Aminocaproic Acid - Aminocaproic Acid tablet
(Aminocaproic Acid)Aminocaproic Acid - Aminocaproic Acid tablet Prescribing Information
Aminocaproic acid is useful in enhancing hemostasis when fibrinolysis contributes to bleeding. In life- threatening situations, transfusion of appropriate blood products and other emergency measures may be required.
Fibrinolytic bleeding may frequently be associated with surgical complications following heart surgery (with or without cardiac bypass procedures) and portacaval shunt; hematological disorders such as amegakaryocytic thrombocytopenia (accompanying aplastic anemia); acute and life-threatening abruptio placentae; hepatic cirrhosis; and neoplastic disease such as carcinoma of the prostate, lung, stomach, and cervix.
Urinary fibrinolysis, usualIy a normal physiological phenomenon, may contribute to excessive urinary tract fibrinolytic bleeding associated with surgical hematuria (following prostatectomy and nephrectomy) or nonsurgical hematuria (accompanying polycystic or neoplastic diseases of the genitourinary system). (See
In patients with upper urinary tract bleeding, aminocaproic acid administration has been known to cause intrarenal obstruction in the form of glomerular capillary thrombosis or clots in the renal pelvis and ureters. For this reason, aminocaproic acid should not be used in hematuria of upper urinary tract origin, unless the possible benefits outweigh the risk.
Subendocardial hemorrhages have been observed in dogs given intravenous infusions of 0.2 times the maximum human therapeutic dose of aminocaproic acid and in monkeys given 8 times the maximum human therapeutic dose of aminocaproic acid.
Fatty degeneration of the myocardium has been reported in dogs given intravenous doses of aminocaproic acid at 0.8 to 3.3 times the maximum human therapeutic dose and in monkeys given intravenous doses of aminocaproic acid at 6 times the maximum human therapeutic dose.
Rarely, skeletal muscle weakness with necrosis of muscle fibers has been reported following prolonged administration. Clinical presentation may range from mild myalgias with weakness and fatigue to a severe proximal myopathy with rhabdomyolysis, myoglobinuria, and acute renal failure. Muscle enzymes, especially creatine phosphokinase (CPK) are elevated. CPK levels should be monitored in patients on long-term therapy. Aminocaproic acid administration should be stopped if a rise in CPK is noted. Resolution follows discontinuation of aminocaproic acid; however, the syndrome may recur if aminocaproic acid is restarted.
The possibility of cardiac muscle damage should also be considered when skeletal myopathy occurs. One case of cardiac and hepatic lesions observed in man has been reported. The patient received 2 g of aminocaproic acid every 6 hours for a total dose of 26 g. Death was due to continued cerebrovascular hemorrhage. Necrotic changes in the heart and liver were noted at autopsy.
In patients with upper urinary tract bleeding, aminocaproic acid administration has been known to cause intrarenal obstruction in the form of glomerular capillary thrombosis or clots in the renal pelvis and ureters. For this reason, aminocaproic acid should not be used in hematuria of upper urinary tract origin, unless the possible benefits outweigh the risk.
Subendocardial hemorrhages have been observed in dogs given intravenous infusions of 0.2 times the maximum human therapeutic dose of aminocaproic acid and in monkeys given 8 times the maximum human therapeutic dose of aminocaproic acid.
Fatty degeneration of the myocardium has been reported in dogs given intravenous doses of aminocaproic acid at 0.8 to 3.3 times the maximum human therapeutic dose and in monkeys given intravenous doses of aminocaproic acid at 6 times the maximum human therapeutic dose.
Rarely, skeletal muscle weakness with necrosis of muscle fibers has been reported following prolonged administration. Clinical presentation may range from mild myalgias with weakness and fatigue to a severe proximal myopathy with rhabdomyolysis, myoglobinuria, and acute renal failure. Muscle enzymes, especially creatine phosphokinase (CPK) are elevated. CPK levels should be monitored in patients on long-term therapy. Aminocaproic acid administration should be stopped if a rise in CPK is noted. Resolution follows discontinuation of aminocaproic acid; however, the syndrome may recur if aminocaproic acid is restarted.
The possibility of cardiac muscle damage should also be considered when skeletal myopathy occurs. One case of cardiac and hepatic lesions observed in man has been reported. The patient received 2 g of aminocaproic acid every 6 hours for a total dose of 26 g. Death was due to continued cerebrovascular hemorrhage. Necrotic changes in the heart and liver were noted at autopsy.
An identical dosage regimen may be followed by administering aminocaproic acid tablets as follows:
For the treatment of acute bleeding syndromes due to elevated fibrinolytic activity, it is suggested that 5 Aminocaproic acid 1000 mg Tablets or 10 Aminocaproic acid 500 mg Tablets (5 g) be administered during the first hour of treatment, followed by a continuing rate of 1 Aminocaproic acid 1000 mg Tablet or 2 Aminocaproic acid 500 mg Tablets (1 g) per hour. This method of treatment would ordinarily be continued for about 8 hours or until the bleeding situation has been controlled.
Aminocaproic acid should not be used when there is evidence of an active intravascular clotting process.
When there is uncertainty as to whether the cause of bleeding is primary fibrinolysis or disseminated intravascular coagulation (DIC), this distinction must be made before administering aminocaproic acid.
The following tests can be applied to differentiate the two conditions:
- Platelet count is usually decreased in DIC but normal in primary fibrinolysis.
- Protamine paracoagulation test is positive in DIC; a precipitate forms when protamine sulfate is dropped into citrated plasma. The test is negative in the presence of primary fibrinolysis.
- The euglobulin clot lysis test is abnormal in primary fibrinolysis but normal in DIC.
Aminocaproic acid must not be used in the presence of DIC without concomitant heparin.
Aminocaproic acid is generally well tolerated. The following adverse experiences have been reported:
In patients with upper urinary tract bleeding, aminocaproic acid administration has been known to cause intrarenal obstruction in the form of glomerular capillary thrombosis or clots in the renal pelvis and ureters. For this reason, aminocaproic acid should not be used in hematuria of upper urinary tract origin, unless the possible benefits outweigh the risk.
Subendocardial hemorrhages have been observed in dogs given intravenous infusions of 0.2 times the maximum human therapeutic dose of aminocaproic acid and in monkeys given 8 times the maximum human therapeutic dose of aminocaproic acid.
Fatty degeneration of the myocardium has been reported in dogs given intravenous doses of aminocaproic acid at 0.8 to 3.3 times the maximum human therapeutic dose and in monkeys given intravenous doses of aminocaproic acid at 6 times the maximum human therapeutic dose.
Rarely, skeletal muscle weakness with necrosis of muscle fibers has been reported following prolonged administration. Clinical presentation may range from mild myalgias with weakness and fatigue to a severe proximal myopathy with rhabdomyolysis, myoglobinuria, and acute renal failure. Muscle enzymes, especially creatine phosphokinase (CPK) are elevated. CPK levels should be monitored in patients on long-term therapy. Aminocaproic acid administration should be stopped if a rise in CPK is noted. Resolution follows discontinuation of aminocaproic acid; however, the syndrome may recur if aminocaproic acid is restarted.
The possibility of cardiac muscle damage should also be considered when skeletal myopathy occurs. One case of cardiac and hepatic lesions observed in man has been reported. The patient received 2 g of aminocaproic acid every 6 hours for a total dose of 26 g. Death was due to continued cerebrovascular hemorrhage. Necrotic changes in the heart and liver were noted at autopsy.
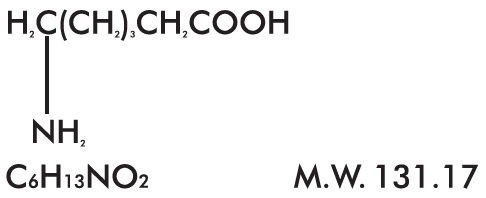
Aminocaproic acid, USP is 6-aminohexanoic acid, which acts as an inhibitor of fibrinolysis. Its chemical structure is:
Aminocaproic acid, USP is soluble in water, acid, and alkaline solutions; it is sparingly soluble in methanol and practically insoluble in chloroform.
Each Aminocaproic Acid Tablet, for oral administration contains 500 mg or 1000 mg of aminocaproic acid and the following inactive ingredients: crospovidone, magnesium stearate, povidone and stearic acid.
The fibrinolysis-inhibitory effects of aminocaproic acid appear to be exerted principally via inhibition of plasminogen activators and to a lesser degree through antiplasmin activity.
In adults, oral absorption appears to be a zero-order process with an absorption rate of 5.2 g/hr. The mean lag time in absorption is 10 minutes. After a single oral dose of 5 g, absorption was complete (F=1). Mean ± SD peak plasma concentrations (164 ± 28 mcg/mL) were reached within 1.2 ± 0.45 hours.
After oral administration, the apparent volume of distribution was estimated to be 23.1 ± 6.6 L (mean± SD). Correspondingly, the volume of distribution after intravenous administration has been reported to be 30.0 ± 8.2 L. After prolonged administration, aminocaproic acid has been found to distribute throughout extravascular and intravascular compartments of the body, penetrating human red blood cells as well as other tissue cells.
Renal excretion is the primary route of elimination. Sixty-five percent of the dose is recovered in the urine as unchanged drug and 11% of the dose appears as the metabolite adipic acid. Renal clearance (116 mL/min) approximates endogenous creatinine clearance. The total body clearance is 169 mL/min. The terminal elimination half-life for aminocaproic acid is approximately 2 hours.