Bleomycin Prescribing Information
It is recommended that Bleomycin for Injection be administered under the supervision of a qualified physician experienced in the use of cancer chemotherapeutic agents. Appropriate management of therapy and complications is possible only when adequate diagnostic and treatment facilities are readily available.
Pulmonary fibrosis is the most severe toxicity associated with Bleomycin for Injection.
The most frequent presentation is pneumonitis occasionally progressing to pulmonary fibrosis. Its occurrence is higher in elderly patients and in those receiving greater than 400 units total dose, but pulmonary toxicity has been observed in young patients and those treated with low doses.
A severe idiosyncratic reaction consisting of hypotension, mental confusion, fever, chills, and wheezing has been reported in approximately 1% of lymphoma patients treated with Bleomycin for Injection.
Bleomycin for Injection should be considered a palliative treatment. It has been shown to be useful in the management of the following neoplasms either as a single agent or in proven combinations with other approved chemotherapeutic agents:
Head and neck (including mouth, tongue, tonsil, nasopharynx, oropharynx, sinus, palate, lip, buccal mucosa, gingivae, epiglottis, skin, larynx), penis, cervix, and vulva. The response to bleomycin is poorer in patients with previously irradiated head and neck cancer.
Hodgkin's disease, non-Hodgkin's lymphoma.
Embryonal cell, choriocarcinoma, and teratocarcinoma.
Bleomycin has also been shown to be useful in the management of:
Bleomycin is effective as a sclerosing agent for the treatment of malignant pleural effusion and prevention of recurrent pleural effusions.
The following dose schedule is recommended:
Pulmonary toxicity of bleomycin appears to be dose-related with a striking increase when the total dose is over 400 units. Total doses over 400 units should be given with great caution.
Improvement of Hodgkin's disease and testicular tumors is prompt and noted within 2 weeks. If no improvement is seen by this time, improvement is unlikely. Squamous cell cancers respond more slowly, sometimes requiring as long as 3 weeks before any improvement is noted.
Sixty units of Bleomycin are dissolved in 50 to 100 mL Sodium Chloride for Injection, 0.9%, USP, and administered through a thoracostomy tube following drainage of excess pleural fluid and confirmation of complete lung expansion. The literature suggests that successful pleurodesis is, in part, dependent upon complete drainage of the pleural fluid and reestablishment of negative intrapleural pressure prior to instillation of a sclerosing agent. Therefore, the amount of drainage from the chest tube should be as minimal as possible prior to instillation of Bleomycin. Although there is no conclusive evidence to support this contention, it is generally accepted that chest tube drainage should be less than 100 mL in a 24-hour period prior to sclerosis. However, Bleomycin instillation may be appropriate when drainage is between 100 to 300 mL under clinical conditions that necessitate sclerosis therapy. The thoracostomy tube is clamped after Bleomcyin instillation. The patient is moved from the supine to the left and right lateral positions several times during the next four hours. The clamp is then removed and suction reestablished. The amount of time the chest tube remains in place following sclerosis is dictated by the clinical situation.
The intrapleural injection of topical anesthetics or systemic narcotic analgesia is generally not required.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
Bleomycin for Injection is contraindicated in patients who have demonstrated a hypersensitive or an idiosyncratic reaction to it.
The most serious side effects are pulmonary adverse reactions, occurring in approximately 10% of treated patients. The most frequent presentation is pneumonitis occasionally progressing to pulmonary fibrosis. Approximately 1% of patients treated have died of pulmonary fibrosis. Pulmonary toxicity is both dose and age related, being more common in patients over 70 years of age and in those receiving over 400 units total dose. This toxicity, however, is unpredictable and has been seen in young patients receiving low doses. Some published reports have suggested that the risk of pulmonary toxicity may be increased when bleomycin is used in combination with G-CSF (filgrastim) or other cytokines. However, randomized clinical studies completed to date have not demonstrated an increased risk of pulmonary complications in patients treated with bleomycin and G-CSF.
Because of lack of specificity of the clinical syndrome, the identification of patients with pulmonary toxicity due to bleomycin sulfate has been extremely difficult. The earliest symptom associated with bleomycin sulfate pulmonary toxicity is dyspnea. The earliest sign is fine rales.
Radiographically, bleomycin-induced pneumonitis produces nonspecific patchy opacities, usually of the lower lung fields. The most common changes in pulmonary function tests are a decrease in total lung volume and a decrease in vital capacity. However, these changes are not predictive of the development of pulmonary fibrosis.
The microscopic tissue changes due to bleomycin toxicity include bronchiolar squamous metaplasia, reactive macrophages, atypical alveolar epithelial cells, fibrinous edema, and interstitial fibrosis. The acute stage may involve capillary changes and subsequent fibrinous exudation into alveoli producing a change similar to hyaline membrane formation and progressing to a diffuse interstitial fibrosis resembling the Hamman-Rich syndrome. These microscopic findings are nonspecific; eg similar changes are seen in radiation pneumonitis and pneumocystic pneumonitis.
To monitor the onset of pulmonary toxicity, roentgenograms of the chest should be taken every 1 to 2 weeks (see
Patients receiving bleomycin must be observed carefully and frequently during and after therapy. It should be used with extreme caution in patients with significant impairment of renal function or compromised pulmonary function.
Pulmonary toxicities occur in 10% of treated patients. In approximately 1%, the nonspecific pneumonitis induced by bleomycin progresses to pulmonary fibrosis and death. Although this is age and dose related, the toxicity is unpredictable. Frequent roentgenograms are recommended (see
A severe idiosyncratic reaction (similar to anaphylaxis) consisting of hypotension, mental confusion, fever, chills, and wheezing has been reported in approximately 1% of lymphoma patients treated with bleomycin. Since these reactions usually occur after the first or second dose, careful monitoring is essential after these doses (see
Renal or hepatic toxicity, beginning as a deterioration in renal or liver function tests, have been reported. These toxicities may occur at any time after initiation of therapy.
Bleomycin can cause fetal harm when administered to a pregnant woman. It has been shown to be teratogenic in rats. Administration of intraperitoneal doses of 1.5 mg/kg/day to rats (about 1.6 times the recommended human dose on a unit/m2basis) on days 6 to 15 of gestation caused skeletal malformations, shortened innominate artery and hydroureter. Bleomycin is abortifacient but not teratogenic in rabbits at intravenous doses of 1.2 mg/kg/day (about 2.4 times the recommended human dose on a unit/m2basis) given on gestation days 6 to 18.
There have been no studies in pregnant women. If Bleomycin for Injection is used during pregnancy, or if the patient becomes pregnant while receiving this drug, the patient should be apprised of the potential hazard to the fetus. Women of childbearing potential should be advised to avoid becoming pregnant during therapy with Bleomycin for Injection.
Because of bleomycin's sensitization of lung tissue, patients who have received bleomycin are at greater risk of developing pulmonary toxicity when oxygen is administered in surgery. While long exposure to very high oxygen concentrations is a known cause of lung damage, after bleomycin administration, lung damage can occur at lower concentrations that are usually considered safe. Suggested preventive measures are:
1. Maintain FIO2 at concentrations approximating that of room air (25%) during surgery and the postoperative period.2. Monitor carefully fluid replacement, focusing more on colloid administration rather than crystalloid.
Sudden onset of an acute chest pain syndrome suggestive of pleuropericarditis has been reported during Bleomycin for Injection infusions. Although each patient must be individually evaluated, further courses of Bleomycin for Injection do not appear to be contraindicated.
Pulmonary adverse events which may be related to the intrapleural administration of Bleomycin have been reported.
Bleomycin for Injection, USP is a mixture of cytotoxic glycopeptide antibiotics isolated from a strain of
It is available as a lyophilized powder for intramuscular, intravenous or subcutaneous injection. Each vial contains sterile bleomycin sulphate equivalent to 15 units or 30 units of bleomycin.
Sulfuric acid or Sodium hydroxide used, if necessary to adjust the pH.
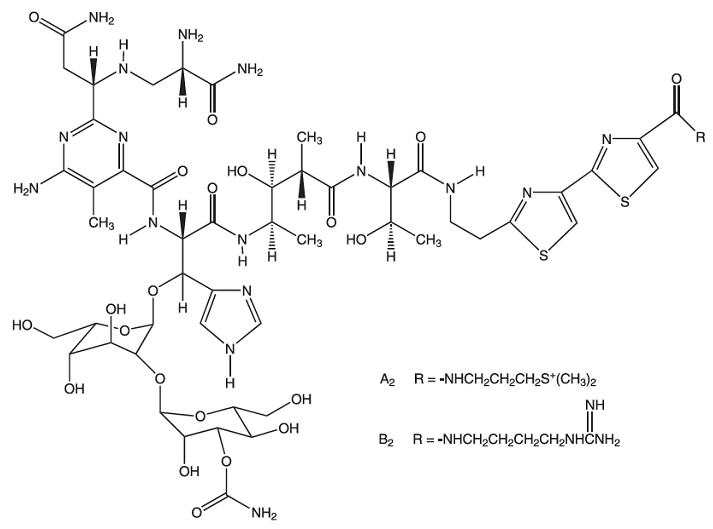
Bleomycins are a group of related basic glycopeptides which differ in the terminal amine substituent of the common structural unit, bleomycin acid. The main components of Bleomycin for Injection are bleomycins A2 and B2. Chemically, bleomycin A2 is N1-[3-(dimethylsulfonio)propyl]-bleomycinamide and bleomycin B2 is N1-[4-(aminoiminomethyl)amino]butyl]-bleomycinamide.
The molecular formula of bleomycin A2 is C55H84N17O21S3 and a calculated molecular weight of 1414. The molecular formula of bleomycin B2 is C55H84N20O21S2 and a calculated molecular weight of 1425. The structural formula of bleomycins A2 and B2 are shown below.