Norditropin prior authorization resources
Most recent state uniform prior authorization forms
Brand Resources
Norditropin patient education
Patient toolkit
Dosage & administration
DOSAGE AND ADMINISTRATION
- Administer by subcutaneous injection to the back of upper arm, abdomen, buttock, or thigh with regular rotation of injection sites (2.1 )
- Pediatric Dosage - divide the calculated weekly dosage into equal doses given either 6, or 7 days per week
- Adult Dosage: Either of the following two dosing regimens may be used:
- Non-weight based dosing: Initiate with a dose of approximately 0.2 mg/day (range, 0.15 mg/day-0.3 mg/day) and increase the dose every 1-2 months by increments of approximately 0.1 mg/day-0.2 mg/day, according to individual patient requirements (2.3 )
- Weight-based dosing (Not recommended for obese patients): Initiate at 0.004 mg/kg daily and increase the dose according to individual patient requirements to a maximum of 0.016 mg/kg daily (2.3 )
Administration and Use Instructions
- Therapy with NORDITROPIN should be supervised by a physician who is experienced in the diagnosis and management of patients with the conditions for which NORDITROPIN is indicated [see Indications and Usage (1) ].
- Fundoscopic examination should be performed routinely before initiating treatment with NORDITROPIN to exclude preexisting papilledema, and periodically thereafter [see Warnings and Precautions (5.5) ].
- Administer NORDITROPIN by subcutaneous injection to the back of the upper arm, abdomen, buttocks, or thigh with regular rotation of injection sites to avoid lipoatrophy.
- Inspect visually for particulate matter and discoloration. NORDITROPIN should be clear and colorless. If the solution is cloudy or contains particulate matter do not use.
- Instructions for delivering the dosage are provided in the PATIENT INFORMATION and INSTRUCTIONS FOR USE leaflets enclosed with the NORDITROPIN FlexPro prefilled pen.
Pediatric Dosage
- Individualize dosage for each patient based on the growth response.
- Divide the calculated weekly NORDITROPIN dosage into equal doses given either 6, or 7 days per week.
- The recommended weekly dose in milligrams (mg) per kilogram (kg) of body weight for pediatric patients is:
- Pediatric GH Deficiency: 0.17 mg/kg/week to 0.24 mg/kg/week (0.024 to 0.034 mg/kg/day)
- Noonan Syndrome: Up to 0.46 mg/kg/week (up to 0.066 mg/kg/day)
- Turner Syndrome: Up to 0.47 mg/kg/week (up to 0.067 mg/kg/day)
- Small for Gestational Age (SGA): Up to 0.47 mg/kg/week (up to 0.067 mg/kg/day)
- In very short pediatric patients, HSDS less than -3, and older pubertal pediatric patients consider initiating treatment with a larger dose of NORDITROPIN (up to 0.067 mg/kg/day). Consider a gradual reduction in dosage if substantial catch-up growth is observed during the first few years of therapy. In pediatric patients less than 4 years of age with less severe short stature, baseline HSDS values between -2 and -3, consider initiating treatment at 0.033 mg/kg/day and titrate the dose as needed.
- Idiopathic Short Stature: Up to 0.47 mg/kg/week (up to 0.067 mg/kg/day)
- Prader-Willi Syndrome: 0.24 mg/kg/week (0.034 mg/kg/day)
- Assess compliance and evaluate other causes of poor growth such as hypothyroidism, under-nutrition, advanced bone age and antibodies to recombinant human growth hormone if patients experience failure to increase height velocity, particularly during the first year of treatment.
- Discontinue NORDITROPIN for stimulation of linear growth once epiphyseal fusion has occurred [see Contraindications (4) ].
Adult Dosage
- Patients who were treated with somatropin for GH deficiency in childhood and whose epiphyses are closed should be reevaluated before continuation of somatropin for GH deficient adults.
- Consider using a lower starting dose and smaller dose increment increases for geriatric patients as they may be at increased risk for adverse reactions with NORDITROPIN than younger individuals [see Use in Specific Populations (8.5) ].
- Estrogen-replete women and patients receiving oral estrogen may require higher doses [see Drug Interactions (7) ].
- Administer the prescribed dose daily.
- Either of two NORDITROPIN dosing regimens may be used:
- Non-weight based
- Initiate NORDITROPIN with a dose of approximately 0.2 mg/day (range, 0.15 mg/day to 0.3 mg/day) and increase the dose every 1-2 months by increments of approximately 0.1 mg/day to 0.2 mg/day, according to individual patient requirements based on the clinical response and serum insulin-like growth factor 1 (IGF-1) concentrations.
- Decrease the dose as necessary on the basis of adverse reactions and/or serum IGF-1 concentrations above the age- and gender-specific normal range.
- Maintenance dosages will vary considerably from person to person, and between male and female patients.
- Weight-based
- Initiate NORDITROPIN at 0.004 mg/kg daily and increase the dose according to individual patient requirements to a maximum of 0.016 mg/kg daily.
- Use the patient’s clinical response, adverse reactions, and determination of age- and gender-adjusted serum IGF-1 concentrations as guidance in dose titration.
- Not recommended for obese patients as they are more likely to experience adverse reactions with this regimen

By using PrescriberAI, you agree to the AI Terms of Use.
Norditropin prescribing information
Warnings and Precautions, Slipped Capital Femoral Epiphysis in Pediatric Patients (5.10 )…..07/2025
INDICATIONS AND USAGE
NORDITROPIN is a recombinant human growth hormone indicated for:
- Pediatric : Treatment of pediatric patients with growth failure due to inadequate secretion of endogenous growth hormone (GH), short stature associated with Noonan syndrome, short stature associated with Turner syndrome, short stature born small for gestational age (SGA) with no catch-up growth by age 2 to 4 years, Idiopathic Short Stature (ISS), and growth failure due to Prader-Willi Syndrome (1.1 )
- Adult : Replacement of endogenous GH in adults with growth hormone deficiency (1.2 )
Pediatric Patients
NORDITROPIN is indicated for the treatment of pediatric patients with:
- growth failure due to inadequate secretion of endogenous growth hormone (GH),
- short stature associated with Noonan syndrome,
- short stature associated with Turner syndrome,
- short stature born small for gestational age (SGA) with no catch-up growth by age 2 years to 4 years of age,
- Idiopathic Short Stature (ISS), height standard deviation score (SDS) <-2.25, and associated with growth rates unlikely to permit attainment of adult height in the normal range,
- growth failure due to Prader-Willi syndrome (PWS).
Adult Patients
NORDITROPIN is indicated for the replacement of endogenous GH in adults with growth hormone deficiency (GHD)
DOSAGE AND ADMINISTRATION
- Administer by subcutaneous injection to the back of upper arm, abdomen, buttock, or thigh with regular rotation of injection sites (2.1 )
- Pediatric Dosage - divide the calculated weekly dosage into equal doses given either 6, or 7 days per week
- Adult Dosage: Either of the following two dosing regimens may be used:
- Non-weight based dosing: Initiate with a dose of approximately 0.2 mg/day (range, 0.15 mg/day-0.3 mg/day) and increase the dose every 1-2 months by increments of approximately 0.1 mg/day-0.2 mg/day, according to individual patient requirements (2.3 )
- Weight-based dosing (Not recommended for obese patients): Initiate at 0.004 mg/kg daily and increase the dose according to individual patient requirements to a maximum of 0.016 mg/kg daily (2.3 )
Administration and Use Instructions
- Therapy with NORDITROPIN should be supervised by a physician who is experienced in the diagnosis and management of patients with the conditions for which NORDITROPIN is indicated [see Indications and Usage (1) ].
- Fundoscopic examination should be performed routinely before initiating treatment with NORDITROPIN to exclude preexisting papilledema, and periodically thereafter [see Warnings and Precautions (5.5) ].
- Administer NORDITROPIN by subcutaneous injection to the back of the upper arm, abdomen, buttocks, or thigh with regular rotation of injection sites to avoid lipoatrophy.
- Inspect visually for particulate matter and discoloration. NORDITROPIN should be clear and colorless. If the solution is cloudy or contains particulate matter do not use.
- Instructions for delivering the dosage are provided in the PATIENT INFORMATION and INSTRUCTIONS FOR USE leaflets enclosed with the NORDITROPIN FlexPro prefilled pen.
Pediatric Dosage
- Individualize dosage for each patient based on the growth response.
- Divide the calculated weekly NORDITROPIN dosage into equal doses given either 6, or 7 days per week.
- The recommended weekly dose in milligrams (mg) per kilogram (kg) of body weight for pediatric patients is:
- Pediatric GH Deficiency: 0.17 mg/kg/week to 0.24 mg/kg/week (0.024 to 0.034 mg/kg/day)
- Noonan Syndrome: Up to 0.46 mg/kg/week (up to 0.066 mg/kg/day)
- Turner Syndrome: Up to 0.47 mg/kg/week (up to 0.067 mg/kg/day)
- Small for Gestational Age (SGA): Up to 0.47 mg/kg/week (up to 0.067 mg/kg/day)
- In very short pediatric patients, HSDS less than -3, and older pubertal pediatric patients consider initiating treatment with a larger dose of NORDITROPIN (up to 0.067 mg/kg/day). Consider a gradual reduction in dosage if substantial catch-up growth is observed during the first few years of therapy. In pediatric patients less than 4 years of age with less severe short stature, baseline HSDS values between -2 and -3, consider initiating treatment at 0.033 mg/kg/day and titrate the dose as needed.
- Idiopathic Short Stature: Up to 0.47 mg/kg/week (up to 0.067 mg/kg/day)
- Prader-Willi Syndrome: 0.24 mg/kg/week (0.034 mg/kg/day)
- Assess compliance and evaluate other causes of poor growth such as hypothyroidism, under-nutrition, advanced bone age and antibodies to recombinant human growth hormone if patients experience failure to increase height velocity, particularly during the first year of treatment.
- Discontinue NORDITROPIN for stimulation of linear growth once epiphyseal fusion has occurred [see Contraindications (4) ].
Adult Dosage
- Patients who were treated with somatropin for GH deficiency in childhood and whose epiphyses are closed should be reevaluated before continuation of somatropin for GH deficient adults.
- Consider using a lower starting dose and smaller dose increment increases for geriatric patients as they may be at increased risk for adverse reactions with NORDITROPIN than younger individuals [see Use in Specific Populations (8.5) ].
- Estrogen-replete women and patients receiving oral estrogen may require higher doses [see Drug Interactions (7) ].
- Administer the prescribed dose daily.
- Either of two NORDITROPIN dosing regimens may be used:
- Non-weight based
- Initiate NORDITROPIN with a dose of approximately 0.2 mg/day (range, 0.15 mg/day to 0.3 mg/day) and increase the dose every 1-2 months by increments of approximately 0.1 mg/day to 0.2 mg/day, according to individual patient requirements based on the clinical response and serum insulin-like growth factor 1 (IGF-1) concentrations.
- Decrease the dose as necessary on the basis of adverse reactions and/or serum IGF-1 concentrations above the age- and gender-specific normal range.
- Maintenance dosages will vary considerably from person to person, and between male and female patients.
- Weight-based
- Initiate NORDITROPIN at 0.004 mg/kg daily and increase the dose according to individual patient requirements to a maximum of 0.016 mg/kg daily.
- Use the patient’s clinical response, adverse reactions, and determination of age- and gender-adjusted serum IGF-1 concentrations as guidance in dose titration.
- Not recommended for obese patients as they are more likely to experience adverse reactions with this regimen
DOSAGE FORMS AND STRENGTHS
Injection: NORDITROPIN is available as a clear and colorless solution in a
- 5 mg/1.5 mL FlexPro single-patient-use pen (orange)
- 10 mg/1.5 mL FlexPro single-patient-use pen (blue)
- 15 mg/1.5 mL FlexPro single-patient-use pen (green)
- 30 mg/3 mL FlexPro single-patient-use pen (purple)
USE IN SPECIFIC POPULATIONS
Pregnancy
Risk Summary
Limited available data with somatropin use in pregnant women are insufficient to determine a drug-associated risk of adverse developmental outcomes. In animal reproduction studies, there was no evidence of fetal or neonatal harm when pregnant rats were administered subcutaneous NORDITROPIN during organogenesis or during lactation at doses approximately 10-times higher than the maximal clinical dose of 0.016 mg/kg, based on body surface area (see Data).
The estimated background risk of birth defects and miscarriage for the indicated population is unknown. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2-4% and 15-20%, respectively.
Data
Animal Data
In an embryo-fetal development study, NORDITROPIN was administered via subcutaneous injection to pregnant rats from gestation Day 6 to 17, corresponding with the period of organogenesis. NORDITROPIN did not adversely affect fetal viability or developmental outcomes at maternal doses that were approximately 10-times the clinical dose of 0.016 mg/kg, based on body surface area.
In a pre- and post-natal development study in pregnant rats, NORDITROPIN was administered from gestation Day 17 through lactation Day 21 (weaning). No adverse developmental effects were observed in the offspring at doses up to 1.1 mg/kg (approximately 10 times the clinical dose of 0.016 mg/kg, based on body surface area).
Lactation
Risk Summary
There is no information regarding the presence of somatropin in human milk. Limited published data indicate that exogenous somatropin does not increase normal breastmilk concentrations of growth hormone. No adverse effects on the breastfed infant have been reported with somatropin. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for NORDITROPIN and any potential adverse effects on the breastfed infant from NORDITROPIN or from the underlying maternal condition.
Pediatric Use
Safety and effectiveness of NORDITROPIN in pediatric patients have been established in growth failure due to inadequate secretion of endogenous growth hormone, short stature associated with Noonan syndrome, short stature associated with Turner syndrome, short stature in children born small for gestational age (SGA) with no catch-up growth by age 2 years to 4 years of age, idiopathic short stature (ISS), and growth failure due to Prader-Willi syndrome (PWS).
Growth Failure due to Inadequate Secretion of Endogenous Growth Hormone
Safety and effectiveness of NORDITROPIN have been established in pediatric patients with growth failure due to growth hormone deficiency in a multi-center, prospective, randomized, open-label, dose-response study in 111 pediatric patients conducted for a two-year period [see Clinical Studies (14.1) ].
Short Stature Associated with Noonan Syndrome
Safety and effectiveness of NORDITROPIN have been established in pediatric patients with Noonan syndrome in a prospective, open-label, randomized, parallel group study in 21 pediatric patients conducted for 2 years [see Clinical Studies (14.2) ].
Short Stature Associated with Turner Syndrome
Safety and effectiveness of NORDITROPIN have been established in pediatric patients with short stature associated with Turner syndrome in two randomized, parallel group, open-label, multicenter studies in 87 pediatric patients [see Clinical Studies (14.3) ].
Short Stature in Pediatric Patients Born Small for Gestational Age (SGA) with No Catch-up Growth by Age 2 Years to 4 Years of Age
Safety and effectiveness of NORDITROPIN have been established in pediatric patients with short stature born SGA with no catch-up growth in a multi-center, randomized, double-blind, two-arm study to final height in 53 pediatric patients and in a randomized study of 84 prepubertal, non-GHD, Japanese pediatric patients [see Clinical Studies (14.4) ].
Idiopathic Short Stature (ISS)
Safety and effectiveness of NORDITROPIN have been established in pediatric patients with ISS based on data from a randomized, open-label clinical study with another somatropin product in 105 pediatric patients [see Clinical Studies (14.5) ].
Growth Failure Due to Prader-Willi Syndrome (PWS)
Safety and effectiveness of NORDITROPIN have been established in pediatric patients with growth failure due to Prader-Willi Syndrome based on data from two randomized, open label, controlled clinical trials with another somatropin product in pediatric patients. There have been reports of sudden death after initiating therapy with somatropin in pediatric patients with Prader-Willi syndrome who had one or more of the following risk factors: severe obesity, history of upper airway obstruction or sleep apnea, or unidentified respiratory infection. Male patients with one or more of these factors may be at greater risk than females. Patients with Prader-Willi syndrome should be evaluated for signs of upper airway obstruction and sleep apnea before initiation of treatment with somatropin. [see Contraindications (4) , Warnings and Precautions (5.2) , Clinical Studies (14.6) ].
Geriatric Use
The safety and effectiveness of NORDITROPIN in patients aged 65 and over has not been evaluated in clinical studies. Elderly patients may be more sensitive to the action of somatropin, and therefore may be more prone to develop adverse reactions. A lower starting dose and smaller dose increments should be considered for older patients [see Dosage and Administration (2.3) ].
CONTRAINDICATIONS
NORDITROPIN is contraindicated in patients with:
- Acute critical illness after open heart surgery, abdominal surgery or multiple accidental trauma, or those with acute respiratory failure due to the risk of increased mortality with use of pharmacologic doses of somatropin [see Warnings and Precautions (5.1) ].
- Pediatric patients with Prader-Willi syndrome who are severely obese, have a history of upper airway obstruction or sleep apnea, or have severe respiratory impairment due to the risk of sudden death [see Warnings and Precautions (5.2) ].
- Active Malignancy [see Warnings and Precautions (5.3) ].
- Hypersensitivity to NORDITROPIN or any of its excipients. Systemic hypersensitivity reactions have been reported with postmarketing use of somatropins [see Warnings and Precautions (5.6) ].
- Active proliferative or severe non-proliferative diabetic retinopathy.
- Pediatric patients with closed epiphyses.
WARNINGS AND PRECAUTIONS
- Increased Risk of Neoplasms : Second neoplasms have occurred in childhood cancer survivors. Monitor patients with preexisting tumors for progression or recurrence. (5.3 )
- Glucose Intolerance and Diabetes Mellitus : NORDITROPIN may decrease insulin sensitivity, particularly at higher doses. Monitor glucose levels periodically in all patients receiving NORDITROPIN, especially in patients with existing diabetes mellitus or at risk for development. (5.4 )
- Intracranial Hypertension (IH) : Has been reported usually within 8 weeks of initiation. Perform fundoscopic examinations prior to initiation and periodically thereafter. If papilledema occurs, stop treatment. (5.5 )
- Severe Hypersensitivity : Serious hypersensitivity reactions may occur. In the event of an allergic reaction, seek prompt medical attention. (5.6 )
- Fluid Retention : May occur in adults and may be dose dependent. (5.7 )
- Hypoadrenalism : Monitor patients for reduced serum cortisol levels and/or need for glucocorticoid dose increases in those with known hypoadrenalism. (5.8 )
- Hypothyroidism : Monitor thyroid function periodically as hypothyroidism may occur or worsen after initiation of somatropin. (5.9 )
- Slipped Capital Femoral Epiphysis in Pediatric Patients : May occur; evaluate patients with onset of a limp or hip/knee pain. (5.10 )
- Progression of Preexisting Scoliosis in Pediatric Patients : Monitor patients with scoliosis for progression. (5.11 )
- Pancreatitis : Has been reported; consider pancreatitis in patients with abdominal pain, especially pediatric patients. (5.12 )
Increased Mortality in Patients with Acute Critical Illness
Increased mortality in patients with acute critical illness due to complications following open heart surgery, abdominal surgery or multiple accidental trauma, or those with acute respiratory failure has been reported after treatment with pharmacologic amounts of somatropin [see Contraindications (4) ]. Two placebo-controlled clinical trials in non-growth hormone deficient adult patients (n=522) with these conditions in intensive care units revealed a significant increase in mortality (42% vs. 19%) among somatropin-treated patients (doses 5.3-8 mg/day) compared to those receiving placebo. The safety of continuing NORDITROPIN treatment in patients receiving replacement doses for approved indications who concurrently develop these illnesses has not been established. NORDITROPIN is not indicated for the treatment of non-GH deficient adults.
Sudden Death in Pediatric Patients with Prader-Willi Syndrome
There have been reports of sudden death after initiating therapy with somatropin in pediatric patients with Prader-Willi syndrome who had one or more of the following risk factors: severe obesity, history of upper airway obstruction or sleep apnea, or unidentified respiratory infection. Male patients with one or more of these factors may be at greater risk than females. Patients with Prader-Willi syndrome should be evaluated for signs of upper airway obstruction and sleep apnea before initiation of treatment with somatropin. If, during treatment with NORDITROPIN, patients show signs of upper airway obstruction (including onset of or increased snoring) and/or new onset sleep apnea, treatment should be interrupted. All patients with Prader-Willi syndrome treated with NORDITROPIN should also have effective weight control and be monitored for signs of respiratory infection, which should be diagnosed as early as possible and treated aggressively [see Contraindications (4) ] .
Increased Risk of Neoplasms
Active Malignancy
There is an increased risk of malignancy progression with somatropin treatment in patients with active malignancy [See Contraindications (4) ]. Any preexisting malignancy should be inactive and its treatment complete prior to instituting therapy with NORDITROPIN. Discontinue NORDITROPIN if there is evidence of recurrent activity.
Risk of Second Neoplasm in Pediatric Patients
There is an increased risk of a second neoplasm in pediatric cancer survivors who were treated with radiation to the brain/head and who developed subsequent GH deficiency and were treated with somatropin. Intracranial tumors, in particular meningiomas, were the most common of these second neoplasms. In adults, it is unknown whether there is any relationship between somatropin replacement therapy and CNS tumor recurrence. Monitor all patients receiving NORDITROPIN who have a history of GH deficiency secondary to an intracranial neoplasm for progression or recurrence of the tumor.
New Malignancy During Treatment
Because pediatric patients with certain rare genetic causes of short stature have an increased risk of developing malignancies, thoroughly consider the risks and benefits of starting NORDITROPIN in these patients. If NORDITROPIN is initiated, carefully monitor patients for development of neoplasms.
Monitor all patients receiving NORDITROPIN carefully for increased growth, or potential malignant changes, of preexisting nevi. Advise patients/caregivers to report marked changes in behavior, onset of headaches, vision disturbances and/or changes in skin pigmentation or changes in the appearance of pre-existing nevi.
Glucose Intolerance and Diabetes Mellitus
Treatment with somatropin may decrease insulin sensitivity, particularly at higher doses. New onset type 2 diabetes mellitus has been reported in patients taking somatropin. Previously undiagnosed impaired glucose tolerance and overt diabetes mellitus may be unmasked. Monitor glucose levels periodically in all patients receiving NORDITROPIN, especially in those with risk factors for diabetes mellitus, such as obesity, Turner syndrome, or a family history of diabetes mellitus. Patients with preexisting type 1 or type 2 diabetes mellitus or impaired glucose tolerance should be monitored closely. The doses of antidiabetic agents may require adjustment when NORDITROPIN is initiated.
Intracranial Hypertension
Intracranial hypertension (IH) with papilledema, visual changes, headache, nausea, and/or vomiting has been reported in a small number of patients treated with somatropins. Symptoms usually occurred within the first eight (8) weeks after the initiation of somatropin therapy. In all reported cases, IH-associated signs and symptoms rapidly resolved after cessation of therapy or a reduction of the somatropin dose. Funduscopic examination should be performed routinely before initiating treatment with NORDITROPIN to exclude preexisting papilledema, and periodically thereafter. If papilledema is observed by funduscopy during somatropin treatment, treatment should be stopped. If somatropin-induced IH is diagnosed, treatment with NORDITROPIN can be restarted at a lower dose after IH-associated signs and symptoms have resolved. Patients with Turner syndrome may be at increased risk for the development of IH.
Severe Hypersensitivity
Serious systemic hypersensitivity reactions including anaphylactic reactions and angioedema have been reported with postmarketing use of somatropins. Patients and caregivers should be informed that such reactions are possible and that prompt medical attention should be sought if an allergic reaction occurs [see Contraindications (4) ].
Fluid Retention
Fluid retention during somatropin replacement therapy in adults may frequently occur. Clinical manifestations of fluid retention (e.g. edema, arthralgia, myalgia, nerve compression syndromes including carpal tunnel syndrome/paraesthesias) are usually transient and dose dependent.
Hypoadrenalism
Patients receiving somatropin therapy who have or are at risk for pituitary hormone deficiency(s) may be at risk for reduced serum cortisol levels and/or unmasking of central (secondary) hypoadrenalism. In addition, patients treated with glucocorticoid replacement for previously diagnosed hypoadrenalism may require an increase in their maintenance or stress doses following initiation of NORDITROPIN treatment. Monitor patients for reduced serum cortisol levels and/or need for glucocorticoid dose increases in those with known hypoadrenalism [see Drug Interactions (7) ].
Hypothyroidism
Undiagnosed/untreated hypothyroidism may prevent an optimal response to NORDITROPIN, in particular, the growth response in pediatric patients. Patients with Turner syndrome have an inherently increased risk of developing autoimmune thyroid disease and primary hypothyroidism. In patients with GH deficiency, central (secondary) hypothyroidism may first become evident or worsen during somatropin treatment. Therefore, patients should have periodic thyroid function tests and thyroid hormone replacement therapy should be initiated or appropriately adjusted when indicated.
Slipped Capital Femoral Epiphysis in Pediatric Patients
Slipped capital femoral epiphysis may occur more frequently in patients with endocrine disorders (including GH deficiency and Turner syndrome) or in patients undergoing rapid growth. Slipped capital femoral epiphysis may lead to osteonecrosis. Cases of slipped capital femoral epiphysis with or without osteonecrosis have been reported in pediatric patients with short stature receiving somatropin, including NORDITROPIN. Evaluate pediatric patients receiving NORDITROPIN with the onset of a limp or complaints of hip or knee pain for slipped capital femoral epiphysis and osteonecrosis and manage accordingly .
Progression of Preexisting Scoliosis in Pediatric Patients
Somatropin increases the growth rate, and progression of existing scoliosis can occur in patients who experience rapid growth. Somatropin has not been shown to increase the occurrence of scoliosis. Monitor patients with a history of scoliosis for progression of scoliosis.
Pancreatitis
Cases of pancreatitis have been reported in pediatric patients and adults receiving somatropin products. There may be a greater risk in pediatric patients compared with adults. Published literature indicates that females who have Turner syndrome may be at greater risk than other pediatric patients receiving somatropin products. Pancreatitis should be considered in patients who develop persistent severe abdominal pain.
Lipoatrophy
When somatropin products are administered subcutaneously at the same site over a long period of time, tissue atrophy may result. Rotate injection sites when administering NORDITROPIN to reduce this risk [see Administration and Use Instructions (2.1) ].
Laboratory Tests
Serum levels of inorganic phosphorus, alkaline phosphatase, parathyroid hormone (PTH) and IGF-I may increase after NORDITROPIN treatment.
ADVERSE REACTIONS
The following important adverse reactions are also described elsewhere in the labeling:
- Increased mortality in patients with acute critical illness [see Warnings and Precautions (5.1) ]
- Sudden death in children with Prader-Willi syndrome [see Warnings and Precautions (5.2) ]
- Neoplasms [see Warnings and Precautions (5.3) ]
- Glucose intolerance and diabetes mellitus [see Warnings and Precautions (5.4) ]
- Intracranial hypertension [see Warnings and Precautions (5.5) ]
- Severe hypersensitivity [see Warnings and Precautions (5.6) ]
- Fluid retention [see Warnings and Precautions (5.7) ]
- Hypoadrenalism [see Warnings and Precautions (5.8) ]
- Hypothyroidism [see Warnings and Precautions (5.9) ]
- Slipped capital femoral epiphysis in pediatric patients [see Warnings and Precautions (5.10) ]
- Progression of preexisting scoliosis in pediatric patients [see Warnings and Precautions (5.11) ]
- Pancreatitis [see Warnings and Precautions (5.12) ]
- Lipoatrophy [see Warnings and Precautions (5.13) ]
Clinical Trials Experience
Because clinical trials are conducted under varying conditions, adverse reaction rates observed during the clinical trials performed with one somatropin product cannot always be directly compared to the rates observed during the clinical trials performed with another somatropin product, and may not reflect the adverse reaction rates observed in practice.
Pediatric Patients
Growth Failure due to Inadequate Secretion of Endogenous Growth Hormone
In one randomized, open label, clinical study the most frequent adverse reactions were headache, pharyngitis, otitis media and fever. There were no clinically significant differences between the three doses assessed in the study (0.025, 0.05 and 0.1 mg/kg/day).
Short Stature Associated with Noonan Syndrome
NORDITROPIN was studied in 21 pediatric patients, 3 years to 14 years of age at doses of 0.033 mg/kg/day and 0.066 mg/kg/day. After the two-year study, patients continued NORDITROPIN treatment until final height was achieved; randomized dose groups were not maintained. Adverse reactions were later collected retrospectively from 18 pediatric patients; total follow-up was 11 years. An additional 6 pediatric patients were not randomized, but followed the protocol and are included in this assessment of adverse reactions.
The most frequent adverse reactions were upper respiratory infection, gastroenteritis, ear infection, and influenza. Cardiac disorders was the system organ class with the second most adverse reactions reported. Scoliosis was reported in 1 and 4 pediatric patients receiving doses of 0.033 mg/kg/day and 0.066 mg/kg/day respectively. The following additional adverse reactions also occurred once: insulin resistance and panic reaction for the 0.033 mg/kg/day dose group; injection site pruritus, bone development abnormal, depression, and self-injurious ideation in the 0.066 mg/kg/day dose group. Headache occurred in 2 cases in the 0.066 mg/kg/day dose group.
Short Stature Associated with Turner Syndrome
In two clinical studies in pediatric patients that were treated until final height with various doses of NORDITROPIN, the most frequently reported adverse reactions were influenza-like illness, otitis media, upper respiratory tract infection, otitis externa, gastroenteritis, eczema and, impaired fasting glucose. Adverse reactions in study 1 were most frequent in the highest dose groups. Three patients in study 1 had excessive growth of hands and/or feet in the high dose groups. Two patients in study 1 had a serious adverse reaction of exacerbation of preexisting scoliosis in the 0.045 mg/kg/day group.
Small for Gestational Age (SGA) with No Catch-up Growth by Age 2-4 Years
In a study, 53 pediatric patients were treated with 2 doses of NORDITROPIN (0.033 or 0.067 mg/kg/day) to final height for up to 13 years (mean duration of treatment 7.9 and 9.5 years for girls and boys, respectively). The most frequently reported adverse reactions were influenza-like illness, upper respiratory tract infection, bronchitis, gastroenteritis, abdominal pain, otitis media, pharyngitis, arthralgia, headache, gynecomastia, and increased sweating. One pediatric patient treated with 0.067 mg/kg/day for 4 years was reported with disproportionate growth of the lower jaw, and another patient treated with 0.067 mg/kg/day developed a melanocytic nevus. 4 pediatric patients treated with 0.067 mg/kg/day and 2 pediatric patients treated with 0.033 mg/kg/day of NORDITROPIN had increased fasting blood glucose levels after 1 year of treatment. In addition, small increases in mean fasting blood glucose and insulin levels after 1 and 2 years of NORDITROPIN treatment appeared to be dose-dependent.
In a second study, 98 Japanese pediatric patients were treated with 2 doses of NORDITROPIN (0.033 or 0.067 mg/kg/day) for 2 years or were untreated for 1 year. Adverse reactions were otitis media, arthralgia and impaired glucose tolerance. Arthralgia and transiently impaired glucose tolerance were reported in the 0.067 mg/kg/day treatment group.
Idiopathic Short Stature
In two open-label clinical studies with another somatropin product in pediatric patients, the most common adverse reactions were upper respiratory tract infections, influenza, tonsillitis, nasopharyngitis, gastroenteritis, headaches, increased appetite, pyrexia, fracture, altered mood, and arthralgia.
Growth Failure Due to Prader-Willi Syndrome
In two clinical studies in pediatric patients with PWS carried out with another somatropin product, the following adverse reactions were reported: edema, aggressiveness, arthralgia, benign intracranial hypertension, hair loss, headache, and myalgia.
Adult Patients
Adults with Growth Hormone Deficiency
Adverse reactions with an incidence of ≥5% occurring in patients with AO GHD during the 6 month placebo-controlled portion of a clinical trial for NORDITROPIN are presented in Table 1 .
Table 1 – Adverse Reactions with ≥5% Overall Incidence in Adult Onset Growth Hormone
Deficient Patients Treated with NORDITROPIN During a Six Month Placebo-Controlled Clinical Trial
Placebo (N=52) | NORDITROPIN (N=53) | |
Adverse Reactions | % | % |
Peripheral Edema | 8 | 42 |
Edema | 0 | 25 |
Arthralgia | 15 | 19 |
Leg Edema | 4 | 15 |
Myalgia | 8 | 15 |
Infection (non-viral) | 8 | 13 |
Paraesthesia | 6 | 11 |
Skeletal Pain | 2 | 11 |
Headache | 6 | 9 |
Bronchitis | 0 | 9 |
Flu-like symptoms | 4 | 8 |
Hypertension | 2 | 8 |
Gastroenteritis | 8 | 8 |
Other Non-Classifiable Disorders (excludes accidental injury) | 6 | 8 |
Increased sweating | 2 | 8 |
Glucose tolerance abnormal | 2 | 6 |
Laryngitis | 6 | 6 |
Type 2 diabetes mellitus | 0 | 5 |
Postmarketing Experience
The following adverse reactions have been identified during post-approval use of somatropin or NORDITROPIN. Because these adverse reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure .
Immune system disorders — Serious systemic hypersensitivity reactions including anaphylactic reactions and angioedema
Skin — Increase in size or number of cutaneous nevi
Endocrine disorders — Hypothyroidism - Gynecomastia
Metabolism and nutrition disorders — Hyperglycemia
Musculoskeletal and connective tissue disorders — Slipped capital femoral epiphysis and osteonecrosis (including Legg-Calvé-Perthes disease) have been reported in pediatric patients treated with growth hormone [see Warnings and Precautions (5.10)]. Cases have been reported with NORDITROPIN.
Investigations — Increase in blood alkaline phosphatase level — Decrease in serum thyroxin (T4) levels
Gastrointestinal — Pancreatitis
Neoplasm — Leukemia has been reported in a small number of GH deficient children treated with somatropin, somatrem (methionylated rhGH) and GH of pituitary origin
DRUG INTERACTIONS
Table 2 includes a list of drugs with clinically important drug interactions when administered concomitantly with NORDITROPIN and instructions for preventing or managing them.
Table 2: Clinically Important Drug Interactions with NORDITROPIN
Glucocorticoids | |
Clinical Impact: | Microsomal enzyme 11β-hydroxysteroid dehydrogenase type 1 (11βHSD-1) is required for conversion of cortisone to its active metabolite, cortisol, in hepatic and adipose tissue. NORDITROPIN inhibits 11βHSD-1. Consequently, individuals with untreated GH deficiency have relative increases in 11βHSD-1 and serum cortisol. Initiation of NORDITROPIN may result in inhibition of 11βHSD-1 and reduced serum cortisol concentrations. |
Intervention: | Patients treated with glucocorticoid replacement for hypoadrenalism may require an increase in their maintenance or stress doses following initiation of NORDITROPIN [see Warnings and Precautions (5.8) ]. |
Examples: | Cortisone acetate and prednisone may be effected more than others since conversion of these drugs to their biologically active metabolites is dependent on the activity of 11βHSD-1. |
Pharmacologic Glucocorticoid Therapy and Supraphysiologic Glucocorticoid Treatment | |
Clinical Impact: | Pharmacologic glucocorticoid therapy and supraphysiologic glucocorticoid treatment may attenuate the growth promoting effects of NORDITROPIN in pediatric patients. |
Intervention: | Carefully adjust glucocorticoid replacement dosing in pediatric patients receiving glucocorticoid treatments to avoid both hypoadrenalism and an inhibitory effect on growth. |
Cytochrome P450-Metabolized Drugs | |
Clinical Impact: | Limited published data indicate that somatropin treatment increases cytochrome P450 (CP450)-mediated antipyrine clearance. NORDITROPIN may alter the clearance of compounds known to be metabolized by CP450 liver enzymes. |
Intervention: | Careful monitoring is advisable when NORDITROPIN is administered in combination with drugs metabolized by CP450 liver enzymes. |
Oral Estrogen | |
Clinical Impact: | Oral estrogens may reduce the serum IGF-1 response to NORDITROPIN. |
Intervention: | Patients receiving oral estrogen replacement may require greater NORDITROPIN dosages [see Dosage and Administration (2.3) ] . |
Insulin and/or Other Hypoglycemic Agents | |
Clinical Impact: | Treatment with NORDITROPIN may decrease insulin sensitivity, particularly at higher doses. |
Intervention: | Patients with diabetes mellitus may require adjustment of their doses of insulin and/or other hypoglycemic agents [see Warnings and Precautions (5.4) ]. |
DESCRIPTION
Somatropin is a human growth hormone (GH) produced by recombinant DNA technology using Escherichia Coli. The protein is comprised of 191 amino acids and has a molecular weight of about 22,000 daltons. The amino acid sequence is identical to that of human growth hormone of pituitary origin.
NORDITROPIN (somatropin) injection is a sterile, clear and colorless solution for subcutaneous use in ready-to-administer prefilled single-patient-use pens with a volume of 1.5 mL or 3 mL with a pH of 6.13–6.20.
Each NORDITROPIN contains the following (see Table 3 ):
Table 3. Contents of NORDITROPIN Pen
Component | 5 mg/1.5 mL | 10 mg/1.5 mL | 15 mg/1.5 mL | 30 mg/3 mL |
Somatropin | 5 mg | 10 mg | 15 mg | 30 mg |
Histidine | 1 mg | 1 mg | 1.7 mg | 3.3 mg |
Mannitol | 60 mg | 60 mg | 58 mg | 117 mg |
Phenol | 4.5 mg | 4.5 mg | 4.5 mg | 9 mg |
Poloxamer 188 | 4.5 mg | 4.5 mg | 4.5 mg | 9 mg |
Hydrochloric acid/sodium hydroxide to adjust pH | as needed | as needed | as needed | as needed |
Water for Injection, USP | up to 1.5 mL | up to 1.5 mL | up to 1.5 mL | up to 3 mL |
CLINICAL PHARMACOLOGY
Mechanism of Action
Somatropin binds to dimeric GH receptors located within the cell membranes of target tissue cells. This interaction results in intracellular signal transduction and subsequent induction of transcription and translation of GH-dependent proteins including IGF-1, IGF BP-3 and acid-labile subunit. Somatropin has direct tissue and metabolic effects or mediated indirectly by IGF-1, including stimulation of chondrocyte differentiation, and proliferation, stimulation hepatic glucose output, protein synthesis and lipolysis.
Somatropin stimulates skeletal growth in pediatric patients with GHD as a result of effects on the growth plates (epiphyses) of long bones. The stimulation of skeletal growth increases linear growth rate (height velocity) in most somatropin-treated pediatric patients. Linear growth is facilitated in part by increased cellular protein synthesis.
Pharmacodynamics
Subcutaneous administration of a single dose of 4 mg NORDITROPIN in healthy subjects (n=26) with suppressed endogenous growth hormone results in an increased mean (SD) IGF-1 level from 190 (46) ng/mL predose to maximal level of 276 (49) ng/mL after approx. 24 hours. After 96 hours, the subjects displayed a mean (SD) IGF-1 concentration of 196 (41) ng/mL, comparable to the predose value.
Pharmacokinetics
Absorption - Somatropin has been studied following subcutaneous and intravenous administration in adult healthy subjects and GHD patients. A single dose administration of 4 mg NORDITROPIN in healthy subjects (n=26) with suppressed endogenous growth hormone resulted in a mean (SD) C max of 34.9 (10.4) ng/mL after approximately 3.0 hours. After a 180-min IV infusion of NORDITROPIN (33 ng/kg/min) administered to GHD patients (n=9), a mean (SD) hGH steady state serum level of approximately 23.1 (15.0) ng/mL was reached at 150 min.
After a SC dose of 0.024 mg/kg or 3 IU/m 2 given in the thigh to adult GHD patients (n=18), mean (SD) C max values of 13.8 (5.8) and 17.1 (10.0) ng/mL were observed for the 4 and 8 mg NORDITROPIN vials, respectively, at approximately 4 to 5 hr. post dose. The absolute bioavailability for NORDITROPIN after the SC route of administration is currently not known.
Distribution — The mean (SD) apparent volume of distribution of somatropin after single dose subcutaneous administration of 4 mg NORDITROPIN in healthy subjects is 43.9 (14.9) L.
Elimination
Metabolism — Extensive metabolism studies have not been conducted. The metabolic fate of somatropin involves classical protein catabolism in both the liver and kidneys.
Excretion – The mean apparent terminal T 1/2 values in healthy adult subjects (n=26) was 2.0 (0.5) hours. In GHD patients receiving 180-min IV infusion of NORDITROPIN (33 ng/kg/min), a mean clearance rate of approximately 2.3 (1.8) mL/min/kg or 139 (105) mL/min for hGH was observed. Following infusion, serum hGH levels had a biexponential decay with a terminal elimination half-life (T 1/2 ) of approximately 21.1 (5.1) min. The mean apparent terminal T 1/2 values in GHD patients receiving a SC dose of 0.024 mg/kg or 3 IU/m 2 was estimated to be approximately 7 to 10 hr. The longer half-life observed after subcutaneous administration is due to slow absorption from the injection site. Urinary excretion of intact somatropin has not been measured.
Geriatric patients — The pharmacokinetics of somatropin have not been studied in patients greater than 65 years of age.
Pediatric patients — The pharmacokinetics of somatropin in pediatric patients are similar to those of adults.
Male and Female Patients — No gender-specific pharmacokinetic studies have been performed with somatropin. The available literature indicates that the pharmacokinetics of somatropin are similar in men and women.
Patients with Renal or Hepatic Impairment — No studies have been performed with somatropin.
Immunogenicity
The observed incidence of anti-drug antibodies is highly dependent on the sensitivity and specificity of the assay. Differences in assay methods preclude meaningful comparisons of the incidence of anti-drug antibodies in the studies described below with the incidence of anti-drug antibodies in other studies, including those of NORDITROPIN or other somatropins. In the case of growth hormone, antibodies with binding capacities lower than 2 mg/mL have not been associated with growth attenuation. In a very small number of patients treated with somatropin, when binding capacity was greater than 2 mg/mL, interference with the growth response was observed.
In clinical trials, GH deficient pediatric patients receiving NORDITROPIN for up to 12 months were tested for induction of antibodies, and 0 of 358 patients developed antibodies with binding capacities above 2 mg/L. Amongst these patients, 165 had previously been treated with other somatropin formulations, and 193 were previously untreated naive patients. Eighteen of 76 children (~24%) treated with NORDITROPIN for short stature born SGA developed anti-rhGH antibodies.
NONCLINICAL TOXICOLOGY
Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenicity and mutagenicity studies have not been conducted with NORDITROPIN.
In a rat study evaluating female fertility, animals were administered once daily subcutaneous doses of 0.1, 0.3, and 1.1 mg/kg NORDITROPIN beginning two weeks prior to mating, throughout mating and during the first 7 days of pregnancy. Delays in the time to mating were observed at doses greater than or equal to 0.3 mg/kg (approximately 3 times the maximum adult clinical dose of 0.016 mg/kg, based on body surface area), but these doses were also associated with increases in the number of corpora lutea and implantations. A decrease in the pregnancy rate was observed at the dose of 1.1 mg/kg (approximately 10 times the clinical dose of 0.016 mg/kg, based on body surface area). Male fertility parameters have not been evaluated with administration of NORDITROPIN.
CLINICAL STUDIES
Growth Failure due to Inadequate Secretion of Endogenous Growth Hormone
The efficacy and safety of NORDITROPIN was assessed in a multicenter, prospective randomized, open label, dose response study with three doses (0.025, 0.05 and 0.1 mg/kg/day). A total of 111 pediatric patients with GH deficiency were randomized to each dose; 37(0.025 mg/kg/day):38(0.05 mg/kg/day):36(0.1 mg/kg/day). Patients met the following entry criteria: chronological age ≥ 3 years with a skeletal age < 10 years if male and < 8 years if female; pubertal stage = stage 1; previously untreated GH deficiency; peak plasma hormone concentration < 7 ng/ml or < 10 ng/ml (depending on assay used) in two tests.
The results are displayed in Table 4 . The adjusted mean increases in HSDS over the 2-year period were 0.81, 1.57 and 1.73 in the 0.025, 0.05 and 0.1 mg/kg/day dose groups, respectively. There was no significant difference in ΔHSDS between the 0.05 and 0.1 mg/kg/day treatment groups. Height velocity (HV, cm/year) and HVSDS increased considerably after initiation of treatment, with the greatest response observed during the first year of treatment.
Table 4 – Efficacy of NORDITROPIN in Pediatric GH Deficiency
NORDITROPIN | |||||||||
0.025 mg/kg/day | 0.05 mg/kg/day | 0.1 mg/kg/day | |||||||
N | Mean | SD | N | Mean | SD | N | Mean | SD | |
Change in Standing Height (cm) | |||||||||
Baseline to Month 12 | 37 | 9.5 | 2.1 | 37 | 13.2• | 2.6 | 34 | 13.7• | 2.7 |
Baseline to Month 24 | 34 | 17.6 | 3.4 | 37 | 22.2• | 4.7 | 33 | 23.7• | 4.0 |
Change in Sitting Height (cm) | |||||||||
Baseline to Month 12 | 32 | 5.4 | 2.4 | 36 | 6.5• | 1.6 | 32 | 7.4•• | 1.5 |
Baseline to Month 24 | 29 | 9.3 | 2.5 | 35 | 10.8•• | 2.6 | 31 | 12.2•• | 2.0 |
Change in Bone Age (yr) | |||||||||
Baseline to Month 12 | 37 | 1.3 | 0.9 | 38 | 1.7 | 0.8 | 34 | 1.6 | 0.8 |
Month 12 to Month 24 | 37 | 0.6 | 2.5 | 38 | 1.4 | 2.7 | 34 | 1.6• | 0.8 |
- •Significant (p <0.05) change from baseline compared to the 0.025 mg/kg/group
••Significant (p <0.05) change from baseline compared to both other groups
Short Stature Associated with Noonan Syndrome
A prospective, open label, randomized, parallel group study with 21 pediatric patients was conducted for 2 years to evaluate the efficacy and safety of NORDITROPIN. Additional 6 children were not randomized, but did follow the protocol. Inclusion criteria included bone age determination showing no significant acceleration, prepubertal status, height SDS <-2, and HV SDS <1 during the 12 months pre-treatment. Exclusion criteria were previous or ongoing treatment with growth hormone, anabolic steroids or corticosteroids, congenital heart disease or other serious disease perceived to possibly have major impact on growth, FPG >6.7 mmol/L (>120 mg/dL), or growth hormone deficiency (peak GH levels <10 ng/mL). The twenty-four, 12 female and 12 male, patients 3 – 14 years of age received either 0.033 mg/kg/day or 0.066 mg/kg/day of NORDITROPIN subcutaneously which was adjusted based on growth response after the first 2 years.
After the initial two-year study, NORDITROPIN treatment continued until final height. Retrospective final height was collected from 18 patients in the study and the 6 who had followed the protocol without randomization. Historical reference materials of height velocity and adult height analyses of Noonan patients served as the controls.
Patients obtained a final height (FH) gain from baseline of 1.5 and 1.6 SDS estimated according to the national and the Noonan reference, respectively. A height gain of 1.5 SDS (national) corresponds to a mean height gain of 9.9 cm in boys and 9.1 cm in girls at 18 years of age, while a height gain of 1.6 SDS (Noonan) corresponds to a mean height gain of 11.5 cm in boys and 11.0 cm in girls at 18 years of age.
A comparison of HV between the two treatment groups during the first two years of treatment for the randomized subjects was 10.1 and 7.6 cm/year with 0.066 mg/kg/day versus 8.55 and 6.7 cm/year with 0.033 mg/kg/day, for Year 1 and Year 2, respectively.
Short Stature Associated with Turner Syndrome
Two randomized, parallel group, open label, multicenter studies were conducted in the Netherlands to evaluate the efficacy and safety of NORDITROPIN. Patients were treated to final height in both studies [height velocity (HV) < 2 cm/year]. Changes in height were expressed as standard deviation scores (SDS) utilizing reference data for untreated Turner syndrome patients as well as the national Dutch population.
In Study 1, 68 euthyroid Caucasian patients stratified based on age and baseline height SDS were randomized in a 1:1:1 ratio to three different NORDITROPIN treatment regimens: 0.045 mg/kg/day (Dose A) for the entire study; 0.045 mg/kg/day for the first year and 0.067 mg/kg/day thereafter (Dose B); or 0.045 mg/kg/day for the first year, 0.067 for the second year, and 0.089 mg/kg/day thereafter (Dose C). At baseline, mean age was 6.5 years, mean height SDS (National standard) was -2.7, and mean HV during the previous year was 6.5 cm/year. Patients also received estrogen therapy after age 12 and following four years of NORDITROPIN treatment if they did not have spontaneous puberty.
Patients were treated for a mean of 8.4 years. As seen in Table 5 , overall mean final height was 161 cm in the 46 children who attained final height. Seventy percent of these children reached a final height within the normal range (height SDS > -2 using the National standard). A greater percentage of children in the two escalated dose groups reached normal final height. The mean changes from baseline to final height in height SDS after treatment with Dose B and Dose C were significantly greater than the mean changes observed after treatment with Dose A (utilizing both the National and Turner standards). The mean changes from baseline to final height in height SDS (Turner standard) in Table 5 correspond to mean height gains of 9.4, 14.1 and 14.4 cm after treatment with Doses A, B and C, respectively. The mean changes from baseline to final height in height SDS (National standard) in Table 5 correspond to mean height gains of 4.5, 9.1 and 9.4 cm after treatment with Doses A, B and C, respectively. In each treatment group, peak HV was observed during treatment Year 1, and then gradually decreased each year; during Year 4, HV was less than the pre-treatment HV. However, between Year 2 and Year 6, a greater HV was observed in the two dose escalation groups compared to the 0.045 mg/kg/day group.
Table 5 – Final Height-Related Results After Treatment of Patients with Turner Syndrome with NORDITROPIN in a Randomized, Dose Escalating Study
Dose A 0.045 mg/kg/day (n = 19) | Dose B up to 0.067 mg/kg/day (n = 15) | Dose C up to 0.089 mg/kg/day (n = 12) | Total (n = 46) | |
Baseline height (cm) 1 | 105 (12) | 108 (12.7) | 107 (11.7) | 106 (11.9) |
Final height (cm) 1 | 157 (6.7) | 163 (6.0) | 163 (4.9) | 161 (6.5) |
Number (%) of patients reaching normal height (height SDS >-2 using National standard) | 10 (53%) | 12 (80%) | 10 (83%) | 32 (70%) |
Height SDS (Turner standard) 2 | ||||
Final [95% CI] | 1.7 [1.4, 2.0] | 2.5 [2.1, 2.8] 3 | 2.5 [2.1, 2.9] 4 | NA |
Change from baseline [95% CI] | 1.5 [1.2, 1.8] | 2.2 [1.9, 2.5] 3 | 2.2 [1.9, 2.6] 4 | NA |
Height SDS (National standard) 2 | ||||
Final [95% CI] | -1.9 [-2.2, -1.6] | -1.2 [-1.5, -0.9] 4 | -1.2 [-1.6, -0.8] 5 | NA |
Change from baseline [95% CI] | 0.7 [0.4, 1.0] | 1.4 [1.1, 1.7] 4 | 1.4 [1.1, 1.8] 5 | NA |
Values are expressed as mean (SD) unless otherwise indicated. SDS: Standard deviation score.
1 Unadjusted (raw) means; 2 Adjusted (least squares) means based on an ANCOVA model including terms for treatment,
duration of treatment, age at baseline, bone age at baseline, height SDS at baseline, age at onset of puberty and mid-parental target height SDS;
3 p=0.005 vs. Dose A; 4 p=0.006 vs. Dose A; 5 p=0.008 vs. Dose A
In Study 2, 19 euthyroid Caucasian patients (with bone age ≤13.9 years) were randomized to treatment with 0.067 mg/kg/day of NORDITROPIN as a single subcutaneous dose in the evening, or divided into two doses (1/3 morning and 2/3 evening). All subjects were treated with concomitant ethinyl estradiol. Overall, at baseline, mean age was 13.6 years, mean height SDS (National standard) was -3.5 and mean HV during the previous year was 4.3 cm/year. Patients were treated for a mean of 3.6 years. In that there were no significant differences between the two treatment groups for any linear growth variables, the data from all patients were pooled. Overall mean final height was 155 cm in the 17 children who attained final height. Height SDS changed significantly from -3.5 at baseline to -2.4 at final height (National standard), and from 0.7 to 1.3 at final height (Turner standard).
Short Stature in Pediatric Patients Born Small for Gestational Age (SGA) with No Catch-up Growth by Age 2-4 Years
A multi-center, randomized, double-blind, two-arm study to final height (Study 1) and a 2-year, multi-center, randomized, double-blind, parallel-group study (Study 2) were conducted to assess the efficacy and safety of NORDITROPIN. Changes in height and height velocity were compared to a national reference population in both studies.
Study 1 included 53, 38 male, 15 female, non-GHD, Dutch prepubertal pediatric patients 3-11 years of age with short stature born SGA with no catch-up growth. Catch-up growth was defined as obtaining a height of ≥ 3 rd percentile within the first 2 years of life or at a later stage. Inclusion criteria included: birth length < 3 rd percentile for gestational age, and height velocity (cm/year) for chronological age < 50 th percentile. Exclusion criteria included chromosomal abnormalities, signs of a syndrome (except for Silver-Russell syndrome), serious/chronic co-morbid disease, malignancy, and previous rhGH therapy. NORDITROPIN was administered subcutaneously daily at bedtime at a dose of approximately 0.033 (Dose A) or 0.067 mg/kg/day (Dose B) for the entire treatment period. Final height was defined as a height velocity below 2 cm/year. Treatment with NORDITROPIN was continued to final height for up to 13 years. Mean duration of treatment was 9.5 years (boys) and 7.9 years (girls).
38 out of 53 children (72%) reached final height. Sixty-three percent (24 out of 38) of the children who reached final height were within the normal range of their healthy peers (Dutch national reference). For both doses combined, actual mean final height was 171 (SD 6.1) cm in boys and 159 (SD 4.3) cm in girls.
As seen in Table 6 , for boys and girls combined, both mean final height SDS, and increase in height SDS from baseline to final height, were significantly greater after treatment with Dose B (0.067 mg/kg/day). A similar dose response was observed for the increase in height SDS from baseline to Year 2 ( Table 6 ).
Overall mean height velocity at baseline was 5.4 cm/y (SD 1.2; n=29). Height velocity was greatest during the first year of NORDITROPIN treatment and was significantly greater after treatment with Dose B (mean 11.1 cm/y [SD 1.9; n=19]) compared with Dose A (mean 9.7 cm/y [SD 1.3; n=10]).
Table 6 – Study 1: Results for Final Height SDS and Change from Baseline to Final Height in Height SDS Using National Standard After Long-Term Treatment of SGA Children with NORDITROPIN
Raw Mean ± SD (N) | |||
Dose A 0.033 mg/kg/day | Dose B 0.067 mg/kg/day | Total | |
Baseline Height SDS | -3.2 ± 0.7 (26) | -3.2 ± 0.7 (27) | -3.2 ± 0.7 (53) |
Adjusted least-squares mean ± standard error (N), Treatment Difference [95% confidence intervals] | |||
Height SDS: Change from Baseline at Year 2 2 | 1.4 ± 0.1 (26) | 1.8 ± 0.1 (26) | Treatment Diff = 0.4 [0.2, 0.7] 3 |
Height SDS: Change from Baseline at Final Height 1 | 1.4 ± 0.2 (19) | 1.8 ± 0.2 (19) | Treatment Diff = 0.5 [0.0, 0.9] 3 |
Final Height SDS 1 | -1.8 ± 0.2 (19) | -1.3 ± 0.2 (19) | |
Final Height SDS > -2 | 13/19 (68%) | 11/19 (58%) | 24/38 (63%) |
SDS: Standard deviation score.
1 Adjusted (least-squares) means based on an ANCOVA model including terms for treatment, gender, age at baseline, bone age at baseline, height SDS at baseline, duration of treatment, peak GH after stimulation and baseline IGF-1.
2 Adjusted (least-squares) means based on an ANCOVA model including terms for treatment, gender, age at baseline, height SDS at baseline, and pubertal status.
3 p<0.05
In study 2, 84 randomized, prepubertal, non-GHD, Japanese children (age 3-8) were treated for 2 years with 0.033 or 0.067 mg/kg/day of NORDITROPIN subcutaneously daily at bedtime or received no treatment for 1 year. Additional inclusion criteria included birth length or weight SDS ≤ -2 or < 10 th percentile for gestational age, height SDS for chronological age ≤ -2, and height velocity SDS for chronological age < 0 within one year prior to Visit 1. Exclusion criteria included diabetes mellitus, history or presence of active malignancy, and serious co-morbid conditions.
As seen in Table 7 , for boys and girls combined, there was a dose-dependent increase in height SDS at Year 1 and Year 2. The increase in height SDS from baseline to Year 2 (0.033 mg/kg/day, 0.8 vs. 0.067 mg/kg/day, 1.4) was significantly greater after treatment with 0.067 mg/kg/day. In addition, the increase in height SDS at Year 1 was significantly greater in both active treatment groups compared to the untreated control group.
Table 7 – Study 2: Results for Change from Baseline in Height SDS At Year 1 and Year 2 Using National Standard After Short-Term Treatment of SGA Children with NORDITROPIN
Raw Mean ± SD (N) | |||
No Treatment | 0.033 mg/kg/day | 0.067 mg/kg/day | |
Height SDS: Baseline | -2.9 ± 0.5 (15) | -3.0 ± 0.6 (35) | -2.9 ± 0.7 (34) |
Height SDS: Year 1 | -2.8 ± 0.5 (15) | -2.4 ± 0.6 (33) | -2.0 ± 0.8 (34) |
Height SDS: Year 2 | NA | -2.2 ± 0.7 (33) | -1.4 ± 0.7 (32) |
Adjusted least-squares mean ± standard error (N), Treatment Diff [95% confidence intervals] | |||
Height SDS: Change from Baseline at Year 1 1 | 0.1 ± 0.1 (15) | 0.6 ± 0.1 (33) | 0.9 ± 0.1 (34) |
0.033 vs. No Treatment: Treatment Diff = 0.5, [0.3, 0.7] 2 0.067 vs. No Treatment: Treatment Diff = 0.8, [0.6, 1.0] 2 0.067 vs. 0.033: Treatment Diff = 0.3, [0.2, 0.5] 2 | |||
Height SDS: Change from Baseline at Year 2 1 | NA | 0.8 ± 0.1 (33) | 1.4 ± 0.1 (32) |
0.067 vs. 0.033: Treatment Diff = 0.6, [0.5, 0.8], p-value < 0.0001 | |||
SDS: Standard deviation score.
1 Adjusted (least-squares) means based on an ANCOVA model including terms for treatment, gender, age at baseline, and height SDS at baseline. All children remained prepubertal during the study.
2 p< 0.0001
Idiopathic Short Stature (ISS)
The efficacy and safety of another somatropin product was evaluated in 105 patients who were retrospectively identified as having ISS in a randomized, open-label, clinical study. Patients were enrolled on the basis of short stature, stimulated GH secretion > 10 ng/mL, and prepubertal status. All patients were observed for height progression for 12 months and were subsequently randomized to this other somatropin product or observation only and followed to final height. Two doses of this other somatropin product were evaluated in this trial: 0.23 mg/kg/week (0.033 mg/kg/day) and 0.47 mg/kg/week (0.067 mg/kg/day). Baseline patient characteristics for the ISS patients who remained prepubertal at randomization (n= 105) were: mean (± SD): chronological age 11.4 (1.3) years, height SDS -2.4 (0.4), height velocity SDS -1.1 (0.8), and height velocity 4.4 (0.9) cm/yr, IGF-1 SDS -0.8 (1.4). Patients were treated for a median duration of 5.7 years. Results for final height SDS are displayed by treatment arm in Table 8 . The observed mean gain in final height was 9.8 cm for females and 5.0 cm for males for both doses combined compared to untreated control subjects. A height gain of 1 SDS was observed in 10% of untreated subjects, 50% of subjects receiving 0.23 mg/kg/week and 69% of subjects receiving 0.47 mg/kg/week.
Table 8 – Final height SDS results for pre-pubertal patients with ISS•
Another Somatropin Product | |||||
Untreated (n=30) | 0.033 mg/kg/day (n=30) | 0.067 mg/kg/day (n=42) | 0.033 vs Untreated (95% CI) | 0.067 vs Untreated (95% CI) | |
Baseline height SDS Final height SDS minus baseline | 0.41 (0.58) | 0.95 (0.75) | 1.36 (0.64) | +0.53 (0.20, 0.87)•• | +0.94 (0.63, 1.26)•• |
Baseline predicted ht Final height SDS minus baseline predicted final height SDS | 0.23 (0.66) | 0.73 (0.63) | 1.05 (0.83) | +0.60 (0.09, 1.11)•• | +0.90 (0.42, 1.39)•• |
Least square means based on ANCOVA (final height SDS and final height SDS minus baseline predicted height SDS were adjusted for baseline height SDS)
• Mean (SD) are observed values
••p<0.05
Growth Failure Due to Prader-Willi Syndrome (PWS)
The safety and efficacy of another somatropin product were evaluated in two randomized, open-label, controlled clinical studies. Patients received either this other somatropin product or no treatment for the first year of the studies, while all patients received this other somatropin product during the second year. This other somatropin product was administered as a daily SC injection, and the dose was calculated for each patient every 3 months. In Study 1, the treatment group received this other somatropin product at a dose of 0.24 mg/kg/week during the entire study. During the second year, the control group received this other somatropin product at a dose of 0.48 mg/kg/week. In Study 2, the treatment group received this other somatropin product at a dose of 0.36 mg/kg/week during the entire study. During the second year, the control group received this other somatropin product at a dose of 0.36 mg/kg/week.
The results are presented in Table 9 . Linear growth continued to increase in the second year, when both groups received treatment with this other somatropin product.
Study 1 | Study 2 | |||
Another Somatropin Product (0.24 mg/kg/week) (n=15) | Untreated Control (n=12) | Another Somatropin Product (0.36 mg/kg/week) (n=7) | Untreated Control (n=9) | |
Linear growth (cm) Baseline height | 112.7 ± 14.9 | 109.5 ± 12.0 | 120.3 ± 17.5 | 120.5 ± 11.2 |
Growth from 0 to 12 months | 11.6• ± 2.3 | 5.0 ± 1.2 | 10.7• ± 2.3 | 4.3 ± 1.5 |
Baseline SDS | -1.6 ± 1.3 | -1.8 ± 1.5 | -2.6 ± 1.7 | -2.1 ± 1.4 |
SDS at 12 months | -0.5• ± 1.3 | -1.9 ± 1.4 | -1.4• ± 1.5 | -2.2 ± 1.4 |
• p <0.05
Adults with Growth Hormone Deficiency (GHD)
A total of six randomized, double-blind, placebo-controlled studies were performed. Two representative studies, one in adult onset (AO) GHD patients and a second in childhood onset (CO) GHD patients, are described below.
Study 1
A single center, randomized, double-blind, placebo-controlled, parallel-group, six month clinical trial was conducted in 31 adults with AO GHD comparing the effects of NORDITROPIN (somatropin) injection and placebo on body composition. Patients in the active treatment arm were treated with NORDITROPIN 0.017 mg/kg/day (not to exceed 1.33 mg/day). The changes from baseline in lean body mass (LBM) and percent total body fat (TBF) were measured by total body potassium (TBP) after 6 months.
Treatment with NORDITROPIN produced a significant increase from baseline in LBM compared to placebo ( Table 10 ).
Table 10 – Lean Body Mass (kg) by TBP
NORDITROPIN (n=15) | Placebo (n=16) | |
Baseline (mean) | 50.27 | 51.72 |
Change from baseline at 6 months (mean) | 1.12 | -0.63 |
Treatment difference (mean) 95% confidence interval p-value | 1.74 (0.65, 2.83) p=0.0028• | |
•Least square mean based on an ANOVA model including treatment and sex as factors
Analysis of the treatment difference on the change from baseline in percent TBF revealed a significant decrease in the NORDITROPIN-treated group compared to the placebo group ( Table 11 ).
Table 11 – Total Body Fat (%) by TBP
NORDITROPIN (n=15) | Placebo (n=16) | |
Baseline (mean) | 44.74 | 42.26 |
Change from baseline at 6 months (mean) | -2.83 | 1.92 |
Treatment difference (mean) 95% confidence interval p-value | -4.74 (-7.18, -2.30) p=0.0004• | |
•Least square mean based on an ANOVA model including treatment and sex as factors
NORDITROPIN also significantly increased serum osteocalcin (a marker of osteoblastic activity).
Study 2
A single center, randomized, double-blind, placebo-controlled, parallel-group, dose-finding, six month clinical trial was conducted in 49 men with CO GHD comparing the effects of NORDITROPIN and placebo on body composition. Patients were randomized to placebo or one of three active treatment groups (0.008, 0.016, and 0.024 mg/kg/day). Thirty three percent of the total dose to which each patient was randomized was administered during weeks 1-4, 67% during weeks 5-8, and 100% for the remainder of the study. The changes from baseline in LBM and percent TBF were measured by TBP after 6 months.
Treatment with NORDITROPIN produced a significant increase from baseline in LBM compared to placebo (pooled data) ( Table 12 ).
Table 12 – Lean Body Mass (kg) by TBP
NORDITROPIN (n=36) | Placebo (n=13) | |
Baseline (mean) | 48.18 | 48.90 |
Change from baseline at 6 months (mean) | 2.06 | 0.70 |
Treatment difference (mean) 95% confidence interval p-value | 1.40 (0.39, 2.41) p=0.0079• | |
•Least square mean based on an ANOVA model including treatment as a factor
Analysis of the treatment difference on the change from baseline in percent TBF revealed a significant decrease in the NORDITROPIN-treated groups (pooled data) compared to the placebo group ( Table 13 ).
Table 13 – Total Body Fat (%) by TBP
NORDITROPIN (n=36) | Placebo (n=13) | |
Baseline (mean) | 34.55 | 34.07 |
Change from baseline at 6 months (mean) | -6.00 | -1.78 |
Treatment difference (mean) 95% confidence interval p-value | -4.24 (-7.11, -1.37) p=0.0048• | |
•Least square mean based on an ANOVA model including treatment as a factor
HOW SUPPLIED/STORAGE AND HANDLING
NORDITROPIN (somatropin) injection is a clear and colorless solution available as FlexPro single-patient-use prefilled pens:
- NORDITROPIN FlexPro 5 mg/1.5 mL (orange) NDC 0169-7704-21
- NORDITROPIN FlexPro 10 mg/1.5 mL (blue) NDC 0169-7705-21
- NORDITROPIN FlexPro 15 mg/1.5 mL (green) NDC 0169-7708-21
- NORDITROPIN FlexPro 30 mg/3 mL (purple) NDC 0169-7703-21
NORDITROPIN 5 mg/1.5 mL, 10 mg/1.5 mL, and 15 mg/1.5 mL FlexPro pens are compatible with FlexPro PenMate. The FlexPro PenMate is an accessory device that is dispensed separately with its enclosed Instructions for Use.
NORDITROPIN 30 mg/3 mL FlexPro pen is not compatible with FlexPro PenMate.
Each NORDITROPIN FlexPro pen is for use by a single patient. A NORDITROPIN FlexPro pen must never be shared between patients, even if the needle is changed.
Unused NORDITROPIN FlexPro prefilled pens must be stored refrigerated at 2°C to 8°C (36°F to 46°F). Do not store directly adjacent to the refrigerator cooling element. Do not freeze. Avoid direct light.
Table 14 – Storage Conditions and Expiration
Before Use | In-use (After 1 st injection) | |
Storage requirement | Storage Option 1 (Refrigeration) | Storage Option 2 (Room temperature) |
2ºC to 8ºC (36ºF to 46ºF) Until exp. date | 2ºC to 8ºC (36ºF to 46ºF) 4 weeks | Up to 25ºC (77ºF) 3 weeks |
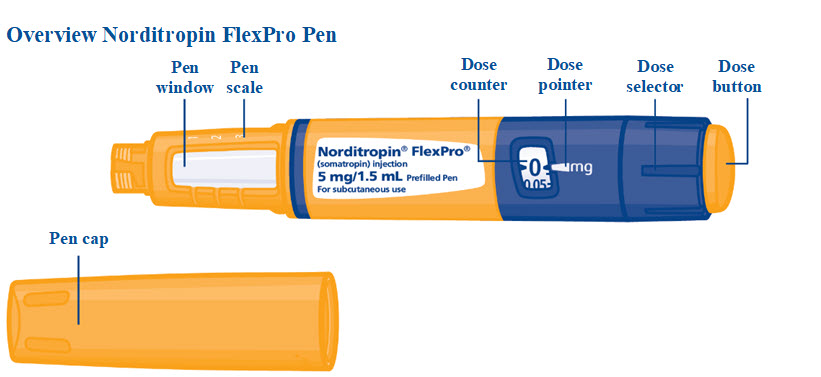
Instructions for Use – 5mg
NORDITROPIN ® [nor-dee-tro-pin] (somatropin) injection, for subcutaneous use 5mg
 | |
 | |
Norditropin FlexPro Pen is for single-patient-use only. | |
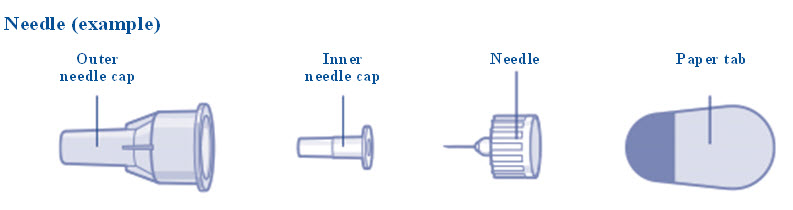
Supplies you will need:
|  |
How to use your Norditropin FlexPro Pen | |
5 steps you should follow for a Norditropin injection:
For further information about your Pen see:
| |
Norditropin is for use under the skin only (subcutaneous). | |
Do not share your Norditropin Pen and needles with another person. You may give another person an infection or get an infection from them. Do not use your Pen without proper training from your healthcare provider . Make sure that you are confident in giving an injection with the Pen before you start your treatment. If you are blind or have poor eyesight and cannot read the dose counter on the Pen, do not use this Pen without help. Get help from a person with good eyesight who is trained to use the Pen. | |
Step 1. Prepare your Norditropin FlexPro Pen | |
| 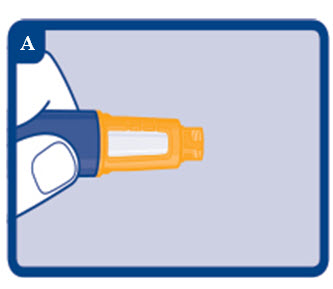 |
| 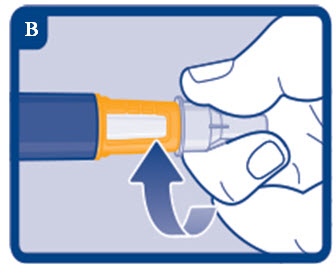 |
ꜝAlways use a new needle for each injection. This reduces the risk of contamination, infection, leakage of Norditropin, and blocked needles leading to incorrect dosing. | |
| 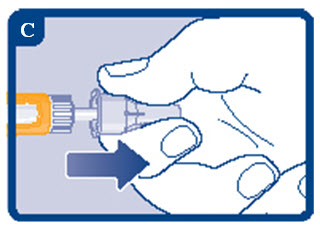 |
|  |
| |
Step 2. Check the Norditropin flow with each new Pen | |
ꜟ If your Pen is already in use , go to step 3.
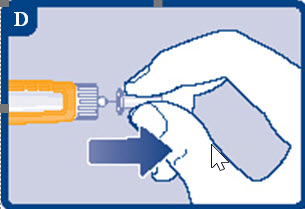
|  |
|  |
|  |
ꜝIf no Norditropin appears , repeat step 2 up to 6 times.
| 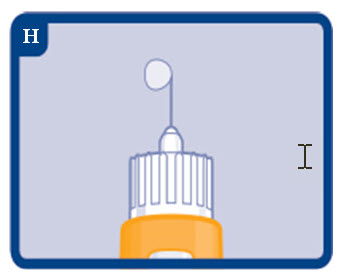 |
Step 3. Select your dose | |
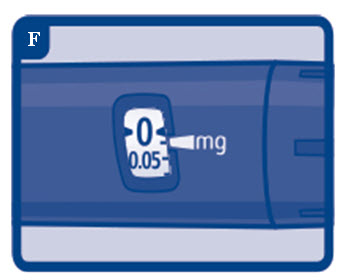
ꜟ If there is not enough Norditropin left to select a full dose, see Frequently Asked Questions . | 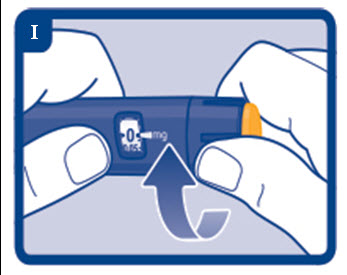 |
ꜟThe dose counter shows the dose in “mg“. See figures J and K. Always use the dose counter to select the exact dose . Do not use the “click“ sounds you hear when you turn the dose selector or the Pen scale to select your dose. Only the dose pointer on the dose counter will show the exact dose selected. | 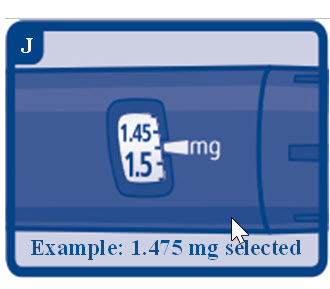 |
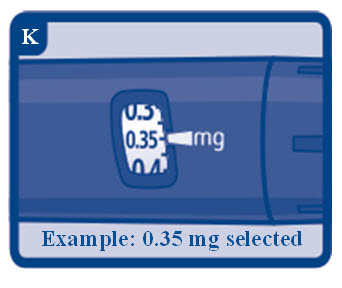 | |
ꜟIf you select the wrong dose, you can turn the dose selector clockwise or counterclockwise to the correct dose. See figure L.
| 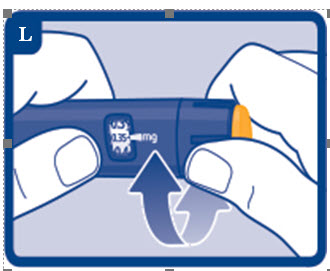 |
Step 4. Inject your dose | |
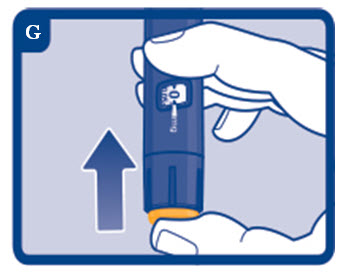
| 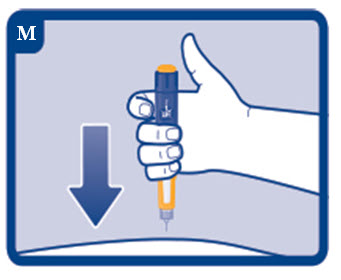 |
ꜟIf “0” does not appear in the dose counter after continuously pressing the dose button, your needle may be blocked or damaged, see Frequently Asked Questions . | 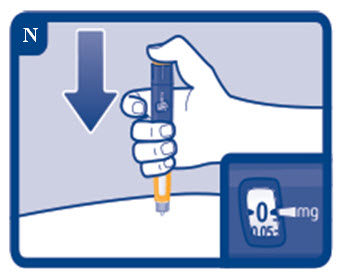 |
| 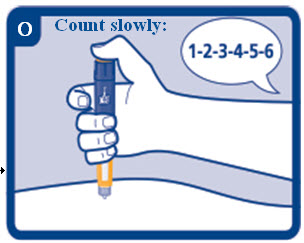 |
ꜟYou may see a drop of Norditropin at the needle tip after injecting. This is normal and does not affect your dose. | 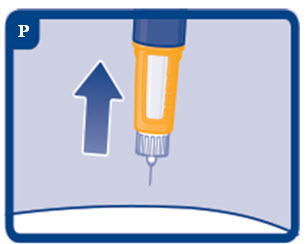 |
Step 5. After your injection | |
|  |
ꜟAlways dispose of the needle after each injection.
|  |
ꜟDo not try to put the needle cap back on . You may stick yourself with the needle. | |
|  |
How should I store Norditropin?
| |
Frequently Asked Questions How do I see how much Norditropin is left in my Pen? | |
The Pen scale shows you approximately how much Norditropin is left in your Pen. See figure T. | 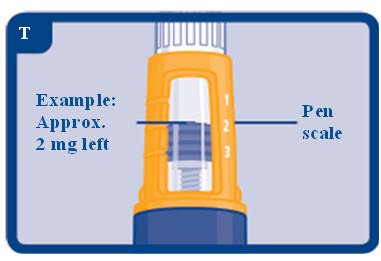 |
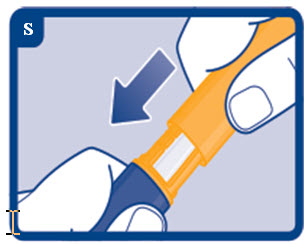
To see how much Norditropin is left in your Pen, use the dose counter: Turn the dose selector clockwise until the dose counter stops. The dose pointer will line up with the number of “mg” left in the Pen. You can select a maximum dose of 2.0 mg. If the dose counter stops with the dose pointer lined up with “2.0”, at least 2.0 mg are left in your Pen. If the dose counter stops with the dose pointer lined up with “1.25”, only 1.25 mg are left in your Pen. See figure U. | 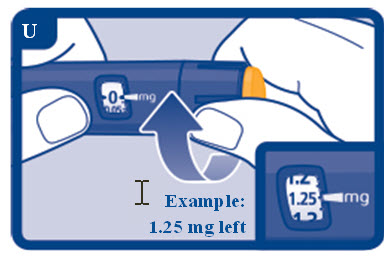 |
What if I need a larger dose than what is left in my Pen? It is not possible to select a larger dose on the dose counter than the number of “mg” left in your Pen. If you need more Norditropin than you have left in your Pen, you can use a new Pen or split your dose between your current Pen and a new Pen. Only split your dose if you have been trained or advised by your healthcare provider on how to do this. You may find it helpful to use a calculator to plan the doses as instructed by your healthcare provider. Be very careful to calculate your split dose correctly so that you do not give the wrong dose . If you are not sure how to split your dose using two Pens, then select and inject the dose you need with a new Pen. | |
What if no Norditropin appears when I check the flow? A. Your needle may be blocked or damaged , if no Norditropin appears at the needle tip. Remove the needle as described in step 5 and repeat steps 1 and 2. B. Your Pen may be defective , if Norditropin still does not appear after changing the needle. Do not use the Pen. Contact Novo Nordisk at 1-888-668-6444. | |
What if “0” does not appear after completing my injection? The needle may be blocked or damaged, and you have not received any Norditropin – even though the dose counter has moved from the dose that you have set. Remove the needle as described in step 5 and repeat steps 1 to 4. If “0” still does not appear after completing the injection, contact Novo Nordisk at 1-888-668-6444. | |
How should I take care of my Pen? Be careful not to drop your Pen or knock it against hard surfaces. Do not expose your Pen to dust, dirt, liquid, or direct light. See “How should I store Norditropin?”. Do not try to refill your Pen, it is already prefilled. When your Pen is empty, throw it away and use a new pen. See “ How do I dispose of used needles and Pens? ”. | |
Frequently Asked Questions | |
What if I drop my Pen? If you drop your Pen or think that something is wrong with it, attach a new disposable needle and check the Norditropin flow before you inject, see steps 1 and 2. Do not try to repair your Pen or pull it apart. | |
How do I clean my Pen? Do not wash, soak, or lubricate your Pen. If necessary, clean it with mild detergent on a moistened cloth. | |
How do I dispose of used needles and Pens? Put your used needles in an FDA-cleared sharps disposal container right away after use. Do not throw away (dispose of) loose needles in your household trash . If you do not have an FDA-cleared sharps disposal container, you may use a household container that is:
When your sharps disposal container is almost full, you will need to follow your community guidelines for the right way to dispose of your sharps disposal container. There may be state or local laws about how you should dispose of used needles and Pens. For more information about safe sharps disposal, and for specific information about safe sharps disposal in the state that you live in, go to the FDA’s website at: http://www.fda.gov/safesharpsdisposal . Do not dispose of your used sharps disposal container in your household trash unless your community guidelines permit this. Do not recycle your used sharps disposal container. When there is not enough medicine left in your Pen for your prescribed dose, the Pen may be thrown away in your household trash after you have removed the needle. | |
ꜟImportant information | |
| |
 | |
This Instructions for Use has been approved by the U.S. Food and Drug Administration. Norditropin ® and FlexPro ® are registered trademarks of Novo Nordisk Health Care AG. Novo Nordisk ® and PenMate ® are registered trademarks of Novo Nordisk A/S. PATENT Information: http://novonordisk-us.com/products/product-patents.html Manufactured by: Novo Nordisk Inc. 800 Scudders Mill Road Plainsboro, NJ 08536 U.S. License No. 1261 For information about NORDITROPIN ® Visit: norditropin.com Or call: 1 (888) 668-6444 Revised: 01/2025 © 2025 Novo Nordisk A/S | |
Mechanism of Action
Somatropin binds to dimeric GH receptors located within the cell membranes of target tissue cells. This interaction results in intracellular signal transduction and subsequent induction of transcription and translation of GH-dependent proteins including IGF-1, IGF BP-3 and acid-labile subunit. Somatropin has direct tissue and metabolic effects or mediated indirectly by IGF-1, including stimulation of chondrocyte differentiation, and proliferation, stimulation hepatic glucose output, protein synthesis and lipolysis.
Somatropin stimulates skeletal growth in pediatric patients with GHD as a result of effects on the growth plates (epiphyses) of long bones. The stimulation of skeletal growth increases linear growth rate (height velocity) in most somatropin-treated pediatric patients. Linear growth is facilitated in part by increased cellular protein synthesis.