Budesonide
Budesonide Prescribing Information
The recommended starting dose and highest recommended dose of budesonide inhalation suspension, based on prior asthma therapy, are listed in the following table.
Previous Therapy | Recommended Starting Dose | Highest Recommended Dose |
Bronchodilators alone | 0.5 mg total daily dose administered either once daily or twice daily in divided doses | 0.5 mg total daily dose |
Inhaled Corticosteroids | 0.5 mg total daily dose administered either once daily or twice daily in divided doses | 1 mg total daily dose |
Oral Corticosteroids | 1 mg total daily dose administered as 0.5 mg twice daily | 1 mg total daily dose |
Budesonide inhalation suspension is available in two strengths, each containing 2 mL: 0.25 mg/2 mL and 0.5 mg/2 mL. Budesonide inhalation suspension is supplied in sealed aluminum foil envelopes containing one plastic strip of five single-dose vials. There are 30 vials in a carton. Each single-dose vial contains 2 mL of sterile liquid suspension.
There are no adequate well-controlled studies of budesonide inhalation suspension in pregnant women. However, there are published studies on the use of budesonide, the active ingredient in budesonide inhalation suspension, in pregnant women. In animal reproduction studies, budesonide, administered by the subcutaneous route, caused structural abnormalities, was embryocidal, and reduced fetal weights in rats and rabbits at less than the maximum recommended human daily inhalation dose (MRHDID), but these effects were not seen in rats that received inhaled doses approximately 2 times the MRHDID (
The estimated background risk of major birth defects and miscarriage of the indicated populations is unknown. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
In women with poorly or moderately controlled asthma, there is an increased risk of several perinatal adverse outcomes such as preeclampsia in the mother and prematurity, low birth weight, and small for gestational age in the neonate. Pregnant women with asthma should be closely monitored and medication adjusted as necessary to maintain optimal asthma control.
There are no well-controlled human studies that have investigated the effects of budesonide inhalation suspension during labor and delivery.
Studies of pregnant women have not shown that inhaled budesonide increases the risk of abnormalities when administered during pregnancy. The results from a large population-based prospective cohort epidemiological study reviewing data from three Swedish registries covering approximately 99% of the pregnancies from 1995 to 1997 (i.e., Swedish Medical Birth Registry; Registry of Congenital Malformations; Child Cardiology Registry) indicate no increased risk for congenital malformations from the use of inhaled budesonide during early pregnancy. Congenital malformations were studied in 2014 infants born to mothers reporting the use of inhaled budesonide for asthma in early pregnancy (usually 10 to 12 weeks after the last menstrual period), the period when most major organ malformations occur. The rate of recorded congenital malformations was similar compared to the general population rate (3.8% vs. 3.5%, respectively). In addition, after exposure to inhaled budesonide, the number of infants born with orofacial clefts was similar to the expected number in the normal population (4 children vs. 3.3, respectively).
These same data were utilized in a second study bringing the total to 2534 infants whose mothers were exposed to inhaled budesonide. In this study, the rate of congenital malformations among infants whose mothers were exposed to inhaled budesonide during early pregnancy was not different from the rate for all newborn babies during the same period (3.6%).
In a fertility and reproduction study, male rats were subcutaneously dosed for 9 weeks and females for 2 weeks prior to pairing and throughout the mating period. Females were dosed up until weaning of their offspring. Budesonide caused a decrease in prenatal viability and viability in the pups at birth and during lactation, along with a decrease in maternal body-weight gain, at doses 0.2 times the MRHDID (on a mcg/m2 basis at maternal subcutaneous doses of 20 mcg/kg/day and above). No such effects were noted at a dose 0.05 times the MRHDID (on a mcg/m2 basis at a maternal subcutaneous dose of 5 mcg/kg/day).
In an embryo-fetal development study in pregnant rabbits dosed during the period of organogenesis from gestation days 6 to 18, budesonide produced fetal loss, decreased fetal weight, and skeletal abnormalities at doses 0.5 times the MRHDID (on a mcg/m2 basis at a maternal subcutaneous dose of 25 mcg/kg/day). In an embryo-fetal development study in pregnant rats dosed during the period of organogenesis from gestation days 6-15, budesonide produced similar adverse fetal effects at doses approximately 5 times the MRHDID (on a mcg/m2 basis at a maternal subcutaneous dose of 500 mcg/kg/day). In another embryo-fetal development study in pregnant rats, no structural abnormalities or embryocidal effects were seen at doses approximately 2 times the MRHDID (on a mcg/m2 basis at maternal inhalation doses up to 250 mcg/kg/day).
In a peri-and post-natal development study, rats dosed from gestation day 15 to postpartum day 21, budesonide had no effects on delivery, but did have an effect on growth and development of offspring. Offspring survival was reduced and surviving offspring had decreased mean body weights at birth and during lactation at doses less than 0.2 times the MRHDID and higher (on a mcg/m2 basis at maternal subcutaneous doses of 20 mcg/kg/day and higher). These findings occurred in the presence of maternal toxicity.
The use of budesonide inhalation suspension is contraindicated in the following conditions:
- Primary treatment of status asthmaticus or other acute episodes of asthma where intensive measures are required.
- Hypersensitivity to budesonide or any of the ingredients of budesonide inhalation suspension [see Warnings and Precautions (,), Description (
5.3 Hypersensitivity Reactions Including AnaphylaxisHypersensitivity reactions including anaphylaxis, rash, contact dermatitis, urticaria, angioedema, and bronchospasm have been reported with use of budesonide inhalation suspension. Discontinue budesonide inhalation suspension if such reactions occur [see
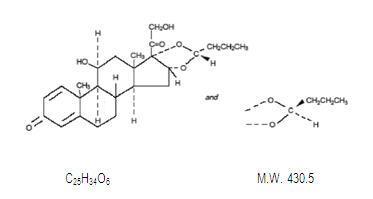
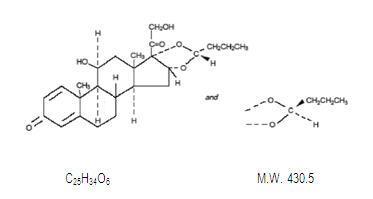
Contraindications].)11 DESCRIPTIONBudesonide, USP, the active component of budesonide inhalation suspension, is a corticosteroid designated chemically as (RS)-11β,16α,17,21-tetrahydroxypregna-1,4-diene-3,20-dione cyclic 16,17-acetal with butyraldehyde. Budesonide, USP is provided as a mixture of two epimers (22R and 22S) and it has the following structural formula:
Budesonide, USP is a white to off-white, tasteless, odorless powder that is practically insoluble in water and in heptane, sparingly soluble in ethanol, and freely soluble in chloroform. Its partition coefficient between octanol and water at pH 7.4 is 1.6 x 103.
Budesonide inhalation suspension is a sterile suspension for inhalation via jet nebulizer and contains the active ingredient budesonide, USP (micronized), and the inactive ingredients: citric acid monohydrate, disodium edetate, polysorbate 80, sodium chloride, tri-sodium citrate dihydrate and water for injection.
Two dose strengths are available in single-dose vials: 0.25 mg and 0.5 mg per 2 mL vial. For budesonide inhalation suspension, like all other nebulized treatments, the amount delivered to the lungs will depend on patient factors, the jet nebulizer utilized, and compressor performance. Using the Pari-LC-Jet Plus®Nebulizer/Pari Master®compressor system, under
in vitroconditions, the mean delivered dose at the mouthpiece (% nominal dose) was approximately 17% at a mean flow rate of 5.5 L/min. The mean nebulization time was 5 minutes or less. Budesonide inhalation suspension should be administered from jet nebulizers at adequate flow rates, via face masks or mouthpieces [seeDosage and Administration].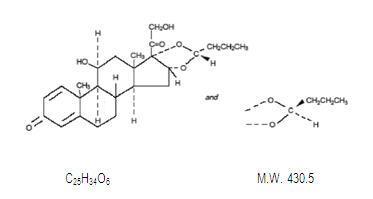
Chemical structure for budesonide Adverse Reactions (].)6.2 Postmarketing ExperienceThe following adverse reactions have been reported during post-approval use of budesonide inhalation suspension. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. Some of these adverse reactions may also have been observed in clinical studies with budesonide inhalation suspension.
Endocrine disorders:symptoms of hypocorticism and hypercorticism [seeWarnings and Precautions]Eye disorders:cataracts, glaucoma, increased intraocular pressure [seeWarnings and Precautions]General disorders and administration site conditions:fever, painImmune system disorders:immediate and delayed hypersensitivity reactions including, anaphylaxis, angioedema, bronchospasm, rash, contact dermatitis, and urticaria [seeContraindications,Warnings and Precautions]Infection and Infestation:sinusitis, pharyngitis, bronchitisMusculoskeletal and connective tissue disorders:avascular necrosis of the femoral head, osteoporosis, growth suppressionNervous system disorders:headachePsychiatric disorders:psychiatric symptoms including psychosis, depression, aggressive reactions, irritability, nervousness, restlessness, and anxietyRespiratory, thoracic, and mediastinal disorders:cough, dysphonia and throat irritationSkin and subcutaneous tissue disorders:skin bruising, facial skin irritationCases of growth suppression have been reported for inhaled corticosteroids including postmarketing reports for budesonide inhalation suspension [see
Warnings and Precautions , Use in Specific Populations].
Systemic and inhaled corticosteroid use may result in the following:
- Candida albicansInfection [seeWarnings and Precautions (])
5.1 Local EffectsIn clinical trials with budesonide inhalation suspension, localized infections with
Candida albicansoccurred in the mouth and pharynx in some patients. The incidences of localized infections ofCandida albicanswere similar between the placebo and budesonide inhalation suspension treatment groups. If these infections develop, they may require treatment with appropriate local or systemic antifungal therapy and/or discontinuance of treatment with budesonide inhalation suspension. Patients should rinse the mouth after inhalation of budesonide inhalation suspension. - Hypersensitivity Reactions Including Anaphylaxis [see Warnings and Precautions (])
5.3 Hypersensitivity Reactions Including AnaphylaxisHypersensitivity reactions including anaphylaxis, rash, contact dermatitis, urticaria, angioedema, and bronchospasm have been reported with use of budesonide inhalation suspension. Discontinue budesonide inhalation suspension if such reactions occur [see
Contraindications]. - Immunosuppression [see Warnings and Precautions (])
5.4 ImmunosuppressionPatients who are on drugs that suppress the immune system are more susceptible to infection than healthy individuals. Chicken pox and measles, for example, can have a more serious or even fatal course in susceptible children or adults using corticosteroids. In children or adults who have not had these diseases, or been properly immunized, particular care should be taken to avoid exposure. How the dose, route, and duration of corticosteroid administration affect the risk of developing a disseminated infection is not known. The contribution of the underlying disease and/or prior corticosteroid treatment to the risk is also not known. If exposed to chicken pox, therapy with varicella zoster immune globulin (VZIG) or pooled intravenous immunoglobulin (IVIG), as appropriate, may be indicated. If exposed to measles, prophylaxis with pooled intramuscular immunoglobulin (IG) may be indicated (see the respective package inserts for complete VZIG and IG prescribing information). If chicken pox develops, treatment with antiviral agents may be considered.
The clinical course of chicken pox or measles infection in patients on inhaled corticosteroids has not been studied. However, a clinical study has examined the immune responsiveness of asthma patients 12 months to 8 years of age who were treated with budesonide inhalation suspension. An open-label non-randomized clinical study examined the immune responsiveness of varicella vaccine in 243 asthma patients 12 months to 8 years of age who were treated with budesonide inhalation suspension 0.25 mg to 1 mg daily (n=151) or non-corticosteroid asthma therapy (n=92) (i.e., beta2-agonists, leukotriene receptor antagonists, cromones). The percentage of patients developing a seroprotective antibody titer of ≥5.0 (gpELISA value) in response to the vaccination was similar in patients treated with budesonide inhalation suspension (85%) compared to patients treated with non-corticosteroid asthma therapy (90%). No patient treated with budesonide inhalation suspension developed chicken pox as a result of vaccination.
Inhaled corticosteroids should be used with caution, if at all, in patients with active or quiescent tuberculosis infection of the respiratory tract, untreated systemic fungal, bacterial, viral, or parasitic infections; or ocular herpes simplex.
- Hypercorticism and Adrenal Suppression [see Warnings and Precautions (])
5.6 Hypercorticism and Adrenal SuppressionBudesonide inhalation suspension will often help control asthma symptoms with less suppression of HPA function than therapeutically equivalent oral doses of prednisone. Since individual sensitivity to effects on cortisol production exists, physicians should consider this information when prescribing budesonide inhalation suspension. Because of the possibility of systemic absorption of inhaled corticosteroids, patients treated with budesonide inhalation suspension should be observed carefully for any evidence of systemic corticosteroid effects. Particular care should be taken in observing patients post-operatively or during periods of stress for evidence of inadequate adrenal response. It is possible that systemic corticosteroid effects such as hypercorticism, and adrenal suppression (including adrenal crisis) may appear in a small number of patients, particularly when budesonide is administered at higher than recommended doses over prolonged periods of time. If such effects occur, the dosage of budesonide inhalation suspension should be reduced slowly, consistent with accepted procedures for tapering of systemic corticosteroids and for management of asthma.
- Reduction in Bone Mineral Density [see Warnings and Precautions (])
5.7 Reduction in Bone Mineral DensityDecreases in bone mineral density (BMD) have been observed with long-term administration of products containing inhaled corticosteroids. The clinical significance of small changes in BMD with regard to long-term outcomes is unknown. Patients with major risk factors for decreased bone mineral content, such as prolonged immobilization, family history of osteoporosis, poor nutrition, or chronic use of drugs that can reduce bone mass (e.g., anticonvulsants and corticosteroids), should be monitored and treated with established standards of care.
- Growth Effects in Pediatric Patients [see Warnings and Precautions (]), Use in Specific Populations (
5.8 Effects on GrowthOrally inhaled corticosteroids, including budesonide, may cause a reduction in growth velocity when administered to pediatric patients. Monitor the growth of pediatric patients receiving budesonide inhalation suspension routinely (e.g., via stadiometry). To minimize the systemic effects of orally inhaled corticosteroids, including budesonide inhalation suspension, each patient should be titrated to his/her lowest effective dose [see
Use in Specific Populations].)8.4 Pediatric UseSafety and effectiveness in children six months to 12 months of age has been evaluated but not established. Safety and effectiveness in children 12 months to 8 years of age have been established [see
Clinical Pharmacology , Adverse Reactions].A 12 week study in 141 pediatric patients 6 to 12 months of age with mild to moderate asthma or recurrent/persistent wheezing was conducted. All patients were randomized to receive either 0.5 mg or 1 mg of budesonide inhalation suspension or placebo once daily. Adrenal-axis function was assessed with an ACTH stimulation test at the beginning and end of the study, and mean changes from baseline in this variable did not indicate adrenal suppression in patients who received budesonide inhalation suspension versus placebo. However, on an individual basis, 7 patients in this study (6 in the budesonide inhalation suspension treatment arms and 1 in the placebo arm) experienced a shift from having a normal baseline stimulated cortisol level to having a subnormal level at Week 12 [
see Clinical Pharmacology]. Pneumonia was observed more frequently in patients treated with budesonide inhalation suspension than in patients treated with placebo, (N = 2, 1, and 0) in the budesonide inhalation suspension 0.5 mg, 1 mg, and placebo groups, respectively.A dose dependent effect on growth was also noted in this 12 week trial. Infants in the placebo arm experienced an average growth of 3.7 cm over 12 weeks compared with 3.5 cm and 3.1 cm in the budesonide inhalation suspension 0.5 mg and 1 mg arms respectively. This corresponds to estimated mean (95% CI) reductions in 12 week growth velocity between placebo and budesonide inhalation suspension 0.5 mg of 0.2 cm (-0.6 to 1.0) and between placebo and budesonide inhalation suspension 1 mg of 0.6 cm (-0.2 to 1.4). These findings support that the use of budesonide inhalation suspension in infants 6 to 12 months of age may result in systemic effects and are consistent with findings of growth suppression in other studies with inhaled corticosteroids.
Controlled clinical studies have shown that inhaled corticosteroids may cause a reduction in growth velocity in pediatric patients. In these studies, the mean reduction in growth velocity was approximately one centimeter per year (range 0.3 to 1.8 cm per year) and appears to be related to dose and duration of exposure. This effect has been observed in the absence of laboratory evidence of hypothalamic-pituitary-adrenal (HPA)-axis suppression, suggesting that growth velocity is a more sensitive indicator of systemic corticosteroid exposure in pediatric patients than some commonly used tests of HPA-axis function. The long-term effects of this reduction in growth velocity associated with orally inhaled corticosteroids, including the impact on final adult height, are unknown. The potential for “catch up” growth following discontinuation of treatment with orally inhaled corticosteroids has not been adequately studied.
In a study of asthmatic children 5 to 12 years of age, those treated with budesonide administered via a dry powder inhaler 200 mcg twice daily (n=311) had a 1.1 centimeter reduction in growth compared with those receiving placebo (n=418) at the end of one year; the difference between these two treatment groups did not increase further over three years of additional treatment. By the end of four years, children treated with the budesonide dry powder inhaler and children treated with placebo had similar growth velocities. Conclusions drawn from this study may be confounded by the unequal use of corticosteroids in the treatment groups and inclusion of data from patients attaining puberty during the course of the study.
The growth of pediatric patients receiving inhaled corticosteroids, including budesonide inhalation suspension, should be monitored routinely (e.g., via stadiometry). The potential growth effects of prolonged treatment should be weighed against clinical benefits obtained and the risks and benefits associated with alternative therapies. To minimize the systemic effects of inhaled corticosteroids, including budesonide inhalation suspension, each patient should be titrated to his/her lowest effective dose [see
Dosage and Administration , Warnings and Precautions]. - Glaucoma, Increased Intraocular Pressure and Cataracts [seeWarnings and Precautions (])
5.9 Glaucoma and CataractsGlaucoma, increased intraocular pressure, and cataracts have been reported following the long-term administration of inhaled corticosteroids, including budesonide. Therefore, close monitoring is warranted in patients with a change in vision or with a history of increased intraocular pressure, glaucoma, and/or cataracts.
- Eosinophilic Conditions and Churg-Strauss Syndrome [see Warnings and Precautions (])
5.11 Eosinophilic Conditions and Churg-Strauss SyndromeIn rare cases, patients on inhaled corticosteroids may present with systemic eosinophilic conditions. Some of these patients have clinical features of vasculitis consistent with Churg-Strauss syndrome, a condition that is often treated with systemic corticosteroids therapy. These events usually, but not always, have been associated with the reduction and/or withdrawal of oral corticosteroid therapy following the introduction of inhaled corticosteroids. Healthcare providers should be alert to eosinophilia, vasculitis rash, worsening pulmonary symptoms, cardiac complications, and/or neuropathy presenting in their patients. A causal relationship between budesonide and these underlying conditions has not been established.
Budesonide, USP, the active component of budesonide inhalation suspension, is a corticosteroid designated chemically as (RS)-11β,16α,17,21-tetrahydroxypregna-1,4-diene-3,20-dione cyclic 16,17-acetal with butyraldehyde. Budesonide, USP is provided as a mixture of two epimers (22R and 22S) and it has the following structural formula:
Budesonide, USP is a white to off-white, tasteless, odorless powder that is practically insoluble in water and in heptane, sparingly soluble in ethanol, and freely soluble in chloroform. Its partition coefficient between octanol and water at pH 7.4 is 1.6 x 103.
Budesonide inhalation suspension is a sterile suspension for inhalation via jet nebulizer and contains the active ingredient budesonide, USP (micronized), and the inactive ingredients: citric acid monohydrate, disodium edetate, polysorbate 80, sodium chloride, tri-sodium citrate dihydrate and water for injection.
Two dose strengths are available in single-dose vials: 0.25 mg and 0.5 mg per 2 mL vial. For budesonide inhalation suspension, like all other nebulized treatments, the amount delivered to the lungs will depend on patient factors, the jet nebulizer utilized, and compressor performance. Using the Pari-LC-Jet Plus® Nebulizer/Pari Master® compressor system, under
The recommended starting dose and highest recommended dose of budesonide inhalation suspension, based on prior asthma therapy, are listed in the following table.
Previous Therapy | Recommended Starting Dose | Highest Recommended Dose |
Bronchodilators alone | 0.5 mg total daily dose administered either once daily or twice daily in divided doses | 0.5 mg total daily dose |
Inhaled Corticosteroids | 0.5 mg total daily dose administered either once daily or twice daily in divided doses | 1 mg total daily dose |
Oral Corticosteroids | 1 mg total daily dose administered as 0.5 mg twice daily | 1 mg total daily dose |
Recommended dosing based on previous therapy . Start with the lowest recommended dose:
- Bronchodilators alone: 0.5 mg once daily or 0.25 mg twice daily
- Inhaled corticosteroids: 0.5 mg once daily or 0.25 mg twice daily up to 0.5 mg twice daily
- Oral corticosteroids: 0.5 mg twice daily
- In symptomatic children not responding to non-steroidal therapy, a starting dose of 0.25 mg once daily may be considered
- If once-daily treatment does not provide adequate control, the total daily dose should be increased and/or administered as a divided dose. Once asthma stability is achieved, titrate the dose downwards.
- For inhalation use via compressed air driven jet nebulizers only (not for use with ultrasonic devices). Not for injection.
Dosing recommendations based on previous therapy are as follows:
- Bronchodilators alone: 0.5 mg once daily or 0.25 mg twice daily
- Inhaled corticosteroids: 0.5 mg once daily or 0.25 mg twice daily up to 0.5 mg twice daily
- Oral corticosteroids: 0.5 mg twice daily
In symptomatic children not responding to non-steroidal therapy, a starting dose of 0.25 mg once daily may be considered. If once-daily treatment does not provide adequate control, the total daily dose should be increased and/or administered as a divided dose. In all patients, it is desirable to downward-titrate to the lowest effective dose once asthma stability is achieved.
Budesonide inhalation suspension should be administered via jet nebulizer connected to an air compressor with an adequate air flow, equipped with a mouthpiece or suitable face mask. Ultrasonic nebulizers are not suitable for the adequate administration of budesonide inhalation suspension and, therefore, are NOT recommended.
The effects of mixing budesonide inhalation suspension with other nebulizable medications have not been adequately assessed. Budesonide inhalation suspension should be administered separately in the nebulizer [see
A Pari-LC-Jet Plus®Nebulizer (with face mask or mouthpiece) connected to a Pari Master®compressor was used to deliver budesonide inhalation suspension to each patient in 3 U.S. controlled clinical studies. The safety and efficacy of budesonide inhalation suspension delivered by other nebulizers and compressors have not been established.