapy, in patients who have received at least three prior lines of therapy including a proteasome inhibitor (PI) and an immunomodulatory agent or who are double-refractory to a PI and an immunomodulatory agent
- high-risk smoldering multiple myeloma as monotherapy
- light chain (AL) amyloidosis in combination with bortezomib, cyclophosphamide and dexamethasone in newly diagnosed patients.
Limitations of Use:
- DARZALEX FASPRO is not indicated and is not recommended for the treatment of patients with light chain (AL) amyloidosis who have NYHA Class IIIB or Class IV cardiac disease or Mayo Stage IIIB outside of controlled clinical trials (1.3 )
Multiple Myeloma
DARZALEX FASPRO is indicated for the treatment of adult patients with [see Clinical Studies (14) ] :
- multiple myeloma in combination with bortezomib, lenalidomide, and dexamethasone for induction and consolidation in newly diagnosed patients who are eligible for autologous stem cell transplant.
- multiple myeloma in combination with bortezomib, lenalidomide, and dexamethasone in newly diagnosed patients who are ineligible for autologous stem cell transplant.
- multiple myeloma in combination with bortezomib, melphalan and prednisone in newly diagnosed patients who are ineligible for autologous stem cell transplant.
- multiple myeloma in combination with lenalidomide and dexamethasone in newly diagnosed patients who are ineligible for autologous stem cell transplant and in patients with relapsed or refractory multiple myeloma who have received at least one prior therapy.
- multiple myeloma in combination with bortezomib, thalidomide, and dexamethasone in newly diagnosed patients who are eligible for autologous stem cell transplant.
- multiple myeloma in combination with bortezomib and dexamethasone in patients who have received at least one prior therapy.
- multiple myeloma in combination with pomalidomide and dexamethasone in patients who have received at least one prior line of therapy including lenalidomide and a proteasome inhibitor.
- multiple myeloma in combination with carfilzomib and dexamethasone in patients with relapsed or refractory multiple myeloma who have received one to three prior lines of therapy.
- multiple myeloma as monotherapy, in patients who have received at least three prior lines of therapy including a proteasome inhibitor (PI) and an immunomodulatory agent or who are double-refractory to a PI and an immunomodulatory agent.
High-Risk Smoldering Multiple Myeloma
DARZALEX FASPRO as monotherapy is indicated for the treatment of adult patients with high-risk smoldering multiple myeloma.
Light Chain Amyloidosis
DARZALEX FASPRO in combination with bortezomib, cyclophosphamide and dexamethasone is indicated for the treatment of adult patients with newly diagnosed light chain (AL) amyloidosis.
Limitations of Use
DARZALEX FASPRO is not indicated and is not recommended for the treatment of patients with light chain (AL) amyloidosis who have NYHA Class IIIB or Class IV cardiac disease or Mayo Stage IIIB outside of controlled clinical trials [see Warnings and Precautions (5.2) ] .
DOSAGE AND ADMINISTRATION
For subcutaneous use only.
- Pre-medicate with a corticosteroid, acetaminophen and a histamine-1 receptor antagonist. (2.6 )
- The recommended dosage of DARZALEX FASPRO is (1,800 mg daratumumab and 30,000 units hyaluronidase) administered subcutaneously into the abdomen over approximately 3 to 5 minutes according to recommended schedule. (2.2 , 2.3 , 2.4 )
- Administer post-medications as recommended. (2.6 )
Important Dosing Information
- DARZALEX FASPRO is for subcutaneous use only.
- Administer medications before and after administration of DARZALEX FASPRO to minimize administration-related reactions [see Dosage and Administration (2.6) ] .
- Type and screen patients prior to starting DARZALEX FASPRO.
Recommended Dosage for Multiple Myeloma
The recommended dose of DARZALEX FASPRO is 1,800 mg/30,000 units (1,800 mg daratumumab and 30,000 units hyaluronidase) administered subcutaneously over approximately 3 to 5 minutes. Tables 1, 2, 3, 4, 5, and 6 provide the recommended dosing schedule when DARZALEX FASPRO is administered as monotherapy or as part of a combination therapy.
Monotherapy and In Combination with Lenalidomide and Dexamethasone (DARZALEX FASPRO-Rd), Pomalidomide and Dexamethasone (DARZALEX FASPRO-Pd) or Carfilzomib and Dexamethasone (DARZALEX FASPRO-Kd)
Use the dosing schedule provided in Table 1 when DARZALEX FASPRO is administered:
- in combination with lenalidomide and dexamethasone (4-week cycle) OR
- in combination with pomalidomide and dexamethasone (4-week cycle) OR
- in combination with carfilzomib and dexamethasone (4-week cycle) OR
- as monotherapy.
| Weeks | Schedule |
|---|---|
| Weeks 1 to 8 | weekly (total of 8 doses) |
| Weeks 9 to 24 First dose of the every-2-week dosing schedule is given at Week 9 | every two weeks (total of 8 doses) |
| Week 25 onwards until disease progression First dose of the every-4-week dosing schedule is given at Week 25 | every four weeks |
When DARZALEX FASPRO is administered as part of a combination therapy, see Clinical Studies (14.2) and the prescribing information for dosage recommendations for the other drugs.
In Combination with Bortezomib, Melphalan and Prednisone (DARZALEX FASPRO-VMP)
Use the dosing schedule provided in Table 2 when DARZALEX FASPRO is administered in combination with bortezomib, melphalan and prednisone (6-week cycle).
| Weeks | Schedule |
|---|---|
| Weeks 1 to 6 | weekly (total of 6 doses) |
| Weeks 7 to 54 First dose of the every-3-week dosing schedule is given at Week 7 | every three weeks (total of 16 doses) |
| Week 55 onwards until disease progression First dose of the every-4-week dosing schedule is given at Week 55 | every four weeks |
When DARZALEX FASPRO is administered as part of a combination therapy, see Clinical Studies (14.1) and the prescribing information for dosage recommendations for the other drugs.
In Combination with Bortezomib, Thalidomide, and Dexamethasone (DARZALEX FASPRO-VTd)
Use the dosing schedule in Table 3 when DARZALEX FASPRO is administered in combination with bortezomib, thalidomide, and dexamethasone (4-week cycle).
| Treatment phase | Weeks | Schedule |
|---|---|---|
| Induction | Weeks 1 to 8 | weekly (total of 8 doses) |
| Weeks 9 to 16 First dose of the every-2-week dosing schedule is given at Week 9 | every two weeks (total of 4 doses) | |
| Stop for high dose chemotherapy and ASCT | ||
| Consolidation | Weeks 1 to 8 First dose of the every-2-week dosing schedule is given at Week 1 upon re-initiation of treatment following ASCT | every two weeks (total of 4 doses) |
When DARZALEX FASPRO is administered as part of a combination therapy, see the prescribing information for dosage recommendations for the other drugs.
In Combination with Bortezomib, Lenalidomide, and Dexamethasone (DARZALEX FASPRO-VRd) for Patients Eligible for Autologous Stem Cell Transplant (ASCT)
Use the dosing schedule in Table 4 when DARZALEX FASPRO is administered in combination with bortezomib, lenalidomide, and dexamethasone (4-week cycle) for treatment of newly diagnosed multiple myeloma patients eligible for ASCT.
| Treatment phase | Weeks | Schedule |
|---|---|---|
| Induction | Weeks 1 to 8 | weekly (total of 8 doses) |
| Weeks 9 to 16 First dose of the every-2-week dosing schedule is given at Week 9 | every two weeks (total of 4 doses) | |
| Stop for high dose chemotherapy and ASCT | ||
| Consolidation | Weeks 1 to 8 First dose of the every-2-week dosing schedule is given at Week 1 upon re-initiation of treatment following ASCT | every two weeks (total of 4 doses) |
When DARZALEX FASPRO is administered as part of a combination therapy, see Clinical Studies (14.1) and the prescribing information for dosage recommendations for the other drugs.
In Combination with Bortezomib, Lenalidomide, and Dexamethasone (DARZALEX FASPRO-VRd) for Patients Who Are Ineligible for ASCT
Use the dosing schedule in Table 5 when DARZALEX FASPRO is administered in combination with bortezomib, lenalidomide, and dexamethasone (3-week cycle) for treatment of newly diagnosed multiple myeloma patients who are ineligible for ASCT.
| Weeks | Schedule |
|---|---|
| Weeks 1 to 6 | weekly (total of 6 doses) |
| Weeks 7 to 24 First dose of the every-3-week dosing schedule is given at Week 7 | every three weeks (total of 6 doses) |
| Week 25 onwards until disease progression First dose of the every-4-week dosing schedule is given at Week 25 | every four weeks |
When DARZALEX FASPRO is administered as part of a combination therapy, see Clinical Studies (14.1) and the prescribing information for dosage recommendations for the other drugs.
In Combination with Bortezomib and Dexamethasone (DARZALEX FASPRO-Vd)
Use the dosing schedule in Table 6 when DARZALEX FASPRO is administered in combination with bortezomib and dexamethasone (3-week cycle).
| Weeks | Schedule |
|---|---|
| Weeks 1 to 9 | weekly (total of 9 doses) |
| Weeks 10 to 24 First dose of the every-3-week dosing schedule is given at Week 10 | every three weeks (total of 5 doses) |
| Week 25 onwards until disease progression First dose of the every-4-week dosing schedule is given at Week 25 | every four weeks |
When DARZALEX FASPRO is administered as part of a combination therapy, see the prescribing information for dosage recommendations for the other drugs.
Recommended Dosage for High-Risk Smoldering Multiple Myeloma
The recommended dose of DARZALEX FASPRO is 1,800 mg/30,000 units (1,800 mg daratumumab and 30,000 units hyaluronidase) administered subcutaneously over approximately 3 to 5 minutes.
Use the dosing schedule provided in Table 7 when DARZALEX FASPRO is administered as monotherapy in high-risk smoldering multiple myeloma patients (4-week cycle).
| Weeks | Schedule |
|---|---|
| Weeks 1 to 8 | weekly (total of 8 doses) |
| Weeks 9 to 24 First dose of the every-2-week dosing schedule is given at Week 9 | every two weeks (total of 8 doses) |
| Week 25 onwards until diagnosis of multiple myeloma or a maximum of 3 years First dose of the every-4-week dosing schedule is given at Week 25 | every four weeks |
Recommended Dosage for Light Chain Amyloidosis
In Combination with Bortezomib, Cyclophosphamide and Dexamethasone (DARZALEX FASPRO-VCd)
The recommended dose of DARZALEX FASPRO is 1,800 mg/30,000 units (1,800 mg daratumumab and 30,000 units hyaluronidase) administered subcutaneously over approximately 3 to 5 minutes.
Use the dosing schedule provided in Table 8 when DARZALEX FASPRO is administered in combination with bortezomib, cyclophosphamide and dexamethasone (4-week cycle).
| Weeks | Schedule |
|---|---|
| Weeks 1 to 8 | weekly (total of 8 doses) |
| Weeks 9 to 24 First dose of the every-2-week dosing schedule is given at Week 9 | every two weeks (total of 8 doses) |
| Week 25 onwards until disease progression or a maximum of 2 years First dose of the every-4-week dosing schedule is given at Week 25 | every four weeks |
When DARZALEX FASPRO is administered as part of a combination therapy, see Clinical Studies (14.4) and the prescribing information for dosage recommendations for the other drugs.
Missed DARZALEX FASPRO Doses
If a dose of DARZALEX FASPRO is missed, administer the dose as soon as possible and adjust the dosing schedule to maintain the dosing interval.
Recommended Concomitant Medications
Pre-medication
Administer the following pre-medications 1 to 3 hours before each dose of DARZALEX FASPRO:
- Acetaminophen 650 mg to 1,000 mg orally
- Diphenhydramine 25 mg to 50 mg (or equivalent) orally or intravenously
- Corticosteroid (long- or intermediate-acting)
- Monotherapy
- Administer methylprednisolone 100 mg (or equivalent) orally or intravenously. Consider reducing the dose of methylprednisolone to 60 mg (or equivalent) following the second dose of DARZALEX FASPRO.
- In Combination
- Administer dexamethasone 20 mg (or equivalent) orally or intravenously prior to every DARZALEX FASPRO administration.
- When dexamethasone is the background regimen-specific corticosteroid, the dexamethasone dose that is part of the background regimen will serve as pre-medication on DARZALEX FASPRO administration days [see Clinical Studies (14) ] .
- Do not administer background regimen-specific corticosteroids (e.g., prednisone) on DARZALEX FASPRO administration days when patients have received dexamethasone (or equivalent) as a pre-medication.
Post-medication
Administer the following post-medications:
- Monotherapy Administer methylprednisolone 20 mg (or an equivalent dose of an intermediate- or long-acting corticosteroid) orally for 2 days starting the day after the administration of DARZALEX FASPRO.
- In Combination Consider administering oral methylprednisolone at a dose of less than or equal to 20 mg (or an equivalent dose of an intermediate- or long-acting corticosteroid) on the day after administration of DARZALEX FASPRO. If a background regimen-specific corticosteroid (e.g., dexamethasone, prednisone) is administered the day after the administration of DARZALEX FASPRO, additional corticosteroids may not be needed [see Clinical Studies (14) ] .
If the patient does not experience a major systemic administration-related reaction after the first 3 doses of DARZALEX FASPRO, consider discontinuing the administration of corticosteroids (excluding any background regimen-specific corticosteroid).
For patients with a history of chronic obstructive pulmonary disease, consider prescribing short and long-acting bronchodilators and inhaled corticosteroids. Following the first 4 doses of DARZALEX FASPRO, consider discontinuing these additional post-medications, if the patient does not experience a major systemic administration-related reaction.
Prophylaxis for Herpes Zoster Reactivation
Initiate antiviral prophylaxis to prevent herpes zoster reactivation within 1 week after starting DARZALEX FASPRO and continue for 3 months following the end of treatment [see Adverse Reactions (6.1) ].
Dosage Modifications for Adverse Reactions
No dose reductions of DARZALEX FASPRO are recommended. Consider withholding DARZALEX FASPRO to allow recovery of blood cell counts in the event of myelosuppression [see Warnings and Precautions (5.4 , 5.5) ] .
Preparation and Administration
DARZALEX FASPRO should be administered by a healthcare provider.
To prevent medication errors, check the vial labels to ensure that the drug being prepared and administered is DARZALEX FASPRO for subcutaneous use. Do not administer DARZALEX FASPRO intravenously .
DARZALEX FASPRO is ready to use.
Preparation
- Remove the DARZALEX FASPRO vial from refrigerated storage [2°C to 8°C (36°F to 46°F)] and equilibrate to ambient temperature [15°C to 30°C (59°F to 86°F)]. Store the unpunctured vial at ambient temperature and ambient light for a maximum of 24 hours. Keep out of direct sunlight. Do not shake.
- Withdraw 15 mL from the vial into a syringe using an 18G to 22G transfer needle with a regular bevel. Insert the needle into the vial at a 90° angle within the ring of the stopper.
- Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. Do not use if opaque particles, discoloration or other foreign particles are present.
- DARZALEX FASPRO is compatible with polypropylene or polyethylene syringe material; polypropylene, polyethylene, or polyvinyl chloride (PVC) subcutaneous infusion sets; and stainless steel transfer and injection needles. Use the product immediately.
- After the solution of DARZALEX FASPRO is withdrawn into the syringe, replace the transfer needle with a syringe closing cap. Label the syringe appropriately to include the route of administration per institutional standards. Label the syringe with the peel-off label.
- To avoid needle clogging, attach the hypodermic injection needle or subcutaneous infusion set to the syringe immediately prior to injection.
Storage
- If the syringe containing DARZALEX FASPRO is not used immediately, store refrigerated at 2°C to 8°C (36°F to 46°F) for up to 24 hours and/or at room temperature at 15°C to 25°C (59°F to 77°F) for up to 12 hours under ambient light.
- Discard if storage time exceeds these limits.
- If stored in the refrigerator, allow the solution to come to room temperature before administration.
Administration
- Inject 15 mL of DARZALEX FASPRO into the subcutaneous tissue of the abdomen approximately 3 inches [7.5 cm] to the right or left of the navel over approximately 3 to 5 minutes. No data are available on performing the injection at other sites of the body.
- Rotate injection sites for successive injections.
- Never inject DARZALEX FASPRO into areas where the skin is red, bruised, tender, hard or areas where there are scars.
- Pause or slow down delivery rate if the patient experiences pain. In the event pain is not alleviated by pausing or slowing down delivery rate, a second injection site may be chosen on the opposite side of the abdomen to deliver the remainder of the dose.
- During treatment with DARZALEX FASPRO, do not administer other medications for subcutaneous use at the same site as DARZALEX FASPRO.
DOSAGE FORMS AND STRENGTHS
Injection: 1,800 mg daratumumab and 30,000 units hyaluronidase per 15 mL (120 mg and 2,000 units/mL) colorless to yellow and clear to opalescent solution in a single-dose vial.
USE IN SPECIFIC POPULATIONS
Pregnancy
Risk Summary
DARZALEX FASPRO can cause fetal harm when administered to a pregnant woman. The assessment of associated risks with daratumumab products is based on the mechanism of action and data from target antigen CD38 knockout animal models (see Data ) . There are no available data on the use of DARZALEX FASPRO in pregnant women to evaluate drug-associated risk of major birth defects, miscarriage or adverse maternal or fetal outcomes. Animal reproduction studies have not been conducted.
In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
The combination of DARZALEX FASPRO and lenalidomide, thalidomide or pomalidomide is contraindicated in pregnant women, because lenalidomide, thalidomide and pomalidomide may cause birth defects and death of the unborn child. Lenalidomide, thalidomide and pomalidomide are only available through a REMS program. Refer to the lenalidomide, thalidomide or pomalidomide prescribing information on use during pregnancy.
Clinical Considerations
Fetal/Neonatal Adverse Reactions
Immunoglobulin G1 (IgG1) monoclonal antibodies are transferred across the placenta. Based on its mechanism of action, DARZALEX FASPRO may cause depletion of fetal CD38 positive immune cells and decreased bone density. Defer administering live vaccines to neonates and infants exposed to daratumumab in utero until a hematology evaluation is completed.
Data
Animal Data
DARZALEX FASPRO for subcutaneous injection contains daratumumab and hyaluronidase . Mice that were genetically modified to eliminate all CD38 expression (CD38 knockout mice) had reduced bone density at birth that recovered by 5 months of age. Data from studies using CD38 knockout animal models also suggest the involvement of CD38 in the regulation of humoral immune responses (mice), feto-maternal immune tolerance (mice), and early embryonic development (frogs).
No systemic exposure of hyaluronidase was detected in monkeys given 220,000 U/kg subcutaneously (440 times higher than the human dose) and there were no effects on embryo-fetal development in pregnant mice given 360,000 U/kg hyaluronidase subcutaneously daily during organogenesis, which is 720 times higher than the human dose.
There were no effects on pre- and post-natal development through sexual maturity in offspring of mice treated daily from implantation through lactation with 1,100,000 U/kg hyaluronidase subcutaneously, which is 2,200 times higher than the human doses.
Lactation
Risk Summary
There is no data on the presence of daratumumab and hyaluronidase in human milk, the effects on the breastfed child, or the effects on milk production. Maternal immunoglobulin G is known to be present in human milk. Published data suggest that antibodies in breast milk do not enter the neonatal and infant circulations in substantial amounts. Because of the potential for serious adverse reactions in the breastfed child when DARZALEX FASPRO is administered with lenalidomide, thalidomide or pomalidomide, advise women not to breastfeed during treatment with DARZALEX FASPRO. Refer to lenalidomide, thalidomide or pomalidomide prescribing information for additional information.
Data
Animal Data
No systemic exposure of hyaluronidase was detected in monkeys given 220,000 U/kg subcutaneously (440 times higher than the human dose) and there were no effects on post-natal development through sexual maturity in offspring of mice treated daily during lactation with 1,100,000 U/kg hyaluronidase subcutaneously, which is 2,200 times higher than the human doses.
Females and Males of Reproductive Potential
DARZALEX FASPRO can cause fetal harm when administered to a pregnant woman [see Use in Specific Populations (8.1) ] .
Pregnancy Testing
With the combination of DARZALEX FASPRO with lenalidomide, thalidomide or pomalidomide, refer to the lenalidomide, thalidomide or pomalidomide labeling for pregnancy testing requirements prior to initiating treatment in females of reproductive potential.
Contraception
Advise females of reproductive potential to use effective contraception during treatment with DARZALEX FASPRO and for 3 months after the last dose. Additionally, refer to the lenalidomide, thalidomide or pomalidomide labeling for additional recommendations for contraception.
Pediatric Use
Safety and effectiveness of DARZALEX FASPRO in pediatric patients have not been established.
Geriatric Use
Of the 291 patients who received DARZALEX FASPRO as monotherapy for relapsed and refractory multiple myeloma, 37% were 65 to <75 years of age, and 19% were 75 years of age and older. No overall differences in effectiveness of DARZALEX FASPRO have been observed between patients ≥65 years of age and younger patients . Adverse reactions that occurred at a higher frequency (≥5% difference) in patients ≥65 years of age included upper respiratory tract infection, urinary tract infection, dizziness, cough, dyspnea, diarrhea, nausea, fatigue, and peripheral edema. Serious adverse reactions that occurred at a higher frequency (≥2% difference) in patients ≥65 years of age included pneumonia.
Of the 214 patients who received DARZALEX FASPRO as combination therapy with pomalidomide and dexamethasone or DARZALEX FASPRO as combination therapy with lenalidomide and low-dose dexamethasone for relapsed and refractory multiple myeloma, 43% were 65 to <75 years of age, and 18% were 75 years of age and older. No overall differences in effectiveness were observed between patients ≥65 years (n=131) and <65 years (n=85). Adverse reactions occurring at a higher frequency (≥5% difference) in patients ≥65 years of age included fatigue, pyrexia, peripheral edema, urinary tract infection, diarrhea, constipation, vomiting, dyspnea, cough, and hyperglycemia. Serious adverse reactions occurring at a higher frequency (≥2% difference) in patients ≥65 years of age included neutropenia, thrombocytopenia, diarrhea, anemia, COVID-19, ischemic colitis, deep vein thrombosis, general physical health deterioration, pulmonary embolism, and urinary tract infection.
Of the 355 patients who were newly diagnosed with multiple myeloma and eligible for ASCT who received DARZALEX FASPRO as combination therapy with bortezomib, lenalidomide and dexamethasone during induction and consolidation in the clinical trial, 74% were <65 years of age, and 26% were 65 to 70 years of age. The clinical trial did not enroll patients older than 70 years of age [see Clinical Studies (14.1) ] . No overall differences in effectiveness of DARZALEX FASPRO in combination with bortezomib, lenalidomide and dexamethasone were observed between patients <65 years of age compared to patients 65 to 70 years of age. Adverse reactions that occurred at a higher frequency (≥5% difference) in patients 65 to 70 years of age included constipation, hemorrhoids, nausea, injection site erythema, bronchitis, nasopharyngitis, back pain, myalgia, pain in extremity, dysgeusia, peripheral motor neuropathy, and insomnia. Serious adverse reactions that occurred at a higher frequency (≥2% difference) in patients 65 to 70 years of age included febrile bone marrow aplasia, atrial fibrillation, pyrexia, and orthostatic hypotension.
Of the 197 patients with newly diagnosed multiple myeloma in CEPHEUS who received DARZALEX FASPRO as combination therapy with bortezomib, lenalidomide and dexamethasone, 61% were 65 to <75 years of age, and 21% were 75 years of age and older. The clinical trial did not enroll patients over age 80 [see Clinical Studies (14.1) ] . No overall differences in effectiveness of DARZALEX FASPRO in combination with bortezomib, lenalidomide and dexamethasone were observed between younger patients and patients ≥75 years. Adverse reactions occurring at a higher frequency (≥5% difference) in patients ≥75 years of age included sensory neuropathy, diarrhea, fatigue, constipation, renal impairment, dizziness, pyrexia, rash, dyspnea, fracture, arrhythmia, decreased appetite, urinary tract infection, injection site reaction, encephalopathy, vomiting, taste disorder, and herpes. Serious adverse reactions occurring at a higher frequency (≥5% difference) in patients ≥75 years of age included urinary tract infection, upper respiratory tract infection, diarrhea, and encephalopathy.
Of the 193 patients who received DARZALEX FASPRO as monotherapy for high-risk smoldering multiple myeloma, 35% (n=67) were 65 to <75 years of age, and 11% (n=21) were 75 years of age and older. No overall difference in effectiveness were observed between patients 65 to 75 years (n=67) and <65 years (n=105); there were too few patients 75 years of age and older to assess for a difference in effectiveness. Adverse reactions that occurred at a higher frequency (≥5% difference) in patients ≥65 years of age were pneumonia, dizziness, arrhythmia, hemorrhage, arthritis, and cataract. Serious adverse reactions occurring at a higher frequency (≥5% difference) in patients ≥65 years of age included pneumonia and fracture.
Of the 193 patients who received DARZALEX FASPRO as part of a combination therapy for light chain (AL) amyloidosis, 35% were 65 to <75 years of age, and 10% were 75 years of age and older. Clinical studies of DARZALEX FASPRO as part of a combination therapy for patients with light chain (AL) amyloidosis did not include sufficient numbers of patients aged 65 and older to determine whether effectiveness differs from that of younger patients. Adverse reactions that occurred at a higher frequency in patients ≥65 years of age were peripheral edema, asthenia, pneumonia and hypotension.
No clinically meaningful differences in the pharmacokinetics of daratumumab were observed in geriatric patients compared to younger adult patients [see Clinical Pharmacology (12.3) ] .
CONTRAINDICATIONS
DARZALEX FASPRO is contraindicated in patients with a history of severe hypersensitivity to daratumumab, hyaluronidase or any of the components of the formulation [see Warnings and Precautions (5.1) and Adverse Reactions (6.2) ].
WARNINGS AND PRECAUTIONS
- Hypersensitivity and Other Administration Reactions : Permanently discontinue DARZALEX FASPRO for life-threatening reactions. (5.1 )
- Cardiac Toxicity in Patients with Light Chain (AL) Amyloidosis : Monitor patients with cardiac involvement more frequently for cardiac adverse reactions and administer supportive care as appropriate. (5.2 )
- Infections : DARZALEX FASPRO can cause serious and fatal infections. Monitor patients for signs and symptoms of infection and treat appropriately. (5.3 )
- Neutropenia : Monitor complete blood cell counts periodically during treatment. Monitor patients with neutropenia for signs of infection. Consider withholding DARZALEX FASPRO to allow recovery of neutrophils. (5.4 )
- Thrombocytopenia : Monitor complete blood cell counts periodically during treatment. Consider withholding DARZALEX FASPRO to allow recovery of platelets. (5.5 )
- Embryo-Fetal Toxicity : Can cause fetal harm. Advise pregnant women of the potential risk to a fetus and advise females of reproductive potential to use effective contraception. (5.6 , 8.1 , 8.3 )
- Interference with cross-matching and red blood cell antibody screening : Type and screen patients prior to starting treatment. Inform blood banks that a patient has received DARZALEX FASPRO. (5.7 , 7.1 )
Hypersensitivity and Other Administration Reactions
Both systemic administration-related reactions, including severe or life-threatening reactions, and local injection-site reactions can occur with DARZALEX FASPRO. Fatal reactions have been reported with daratumumab-containing products, including DARZALEX FASPRO [see Adverse Reactions (6.2) ] .
Systemic Reactions
In a pooled safety population of 1446 patients with multiple myeloma (N=1253) or light chain (AL) amyloidosis (N=193) who received DARZALEX FASPRO as monotherapy or as part of a combination therapy, 7% of patients experienced a systemic administration-related reaction (Grade 2: 3%, Grade 3: 0.8%, Grade 4: 0.1%). In patients with high-risk smoldering multiple myeloma (N=193), systemic administration-related reactions occurred in 17% of patients in AQUILA (Grade 2: 7%, Grade 3: 1%).
In all patients (N=1639), systemic administration-related reactions occurred in 7% of patients with the first injection, 0.5% with the second injection, and cumulatively 1% with subsequent injections. The median time to onset was 3.2 hours (range: 4 minutes to 3.5 days). Of the 283 systemic administration-related reactions that occurred in 135 patients, 240 (85%) occurred on the day of DARZALEX FASPRO administration. Delayed systemic administration-related reactions have occurred in 1% of the patients.
Severe reactions include hypoxia, dyspnea, hypertension, and tachycardia, and ocular adverse reactions, including choroidal effusion, acute myopia, and acute angle closure glaucoma. Other signs and symptoms of systemic administration-related reactions may include respiratory symptoms, such as bronchospasm, nasal congestion, cough, throat irritation, allergic rhinitis, and wheezing, as well as anaphylactic reaction, pyrexia, chest pain, pruritus, chills, vomiting, nausea, hypotension, and blurred vision.
Pre-medicate patients with histamine-1 receptor antagonist, acetaminophen and corticosteroids [see Dosage and Administration (2.6) ] . Monitor patients for systemic administration-related reactions, especially following the first and second injections. For anaphylactic reaction or life-threatening (Grade 4) administration-related reactions, immediately and permanently discontinue DARZALEX FASPRO. Consider administering corticosteroids and other medications after the administration of DARZALEX FASPRO depending on dosing regimen and medical history to minimize the risk of delayed (defined as occurring the day after administration) systemic administration-related reactions [see Dosage and Administration (2.6) ] .
Ocular adverse reactions, including acute myopia and narrowing of the anterior chamber angle due to ciliochoroidal effusions with potential for increased intraocular pressure or glaucoma, have occurred with daratumumab-containing products. If ocular symptoms occur, interrupt DARZALEX FASPRO and seek immediate ophthalmologic evaluation prior to restarting DARZALEX FASPRO.
Local Reactions
In this pooled safety population of 1446 patients with multiple myeloma (N=1253) or light chain (AL) amyloidosis (N=193), injection-site reactions occurred in 8% of patients, including Grade 2 reactions in 1.1%. The most frequent (>1%) injection-site reactions were injection site erythema and injection site rash. In patients with high-risk smoldering multiple myeloma (N=193), injection-site reactions occurred in 28% of patients, including Grade 2 reactions in 3%. These local reactions occurred a median of 6 minutes (range: 0 minutes to 6.5 days) after starting administration of DARZALEX FASPRO. Monitor for local reactions and consider symptomatic management.
Cardiac Toxicity in Patients with Light Chain (AL) Amyloidosis
Serious or fatal cardiac adverse reactions occurred in patients with light chain (AL) amyloidosis who received DARZALEX FASPRO in combination with bortezomib, cyclophosphamide and dexamethasone [see Adverse Reactions (6.1) ] . Serious cardiac disorders occurred in 16% and fatal cardiac disorders occurred in 10% of patients. Patients with NYHA Class IIIA or Mayo Stage IIIA disease may be at greater risk. Patients with NYHA Class IIIB or IV disease were not studied.
Monitor patients with cardiac involvement of light chain (AL) amyloidosis more frequently for cardiac adverse reactions and administer supportive care as appropriate.
Infections
DARZALEX FASPRO can cause serious, life-threatening, or fatal infections. In patients who received DARZALEX FASPRO in a pooled safety population including patients with smoldering multiple myeloma and light chain (AL) amyloidosis (N=1639), serious infections, including opportunistic infections, occurred in 24% of patients, Grade 3 or 4 infections occurred in 22%, and fatal infections occurred in 2.5%. The most common type of serious infection reported was pneumonia (8.5%).
Monitor patients for signs and symptoms of infection prior to and during treatment with DARZALEX FASPRO and treat appropriately. Administer prophylactic antimicrobials according to guidelines [see Dosage and Administration (2.6) ] .
Neutropenia
Daratumumab may increase neutropenia induced by background therapy [see Adverse Reactions (6.1) ] .
Monitor complete blood cell counts periodically during treatment according to manufacturer's prescribing information for background therapies. Monitor patients with neutropenia for signs of infection. Consider withholding DARZALEX FASPRO until recovery of neutrophils. In lower body weight patients receiving DARZALEX FASPRO, higher rates of Grade 3–4 neutropenia were observed.
Thrombocytopenia
Daratumumab may increase thrombocytopenia induced by background therapy [see Adverse Reactions (6.1) ] .
Monitor complete blood cell counts periodically during treatment according to manufacturer's prescribing information for background therapies. Consider withholding DARZALEX FASPRO until recovery of platelets.
Embryo-Fetal Toxicity
Based on the mechanism of action, DARZALEX FASPRO can cause fetal harm when administered to a pregnant woman. DARZALEX FASPRO may cause depletion of fetal immune cells and decreased bone density. Advise pregnant women of the potential risk to a fetus. Advise females with reproductive potential to use effective contraception during treatment with DARZALEX FASPRO and for 3 months after the last dose [see Use in Specific Populations (8.1 , 8.3) ] .
The combination of DARZALEX FASPRO with lenalidomide, thalidomide or pomalidomide is contraindicated in pregnant women, because lenalidomide, thalidomide or pomalidomide may cause birth defects and death of the unborn child. Refer to the lenalidomide, thalidomide or pomalidomide prescribing information on use during pregnancy.
Interference with Serological Testing
Daratumumab binds to CD38 on red blood cells (RBCs) and results in a positive Indirect Antiglobulin Test (Indirect Coombs test). Daratumumab-mediated positive indirect antiglobulin test may persist for up to 6 months after the last daratumumab administration. Daratumumab bound to RBCs masks detection of antibodies to minor antigens in the patient's serum [see References (15) ] . The determination of a patient's ABO and Rh blood type are not impacted [see Drug Interactions (7.1) ] .
Notify blood transfusion centers of this interference with serological testing and inform blood banks that a patient has received DARZALEX FASPRO. Type and screen patients prior to starting DARZALEX FASPRO [see Dosage and Administration (2.1) ] .
Interference with Determination of Complete Response
Daratumumab is a human IgG kappa monoclonal antibody that can be detected on both the serum protein electrophoresis (SPE) and immunofixation (IFE) assays used for the clinical monitoring of endogenous M-protein [see Drug Interactions (7.1) ] . This interference can impact the determination of complete response and of disease progression in some DARZALEX FASPRO-treated patients with IgG kappa myeloma protein.
ADVERSE REACTIONS
The following clinically significant adverse reactions are described elsewhere in the labeling:
- Hypersensitivity and Other Administration Reactions [see Warnings and Precautions (5.1) ] .
- Cardiac Toxicity in Patients with Light Chain (AL) Amyloidosis [see Warnings and Precautions (5.2) ] .
- Infections [see Warnings and Precautions (5.3) ] .
- Neutropenia [see Warnings and Precautions (5.4) ] .
- Thrombocytopenia [see Warnings and Precautions (5.5) ] .
Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Newly Diagnosed Multiple Myeloma Eligible for Autologous Stem Cell Transplant
In Combination with Bortezomib, Lenalidomide and Dexamethasone
The safety of DARZALEX FASPRO in combination with bortezomib, lenalidomide and dexamethasone (n=351) from the start of induction to the end of consolidation compared to bortezomib, lenalidomide and dexamethasone (VRd) (n=347) was evaluated in PERSEUS [see Clinical Studies (14.1) ] . Patients received DARZALEX FASPRO 1,800 mg/30,000 units administered subcutaneously once weekly from weeks 1 to 8 and once every 2 weeks from weeks 9 to 16 during induction in combination with VRd or VRd alone. After week 16, patients underwent stem cell mobilization, high dose chemotherapy, and ASCT. Within 12 weeks of ASCT, and when engraftment was complete, patients received DARZALEX FASPRO once every 2 weeks from weeks 1 to 8 during consolidation in combination with VRd or VRd alone.
The median duration of treatment for induction and consolidation was 9.9 months (0.5 to 18.5 months) for DARZALEX FASPRO-VRd.
Serious adverse reactions occurred in 37% of patients who received DARZALEX FASPRO-VRd. The most frequent serious adverse reaction in >5% of patients who received DARZALEX FASPRO-VRd was pneumonia (6%). Fatal adverse reactions occurred in 1.7% of patients who received DARZALEX FASPRO-VRd.
Permanent treatment discontinuation due to an adverse reaction occurred in 2% of patients who received DARZALEX FASPRO-VRd. An adverse reaction which resulted in permanent discontinuation of DARZALEX FASPRO-VRd in more than 1 patient included sepsis.
The most common adverse reactions (≥20%) were peripheral neuropathy, fatigue, upper respiratory infection, constipation, musculoskeletal pain, insomnia, rash, diarrhea, edema, and pyrexia.
Table 9 summarizes the adverse reactions in patients who received DARZALEX FASPRO in PERSEUS.
| Adverse Reaction | DARZALEX FASPRO-VRd (N=351) | VRd (N=347) | ||
|---|---|---|---|---|
| All Grades (%) | Grade 3 or 4 (%) | All Grades (%) | Grade 3 or 4 (%) | |
| Key: VRd=bortezomib-lenalidomide-dexamethasone | ||||
| Nervous system disorders | ||||
| Peripheral neuropathy Peripheral neuropathy includes neuropathy peripheral, peripheral motor neuropathy, peripheral sensorimotor neuropathy, and peripheral sensory neuropathy. | 52 | 5 | 54 | 4 |
| Paresthesia | 11 | <1 Only Grade 3 adverse reactions occurred. | 11 | <1 |
| General disorders and administration site conditions | ||||
| Fatigue Includes other related terms. | 35 | 3 | 37 | 5 |
| Edema | 22 | 1 | 21 | 1 |
| Pyrexia | 21 | 2 | 22 | 3 |
| Infections | ||||
| Upper respiratory tract infection Upper respiratory tract infection includes fungal pharyngitis, h1n1 influenza, influenza, influenza like illness, laryngitis, nasopharyngitis, oral candidiasis, oropharyngeal candidiasis, parainfluenzae virus infection, pharyngitis, respiratory moniliasis, respiratory syncytial virus infection, respiratory tract infection, respiratory tract infection viral, rhinitis, rhinovirus infection, sinusitis, tonsillitis, upper respiratory tract infection, viral tonsillitis, and viral upper respiratory tract infection. | 32 | 1 | 26 | 2 |
| Pneumonia Pneumonia includes bronchopulmonary aspergillosis, lower respiratory tract infection, pneumocystis jirovecii pneumonia, pneumonia, pneumonia bacterial, pneumonia cytomegaloviral, pneumonia influenzal, pneumonia klebsiella, pneumonia legionella, and pneumonia streptococcal. | 14 | 9 | 10 | 6 Fatal adverse reactions included Pneumonia: n=1 (0.3%) in the VRd arm. |
| Gastrointestinal disorders | ||||
| Constipation | 31 | 2 | 30 | 2 |
| Diarrhea | 23 | 3 | 25 | 5 |
| Nausea | 16 | 1 | 12 | 1 |
| Abdominal pain | 11 | 0 | 12 | 0 |
| Musculoskeletal and connective tissue disorders | ||||
| Musculoskeletal pain | 26 | 1 | 23 | 1 |
| Muscle spasm | 12 | 0 | 9 | <1 |
| Psychiatric disorders | ||||
| Insomnia | 26 | 2 | 16 | 2 |
| Skin and subcutaneous tissue disorders | ||||
| Rash | 25 | 3 | 31 | 5 |
| Hepatobiliary disorders | ||||
| Hepatotoxicity Hepatotoxicity includes alanine aminotransferase increased, aspartate aminotransferase increased, hepatic cytolysis, hepatic failure, hepatic function abnormal, hepatotoxicity, hyperbilirubinemia, hypertransaminasemia, and liver disorder | 16 | 6 | 16 | 5 |
| Respiratory, thoracic and mediastinal disorders | ||||
| Cough | 12 | <1 | 8 | 0 |
Clinically relevant adverse reactions in <10% of patients who received DARZALEX FASPRO with bortezomib, lenalidomide and dexamethasone include:
- Gastrointestinal disorders: vomiting, hemorrhoids
- Musculoskeletal and connective tissue disorders: arthralgia
- Infections: bronchitis, sepsis, urinary tract infection, herpes zoster, Covid-19, cytomegalovirus infection
- Respiratory, thoracic, and mediastinal disorders: dyspnea, pulmonary edema
- Metabolism and nutrition disorders: hypocalcemia, decreased appetite, hyperglycemia, dehydration
- Vascular disorders: hypotension, hypertension, orthostatic hypotension
- General disorders and administration site conditions: infusion reactions, injection site reaction, chills
- Nervous system disorders: dizziness, headache, syncope
- Cardiac disorders: thrombosis, atrial fibrillation, tachycardia
- Skin and subcutaneous tissue disorders: pruritus
Table 10 summarizes the laboratory abnormalities in patients who received DARZALEX FASPRO in PERSEUS.
| Laboratory Abnormality | DARZALEX FASPRO-VRd Denominator is based on number of subjects with a baseline and post-baseline laboratory value for each laboratory test: N=351 for DARZALEX FASPRO-VRd and N=346 for VRd. | VRd | ||
|---|---|---|---|---|
| All Grades (%) | Grade 3 or4 (%) | All Grades (%) | Grade 3 or 4 (%) | |
| Key: VRd=bortezomib-lenalidomide-dexamethasone | ||||
| Hematology | ||||
| Decreased platelets | 89 | 34 | 78 | 25 |
| Decreased lymphocytes | 87 | 69 | 69 | 43 |
| Decreased leukocytes | 78 | 47 | 56 | 22 |
| Decreased neutrophils | 67 | 52 | 47 | 34 |
| Decreased hemoglobin | 39 | 7 | 43 | 6 |
| Chemistry | ||||
| Increased alanine aminotransferase (ALT) | 52 | 7 | 48 | 5 |
| Decreased sodium | 40 | 5 | 25 | 5 |
| Increased alkaline phosphatase | 39 | 0 | 36 | 1 |
| Decreased potassium | 30 | 6 | 24 | 3 |
Newly Diagnosed Multiple Myeloma Ineligible for Autologous Stem Cell Transplant
In Combination with Bortezomib, Lenalidomide and Dexamethasone
The safety of DARZALEX FASPRO in combination with bortezomib, lenalidomide and dexamethasone compared to bortezomib, lenalidomide and dexamethasone (VRd) was evaluated in CEPHEUS in patients with newly diagnosed multiple myeloma who were ineligible for ASCT or refused ASCT as initial therapy [see Clinical Studies (14.1) ] . Patients received DARZALEX FASPRO 1,800 mg/30,000 units administered subcutaneously once weekly from weeks 1 to 6, once every 3 weeks from weeks 7 to 24 and once every 4 weeks starting with week 25 until disease progression or unacceptable toxicity in combination with VRd (n=197) or VRd alone (n=195).
The median duration of treatment was 56.3 months (0.1 to 64.6 months) for DARZALEX FASPRO-VRd and 34.3 months (0.5 to 63.8 months) for VRd.
Serious adverse reactions occurred in 72% of patients who received DARZALEX FASPRO-VRd. The most frequent serious adverse reactions in >5% of patients who received DARZALEX FASPRO-VRd were pneumonia (19%), COVID-19 (12%), thromboembolism (7%), and diarrhea (6%). Fatal adverse reactions occurred in 16.8% of patients who received DARZALEX FASPRO-VRd. Fatal adverse reactions that occurred in more than 1 patient included pneumonia (4%), COVID-19 (4%), and myocardial infarction (2%).
Permanent treatment discontinuation due to an adverse reaction occurred in 8% of patients who received DARZALEX FASPRO-VRd. An adverse reaction which resulted in permanent discontinuation of DARZALEX FASPRO-VRd in more than 1 patient included pneumonia.
The most common adverse reactions (≥20%) were upper respiratory tract infection, sensory neuropathy, musculoskeletal pain, diarrhea, fatigue, edema, rash, motor dysfunction, COVID-19, constipation, sleep disorder, cough, pneumonia, renal impairment, dizziness, nausea, urinary tract infection, pyrexia, abdominal pain, dyspnea, decreased appetite, and bruising.
Table 11 summarized the adverse reactions in patients who received DARZALEX FASPRO in CEPHEUS.
| Adverse Reaction | DARZALEX FASPRO-VRd (N=197) | VRd (N=195) | ||
|---|---|---|---|---|
| All Grades (%) | Grade 3 or 4 (%) | All Grades (%) | Grade 3 or 4 (%) | |
| Key: VRd=bortezomib-lenalidomide dexamethasone | ||||
| Infections | ||||
| Upper respiratory tract infection Upper respiratory tract infection includes acute sinusitis, influenza, influenza like illness, laryngitis, nasal congestion, nasopharyngitis, parainfluenzae virus infection, pharyngitis, pharyngitis streptococcal, respiratory syncytial virus infection, respiratory tract infection, respiratory tract infection bacterial, respiratory tract infection viral, rhinitis, rhinovirus infection, sinus congestion, sinus disorder, sinusitis, tonsillitis, tracheitis, upper respiratory tract infection, upper respiratory tract inflammation, and viral upper respiratory tract infection. | 75 | 4 Only Grade 3 adverse reactions occurred. | 63 | 3 |
| COVID-19 Includes other related terms. | 39 Fatal adverse reactions occurred for Abdominal pain: n=1 (1%) in the DARZALEX FASPRO-VRd arm; COVID-19: n=7 (4%) in the DARZALEX FASPRO-VRd arm and n=5 (3%) in the VRd arm; Pneumonia: n=8 (4%) in the DARZALEX FASPRO-VRd arm and n=5 (3%) in the VRd arm; Dyspnea: n=1 (1%) in the DARZALEX FASPRO-VRd arm. | 9 | 25 | 3 |
| Pneumonia Pneumonia includes bronchopulmonary aspergillosis, covid-19 pneumonia, lower respiratory tract infection, pneumocystis jirovecii pneumonia, pneumonia, pneumonia aspiration, pneumonia bacterial, pneumonia cryptococcal, pneumonia influenzal, pneumonia klebsiella, pneumonia legionella, pneumonia pneumococcal, pneumonia respiratory syncytial viral, pneumonia viral, and tuberculosis. | 31 | 16 | 26 | 15 |
| Urinary tract infection | 24 | 4 | 17 | 3 |
| Nervous system disorders | ||||
| Sensory neuropathy Sensory neuropathy includes anosmia, burning sensation, dysesthesia, hyperesthesia, hyperesthesia teeth, hypoesthesia, hypoesthesia oral, neuralgia, neuropathy peripheral, oral dysesthesia, palmar-plantar erythrodysesthesia syndrome, paresthesia, paresthesia oral, peripheral sensorimotor neuropathy, peripheral sensory neuropathy, polyneuropathy, and skin burning sensation. | 72 | 12 | 72 | 10 |
| Motor dysfunction Motor dysfunction includes balance disorder, essential tremor, extrapyramidal disorder, facial paralysis, gait disturbance, hypotonia, mobility decreased, motor dysfunction, muscle contractions involuntary, muscle contracture, muscle spasms, muscular weakness, myopathy, paraparesis, peripheral motor neuropathy, peroneal nerve palsy, pharyngeal paresthesia, and tremor. | 44 | 11 | 37 | 7 |
| Dizziness | 26 | 2 | 26 | 1 |
| Musculoskeletal and connective tissue disorders | ||||
| Musculoskeletal pain | 62 | 9 | 61 | 7 |
| Gastrointestinal disorders | ||||
| Diarrhea | 57 | 12 | 59 | 9 |
| Constipation | 38 | 2 | 42 | 3 |
| Nausea | 25 | 0 | 25 | 2 |
| Abdominal pain | 23 | 1 | 17 | 2 |
| General disorders and administration site conditions | ||||
| Fatigue | 56 | 14 | 53 | 11 |
| Edema | 54 | 4 | 46 | 2 |
| Pyrexia | 24 | 1 | 16 | 1 |
| Skin and subcutaneous tissue disorders | ||||
| Rash | 50 | 8 | 47 | 7 |
| Psychiatric disorders | ||||
| Sleep disorder | 33 | 3 | 33 | 2 |
| Respiratory, thoracic and mediastinal disorders | ||||
| Cough | 32 | 1 | 21 | 1 |
| Dyspnea | 21 | 2 | 17 | 1 |
| Renal and urinary disorders | ||||
| Renal impairment Renal impairment includes acute kidney injury, blood creatinine increased, chronic kidney disease, creatinine renal clearance decreased, glomerular filtration rate decreased, prerenal failure, renal failure, renal impairment, and renal injury. | 26 | 7 | 25 | 6 |
| Metabolism and nutrition disorders | ||||
| Decreased appetite | 21 | 1 | 20 | 3 |
| Injury, poisoning and procedural complications | ||||
| Bruising | 20 | 0 | 12 | 0 |
Clinically relevant adverse reactions in <20% of patients who received DARZALEX FASPRO with bortezomib, lenalidomide and dexamethasone include:
- Infections: bronchitis, sepsis, herpes zoster, hepatitis B reactivation
- Gastrointestinal disorders: vomiting, pancreatitis
- Metabolism and nutrition disorders: hyperglycemia
- Vascular disorders: hypertension, hypotension, thromboembolism, hemorrhage
- Nervous system disorders: headache, syncope
- General disorders and administration site conditions: chills, infusion reactions, injection site reactions
- Cardiac disorders: atrial fibrillation
- Skin and subcutaneous tissue disorders: pruritus
Table 12 summarizes the laboratory abnormalities in patients who received DARZALEX FASPRO in CEPHEUS.
| Laboratory Abnormality | DARZALEX FASPRO-VRd Denominator is based on number of subjects with a baseline and post-baseline laboratory value for each laboratory test: N=197 for DARZALEX FASPRO-VRd and N=194 for VRd. | VRd | ||
|---|---|---|---|---|
| All Grades (%) | Grade 3 or 4 (%) | All Grades (%) | Grade 3 or 4 (%) | |
| Key: VRd=bortezomib-lenalidomide-dexamethasone | ||||
| Hematology | ||||
| Decreased leukocytes | 93 | 39 | 77 | 15 |
| Decreased neutrophils | 89 | 49 | 75 | 35 |
| Decreased lymphocytes | 87 | 55 | 72 | 38 |
| Decreased platelets | 81 | 31 | 73 | 23 |
| Decreased hemoglobin | 53 | 14 | 52 | 16 |
| Chemistry | ||||
| Increased alanine aminotransferase (ALT) | 66 | 7 | 61 | 3 |
| Increased creatinine | 54 | 5 | 56 | 3 |
| Decreased potassium | 53 | 19 | 36 | 12 |
| Decreased sodium | 48 | 16 | 40 | 13 |
| Increased aspartate aminotransferase (AST) | 43 | 3 | 46 | 3 |
| Increased alkaline phosphatase | 43 | 2 | 31 | 1 |
| Decreased corrected calcium | 32 | 5 | 26 | 5 |
Newly Diagnosed Multiple Myeloma Ineligible for Autologous Stem Cell Transplant
In Combination with Bortezomib, Melphalan and Prednisone
The safety of DARZALEX FASPRO with bortezomib, melphalan and prednisone was evaluated in a single-arm cohort of PLEIADES [see Clinical Studies (14.1) ] . Patients received DARZALEX FASPRO 1,800 mg/30,000 units administered subcutaneously once weekly from weeks 1 to 6, once every 3 weeks from weeks 7 to 54 and once every 4 weeks starting with week 55 until disease progression or unacceptable toxicity (N=67) in combination with bortezomib, melphalan and prednisone. Among these patients, 93% were exposed for 6 months or longer and 19% were exposed for greater than one year.
Serious adverse reactions occurred in 39% of patients who received DARZALEX FASPRO. Serious adverse reactions in >5% of patients included pneumonia and pyrexia. Fatal adverse reactions occurred in 3% of patients.
Permanent discontinuation of DARZALEX FASPRO due to an adverse reaction occurred in 4.5% of patients. The adverse reaction resulting in permanent discontinuation of DARZALEX FASPRO in more than 1 patient was neutropenic sepsis.
Dosage interruptions (defined as dose delays or skipped doses) due to an adverse reaction occurred in 51% of patients who received DARZALEX FASPRO. Adverse reactions requiring dosage interruptions in >5% of patients included thrombocytopenia, neutropenia, anemia, and pneumonia.
The most common adverse reactions (≥20%) were upper respiratory tract infection, constipation, nausea, fatigue, pyrexia, peripheral sensory neuropathy, diarrhea, cough, insomnia, vomiting, and back pain.
Table 13 summarizes the adverse reactions in patients who received DARZALEX FASPRO in PLEIADES.
| Adverse Reaction | DARZALEX FASPRO with Bortezomib, Melphalan and Prednisone (N=67) | |
|---|---|---|
| All Grades (%) | Grades ≥3 (%) | |
| Infections | ||
| Upper respiratory tract infection Upper respiratory tract infection includes nasopharyngitis, respiratory syncytial virus infection, respiratory tract infection, rhinitis, tonsillitis, upper respiratory tract infection, and viral pharyngitis. | 39 | 0 |
| Bronchitis | 16 | 0 |
| Pneumonia Pneumonia includes lower respiratory tract infection, lung infection, pneumocystis jirovecii pneumonia, pneumonia, and pneumonia bacterial. | 15 | 7 Only Grade 3 adverse reactions occurred. |
| Gastrointestinal disorders | ||
| Constipation | 37 | 0 |
| Nausea | 36 | 0 |
| Diarrhea | 33 | 3 |
| Vomiting | 21 | 0 |
| Abdominal pain Abdominal pain includes abdominal pain, and abdominal pain upper. | 13 | 0 |
| General disorders and administration site conditions | ||
| Fatigue Fatigue includes asthenia, and fatigue. | 36 | 3 |
| Pyrexia | 34 | 0 |
| Edema peripheral Edema peripheral includes edema, edema peripheral, and peripheral swelling. | 13 | 1 |
| Nervous system disorders | ||
| Peripheral sensory neuropathy | 34 | 1 |
| Dizziness | 10 | 0 |
| Respiratory, thoracic and mediastinal disorders | ||
| Cough Cough includes cough, and productive cough. | 24 | 0 |
| Psychiatric disorders | ||
| Insomnia | 22 | 3 |
| Musculoskeletal and connective tissue disorders | ||
| Back pain | 21 | 3 |
| Musculoskeletal chest pain | 12 | 0 |
| Metabolism and nutrition disorders | ||
| Decreased appetite | 15 | 1 |
| Skin and subcutaneous tissue disorders | ||
| Rash | 13 | 0 |
| Pruritus | 12 | 0 |
| Vascular disorders | ||
| Hypertension | 13 | 6 |
| Hypotension | 10 | 3 |
Clinically relevant adverse reactions in <10% of patients who received DARZALEX FASPRO with bortezomib, melphalan and prednisone included:
- General disorders and administration site conditions: infusion reaction, injection site reaction, chills
- Infections: herpes zoster, urinary tract infection, influenza, sepsis
- Musculoskeletal and connective tissue disorders: arthralgia, muscle spasms
- Nervous system disorders: headache, paresthesia
- Metabolism and nutrition disorders: hypocalcemia, hyperglycemia
- Respiratory, thoracic and mediastinal disorders: dyspnea, pulmonary edema
- Cardiac disorders: atrial fibrillation
Table 14 summarizes the laboratory abnormalities in patients who received DARZALEX FASPRO in PLEIADES.
| Laboratory Abnormality | DARZALEX FASPRO with Bortezomib, Melphalan and Prednisone Denominator is based on the safety population treated with DARZALEX FASPRO-VMP (N=67). | |
|---|---|---|
| All Grades (%) | Grades 3–4 (%) | |
| Decreased leukocytes | 96 | 52 |
| Decreased lymphocytes | 93 | 84 |
| Decreased platelets | 93 | 42 |
| Decreased neutrophils | 88 | 49 |
| Decreased hemoglobin | 48 | 19 |
Relapsed/Refractory Multiple Myeloma
In Combination with Lenalidomide and Dexamethasone
The safety of DARZALEX FASPRO with lenalidomide and dexamethasone was evaluated in a single-arm cohort of PLEIADES [see Clinical Studies (14.2) ]. Patients received DARZALEX FASPRO 1,800 mg/30,000 units administered subcutaneously once weekly from weeks 1 to 8, once every 2 weeks from weeks 9 to 24 and once every 4 weeks starting with week 25 until disease progression or unacceptable toxicity (N=65) in combination with lenalidomide and dexamethasone. Among these patients, 92% were exposed for 6 months or longer and 20% were exposed for greater than one year.
Serious adverse reactions occurred in 48% of patients who received DARZALEX FASPRO. Serious adverse reactions in >5% of patients included pneumonia, influenza and diarrhea. Fatal adverse reactions occurred in 3.1% of patients.
Permanent discontinuation of DARZALEX FASPRO due to an adverse reaction occurred in 11% of patients who received DARZALEX FASPRO. Adverse reactions resulting in permanent discontinuation of DARZALEX FASPRO in more than 1 patient were pneumonia and anemia.
Dosage interruptions due to an adverse reaction occurred in 63% of patients who received DARZALEX FASPRO. Adverse reactions requiring dosage interruptions in >5% of patients included neutropenia, pneumonia, upper respiratory tract infection, influenza, dyspnea, and blood creatinine increased.
The most common adverse reactions (≥20%) were fatigue, diarrhea, upper respiratory tract infection, muscle spasms, constipation, pyrexia, pneumonia, and dyspnea.
Table 15 summarizes the adverse reactions in patients who received DARZALEX FASPRO in PLEIADES.
| Adverse Reaction | DARZALEX FASPRO with Lenalidomide and Dexamethasone (N=65) | |
|---|---|---|
| All Grades (%) | Grades ≥3 (%) | |
| General disorders and administration site conditions | ||
| Fatigue Fatigue includes asthenia, and fatigue. | 52 | 5 Only Grade 3 adverse reactions occurred. |
| Pyrexia | 23 | 2 |
| Edema peripheral | 18 | 3 |
| Gastrointestinal disorders | ||
| Diarrhea | 45 | 5 |
| Constipation | 26 | 2 |
| Nausea | 12 | 0 |
| Vomiting | 11 | 0 |
| Infections | ||
| Upper respiratory tract infection Upper respiratory tract infection includes nasopharyngitis, pharyngitis, respiratory tract infection viral, rhinitis, sinusitis, upper respiratory tract infection, and upper respiratory tract infection bacterial. | 43 | 3 |
| Pneumonia Pneumonia includes lower respiratory tract infection, lung infection, and pneumonia. | 23 | 17 |
| Bronchitis Bronchitis includes bronchitis, and bronchitis viral. | 14 | 2 |
| Urinary tract infection | 11 | 0 |
| Musculoskeletal and connective tissue disorders | ||
| Muscle spasms | 31 | 2 |
| Back pain | 14 | 0 |
| Respiratory, thoracic and mediastinal disorders | ||
| Dyspnea Dyspnea includes dyspnea, and dyspnea exertional. | 22 | 3 |
| Cough Cough includes cough, and productive cough. | 14 | 0 |
| Nervous system disorders | ||
| Peripheral sensory neuropathy | 17 | 2 |
| Psychiatric disorders | ||
| Insomnia | 17 | 5 |
| Metabolism and nutrition disorders | ||
| Hyperglycemia | 12 | 9 |
| Hypocalcemia | 11 | 0 |
Clinically relevant adverse reactions in <10% of patients who received DARZALEX FASPRO with lenalidomide and dexamethasone included:
- Musculoskeletal and connective tissue disorders: arthralgia, musculoskeletal chest pain
- Nervous system disorders: dizziness, headache, paresthesia
- Skin and subcutaneous tissue disorders: rash, pruritus
- Gastrointestinal disorders: abdominal pain
- Infections: influenza, sepsis, herpes zoster
- Metabolism and nutrition disorders: decreased appetite
- Cardiac disorders: atrial fibrillation
- General disorders and administration site conditions: chills, infusion reaction, injection site reaction
- Vascular disorders: hypotension, hypertension
Table 16 summarizes the laboratory abnormalities in patients who received DARZALEX FASPRO in PLEIADES.
| Laboratory Abnormality | DARZALEX FASPRO with Lenalidomide and Dexamethasone Denominator is based on the safety population treated with DARZALEX FASPRO-Rd (N=65). | |
|---|---|---|
| All Grades (%) | Grades 3–4 (%) | |
| Decreased leukocytes | 94 | 34 |
| Decreased lymphocytes | 82 | 58 |
| Decreased platelets | 86 | 9 |
| Decreased neutrophils | 89 | 52 |
| Decreased hemoglobin | 45 | 8 |
In Combination with Pomalidomide and Dexamethasone
The safety of DARZALEX FASPRO with pomalidomide and dexamethasone compared to pomalidomide and dexamethasone (Pd) in patients who had received at least one prior line of therapy with lenalidomide and a proteasome inhibitor (PI) was evaluated in APOLLO [see Clinical Studies (14.2) ] . Patients received DARZALEX FASPRO 1,800 mg/30,000 units administered subcutaneously once weekly from weeks 1 to 8, once every 2 weeks from weeks 9 to 24 and once every 4 weeks starting with week 25 until disease progression or unacceptable toxicity in combination with pomalidomide and dexamethasone (n=149) or pomalidomide and dexamethasone (n=150). Among patients receiving DARZALEX FASPRO-Pd, 71% were exposed for 6 months or longer and 50% were exposed for greater than one year.
Serious adverse reactions occurred in 50% of patients who received DARZALEX FASPRO-Pd. The most frequent serious adverse reactions in >5% of patients who received DARZALEX FASPRO-Pd were pneumonia (15%) and lower respiratory tract infection (12%). Fatal adverse reactions occurred in 7% of patients who received DARZALEX FASPRO-Pd.
Permanent treatment discontinuation due to an adverse reaction occurred in 2% of patients who received DARZALEX FASPRO-Pd.
The most common adverse reactions (≥20%) were fatigue, pneumonia, upper respiratory tract infection, and diarrhea.
Table 17 summarizes the adverse reactions in patients who received DARZALEX FASPRO in APOLLO.
| Adverse Reaction | DARZALEX FASPRO-Pd (N=149) | Pd (N=150) | ||
|---|---|---|---|---|
| All Grades (%) | Grades ≥3 (%) | All Grades (%) | Grades ≥3 (%) | |
| Key: Pd=pomalidomide-dexamethasone | ||||
| General disorders and administration site conditions | ||||
| Fatigue Fatigue includes asthenia, and fatigue. | 46 | 13 | 39 | 5 Only Grade 3 adverse reactions occurred. |
| Pyrexia | 19 | 0 | 14 | 0 |
| Edema peripheral Edema peripheral includes edema, edema peripheral and peripheral swelling. | 15 | 0 | 9 | 0 |
| Infections | ||||
| Pneumonia Pneumonia includes atypical pneumonia, lower respiratory tract infection, pneumonia, pneumonia aspiration, pneumonia bacterial, and pneumonia respiratory syncytial viral. | 38 | 23 Grade 5 adverse reactions occurred, n=3 (2.0%) in the DARZALEX FASPRO-Pd arm and n=2 (1.3%) in the Pd arm. | 27 | 17 |
| Upper respiratory infection Upper respiratory tract infection includes nasopharyngitis, pharyngitis, respiratory syncytial virus infection, respiratory tract infection, respiratory tract infection viral, rhinitis, sinusitis, tonsillitis, upper respiratory tract infection, and viral upper respiratory tract infection. | 36 | 1 | 22 | 2 |
| Gastrointestinal disorders | ||||
| Diarrhea | 22 | 5 | 14 | 1 |
| Respiratory, thoracic and mediastinal disorders | ||||
| Cough Cough includes cough, and productive cough. | 13 | 0 | 8 | 0 |
Clinically relevant adverse reactions in <10% of patients who received DARZALEX FASPRO with pomalidomide and dexamethasone include:
- Metabolism and nutrition disorders: hypocalcemia, hypokalemia, decreased appetite, dehydration
- Nervous system disorders: peripheral sensory neuropathy, syncope, headache, paresthesia, dizziness
- Musculoskeletal and connective tissue disorders: muscle spasms, musculoskeletal chest pain, arthralgia
- Psychiatric disorders: insomnia
- Gastrointestinal disorders: nausea, abdominal pain, vomiting
- Skin and subcutaneous tissue disorders: rash, pruritus
- Cardiac disorders: atrial fibrillation
- General disorders and administration site conditions: infusion reactions, chills, injection site reaction
- Infections: urinary tract infection, influenza, hepatitis B reactivation, herpes zoster, sepsis
- Vascular disorders: hypertension, hypotension
Table 18 summarizes the laboratory abnormalities in patients who received DARZALEX FASPRO in APOLLO.
| Laboratory Abnormality | DARZALEX FASPRO-Pd Denominator is based on number of subjects with a baseline and post-baseline laboratory value for each laboratory test: N=148 for DARZALEX FASPRO-Pd and N=149 for Pd. | Pd | ||
|---|---|---|---|---|
| All Grades (%) | Grades 3–4 (%) | All Grades (%) | Grades 3–4 (%) | |
| Key: Pd=pomalidomide-dexamethasone | ||||
| Decreased neutrophils | 97 | 84 | 84 | 63 |
| Decreased leukocytes | 95 | 64 | 82 | 40 |
| Decreased lymphocytes | 93 | 59 | 79 | 33 |
| Decreased platelets | 75 | 19 | 60 | 19 |
| Decreased hemoglobin | 51 | 16 | 57 | 15 |
In Combination with Carfilzomib and Dexamethasone
The safety of DARZALEX FASPRO with carfilzomib and dexamethasone was evaluated in a single-arm cohort of PLEIADES [see Clinical Studies (14.2) ]. Patients received DARZALEX FASPRO 1,800 mg/30,000 units administered subcutaneously once weekly from Weeks 1 to 8, once every 2 weeks from Weeks 9 to 24 and once every 4 weeks starting with Week 25 until disease progression or unacceptable toxicity (N=66) in combination with carfilzomib and dexamethasone. Among these patients, 77% were exposed for 6 months or longer and 27% were exposed for greater than one year.
Serious adverse reactions occurred in 27% of patients who received DARZALEX FASPRO in combination with carfilzomib and dexamethasone. Fatal adverse reactions occurred in 3% of patients who received DARZALEX FASPRO in combination with carfilzomib and dexamethasone.
Permanent discontinuation of DARZALEX FASPRO due to an adverse reaction occurred in 6% of patients who received DARZALEX FASPRO.
Dosage interruptions due to an adverse reaction occurred in 46% of patients who received DARZALEX FASPRO.
The most common adverse reactions (≥20%) were upper respiratory tract infection, fatigue, insomnia, hypertension, diarrhea, cough, dyspnea, headache, pyrexia, nausea, and edema peripheral.
Table 19 summarizes the adverse reactions in patients who received DARZALEX FASPRO with carfilzomib and dexamethasone (DARZALEX FASPRO-Kd) in PLEIADES.
| Adverse Reaction | DARZALEX FASPRO-Kd (N=66) | |
|---|---|---|
| All Grades (%) | Grade ≥3 (%) | |
| Infections and infestations | ||
| Upper respiratory tract infection Upper respiratory tract infection includes nasopharyngitis, pharyngitis, respiratory tract infection, respiratory tract infection viral, rhinitis, sinusitis, tonsillitis, upper respiratory tract infection, viral pharyngitis, and viral upper respiratory tract infection. | 52 | 0 |
| Bronchitis Bronchitis includes bronchitis, and bronchitis viral. | 12 | 2 Only Grade 3 adverse reactions occurred. |
| General disorders and administration site conditions | ||
| Fatigue Fatigue includes asthenia, and fatigue. | 39 | 2 |
| Pyrexia | 21 | 2 |
| Edema peripheral Edema peripheral includes generalized edema, edema peripheral, and peripheral swelling. | 20 | 0 |
| Psychiatric disorders | ||
| Insomnia | 33 | 6 |
| Vascular disorders | ||
| Hypertension Hypertension includes blood pressure increased, and hypertension. | 32 | 21 |
| Gastrointestinal disorders | ||
| Diarrhea | 29 | 0 |
| Nausea | 21 | 0 |
| Vomiting | 15 | 0 |
| Respiratory, thoracic and mediastinal disorders | ||
| Cough Cough includes cough, and productive cough. | 24 | 0 |
| Dyspnea Dyspnea includes dyspnea, and dyspnea exertional. | 23 | 2 |
| Nervous system disorders | ||
| Headache | 23 | 0 |
| Peripheral sensory neuropathy | 11 | 0 |
| Musculoskeletal and connective tissue disorders | ||
| Back pain | 17 | 2 |
| Musculoskeletal chest pain | 11 | 0 |
Clinically relevant adverse reactions in <10% of patients who received DARZALEX FASPRO with carfilzomib and dexamethasone include:
- Gastrointestinal disorders: abdominal pain, constipation, pancreatitis
- Infection and infestations: pneumonia, influenza, urinary tract infection, herpes zoster, sepsis
- Metabolism and nutrition disorders: hyperglycemia, decreased appetite, hypocalcemia
- Musculoskeletal and connective tissue disorders: muscle spasms, arthralgia
- Nervous system disorders: paresthesia, dizziness, syncope
- General disorders and administration site conditions: injection site reaction, infusion reactions, chills
- Skin and subcutaneous tissue disorders: rash, pruritus
- Cardiac disorders: cardiac failure
- Vascular disorders: hypotension
Table 20 summarizes the laboratory abnormalities in patients who received DARZALEX FASPRO with carfilzomib and dexamethasone in PLEIADES.
| Laboratory Abnormality | DARZALEX FASPRO-Kd Denominator is based on the safety population treated with DARZALEX FASPRO-Kd (N=66). | |
|---|---|---|
| All Grades (%) | Grades 3–4 (%) | |
| Decreased platelets | 88 | 18 |
| Decreased lymphocytes | 83 | 50 |
| Decreased leukocytes | 68 | 18 |
| Decreased neutrophils | 55 | 15 |
| Decreased hemoglobin | 47 | 6 |
| Decreased corrected calcium | 45 | 2 |
| Increased alanine aminotransferase (ALT) | 35 | 5 |
Monotherapy
The safety of DARZALEX FASPRO as monotherapy was evaluated in COLUMBA [see Clinical Studies (14.2) ]. Patients received DARZALEX FASPRO 1,800 mg/30,000 units administered subcutaneously or daratumumab 16 mg/kg administered intravenously; each administered once weekly from weeks 1 to 8, once every 2 weeks from weeks 9 to 24 and once every 4 weeks starting with week 25 until disease progression or unacceptable toxicity. Among patients receiving DARZALEX FASPRO, 37% were exposed for 6 months or longer and 1% were exposed for greater than one year.
Serious adverse reactions occurred in 26% of patients who received DARZALEX FASPRO. Fatal adverse reactions occurred in 5% of patients. Fatal adverse reactions occurring in more than 1 patient were general physical health deterioration, septic shock, and respiratory failure.
Permanent discontinuation due to an adverse reaction occurred in 10% of patients who received DARZALEX FASPRO. Adverse reactions resulting in permanent discontinuation of DARZALEX FASPRO in more than 2 patients were thrombocytopenia and hypercalcemia.
Dosage interruptions due to an adverse reaction occurred in 26% of patients who received DARZALEX FASPRO. Adverse reactions requiring dosage interruption in >5% of patients included thrombocytopenia.
The most common adverse reaction (≥20%) was upper respiratory tract infection.
Table 21 summarizes the adverse reactions in COLUMBA.
| Adverse Reaction | DARZALEX FASPRO (N=260) | Intravenous Daratumumab (N=258) | ||
|---|---|---|---|---|
| All Grades (%) | Grade ≥3 (%) | All Grades (%) | Grade ≥3 (%) | |
| Infections | ||||
| Upper respiratory tract infection Upper respiratory tract infection includes acute sinusitis, nasopharyngitis, pharyngitis, respiratory syncytial virus infection, respiratory tract infection, rhinitis, rhinovirus infection, sinusitis, and upper respiratory tract infection. | 24 | 1 Only Grade 3 adverse reactions occurred. | 22 | 1 |
| Pneumonia Pneumonia includes lower respiratory tract infection, lung infection, pneumocystis jirovecii pneumonia, and pneumonia. | 8 | 5 | 10 | 6 Grade 5 adverse reactions occurred. |
| Gastrointestinal disorders | ||||
| Diarrhea | 15 | 1 | 11 | 0.4 |
| Nausea | 8 | 0.4 | 11 | 0.4 |
| General disorders and administration site conditions | ||||
| Fatigue Fatigue includes asthenia, and fatigue. | 15 | 1 | 16 | 2 |
| Infusion reactions Infusion reactions includes terms determined by investigators to be related to infusion. | 13 | 2 | 34 | 5 |
| Pyrexia | 13 | 0 | 13 | 1 |
| Chills | 6 | 0.4 | 12 | 1 |
| Musculoskeletal and connective tissue disorders | ||||
| Back pain | 10 | 2 | 12 | 3 |
| Respiratory, thoracic and mediastinal disorders | ||||
| Cough Cough includes cough, and productive cough. | 9 | 1 | 14 | 0 |
| Dyspnea Dyspnea includes dyspnea, and dyspnea exertional. | 6 | 1 | 11 | 1 |
Clinically relevant adverse reactions in <10% of patients who received DARZALEX FASPRO included:
- General disorders and administration site conditions: injection site reaction, peripheral edema
- Musculoskeletal and connective tissue disorders: arthralgia, musculoskeletal chest pain, muscle spasms
- Gastrointestinal disorders: constipation, vomiting, abdominal pain
- Metabolism and nutrition disorders: decreased appetite, hyperglycemia, hypocalcemia, dehydration
- Psychiatric disorders: insomnia
- Vascular disorders: hypertension, hypotension
- Nervous system disorders: dizziness, peripheral sensory neuropathy, paresthesia
- Infections: bronchitis, influenza, urinary tract infection, herpes zoster, sepsis, hepatitis B virus reactivation
- Skin and subcutaneous tissue disorders: pruritus, rash
- Cardiac disorders: atrial fibrillation
- Respiratory, thoracic and mediastinal disorders: pulmonary edema
Table 22 summarizes the laboratory abnormalities in COLUMBA.
| Laboratory Abnormality | DARZALEX FASPRO Denominator is based on the safety population treated with DARZALEX FASPRO (N=260) and Intravenous Daratumumab (N=258). | Intravenous Daratumumab | ||
|---|---|---|---|---|
| All Grades (%) | Grades 3–4 (%) | All Grades (%) | Grades 3–4 (%) | |
| Decreased leukocytes | 65 | 19 | 57 | 14 |
| Decreased lymphocytes | 59 | 36 | 56 | 36 |
| Decreased neutrophils | 55 | 19 | 43 | 11 |
| Decreased platelets | 43 | 16 | 45 | 14 |
| Decreased hemoglobin | 42 | 14 | 39 | 16 |
High-Risk Smoldering Multiple Myeloma
The safety of DARZALEX FASPRO as monotherapy in patients with high-risk smoldering multiple myeloma was evaluated in AQUILA [see Clinical Studies (14.3) ] . Patients received DARZALEX FASPRO 1,800 mg/30,000 units administered subcutaneously once weekly from weeks 1 to 8, once every 2 weeks from weeks 9 to 24 and once every 4 weeks starting with week 25 until 39 cycles or up to 36 months or until diagnosis of multiple myeloma or unacceptable toxicity.
The median duration of treatment for patients receiving DARZALEX FASPRO was 35 months (0 to 36 months).
Serious adverse reactions occurred in 29% of patients who received DARZALEX FASPRO. The most frequent serious adverse reactions in ≥2% of patients who received DARZALEX FASPRO were pneumonia (7%), fracture (3%), sepsis (2%), and upper respiratory tract infection (2%). Fatal adverse reactions occurred in 1% of patients who received DARZALEX FASPRO, including COVID-19 (0.5%) and pneumonia (0.5%).
Permanent treatment discontinuation due to an adverse reaction occurred in 6% of patients who received DARZALEX FASPRO. Adverse reactions which resulted in permanent discontinuation of DARZALEX FASPRO in more than 1 patient included fatigue, anxiety, and dyspnea.
Dosage interruptions of DARZALEX FASPRO due to an adverse reaction occurred in 47% of patients. Adverse reactions which required dosage interruption in ≥5% of patients included upper respiratory infection, pneumonia, and COVID-19.
The most common adverse reactions (≥20%) were upper respiratory tract infection, musculoskeletal pain, fatigue, diarrhea, rash, sleep disorder, sensory neuropathy, and injection site reactions.
Table 23 summarizes the adverse reactions in patients who received DARZALEX FASPRO in AQUILA.
| DARZALEX FASPRO (N=193) | ACTM (N=196) | |||
|---|---|---|---|---|
| Adverse Reaction | All Grades (%) | Grade 3 or 4 (%) | All Grades (%) | Grade 3 or 4 (%) |
| Key: ACTM=active monitoring | ||||
| Infections | ||||
| Upper respiratory tract infection Upper respiratory tract infection includes acute sinusitis, adenoviral upper respiratory infection, catarrh, influenza, influenza like illness, laryngitis, metapneumovirus infection, nasal congestion, nasopharyngitis, parainfluenzae virus infection, pharyngitis, respiratory tract congestion, respiratory tract infection, respiratory tract infection viral, sinus congestion, sinusitis, throat irritation, tonsillitis, tracheitis, upper respiratory tract congestion, upper respiratory tract infection, upper respiratory tract infection bacterial, upper-airway cough syndrome, and viral upper respiratory tract infection. | 66 | 1 Only Grade 3 adverse reactions occurred. | 27 | 0 |
| Pneumonia Pneumonia includes covid-19 pneumonia, lower respiratory tract infection, organizing pneumonia, pneumonia, pneumonia bacterial, pneumonia pneumococcal, pneumonia streptococcal, and pneumonia viral. | 16 | 7 Fatal adverse reactions occurred for Pneumonia: n=1 (1%) in the DARZALEX FASPRO arm. | 8 | 3 |
| Rhinitis Rhinitis includes rhinitis, rhinitis atrophic, rhinorrhea, rhinovirus infection, and viral rhinitis. | 10 | 0 | 2 | 0 |
| Musculoskeletal and connective tissue disorders | ||||
| Musculoskeletal pain Musculoskeletal pain includes arthralgia, axillary pain, back pain, breast pain, chest pain, facial spasm, fibromyalgia, flank pain, groin pain, muscle fatigue, muscle rupture, muscle spasms, muscle strain, muscle tightness, muscular weakness, musculoskeletal chest pain, musculoskeletal pain, musculoskeletal stiffness, myalgia, neck pain, non-cardiac chest pain, pain, pain in extremity, pain in jaw, periarthritis, radicular pain, rotator cuff syndrome, spinal pain, spinal stenosis, and tendon pain. | 59 | 1 | 42 | 3 |
| General disorders and administration site conditions | ||||
| Fatigue Fatigue includes asthenia, fatigue, and malaise. | 42 | 3 | 21 | 1 |
| Injection site reactions Injection site reaction includes injection site discoloration, injection site erythema, injection site hemorrhage, injection site induration, injection site edema, injection site pain, injection site pruritus, injection site rash, injection site swelling, injection site urticaria, injection site vesicles, and injection site warmth. | 20 | 0 | 0 | 0 |
| Infusion-related reactions Infusion-related reactions includes terms determined by investigators to be related to infusion. | 17 | 1 | 0 | 0 |
| Pyrexia | 17 | 0 | 3 | 1 |
| Edema Edema includes brain edema, eye swelling, eyelid edema, generalized edema, joint swelling, laryngeal edema, localized edema, edema, edema peripheral, peripheral swelling, post procedural edema, post procedural swelling, swelling face, and swelling of eyelid. | 15 | 1 | 5 | 1 |
| Gastrointestinal disorders | ||||
| Diarrhea | 27 | 2 | 5 | 1 |
| Nausea | 19 | 0 | 5 | 0 |
| Abdominal pain Abdominal pain includes abdominal discomfort, abdominal pain, abdominal pain lower, abdominal pain upper, abdominal tenderness, epigastric discomfort, and gastrointestinal pain. | 17 | 1 | 7 | 2 |
| Skin and subcutaneous tissue disorders | ||||
| Rash Rash includes acne, dermatitis, dermatitis allergic, dermatitis bullous, dermatitis contact, drug eruption, drug hypersensitivity, eczema, eczema asteatotic, eczema infected, erysipelas, erythema, erythema multiforme, rash, rash erythematous, rash maculo-papular, rash papular, rash pruritic, seborrheic dermatitis, seborrheic keratosis, skin lesion, skin reaction, skin ulcer, and urticaria. | 27 | 1 | 6 | 1 |
| Psychiatric disorders | ||||
| Sleep disorder Sleep disorder includes insomnia, restless legs syndrome, sleep apnea syndrome, sleep deficit, and sleep disorder. | 24 | 1 | 5 | 0 |
| Nervous system disorders | ||||
| Sensory neuropathy Sensory neuropathy includes allodynia, anosmia, burning sensation, carpal tunnel syndrome, cervical radiculopathy, cervicobrachial syndrome, dysesthesia, hypoesthesia, hypoesthesia oral, paresthesia, paresthesia oral, peripheral sensorimotor neuropathy, peripheral sensory neuropathy, pharyngeal paresthesia, polyneuropathy, and sensory disturbance. | 20 | 0 | 8 | 0 |
| Headache Headache includes headache, migraine, and vascular headache. | 18 | 1 | 8 | 0 |
| Dizziness Dizziness includes dizziness, and dizziness postural. | 12 | 0 | 5 | 0 |
| Respiratory, thoracic and mediastinal disorders | ||||
| Cough Cough includes cough, and productive cough. | 19 | 0 | 7 | 0 |
| Dyspnea Dyspnea includes dyspnea, and dyspnea exertional. | 18 | 1 | 6 | 1 |
Clinically relevant adverse reactions in <10% of patients who received DARZALEX FASPRO included:
- Gastrointestinal disorders: constipation, vomiting
- Skin and subcutaneous tissue disorders: pruritus
- Infections: bronchitis, urinary tract infection, herpes zoster, sepsis
- General disorders and administration site conditions: chills
- Metabolism and nutrition disorders: decreased appetite, hyperglycemia, dehydration
- Nervous system disorders: syncope
- Vascular disorders: hypotension
Table 24 summarizes the laboratory abnormalities in patients who received DARZALEX FASPRO in AQUILA.
| DARZALEX FASPRO Denominator is based on number of subjects with a baseline and post-baseline laboratory value for each laboratory test: N=191 for DARZALEX FASPRO and N=191 for ACTM. | ACTM | |||
|---|---|---|---|---|
| Laboratory Abnormality | All Grades (%) | Grade 3 or 4 (%) | All Grades (%) | Grade 3 or 4 (%) |
| Key: ACTM=active monitoring | ||||
| Hematology | ||||
| Decreased lymphocytes | 47 | 6 | 12 | 3 |
| Decreased hemoglobin | 42 | 0 | 44 | 2 |
| Decreased leukocytes | 34 | 3 | 27 | 2 |
| Decreased neutrophils | 34 | 6 | 29 | 4 |
| Decreased platelets | 19 | 1 | 9 | 1 |
| Chemistry | ||||
| Decreased albumin | 28 | 0 | 15 | 1 |
| Increased alanine aminotransferase (ALT) | 25 | 1 | 13 | 1 |
| Decreased sodium | 24 | 3 | 19 | 2 |
| Increased creatinine | 20 | 0 | 13 | 1 |
| Increased aspartate aminotransferase (AST) | 20 | 0 | 12 | 1 |
Light Chain Amyloidosis
In Combination with Bortezomib, Cyclophosphamide and Dexamethasone
The safety of DARZALEX FASPRO with bortezomib, cyclophosphamide and dexamethasone (DARZALEX FASPRO-VCd) was evaluated in ANDROMEDA [see Clinical Studies (14.4) ] . Patients received DARZALEX FASPRO 1,800 mg/30,000 units administered subcutaneously once weekly from weeks 1 to 8, once every 2 weeks from weeks 9 to 24 and once every 4 weeks starting with week 25 until disease progression or unacceptable toxicity or a maximum of 2 years. Among patients who received DARZALEX FASPRO-VCd, 74% were exposed for 6 months or longer and 32% were exposed for greater than one year.
Serious adverse reactions occurred in 43% of patients who received DARZALEX FASPRO in combination with VCd. Serious adverse reactions that occurred in at least 5% of patients in the DARZALEX FASPRO-VCd arm were pneumonia (9%), cardiac failure (8%), and sepsis (5%). Fatal adverse reactions occurred in 11% of patients. Fatal adverse reactions that occurred in more than one patient included cardiac arrest (4%), sudden death (3%), cardiac failure (3%), and sepsis (1%).
Permanent discontinuation of DARZALEX FASPRO due to an adverse reaction occurred in 5% of patients. Adverse reactions resulting in permanent discontinuation of DARZALEX FASPRO in more than one patient were pneumonia, sepsis, and cardiac failure.
Dosage interruptions (defined as dose delays or skipped doses) due to an adverse reaction occurred in 36% of patients who received DARZALEX FASPRO. Adverse reactions which required a dosage interruption in ≥3% of patients included upper respiratory tract infection (9%), pneumonia (6%), cardiac failure (4%), fatigue (3%), herpes zoster (3%), dyspnea (3%), and neutropenia (3%).
The most common adverse reactions (≥20%) were upper respiratory tract infection, diarrhea, peripheral edema, constipation, fatigue, peripheral sensory neuropathy, nausea, insomnia, dyspnea, and cough.
Table 25 below summarizes the adverse reactions in patients who received DARZALEX FASPRO in ANDROMEDA.
| Adverse Reaction | DARZALEX FASPRO-VCd (N=193) | VCd (N=188) | ||
|---|---|---|---|---|
| All Grades (%) | Grades 3–4 (%) | All Grades (%) | Grades 3–4 (%) | |
| Infections | ||||
| Upper respiratory tract infection Upper respiratory tract infection includes laryngitis, nasopharyngitis, pharyngitis, respiratory syncytial virus infection, respiratory tract infection, respiratory tract infection viral, rhinitis, rhinovirus infection, sinusitis, tonsillitis, tracheitis, upper respiratory tract infection, upper respiratory tract infection bacterial, and viral upper respiratory tract infection. | 40 | 1 Only Grade 3 adverse reactions occurred. | 21 | 1 |
| Pneumonia Pneumonia includes lower respiratory tract infection, pneumonia, pneumonia aspiration, and pneumonia pneumococcal. | 15 | 10 | 9 | 5 |
| Gastrointestinal disorders | ||||
| Diarrhea | 36 | 6 | 30 | 4 |
| Constipation | 34 | 2 | 29 | 0 |
| Nervous system disorders | ||||
| Peripheral sensory neuropathy | 31 | 3 | 20 | 2 |
| Respiratory, thoracic and mediastinal disorders | ||||
| Dyspnea Dyspnea includes dyspnea, and dyspnea exertional. | 26 | 4 | 20 | 4 |
| Cough Cough includes cough, and productive cough. | 20 | 1 | 11 | 0 |
| Musculoskeletal and connective tissue disorders | ||||
| Back pain | 12 | 2 | 6 | 0 |
| Arthralgia | 10 | 0 | 5 | 0 |
| Muscle spasms | 10 | 1 | 5 | 0 |
| Cardiac disorders | ||||
| Arrhythmia Arrhythmia includes atrial flutter, atrial fibrillation, supraventricular tachycardia, bradycardia, arrhythmia, bradyarrhythmia, cardiac flutter, extrasystoles, supraventricular extrasystoles, ventricular arrhythmia, ventricular extrasystoles, atrial tachycardia, ventricular tachycardia | 11 | 4 | 5 | 2 |
| General disorders and administration site conditions | ||||
| Injection site reactions Injection site reactions includes terms determined by investigators to be related to daratumumab injection. | 11 | 0 | 0 | 0 |
Clinically relevant adverse reactions not included in Table 25 and occurred in patients who received DARZALEX FASPRO with bortezomib, cyclophosphamide and dexamethasone included:
- Skin and subcutaneous tissue disorders: rash, pruritus
- Nervous system disorders: paresthesia
- General disorders and administration site conditions: infusion reaction, chills
- Cardiac disorders: cardiac failure Cardiac failure includes cardiac dysfunction, cardiac failure, cardiac failure congestive, cardiovascular insufficiency, diastolic dysfunction, pulmonary edema, and left ventricular dysfunction occurred in 11% of patients. , cardiac arrest
- Metabolism and nutrition disorders: hyperglycemia, hypocalcemia, dehydration
- Infections: bronchitis, herpes zoster, sepsis, urinary tract infection, influenza
- Vascular disorders: hypertension
- Musculoskeletal and connective tissue disorders: musculoskeletal chest pain
- Gastrointestinal disorders: pancreatitis
- Respiratory, thoracic and mediastinal disorders: pulmonary edema
Table 26 summarizes the laboratory abnormalities in patients who received DARZALEX FASPRO in ANDROMEDA.
| Laboratory Abnormality | DARZALEX FASPRO-VCd | VCd | ||
|---|---|---|---|---|
| All Grades (%) | Grades 3–4 (%) | All Grades (%) | Grades 3–4 (%) | |
| Denominator is based on the number of patients with a baseline and post-baseline laboratory value for each laboratory test, N=188 for DARZALEX FASPRO-VCd and N=186 for VCd. | ||||
| Decreased lymphocytes | 81 | 54 | 71 | 46 |
| Decreased hemoglobin | 66 | 6 | 70 | 6 |
| Decreased leukocytes | 60 | 7 | 46 | 4 |
| Decreased platelets | 46 | 3 | 40 | 4 |
| Decreased neutrophils | 30 | 6 | 18 | 4 |
Cardiac Adverse Reactions in Light Chain (AL) Amyloidosis
Among patients who received DARZALEX FASPRO in combination with VCd, 72% of patients had baseline cardiac involvement with Mayo Cardiac Stage I (3%), Stage II (46%) and Stage III (51%). Serious cardiac disorders occurred in 16% of patients (8% of patients with Mayo Cardiac Stage I and II and 28% of patients with Stage III). Serious cardiac disorders in >2% of patients included cardiac failure (8%), cardiac arrest (4%) and arrhythmia (4%). Fatal cardiac disorders occurred in 10% of patients (5% of patients with Mayo Cardiac Stage I and II and 19% of patients with Stage III) who received DARZALEX FASPRO in combination with VCd. Fatal cardiac disorders that occurred in more than one patient in the DARZALEX FASPRO-VCd arm included cardiac arrest (4%), sudden death (3%), and cardiac failure (3%).
Postmarketing Experience
The following adverse reactions have been identified with post-approval use of daratumumab. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Immune System : Anaphylactic reaction, Systemic administration reactions (including death)
Gastrointestinal: Pancreatitis
Infections: Cytomegalovirus, Listeriosis
DRUG INTERACTIONS
Effects of Daratumumab on Laboratory Tests
Interference with Indirect Antiglobulin Tests (Indirect Coombs Test)
Daratumumab binds to CD38 on RBCs and interferes with compatibility testing, including antibody screening and cross matching. Daratumumab interference mitigation methods include treating reagent RBCs with dithiothreitol (DTT) to disrupt daratumumab binding [see References (15) ] or genotyping. Since the Kell blood group system is also sensitive to DTT treatment, supply K-negative units after ruling out or identifying alloantibodies using DTT-treated RBCs.
If an emergency transfusion is required, administer non-cross-matched ABO/RhD-compatible RBCs per local blood bank practices.
Interference with Serum Protein Electrophoresis and Immunofixation Tests
Daratumumab may be detected on serum protein electrophoresis (SPE) and immunofixation (IFE) assays used for monitoring disease monoclonal immunoglobulins (M protein). False positive SPE and IFE assay results may occur for patients with IgG kappa myeloma protein impacting initial assessment of complete responses by International Myeloma Working Group (IMWG) criteria. In DARZALEX FASPRO-treated patients with persistent very good partial response, where daratumumab interference is suspected, consider using a FDA-approved daratumumab-specific IFE assay to distinguish daratumumab from any remaining endogenous M protein in the patient's serum, to facilitate determination of a complete response.
DESCRIPTION
Daratumumab is an immunoglobulin G1 kappa (IgG1κ) human monoclonal antibody that binds to the CD38 antigen. Daratumumab is produced in Chinese Hamster Ovary (CHO) cells using recombinant DNA technology. The molecular weight of daratumumab is approximately 148 kDa.
Hyaluronidase (recombinant human) is an endoglycosidase used to increase the dispersion and absorption of co-administered drugs when administered subcutaneously. It is a glycosylated single-chain protein produced by Chinese Hamster Ovary cells containing a DNA plasmid encoding for a soluble fragment of human hyaluronidase (PH20). Hyaluronidase (recombinant human) has a molecular weight of approximately 61 kDa.
DARZALEX FASPRO ® (daratumumab and hyaluronidase-fihj) injection is a sterile, preservative-free, colorless to yellow, and clear to opalescent solution supplied in a single-dose vial for subcutaneous administration.
Each DARZALEX FASPRO 15 mL single-dose vial contains 1,800 mg of daratumumab and 30,000 units of hyaluronidase, L-histidine (4.9 mg), L-histidine hydrochloride monohydrate (18.4 mg), L-methionine (13.5 mg), polysorbate 20 (6 mg), sorbitol (735.1 mg), and Water for Injection, USP.
CLINICAL PHARMACOLOGY
Mechanism of Action
CD38 is a transmembrane glycoprotein (48 kDa) expressed on the surface of hematopoietic cells, including clonal plasma cells in multiple myeloma and light chain (AL) amyloidosis, as well as other cell types. Surface CD38 has multiple functions, including receptor mediated adhesion, signaling, and modulation of cyclase and hydrolase activity. Daratumumab is an IgG1κ human monoclonal antibody (mAb) that binds to CD38 and inhibits the growth of CD38 expressing tumor cells by inducing apoptosis directly through Fc mediated cross linking as well as by immune-mediated tumor cell lysis through complement dependent cytotoxicity (CDC), antibody dependent cell mediated cytotoxicity (ADCC) and antibody dependent cellular phagocytosis (ADCP). A subset of myeloid derived suppressor cells (CD38+MDSCs), regulatory T cells (CD38+T regs ) and B cells (CD38+B regs ) are decreased by daratumumab.
Hyaluronan is a polysaccharide found in the extracellular matrix of the subcutaneous tissue. It is depolymerized by the naturally occurring enzyme hyaluronidase. Unlike the stable structural components of the interstitial matrix, hyaluronan has a half-life of approximately 0.5 days. Hyaluronidase increases permeability of the subcutaneous tissue by depolymerizing hyaluronan. In the doses administered, hyaluronidase in DARZALEX FASPRO acts locally. The effects of hyaluronidase are reversible and permeability of the subcutaneous tissue is restored within 24 to 48 hours.
Pharmacodynamics
NK cells express CD38 and are susceptible to daratumumab mediated cell lysis. Decreases in absolute counts and percentages of total NK cells (CD16+CD56+) and activated (CD16+CD56 dim ) NK cells in peripheral whole blood and bone marrow were observed with DARZALEX FASPRO treatment.
Cardiac Electrophysiology
DARZALEX FASPRO as a large protein has a low likelihood of direct ion channel interactions. There is no evidence from non-clinical or clinical data to suggest that DARZALEX FASPRO has the potential to delay ventricular repolarization.
Exposure-Response Relationship
The exposure-response relationship and time course of pharmacodynamics of DARZALEX FASPRO have not been fully characterized.
Pharmacokinetics
Following the recommended dose of DARZALEX FASPRO 1,800 mg/30,000 units subcutaneously once weekly for 8 weeks, daratumumab peak concentration (C max ) increased 4.8-fold and area under the curve (AUC 0–7 days ) increased 5.4-fold from the 1 st dose to the 8 th dose as monotherapy. Maximum trough concentrations for DARZALEX FASPRO are typically observed at the end of the weekly dosing regimens for both monotherapy and combination therapies. The mean ± standard deviation (SD) maximum trough serum concentration (C trough ) after the 8 th dose was 593 ± 306 µg/mL when DARZALEX FASPRO was administered as monotherapy in patients with multiple myeloma, 654 ± 243 µg/mL when DARZALEX FASPRO was administered as monotherapy in patients with smoldering multiple myeloma, and 537 ± 277 µg/mL, 526 ± 226 µg/mL, 756 ± 276 µg/mL, and 526 ± 209 µg/mL when DARZALEX FASPRO was administered as combination with Pd, Rd, Kd, and VRd in the PERSEUS trial, respectively. The observed mean ± SD maximum C trough after the 6 th dose was 407 ± 183 µg/mL when DARZALEX FASPRO was administered as combination with VRd in the CEPHEUS trial.
Table 27 lists the observed mean (±SD) maximum trough concentrations (C trough ) after the 8 th dose, simulated median (5 th –95 th percentiles) maximum C trough after the 8 th dose, simulated median (5 th –95 th percentiles) C max after the 8 th dose, and simulated median (5 th –95 th percentiles) area under the curve (AUC 0–7day ) after the 8 th dose following DARZALEX FASPRO 1,800 mg/30,000 units administered subcutaneously or daratumumab 16 mg/kg administered intravenously in patients with multiple myeloma, smoldering multiple myeloma or light chain (AL) amyloidosis. Daratumumab exposures were similar between patients treated with DARZALEX FASPRO 1,800 mg/30,000 units monotherapy and combination therapies.
| Parameter | Intravenous Daratumumab 16 mg/kg Monotherapy in Patients with Multiple Myeloma | DARZALEX FASPRO 1,800 mg/30,000 units Monotherapy in Patients with Multiple Myeloma | DARZALEX FASPRO 1,800 mg/30,000 units Monotherapy in Patients with Smoldering Multiple Myeloma | DARZALEX FASPRO 1,800 mg/30,000 units in combination with VRd in Patients with Transplant Eligible Multiple Myeloma | DARZALEX FASPRO 1,800 mg/30,000 units in combination with VCd in Patients with Light Chain (AL) Amyloidosis |
|---|---|---|---|---|---|
| Observed mean±SD max C trough after 8 th dose (µg/mL) | 522±226 Geometric mean ratio between 1,800 mg SC and 16 mg/kg was 108% (90% CI: 96, 122) in patients with multiple myeloma | 593±306 | 654±243 | 526±209 | 597±232 |
| Simulated median (5 th –95 th percentiles) max C trough after 8 th dose (µg/mL) | 472 (144–809) | 563 (177–1063) | 690 (269–1034) | 651 (413–915) | 662 (315–1037) |
| Simulated median (5 th –95 th percentiles) C max after 8 th dose (µg/mL) | 688 (369–1061) | 592 (234–1114) | 780 (340–1152) | 678 (431–958) | 729 (390–1105) |
| Simulated median (5 th –95 th percentiles) AUC 0–7days after 8 th dose (µg/mL∙day) | 4019 (1740–6370) | 4017 (1515–7564) | 5043 (2242–7426) | 4637 (2941–6522) | 4855 (2562–7522) |
Absorption
At the recommended dose of DARZALEX FASPRO 1,800 mg/30,000 units, the absolute bioavailability is 69%, with peak concentrations occurring around 3 days (T max ) in patients with multiple myeloma. Peak concentrations occurred around 4 days in patients with light chain (AL) amyloidosis.
Distribution
The estimated mean (coefficient of variation, CV) volume of distribution for the central compartment is 5.2 L (37%) and peripheral compartment was 3.8 L in patients with multiple myeloma. The estimated mean volume of distribution was 10.8 L (28%) in patients with light chain (AL) amyloidosis.
Elimination
Daratumumab is cleared by parallel linear and nonlinear saturable target mediated clearances. The estimated mean (CV%) linear clearance of daratumumab is 119 mL/day (59%) in patients with multiple myeloma and is 210 mL/day (42%) in patients with light chain (AL) amyloidosis. The estimated mean (CV%) elimination half-life associated with linear clearance is 20 days (22%) in patients with multiple myeloma and 28 days (74%) in patients with light chain (AL) amyloidosis.
Specific Populations
The following population characteristics have no clinically meaningful effect on the pharmacokinetics of daratumumab in patients administered DARZALEX FASPRO as monotherapy or as combination therapy: sex, age (33 to 92 years), renal impairment [Creatinine clearance (CLcr) 15 to 89 mL/min as determined by the Cockcroft-Gault formula], and mild hepatic impairment (total bilirubin 1 to 1.5 times ULN and AST>ULN). The effect of moderate and severe hepatic impairment on daratumumab pharmacokinetics is unknown.
Racial or Ethnic Groups
Of 190 patients with light chain (AL) amyloidosis who received DARZALEX FASPRO and had a maximum C trough after the 8 th dose, African-Americans (4%) had 24% higher daratumumab mean maximum C trough after the 8 th dose compared to that of Whites (83%) and Asians (10%) had 16% higher mean maximum C trough after the 8 th dose compared to that of Whites. The difference in exposure between that of Asians and Whites could be explained in part by differences in body size. The effect of African-American race on exposure and related safety and efficacy of daratumumab is unknown.
Body Weight
In patients with multiple myeloma who received DARZALEX FASPRO 1,800 mg/30,000 units as monotherapy, the mean maximum C trough after the 8 th dose was 12% lower in the higher body weight (BW) group (>85 kg), while the mean maximum C trough after the 8 th dose was 81% higher in the lower BW group (≤50 kg) compared to the corresponding BW groups in the intravenous daratumumab arm.
In patients with light chain (AL) amyloidosis who received DARZALEX FASPRO 1,800 mg/30,000 units in combination and had a maximum C trough after the 8 th dose, the mean maximum C trough after the 8 th dose was 22% lower in the higher BW group (>85 kg), while the mean maximum C trough was 37% higher in the lower BW group (≤50 kg) compared to the patients with body weight of 51–85 kg.
Immunogenicity
The observed incidence of anti-drug antibody (ADA, including neutralizing antibody) is highly dependent on the sensitivity and specificity of the assay. Differences in assay methods preclude meaningful comparisons of the incidence of ADA in the studies described below with the incidence of ADA in other studies, including those of daratumumab or of other daratumumab products.
With the median DARZALEX FASPRO treatment ranging from 6.5 to 56.6 months across 9 clinical trials of patients with smoldering multiple myeloma, multiple myeloma and light chain (AL) amyloidosis treated with DARZALEX as monotherapy or as combination therapies, the incidence of anti-daratumumab antibody development was 0.6% (9/1,563) and 8 patients tested positive for neutralizing antibodies. Because of the low occurrence of anti-daratumumab antibodies, the effect of these antibodies on the pharmacokinetics, pharmacodynamics, safety, and/or effectiveness of daratumumab products is unknown.
With the median DARZALEX FASPRO treatment ranging from 6.5 to 56.5 months across 9 clinical trials of patients with smoldering multiple myeloma, multiple myeloma and light chain (AL) amyloidosis treated with DARZALEX as monotherapy or as combination therapies, the incidence of anti-rHuPH20 antibody development was 8.7% (136/1,555) and 1 patient tested positive for neutralizing antibodies. There was no identified clinically significant effect of anti-rHuPH20 antibodies on pharmacokinetics, pharmacodynamics, safety, or effectiveness of daratumumab products.
NONCLINICAL TOXICOLOGY
Carcinogenesis, Mutagenesis, Impairment of Fertility
No carcinogenicity or genotoxicity studies have been conducted with daratumumab. No animal studies have been performed to evaluate the potential effects of daratumumab on reproduction or development, or to determine potential effects on fertility in males or females.
No carcinogenicity, genotoxicity, or fertility studies were conducted for recombinant human hyaluronidase. There were no effects on reproductive tissues and function and no systemic exposure of hyaluronidase in monkeys given 220,000 U/kg/week subcutaneously (440 times higher than the human dose) for 39 weeks. As hyaluronidase is a recombinant form of the endogenous human hyaluronidase, no carcinogenicity, mutagenesis, or effects on fertility are expected.
CLINICAL STUDIES
Newly Diagnosed Multiple Myeloma
In Combination with Bortezomib, Lenalidomide and Dexamethasone in Patients Eligible for Autologous Stem Cell Transplant
The efficacy of DARZALEX FASPRO with bortezomib, lenalidomide and dexamethasone (DARZALEX FASPRO-VRd) during induction and consolidation was evaluated in PERSEUS (NCT03710603), an open-label, randomized, active-controlled trial in patients with newly diagnosed multiple myeloma eligible for ASCT. Enrollment was limited to patients 70 years of age and younger.
Patients received DARZALEX FASPRO 1,800 mg/30,000 units administered subcutaneously once weekly from weeks 1 to 8 and once every 2 weeks from weeks 9 to 16 during induction. After week 16, patients underwent stem cell mobilization, high dose chemotherapy, and ASCT. Within 12 weeks of ASCT, and when engraftment was complete, patients received DARZALEX FASPRO once every 2 weeks from weeks 1 to 8 during consolidation. Bortezomib was administered by subcutaneous injection at a dose of 1.3 mg/m 2 body surface area twice weekly for two weeks (days 1, 4, 8, and 11) of each 28-day cycle for weeks 1–16 during induction and weeks 1–8 during consolidation. Lenalidomide was administered orally at 25 mg daily (days 1–21) during weeks 1–16 during induction and weeks 1–8 during consolidation. Dexamethasone (oral or intravenous) was administered at 40 mg on Days 1–4 and Days 9–12 during weeks 1–16 during induction and weeks 1–8 during consolidation. On the days of DARZALEX FASPRO injection, the dexamethasone dose was administered orally or intravenously as a pre-injection medication. Following consolidation, patients received an investigational treatment regimen for maintenance that included DARZALEX FASPRO in combination with lenalidomide or lenalidomide alone. The trial was not designed to isolate the effect of DARZALEX FASPRO in the maintenance phase of treatment. The efficacy of DARZALEX FASPRO in combination with lenalidomide for maintenance has not been established.
The major efficacy outcome measure was progression-free survival (PFS) by independent review committee (IRC) based on IMWG response criteria.
A total of 709 patients were randomized: 355 to the DARZALEX FASPRO-VRd arm and 354 to the VRd arm. The median age was 60 years (range: 31 to 70); 59% were male, 92% were White, 1% were Black or African American, and 1% were Asian. Fifty-one percent had ISS Stage I, 34% had ISS Stage II, 15% had ISS Stage III disease. High-risk cytogenetics (presence of del(17p), t(4;14), t(14,16)) were present in 22% of patients.
PERSEUS demonstrated an improvement in PFS in the DARZALEX FASPRO-VRd arm as compared to the VRd arm; the median PFS had not been reached in either arm. Treatment with DARZALEX FASPRO-VRd resulted in a reduction in the risk of disease progression or death by 60% compared to VRd alone (HR [95% CI]: 0.40 [0.29, 0.57]; p-value < 0.0001).
Figure 1: Kaplan-Meier Curve of PFS in PERSEUS

Additional efficacy results from PERSEUS are presented in Table 28.
| DARZALEX FASPRO-VRd (n=355) | VRd (n=354) | |
|---|---|---|
| VRd = bortezomib-lenalidomide-dexamethasone; MRD=minimal residual disease; CI=confidence interval | ||
| Overall response (sCR+CR+VGPR+PR), n (%) Based on intent-to-treat population | 338 (95.2%) | 326 (92.1%) |
| Stringent complete response (sCR) | 67 (18.9%) | 46 (13.0%) |
| Complete response (CR) | 91 (25.6%) | 77 (21.8%) |
| Very good partial response (VGPR) | 165 (46.5%) | 168 (47.5%) |
| Partial response (PR) | 15 (4.2%) | 35 (9.9%) |
| CR or better (sCR+CR), n (%) | 158 (44.5%) | 123 (34.7%) |
| 95% CI (%) Exact 95% confidence interval | (39.3%, 49.9%) | (29.8%, 40.0%) |
| MRD negativity rate , Based on threshold of 10 -5 using a next-generation sequencing assay (clonoSEQ) , Patients achieved both MRD negativity (threshold of 10 -5 ) and response of CR or better , n (%) | 204 (57.5%) | 115 (32.5%) |
| 95% CI (%) | (52.1%, 62.7%) | (27.6%, 37.6%) |
| MRD negativity rate in patients with CR or better , Based on patients with CR or better response by the end of consolidation | ||
| Number of patients with CR or better | n=158 | n=123 |
| MRD negativity rate n (%) | 121 (76.6%) | 72 (58.5%) |
| 95% CI (%) | (69.2%, 82.9%) | (49.3%, 67.3%) |
In Combination with Bortezomib, Lenalidomide and Dexamethasone in Patients Who Are Ineligible for ASCT
The efficacy of DARZALEX FASPRO with bortezomib, lenalidomide and dexamethasone (DARZALEX FASPRO-VRd) versus bortezomib, lenalidomide and dexamethasone (VRd) was evaluated in CEPHEUS (NCT03652064), an open-label, randomized, active-controlled trial in patients with newly diagnosed multiple myeloma who were ineligible for ASCT or refused ASCT as initial therapy.
Patients received DARZALEX FASPRO 1,800 mg/30,000 units administered subcutaneously once weekly from weeks 1 to 6, once every three weeks from weeks 7 to 24, and once every 4 weeks starting with week 25 until disease progression or unacceptable toxicity. Bortezomib was administered by subcutaneous injection at a dose of 1.3 mg/m 2 body surface area twice weekly (days 1, 4, 8, and 11) in repeated 21-day (3-week) cycles from Cycles 1–8. Lenalidomide was administered orally at 25 mg daily on Days 1–14 of Cycles 1–8 and on Days 1–21 during Cycles 9 and beyond. Dexamethasone was administered orally at 20 mg on Days 1, 2, 4, 5, 8, 9, 11, and 12 of Cycles 1–8 (or at 20 mg on Days 1, 4, 8, and 11 for patients >75 years or BMI <18.5) and at 40 mg on Days 1, 8, 15, and 22 during Cycles 9 and beyond (or at a reduced dose of 20 mg per week for patients >75 years or BMI <18.5). On the days of DARZALEX FASPRO injection, the dexamethasone dose was administered orally or intravenously as a pre-injection medication.
The effectiveness of DARZALEX FASPRO-VRd has not been established in patients who refused ASCT as initial therapy.
The major efficacy outcome measures were overall minimal residual disease (MRD) negativity rate and progression-free survival (PFS) by independent review committee (IRC) based on IMWG response criteria.
A total of 395 patients were randomized: 197 to the DARZALEX FASPRO-VRd arm and 198 to the VRd arm. The median age was 70 years (range: 31 to 80); 50% were male and 81% were White, 5% were Black or African American, and 6% were Asian. Thirty-four percent had ISS Stage I, 38% had ISS Stage II, and 28% had ISS Stage III disease. High-risk cytogenetics (presence of del(17p), t(4;14), t(14,16)) were present in 13% of patients.
The trial demonstrated a statistically significant improvement in overall MRD negativity rate, PFS, CR or better rate, and sustained MRD negativity rate, as shown in Table 29 and Figure 2.
| DARZALEX FASPRO-VRd (N=197) | VRd (N=198) | |
|---|---|---|
| VRd=bortezomib-lenalidomide-dexamethasone; PFS=progression-free survival; MRD=minimal residual disease; CI=confidence interval; NR = not reached; NE = not evaluable. | ||
| PFS based on IRC Interim analysis: Median follow-up of 39 months (cut-off date 08 September 2022). | ||
| Number of events, n (%) | 46 (23.4%) | 68 (34.3%) |
| Median, months with 95% CI | NR (NE, NE) | NR (NE, NE) |
| Hazard ratio with 95% CI Hazard ratio and 95% CI from a Cox proportional hazards model with treatment as the sole explanatory variable and stratified with ISS staging (I, II, III), and age/transplant eligibility (<70 years ineligible, or <70 years and refusal to transplant, or ≥70 years) as randomized. A hazard ratio <1 indicates an advantage for D-VRd. | 0.60 (0.41, 0.88) | |
| p-value p-value is based on the log-rank test stratified with ISS staging (I, II, III), and age/transplant eligibility (<70 years ineligible, or <70 years and refusal to transplant, or ≥70 years) as randomized. | 0.0078 | |
| MRD negativity rate n (%) Primary analysis: Median follow-up of 22 months (cut-off date 08 April 2021). , Patients achieved both MRD negativity (threshold of 10 -5 ) and CR or better. All MRD testing was performed with a next-generation sequencing assay (clonoSEQ). | 103 (52.3%) | 69 (34.8%) |
| p-value p-value from Cochran Mantel-Haenszel Chi-Squared test. | 0.0005 | |
| Overall CR or better (sCR+CR) n (%) | 150 (76.1%) | 116 (58.6%) |
| p-value | 0.0002 | |
| MRD negativity rate in patients with CR or better , Patients achieving MRD negativity (threshold of 10 -5 ) among only patients achieving a response of CR or better. | ||
| Number of patients with CR or better | n=150 | n=116 |
| MRD negativity rate n (%) | 103 (68.7%) | 69 (59.5%) |
| 95% CI (%) Exact 95% confidence interval. | (60.6%, 76.0%) | (50.0%, 68.5%) |
| Sustained MRD negativity rate n (%) , Sustained MRD negativity is defined as confirmed MRD negative status at two examinations at least 1 year apart without MRD positive status in between. | 84 (42.6%) | 50 (25.3%) |
| p-value p-value from Fisher's exact test. | 0.0003 | |
| Overall response (sCR+CR+VGPR+PR) n(%) Final analysis: Median follow-up of 59 months (cut-off date 07 May 2024). | 191 (97.0%) | 185 (93.4%) |
| Stringent Complete Response (sCR) | 128 (65.0%) | 89 (44.9%) |
| Complete response (CR) | 32 (16.2%) | 33 (16.7%) |
| Very good partial response (VGPR) | 23 (11.7%) | 49 (24.7%) |
| Partial response (PR) | 8 (4.1%) | 14 (7.1%) |
| Figure 2: Kaplan-Meier Curve of PFS in CEPHEUS PFS median follow-up of 39 months |
|---|
 |
In Combination with Bortezomib, Melphalan and Prednisone in Patients Ineligible for Autologous Stem Cell Transplant
The efficacy of DARZALEX FASPRO with bortezomib, melphalan and prednisone was evaluated in a single-arm cohort of PLEIADES (NCT03412565), a multi-cohort, open-label trial. Eligible patients were required to have newly diagnosed multiple myeloma who are ineligible for transplant. Patients received DARZALEX FASPRO 1,800 mg/30,000 units administered subcutaneously once weekly from weeks 1 to 6, once every 3 weeks from weeks 7 to 54 and once every 4 weeks starting with week 55 until disease progression or unacceptable toxicity; bortezomib 1.3 mg/m 2 subcutaneously twice weekly on Weeks 1, 2, 4 and 5 for the first 6-week cycle (Cycle 1; 8 doses), followed by once weekly on Weeks 1, 2, 4 and 5 for eight more 6-week cycles (Cycles 2–9; 4 doses per cycle); and melphalan 9 mg/m 2 and prednisone 60 mg/m 2 orally on Days 1 to 4 of the nine 6-week cycles (Cycles 1–9). The major efficacy outcome measure was overall response rate (ORR).
A total of 67 patients received DARZALEX FASPRO with VMP. The median age was 75 years (range: 66 to 86 years); 46% were male; 69% were White, 8% Asian, and 2% Black or African American; and 33% had ISS Stage I, 45% had ISS Stage II, and 22% had ISS Stage III disease.
Efficacy results are summarized in Table 30. The median duration of follow-up for patients was 6.9 months.
| DARZALEX FASPRO-VMP (N=67) | |
|---|---|
| CI=confidence interval | |
| Overall response rate (sCR+CR+VGPR+PR), n (%) Based on treated patients | 59 (88%) |
| 95% CI (%) | (78%, 95%) |
| Stringent complete response (sCR) | 5 (8%) |
| Complete response (CR) | 7 (10%) |
| Very good partial response (VGPR) | 31 (46%) |
| Partial response (PR) | 16 (24%) |
Relapsed/Refractory Multiple Myeloma
In Combination with Lenalidomide and Dexamethasone
The efficacy of DARZALEX FASPRO with lenalidomide and dexamethasone (DARZALEX FASPRO-Rd) was evaluated in a single-arm cohort of PLEIADES (NCT03412565), a multi-cohort, open-label trial. Patients received DARZALEX FASPRO 1,800 mg/30,000 units administered subcutaneously once weekly from weeks 1 to 8, once every 2 weeks from weeks 9 to 24 and once every 4 weeks starting with week 25 until disease progression or unacceptable toxicity with lenalidomide 25 mg once daily orally on Days 1–21 of each 28-day cycle; and dexamethasone 40 mg per week (or a reduced dose of 20 mg per week for patients >75 years or BMI <18.5). The major efficacy outcome measure was ORR.
A total of 65 patients received DARZALEX FASPRO with Rd. The median age was 69 years (range: 33 to 82 years); 69% were male; 69% were White, and 3% Black or African American; and 42% had ISS Stage I, 30% had ISS Stage II, and 28% had ISS Stage III disease. Patients had received a median of 1 prior line of therapy. A total of 52% of patients had a prior ASCT; 95% of patients received a prior PI; 59% received a prior immunomodulatory agent, including 22% who received prior lenalidomide; and 54% of patients received both a prior PI and immunomodulatory agent.
Efficacy results are summarized in Table 31. The median duration of follow-up for patients was 7.1 months.
| DARZALEX FASPRO-Rd (N=65) | |
|---|---|
| CI=confidence interval | |
| Overall response rate (sCR+CR+VGPR+PR), n (%) Based on treated patients | 59 (91%) |
| 95% CI (%) | (81%, 97%) |
| Stringent complete response (sCR) | 4 (6%) |
| Complete response (CR) | 8 (12%) |
| Very good partial response (VGPR) | 30 (46%) |
| Partial response (PR) | 17 (26%) |
In Combination with Pomalidomide and Dexamethasone
The efficacy of DARZALEX FASPRO with pomalidomide and dexamethasone (DARZALEX FASPRO-Pd) versus pomalidomide and dexamethasone (Pd) alone was evaluated in APOLLO (NCT03180736), an open-label, randomized, active-controlled trial. Patients received DARZALEX FASPRO 1,800 mg/30,000 units administered subcutaneously once weekly from weeks 1 to 8, once every 2 weeks from weeks 9 to 24 and once every 4 weeks starting with week 25 until disease progression or unacceptable toxicity with pomalidomide 4 mg once daily orally on Days 1–21 of each 28-day cycle; and dexamethasone 40 mg per week (or a reduced dose of 20 mg per week for patients >75 years). The major efficacy outcome measure was progression-free survival (PFS).
A total of 304 patients were randomized: 151 to the DARZALEX FASPRO-Pd arm and 153 to the Pd arm. The median age was 67 years (range: 35 to 90); 53% were male and 89% were White, <1% were Black or African American, and <1% were Asian, and 45% had ISS Stage I, 33% had ISS Stage II, and 22% had ISS Stage III disease. Patients had received a median of 2 prior lines of therapy (range 1–5), with 11% of patients having received 1 prior line of therapy and 75% of patients having received 2–3 prior lines of therapy. All patients received a prior treatment with a PI and lenalidomide, and 56% of patients received prior ASCT. The majority of patients were refractory to lenalidomide (80%), a PI (48%), or both an immunomodulatory agent and a PI (42%).
APOLLO demonstrated an improvement in PFS in the DARZALEX FASPRO-Pd treatment group as compared to the Pd treatment group; the median PFS was 12.4 months in the DARZALEX FASPRO-Pd treatment group and 6.9 months in the Pd treatment group (HR [95% CI]: 0.63 [0.47, 0.85]; p-value = 0.0018), representing a 37% reduction in the risk of disease progression or death for patients treated with DARZALEX FASPRO-Pd versus Pd.
Figure 3: Kaplan-Meier Curve of PFS in APOLLO
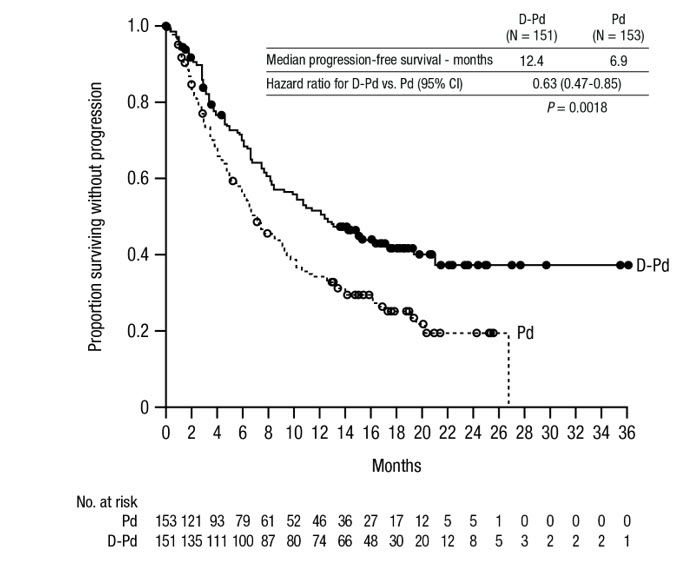
Additional efficacy results from APOLLO are presented in Table 32.
| DARZALEX FASPRO-Pd (n=151) | Pd (n=153) | |
|---|---|---|
| Pd=pomalidomide-dexamethasone; MRD=minimal residual disease; CI=confidence interval | ||
| Overall response (sCR+CR+VGPR+PR) n (%) | 104 (68.9%) | 71 (46.4%) |
| P-value p-value from Cochran Mantel-Haenszel Chi-Squared test adjusted for stratification factors | <0.0001 | |
| Stringent complete response (sCR) | 14 (9.3%) | 2 (1.3%) |
| Complete response (CR) | 23 (15.2%) | 4 (2.6%) |
| Very good partial response (VGPR) | 40 (26.5%) | 24 (15.7%) |
| Partial response (PR) | 27 (17.9%) | 41 (26.8%) |
| MRD negativity rate Based on the intent-to-treat population , Based on threshold of 10 -5 using a next-generation sequencing assay (clonoSEQ). n (%) | 13 (8.6%) | 3 (2.0%) |
| 95% CI (%) | (4.7%, 14.3%) | (0.4%, 5.6%) |
| P-value p-value from Fisher's exact test. | 0.0102 | |
| MRD negativity rate in patients with CR or better | ||
| Number of patients with CR or better | N=37 | N=6 |
| MRD negativity rate n (%) | 13 (35.1%) | 3 (50.0%) |
| 95% CI (%) | (20.2%, 52.5%) | (11.8%, 88.2%) |
In responders, the median time to response was 1 month (range: 0.9 to 9.1 months) in the DARZALEX FASPRO-Pd group and 1.9 months (range: 0.9 to 17.3 months) in the Pd group. The median duration of response had not been reached in the DARZALEX FASPRO-Pd group (range: 1 to 34.9+ months) and was 15.9 months (range: 1+ to 24.8 months) in the Pd group.
With a median follow-up of 16.9 months, 99 deaths were observed; 48 in the DARZALEX FASPRO-Pd group and 51 in the Pd group. Median OS was not reached for either treatment group.
In Combination with Carfilzomib and Dexamethasone
The efficacy of DARZALEX FASPRO with carfilzomib and dexamethasone (DARZALEX FASPRO-Kd) was evaluated in a single-arm cohort of PLEIADES (NCT03412565), a multi-cohort, open-label trial. This cohort enrolled patients with relapsed or refractory multiple myeloma excluding patients with left ventricular ejection fraction (LVEF) less than 40%, myocardial infarction within 6 months, uncontrolled cardiac arrhythmia, or uncontrolled hypertension (systolic blood pressure >159 mmHg or diastolic >99 mmHg despite optimal treatment). Patients received DARZALEX FASPRO 1,800 mg/30,000 units administered subcutaneously once weekly from Weeks 1 to 8, once every 2 weeks from Weeks 9 to 24 and once every 4 weeks starting with Week 25 until disease progression or unacceptable toxicity with carfilzomib administered by IV infusion at a dose of 20 mg/m 2 on Cycle 1 Day 1 and if a dose of 20 mg/m 2 was tolerated, carfilzomib was administered at a dose of 70 mg/m 2 as a 30-minute IV infusion, on Cycle 1 Day 8 and Day 15, and then Day 1, 8 and 15 of each cycle and dexamethasone 40 mg per week (or a reduced dose of 20 mg per week for patients ≥75 years or BMI <18.5). The major efficacy outcome measure was ORR.
A total of 66 patients received DARZALEX FASPRO with Kd. The median age was 61 years (range: 42 to 84); 52% were male; 73% were White and 3% Black or African American; and 68% had ISS Stage I, 18% had ISS Stage II, and 14% had ISS Stage III disease. A total of 79% of patients had a prior ASCT; 91% of patients received a prior PI. All patients received 1 prior line of therapy with exposure to lenalidomide and 62% of patients were refractory to lenalidomide.
Efficacy results are summarized in Table 33. At a median follow-up of 9.2 months, the median duration of response had not been reached and an estimated 85.2% (95% CI: 72.5, 92.3) maintained response for at least 6 months and 82.5% (95% CI: 68.9, 90.6) maintained response for at least 9 months.
| DARZALEX FASPRO-Kd (N=66) | |
|---|---|
| CI=confidence interval | |
| Overall response rate (sCR+CR+VGPR+PR), n (%) Based on treated patients | 56 (84.8%) |
| 95% CI (%) | (73.9%, 92.5%) |
| Stringent complete response (sCR) | 11 (16.7%) |
| Complete response (CR) | 14 (21.2%) |
| Very good partial response (VGPR) | 26 (39.4%) |
| Partial response (PR) | 5 (7.6%) |
Monotherapy
The efficacy of DARZALEX FASPRO as monotherapy was evaluated in COLUMBA (NCT03277105), an open-label, randomized, non-inferiority study. Eligible patients were required to have relapsed or refractory multiple myeloma who had received at least 3 prior lines of therapy including a proteasome inhibitor and an immunomodulatory agent or who were double-refractory to a proteasome inhibitor and an immunomodulatory agent. Patients were randomized to receive DARZALEX FASPRO 1,800 mg/30,000 units administered subcutaneously or daratumumab 16 mg/kg administered intravenously; each administered once weekly from weeks 1 to 8, once every 2 weeks from weeks 9 to 24 and once every 4 weeks starting with week 25 until unacceptable toxicity or disease progression. The major efficacy outcome measures were ORR by the IMWG response criteria and maximum C trough at pre-dose Cycle 3 Day 1 [see Clinical Pharmacology (12.3) ] . Randomization was stratified by body weight, myeloma type, and number of prior lines of therapy.
A total of 522 patients were randomized: 263 to the DARZALEX FASPRO arm and 259 to the intravenous daratumumab arm. The median age was 67 years (range: 33 to 92 years); 55% were male; and 78% were White, 14% Asian, and 3% Black or African American. The median weight was 73 kg (range: 29 to 138). Patients had received a median of 4 prior lines of therapy. A total of 51% of patients had a prior ASCT; 100% of patients received both a PI and an immunomodulatory agent. Forty-nine percent of patients were refractory both a PI and an immunomodulatory agent. Eighty-two percent of patients were refractory to their last line of prior systemic therapy.
The results show that DARZALEX FASPRO 1,800 mg/30,000 units administered subcutaneously is non-inferior to daratumumab 16 mg/kg administered intravenously in terms of ORR and maximum trough concentration [see Clinical Pharmacology (12.3) ] . Median progression-free survival was 5.6 months in the DARZALEX FASPRO arm and 6.1 months in the intravenous daratumumab arm. ORR results are provided in Table 34.
| DARZALEX FASPRO (N=263) | Intravenous Daratumumab (N=259) | |
|---|---|---|
| Overall response (sCR+CR+VGPR+PR), n (%) Based on intent-to-treat population. | 108 (41%) | 96 (37%) |
| 95% CI (%) | (35%, 47%) | (31%, 43%) |
| Ratio of response rates (95% CI) | 1.11 (0.89, 1.37) | |
| CR or better, n (%) | 5 (1.9%) | 7 (2.7%) |
| Very good partial response (VGPR) | 45 (17%) | 37 (14%) |
| Partial response (PR) | 58 (22%) | 52 (20%) |
High-Risk Smoldering Multiple Myeloma
Monotherapy
The efficacy of DARZALEX FASPRO as monotherapy versus active monitoring was evaluated in AQUILA (NCT03301220), an open-label, randomized trial in patients with high-risk smoldering multiple myeloma.
Patients randomized to the treatment arm received DARZALEX FASPRO 1,800 mg/30,000 units administered subcutaneously once weekly from weeks 1 to 8, once every 2 weeks from weeks 9 to 24 and once every 4 weeks starting with week 25 until 39 cycles or up to 36 months or until diagnosis to multiple myeloma or unacceptable toxicity.
The major efficacy outcome measure was progression-free survival (PFS) by independent review committee (IRC) as defined as the diagnosis of multiple myeloma based on the IMWG diagnostic criteria for multiple myeloma or death.
A total of 390 patients were randomized: 194 to the DARZALEX FASPRO arm and 196 to the active monitoring arm. The median age was 64 years (range: 31 to 86); 12% were ≥75 years; 48% were male; 83% White, 8% Asian, and 3% were Black or African American. Forty-one percent of patients had 2 or more of the following criteria for high-risk smoldering multiple myeloma: serum monoclonal protein level >2 g/dL, involved-to-uninvolved serum-free light chain ratio >20, and bone marrow plasma cells >20%. DARZALEX FASPRO is only indicated for patients with high-risk smoldering multiple myeloma. It is not indicated for other risk categories.
PFS results are shown in Figure 4.
Figure 4: Kaplan-Meier Curve of PFS in AQUILA
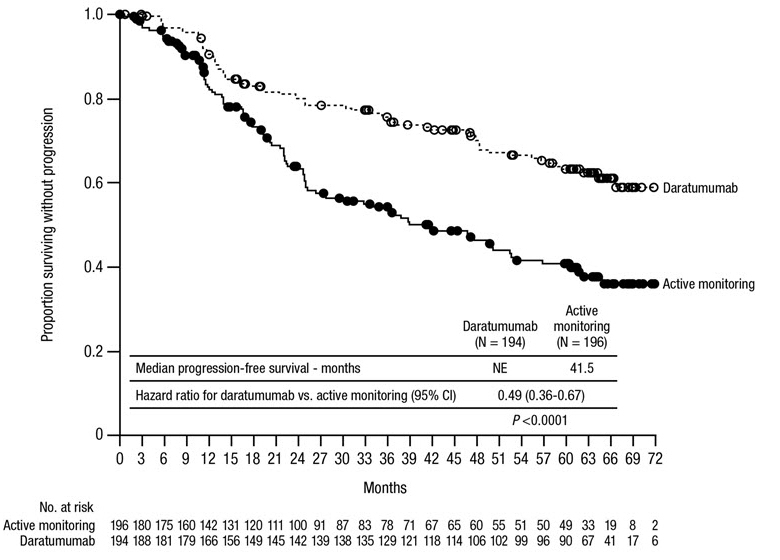
Additional efficacy results from AQUILA are presented in Table 35.
| DARZALEX FASPRO (n=194) | Active Monitoring (n=196) | |
|---|---|---|
| Overall response (sCR+CR+VGPR+PR), n (%) | 123 (63.4%) | 2 (1.0%) |
| Stringent complete response (sCR) | 7 (3.6%) | 0 |
| Complete response (CR) | 10 (5.2%) | 0 |
| Very good partial response (VGPR) | 41 (21.1%) | 1 (0.5%) |
| Partial response (PR) | 65 (33.5%) | 1 (0.5%) |
Light Chain Amyloidosis
In Combination with Bortezomib, Cyclophosphamide and Dexamethasone
The efficacy of DARZALEX FASPRO with VCd was evaluated in ANDROMEDA (NCT03201965), an open-label, randomized, active-controlled trial. Eligible patients were required to have newly diagnosed light chain (AL) amyloidosis with at least one affected organ, measurable hematologic disease, Cardiac Stage I–IIIA (based on European Modification of Mayo 2004 Cardiac Stage), and NYHA Class I–IIIA. Patients with NYHA Class IIIB and IV were excluded. Patients were randomized to receive bortezomib 1.3 mg/m 2 administered subcutaneously, cyclophosphamide 300 mg/m 2 (max dose 500 mg) administered orally or intravenously, and dexamethasone 40 mg (or a reduced dose of 20 mg for patients >70 years or body mass index <18.5 or who have hypervolemia, poorly controlled diabetes mellitus or prior intolerance to steroid therapy) administered orally or intravenously on Days 1, 8, 15, and 22 of each 28-day cycle with or without DARZALEX FASPRO 1,800 mg/30,000 units subcutaneously once weekly from weeks 1 to 8, once every 2 weeks from weeks 9 to 24 and once every 4 weeks starting with week 25 until disease progression or a maximum of two years. When DARZALEX FASPRO and dexamethasone were administered on the same day, dexamethasone 20 mg was administered before DARZALEX FASPRO with the remaining dose of dexamethasone administered after DARZALEX FASPRO if applicable. The major efficacy outcome measure was confirmed hematologic complete response (HemCR) rate based on Consensus Criteria as determined by the Independent Review Committee (negative serum and urine immunofixation, involved free light chain level decrease to less than the upper limit of normal, and normal free light chain ratio). Randomization was stratified by Cardiac Stage (European Modification of Mayo 2004 Cardiac Stage) countries that typically offer autologous stem cell transplant (ASCT) for patients with light chain (AL) amyloidosis, and renal function.
A total of 388 patients were randomized: 195 to DARZALEX FASPRO-VCd and 193 to VCd. The median patient age was 64 years (range: 34 to 87 years); 58% were male; 76% White, 17% Asian, and 3% Black or African American; 23% had light chain (AL) amyloidosis Cardiac Stage I, 40% had Stage II, and 37% had Stage IIIA. The median number of organs involved was 2 (range: 1–6) and 66% of patients had 2 or more organs involved. Vital organ involvement was: cardiac 71%, renal 59% and hepatic 8%. The majority (79%) of patients had lambda free light chain disease.
Efficacy results are summarized in Table 36.
| DARZALEX FASPRO-VCd (n=195) | VCd (n=193) | |
|---|---|---|
| VCd=bortezomib-cyclophosphamide-dexamethasone | ||
| Hematologic complete response (HemCR), n (%) | 82 (42%) | 26 (13%) |
| p-value p-value from Cochran Mantel-Haenszel Chi-Squared test. | <0.0001 | |
| Very good partial response (VGPR), n (%) | 71 (36%) | 69 (36%) |
| Partial response (PR), n (%) | 26 (13%) | 53 (27%) |
| Hematologic VGPR or better (HemCR + VGPR), n (%) | 153 (78%) | 95 (49%) |
| Major organ deterioration progression-free survival Major organ deterioration-PFS defined as hematologic progression, major organ (cardiac or renal) deterioration or death , Hazard ratio with 95% CI | 0.58 (0.37, 0.92) | |
The median time to HemCR was 59 days (range: 8 to 299 days) in the DARZALEX FASPRO-VCd arm and 59 days (range: 16 to 340 days) in the VCd arm. The median time to VGPR or better was 17 days (range: 5 to 336 days) in the DARZALEX FASPRO-VCd arm and 25 days (range: 8 to 171 days) in the VCd arm. The median duration of HemCR had not been reached in either arm.
After a median follow-up of 61.4 months, ANDROMEDA demonstrated an improvement in major organ deterioration progression free survival (MOD-PFS) in the DARZALEX FASPRO-VCd arm as compared to the VCd arm (HR=0.47; 95% CI: 0.33, 0.67; p<0.0001), representing a 53% reduction in the risk of hematologic progression, major organ deterioration, or death in patients treated in the DARZALEX FASPRO-VCd arm. The median MOD-PFS was not reached in the DARZALEX FASPRO-VCd arm and was 30.2 months in the VCd arm.
Figure 5: Kaplan-Meier Curve of MOD-PFS in ANDROMEDA
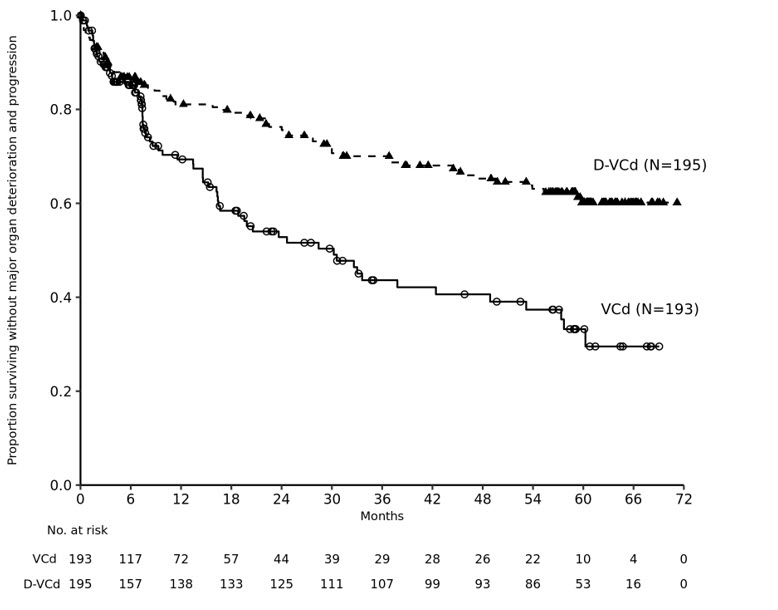
After a median follow-up of 61.4 months, ANDROMEDA demonstrated an improvement in overall survival (OS) in the DARZALEX FASPRO-VCd arm as compared to the VCd arm (HR=0.62; 95% CI: 0.42, 0.90; p=0.0121), representing a 38% reduction in the risk of death in patients treated in the DARZALEX FASPRO-VCd arm. The median OS had not been reached in either arm.
Figure 6: Kaplan-Meier Curve of OS in ANDROMEDA
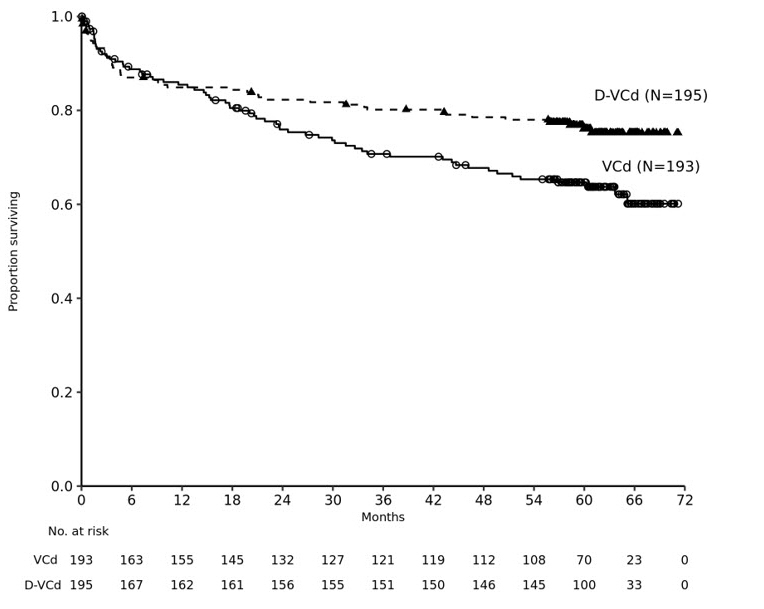
HOW SUPPLIED/STORAGE AND HANDLING
DARZALEX FASPRO ® (daratumumab and hyaluronidase-fihj) injection is a sterile, preservative-free, colorless to yellow, and clear to opalescent solution for subcutaneous use supplied as individually packaged single-dose vials providing 1,800 mg of daratumumab and 30,000 units of hyaluronidase per 15 mL (NDC 57894-503-01).
Store DARZALEX FASPRO vials in a refrigerator at 2ºC to 8ºC (36ºF to 46ºF) in the original carton to protect from light.
Do not freeze or shake.
Mechanism of Action
CD38 is a transmembrane glycoprotein (48 kDa) expressed on the surface of hematopoietic cells, including clonal plasma cells in multiple myeloma and light chain (AL) amyloidosis, as well as other cell types. Surface CD38 has multiple functions, including receptor mediated adhesion, signaling, and modulation of cyclase and hydrolase activity. Daratumumab is an IgG1κ human monoclonal antibody (mAb) that binds to CD38 and inhibits the growth of CD38 expressing tumor cells by inducing apoptosis directly through Fc mediated cross linking as well as by immune-mediated tumor cell lysis through complement dependent cytotoxicity (CDC), antibody dependent cell mediated cytotoxicity (ADCC) and antibody dependent cellular phagocytosis (ADCP). A subset of myeloid derived suppressor cells (CD38+MDSCs), regulatory T cells (CD38+T regs ) and B cells (CD38+B regs ) are decreased by daratumumab.
Hyaluronan is a polysaccharide found in the extracellular matrix of the subcutaneous tissue. It is depolymerized by the naturally occurring enzyme hyaluronidase. Unlike the stable structural components of the interstitial matrix, hyaluronan has a half-life of approximately 0.5 days. Hyaluronidase increases permeability of the subcutaneous tissue by depolymerizing hyaluronan. In the doses administered, hyaluronidase in DARZALEX FASPRO acts locally. The effects of hyaluronidase are reversible and permeability of the subcutaneous tissue is restored within 24 to 48 hours.