Calcitriol
Calcitriol Prescribing Information
Calcitriol capsules re indicated in the management of secondary hyperparathyroidism and resultant metabolic bone disease in patients with moderate to severe chronic renal failure (Ccr 15 to 55 mL/min) not yet on dialysis. In children, the creatinine clearance value must be corrected for a surface area of 1.73 square meters. A serum iPTH level of ≥100 pg/mL is strongly suggestive of secondary hyperparathyroidism.
Calcitriol capsules are indicated in the management of hypocalcemia and the resultant metabolic bone disease in patients undergoing chronic renal dialysis. In these patients, calcitriol capsules administration enhances calcium absorption, reduces serum alkaline phosphatase levels, and may reduce elevated parathyroid hormone levels and the histological manifestations of osteitis fibrosa cystica and defective mineralization.
Calcitriol capsules are also indicated in the management of hypocalcemia and its clinical manifestations in patients with postsurgical hypoparathyroidism, idiopathic hypoparathyroidism, and pseudohypoparathyroidism.
The optimal daily dose of calcitriol capsules must be carefully determined for each patient. Calcitriol capsules are administered orally as a capsule (0.25 mcg or 0.50 mcg). Calcitriol capsules therapy should always be started at the lowest possible dose and should not be increased without careful monitoring of serum calcium.
The effectiveness of calcitriol capsules therapy is predicated on the assumption that each patient is receiving an adequate but not excessive daily intake of calcium. Patients are advised to have a dietary intake of calcium at a minimum of 600 mg daily. The U.S. RDA for calcium in adults is 800 mg to 1200 mg. To ensure that each patient receives an adequate daily intake of calcium, the physician should either prescribe a calcium supplement or instruct the patient in proper dietary measures.
Because of improved calcium absorption from the gastrointestinal tract, some patients on calcitriol capsules may be maintained on a lower calcium intake. Patients who tend to develop hypercalcemia may require only low doses of calcium or no supplementation at all.
During the titration period of treatment with calcitriol capsules, serum calcium levels should be checked at least twice weekly. When the optimal dosage of calcitriol capsules has been determined, serum calcium levels should be checked every month (or as given below for individual indications). Samples for serum calcium estimation should be taken without a tourniquet.
The recommended initial dose of calcitriol capsules is 0.25 mcg/day. If a satisfactory response in the biochemical parameters and clinical manifestations of the disease state is not observed, dosage may be increased by 0.25 mcg/day at 4- to 8-week intervals. During this titration period, serum calcium levels should be obtained at least twice weekly, and if hypercalcemia is noted, the drug should be immediately discontinued until normocalcemia ensues (see
Patients with normal or only slightly reduced serum calcium levels may respond to calcitriol capsules doses of 0.25 mcg every other day. Most patients undergoing hemodialysis respond to doses between 0.5 and 1 mcg/day.
Oral calcitriol capsules may normalize plasma-ionized calcium in some uremic patients, yet fail to suppress parathyroid hyperfunction. In these individuals with autonomous parathyroid hyperfunction, oral calcitriol capsules may be useful to maintain normocalcemia, but has not been shown to be adequate treatment for hyperparathyroidism.
Calcitriol, USP should not be given to patients with hypercalcemia or evidence of vitamin D toxicity. Use of calcitriol capsules in patients with known hypersensitivity to calcitriol, USP (or drugs of the same class) or any of the inactive ingredients is contraindicated.
Since calcitriol is believed to be the active hormone which exerts vitamin D activity in the body, adverse effects are, in general, similar to those encountered with excessive vitamin D intake, i.e., hypercalcemia syndrome or calcium intoxication, depending on the severity and duration of hypercalcemia (see
Overdosage of any form of vitamin D is dangerous (see
Calcitriol is the most potent metabolite of vitamin D available. The administration of calcitriol to patients in excess of their daily requirements can cause hypercalcemia, hypercalciuria, and hyperphosphatemia. Therefore, pharmacologic doses of vitamin D and its derivatives should be withheld during calcitriol treatment to avoid possible additive effects and hypercalcemia. If treatment is switched from ergocalciferol (vitamin D2) to calcitriol, it may take several months for the ergocalciferol level in the blood to return to the baseline value (see
Calcitriol increases inorganic phosphate levels in serum. While this is desirable in patients with hypophosphatemia, caution is called for in patients with renal failure because of the danger of ectopic calcification. A nonaluminum phosphate-binding compound and a low-phosphate diet should be used to control serum phosphorus levels in patients undergoing dialysis.
Magnesium-containing preparations (eg, antacids) and calcitriol should not be used concomitantly in patients on chronic renal dialysis because such use may lead to the development of hypermagnesemia.
Studies in dogs and rats given calcitriol for up to 26 weeks have shown that small increases of calcitriol above endogenous levels can lead to abnormalities of calcium metabolism with the potential for calcification of many tissues in the body.
The early and late signs and symptoms of vitamin D intoxication associated with hypercalcemia include:
In clinical studies on hypoparathyroidism and pseudohypoparathyroidism, hypercalcemia was noted on at least one occasion in about 1 in 3 patients and hypercalciuria in about 1 in 7 patients. Elevated serum creatinine levels were observed in about 1 in 6 patients (approximately one half of whom had normal levels at baseline).
In concurrent hypercalcemia and hyperphosphatemia, soft-tissue calcification may occur; this can be seen radiographically (see
Overdosage of any form of vitamin D is dangerous (see
Calcitriol is the most potent metabolite of vitamin D available. The administration of calcitriol to patients in excess of their daily requirements can cause hypercalcemia, hypercalciuria, and hyperphosphatemia. Therefore, pharmacologic doses of vitamin D and its derivatives should be withheld during calcitriol treatment to avoid possible additive effects and hypercalcemia. If treatment is switched from ergocalciferol (vitamin D2) to calcitriol, it may take several months for the ergocalciferol level in the blood to return to the baseline value (see
Calcitriol increases inorganic phosphate levels in serum. While this is desirable in patients with hypophosphatemia, caution is called for in patients with renal failure because of the danger of ectopic calcification. A nonaluminum phosphate-binding compound and a low-phosphate diet should be used to control serum phosphorus levels in patients undergoing dialysis.
Magnesium-containing preparations (eg, antacids) and calcitriol should not be used concomitantly in patients on chronic renal dialysis because such use may lead to the development of hypermagnesemia.
Studies in dogs and rats given calcitriol for up to 26 weeks have shown that small increases of calcitriol above endogenous levels can lead to abnormalities of calcium metabolism with the potential for calcification of many tissues in the body.
In patients with normal renal function, chronic hypercalcemia may be associated with an increase in serum creatinine (see
Hypersensitivity reactions (pruritus, rash, urticaria, and very rarely severe erythematous skin disorders) may occur in susceptible individuals. One case of erythema multiforme and one case of allergic reaction (swelling of lips and hives all over the body) were confirmed by rechallenge.
Calcitriol is a synthetic vitamin D analog which is active in the regulation of the absorption of calcium from the gastrointestinal tract and its utilization in the body. Calcitriol capsules are available as containing either 0.25 mcg or 0.5 mcg calcitriol, USP. Calcitriol capsules contain butylated hydroxyanisole (BHA) and butylated hydroxytoluene (BHT) as antioxidants. The capsules also contain medium chain triglycerides. Gelatin capsule shells contain FD&C Yellow No. 6, gelatin, glycerin, methyl paraben sodium, propyl paraben sodium, purified water, and titanium dioxide. The 0.5 mcg capsules also contain FD&C Red No. 40.
Calcitriol, USP is a white, crystalline compound which occurs naturally in humans. It has a calculated molecular weight of 416.65 and is soluble in organic solvents but relatively insoluble in water. Chemically, calcitriol, USP is 9,10- seco(5Z,7E)-5,7,10(19)-cholestatriene-1α, 3β, 25-triol and has the following structural formula:
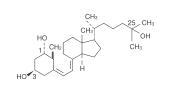
The other names frequently used for calcitriol, USP are 1α,25-dihydroxycholecalciferol, 1,25-dihydroxyvitamin D3, 1,25-DHCC, 1,25(OH)2D3 and 1,25-diOHC.
Man's natural supply of vitamin D depends mainly on exposure to the ultraviolet rays of the sun for conversion of 7-dehydrocholesterol in the skin to vitamin D3 (cholecalciferol). Vitamin D3 must be metabolically activated in the liver and the kidney before it is fully active as a regulator of calcium and phosphorus metabolism at target tissues. The initial transformation of vitamin D3 is catalyzed by a vitamin D3-25-hydroxylase enzyme (25-OHase) present in the liver, and the product of this reaction is 25-hydroxyvitamin D3 [25-(OH)D3]. Hydroxylation of 25-(OH)D3 occurs in the mitochondria of kidney tissue, activated by the renal 25-hydroxyvitamin D3-1 alpha-hydroxylase (alpha-OHase), to produce 1,25-(OH)2D3 (calcitriol), the active form of vitamin D3. Endogenous synthesis and catabolism of calcitriol, as well as physiological control mechanisms affecting these processes, play a critical role regulating the serum level of calcitriol. Physiological daily production is normally 0.5 to 1 mcg and is somewhat higher during periods of increased bone synthesis (eg, growth or pregnancy).
The two known sites of action of calcitriol are intestine and bone. A calcitriol receptor-binding protein appears to exist in the mucosa of human intestine. Additional evidence suggests that calcitriol may also act on the kidney and the parathyroid glands. Calcitriol is the most active known form of vitamin D3 in stimulating intestinal calcium transport. In acutely uremic rats calcitriol has been shown to stimulate intestinal calcium absorption.
The kidneys of uremic patients cannot adequately synthesize calcitriol, the active hormone formed from precursor vitamin D. Resultant hypocalcemia and secondary hyperparathyroidism are a major cause of the metabolic bone disease of renal failure. However, other bone-toxic substances which accumulate in uremia (eg, aluminum) may also contribute.
The beneficial effect of calcitriol in renal osteodystrophy appears to result from correction of hypocalcemia and secondary hyperparathyroidism. It is uncertain whether calcitriol produces other independent beneficial effects. Calcitriol treatment is not associated with an accelerated rate of renal function deterioration. No radiographic evidence of extraskeletal calcification has been found in predialysis patients following treatment. The duration of pharmacologic activity of a single dose of calcitriol is about 3 to 5 days.
Calcitriol is rapidly absorbed from the intestine. Peak serum concentrations (above basal values) were reached within 3 to 6 hours following oral administration of single doses of 0.25 to 1 mcg of calcitriol. Following a single oral dose of 0.5 mcg, mean serum concentrations of calcitriol rose from a baseline value of 40±4.4 (SD) pg/mL to 60±4.4 pg/mL at 2 hours, and declined to 53±6.9 at 4 hours, 50±7 at 8 hours, 44±4.6 at 12 hours, and 41.5±5.1 at 24 hours.
Following multiple-dose administration, serum calcitriol levels reached steady-state within 7 days.
Calcitriol is approximately 99.9% bound in blood. Calcitriol and other vitamin D metabolites are transported in blood, by an alpha-globulin vitamin D binding protein. There is evidence that maternal calcitriol may enter the fetal circulation. Calcitriol is transferred into human breast milk at low levels (ie, 2.2±0.1 pg/mL).
Enterohepatic recycling and biliary excretion of calcitriol occur. The metabolites of calcitriol are excreted primarily in feces. Following intravenous administration of radiolabeled calcitriol in normal subjects, approximately 27% and 7% of the radioactivity appeared in the feces and urine, respectively, within 24 hours. When a 1-mcg oral dose of radiolabeled calcitriol was administered to normal subjects, approximately 10% of the total radioactivity appeared in urine within 24 hours. Cumulative excretion of radioactivity on the sixth day following intravenous administration of radiolabeled calcitriol averaged 16% in urine and 49% in feces. The elimination half-life of calcitriol in serum after single oral doses is about 5 to 8 hours in normal subjects.
The steady-state pharmacokinetics of oral calcitriol were determined in a small group of pediatric patients (age range: 1.8 to 16 years) undergoing peritoneal dialysis. Calcitriol was administered for 2 months at an average dose of 10.2 ng/kg (SD 5.5 ng/kg). In this pediatric population, mean Cmax was 116 pmol/L, mean serum half-life was 27.4 hours, and mean clearance was 15.3 mL/hr/kg.1
No studies have examined the pharmacokinetics of calcitriol in geriatric patients.
Controlled studies examining the influence of gender on calcitriol have not been conducted.
Controlled studies examining the influence of hepatic disease on calcitriol have not been conducted.
Lower predose and peak calcitriol levels in serum were observed in patients with nephrotic syndrome and in patients undergoing hemodialysis compared with healthy subjects. The elimination half-life of calcitriol increased by at least twofold in chronic renal failure and hemodialysis patients compared with healthy subjects. Peak serum levels in patients with nephrotic syndrome were reached in 4 hours. For patients requiring hemodialysis peak serum levels were reached in 8 to 12 hours; half-lives were estimated to be 16.2 and 21.9 hours, respectively.