Chlorpromazine Hydrochloride - Chlorpromazine Hydrochloride tablet, Coated
(Chlorpromazine Hydrochloride)Chlorpromazine Hydrochloride - Chlorpromazine Hydrochloride tablet, Coated Prescribing Information
Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Analyses of seventeen placebo-controlled trials (modal duration of 10 weeks), largely in patients taking atypical antipsychotic drugs, revealed a risk of death in drug-treated patients of between 1.6 to 1.7 times the risk of death in placebo-treated patients. Over the course of a typical 10-week controlled trial, the rate of death in drug-treated patients was about 4.5%, compared to a rate of about 2.6% in the placebo group. Although the causes of death were varied, most of the deaths appeared to be either cardiovascular (e.g., heart failure, sudden death) or infectious (e.g., pneumonia) in nature. Observational studies suggest that, similar to atypical antipsychotic drugs, treatment with conventional antipsychotic drugs may increase mortality. The extent to which the findings of increased mortality in observational studies may be attributed to the antipsychotic drug as opposed to some characteristic(s) of the patients is not clear.
Chlorpromazine hydrochloride is not approved for the treatment of patients with dementia-related psychosis (see
Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Chlorpromazine hydrochloride is not approved for the treatment of patients with dementia-related psychosis (see BOXED WARNING).
The extrapyramidal symptoms which can occur secondary to chlorpromazine may be confused with the central nervous system signs of an undiagnosed primary disease responsible for the vomiting, e.g., Reye's syndrome or other encephalopathy. The use of chlorpromazine and other potential hepatotoxins should be avoided in children and adolescents whose signs and symptoms suggest Reye's syndrome.
Both the risk of developing the syndrome and the likelihood that it will become irreversible are believed to increase as the duration of treatment and the total cumulative dose of antipsychotic drugs administered to the patient increase. However, the syndrome can develop, although much less commonly, after relatively brief treatment periods at low doses.
There is no known treatment for established cases of tardive dyskinesia, although the syndrome may remit, partially or completely, if antipsychotic treatment is withdrawn. Antipsychotic treatment itself, however, may suppress (or partially suppress) the signs and symptoms of the syndrome and therapy may possibly mask the underlying disease process. The effect that symptomatic suppression has upon the long-term course of the syndrome is unknown.
Given these considerations, antipsychotics should be prescribed in a manner that is most likely to minimize the occurrence of tardive dyskinesia. Chronic antipsychotic treatment should generally be reserved for patients who suffer from a chronic illness that, 1) is known to respond to antipsychotic drugs, and, 2) for whom alternative, equally effective, but potentially less harmful treatments are
If signs and symptoms of tardive dyskinesia appear in a patient on antipsychotics, drug discontinuation should be considered. However, some patients may require treatment despite the presence of the syndrome.
For further information about the description of tardive dyskinesia and its clinical detection, please refer to the sections on PRECAUTIONSand ADVERSE REACTIONS.
The diagnostic evaluation of patients with this syndrome is complicated. In arriving at a diagnosis, it is important to identify cases where the clinical presentation includes both serious medical illness (e.g., pneumonia, systemic infection, etc.) and untreated or inadequately treated extrapyramidal signs and symptoms (EPS). Other important considerations in the differential diagnosis include central anticholinergic toxicity, heat stroke, drug fever and primary central nervous system (CNS) pathology.
The management of NMS should include 1) immediate discontinuation of antipsychotic drugs and other drugs not essential to concurrent therapy, 2) intensive symptomatic treatment and medical monitoring, and 3) treatment of any concomitant serious medical problems for which specific treatments are available. There is no general agreement about specific pharmacological treatment regimens for uncomplicated NMS.
If a patient requires antipsychotic drug treatment after recovery from NMS, the potential reintroduction of drug therapy should be carefully considered. The patient should be carefully monitored, since recurrences of NMS have been reported.
An encephalopathic syndrome (characterized by weakness, lethargy, fever, tremulousness and confusion, extrapyramidal symptoms, leukocytosis, elevated serum enzymes, BUN and FBS) has occurred in a few patients treated with lithium plus an antipsychotic. In some instances, the syndrome was followed by irreversible brain damage. Because of a possible causal relationship between these events and the concomitant administration of lithium and antipsychotics, patients receiving such combined therapy should be monitored closely for early evidence of neurologic toxicity and treatment discontinued promptly if such signs appear. This encephalopathic syndrome may be similar to or the same as neuroleptic malignant syndrome (NMS).
Patients with bone marrow depression or who have previously demonstrated a hypersensitivity reaction (e.g., blood dyscrasias, jaundice) with a phenothiazine, should not receive any phenothiazine, including chlorpromazine, unless in the judgment of the physician the potential benefits of treatment outweigh the possible hazard.
Chlorpromazine may impair mental and/or physical abilities, especially during the first few days of therapy. Therefore, caution patients about activities requiring alertness (e.g., operating vehicles or machinery).
The use of alcohol with this drug should be avoided due to possible additive effects and hypotension.
Chlorpromazine may counteract the antihypertensive effect of guanethidine and related compounds.
Chlorpromazine may cause somnolence, postural hypotension, motor and sensory instability, which may lead to falls and, consequently, fractures or other injuries. For patients with diseases, conditions, or medications that could exacerbate these effects, complete fall risk assessments when initiating antipsychotic treatment and recurrently for patients on long-term antipsychotic therapy.
Reproductive studies in rodents have demonstrated potential for embryotoxicity, increased neonatal mortality and nursing transfer of the drug. Tests in the offspring of the drug–treated rodents demonstrate decreased performance. The possibility of permanent neurological damage cannot be excluded.
Chlorpromazine Hydrochloride should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
For the management of manifestations of psychotic disorders.
For the treatment of schizophrenia.
To control nausea and vomiting.
For relief of restlessness and apprehension before surgery.
For acute intermittent porphyria.
As an adjunct in the treatment of tetanus.
To control the manifestations of the manic type of manic-depressive illness.
For relief of intractable hiccups.
For the treatment of severe behavioral problems in children (1 to 12 years of age) marked by combativeness and/or explosive hyperexcitable behavior (out of proportion to immediate provocations), and in the short-term treatment of hyperactive children who show excessive motor activity with accompanying conduct disorders consisting of some or all of the following symptoms: impulsivity, difficulty sustaining attention, aggressivity, mood lability and poor frustration tolerance.
Adjust dosage to individual and the severity of his condition, recognizing that the milligram for milligram potency relationship among all dosage forms has not been precisely established clinically. It is important to increase dosage until symptoms are controlled. Dosage should be increased more gradually in debilitated or emaciated patients. In continued therapy, gradually reduce dosage to the lowest effective maintenance level, after symptoms have been controlled for a reasonable period.
The 100 mg and 200 mg tablets are for use in severe neuropsychiatric conditions.
Hospitalized Patients:
Do not use in patients with known hypersensitivity to phenothiazines.
Do not use in comatose states or in the presence of large amounts of central nervous system depressants (alcohol, barbiturates, narcotics, etc.).
There is no conclusive evidence that preexisting liver disease makes patients more susceptible to jaundice. Alcoholics with cirrhosis have been successfully treated with chlorpromazine without complications. Nevertheless, the medication should be used cautiously in patients with liver disease. Patients who have experienced jaundice with a phenothiazine should not, if possible, be reexposed to chlorpromazine or other phenothiazines.
If fever with grippe-like symptoms occurs, appropriate liver studies should be conducted. If tests indicate an abnormality, stop treatment.
Liver function tests in jaundice induced by the drug may mimic extrahepatic obstruction; withhold exploratory laparotomy until extrahepatic obstruction is confirmed.
Most cases have occurred between the fourth and tenth weeks of therapy; patients should be watched closely during that period.
Moderate suppression of white blood cells is not an indication for stopping treatment unless accompanied by the symptoms described above.
Hypotensive Effects
To control hypotension, place patient in head–low position with legs raised. If a vasoconstrictor is required, norepinephrine and phenylephrine are the most suitable. Other pressor agents, including epinephrine, should not be used as they may cause a paradoxical further lowering of blood pressure.
Extrapyramidal Symptoms
Class effect:
If these symptoms become too troublesome, they can usually be controlled by a reduction of dosage or change of drug. Treatment with anti–parkinsonian agents, benzodiazepines or propranolol may be helpful.
There is no known effective treatment for tardive dyskinesia; anti-parkinsonism agents do not alleviate the symptoms of this syndrome. If clinically feasible, it is suggested that all antipsychotic agents be discontinued if these symptoms appear. Should it be necessary to reinstitute treatment, or increase the dosage of the agent, or switch to a different antipsychotic agent, the syndrome may be masked.
It has been reported that fine vermicular movements of the tongue may be an early sign of the syndrome and, if the medication is stopped at that time, the syndrome may not develop.
Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Chlorpromazine hydrochloride is not approved for the treatment of patients with dementia-related psychosis (see BOXED WARNING).
The extrapyramidal symptoms which can occur secondary to chlorpromazine may be confused with the central nervous system signs of an undiagnosed primary disease responsible for the vomiting, e.g., Reye's syndrome or other encephalopathy. The use of chlorpromazine and other potential hepatotoxins should be avoided in children and adolescents whose signs and symptoms suggest Reye's syndrome.
Both the risk of developing the syndrome and the likelihood that it will become irreversible are believed to increase as the duration of treatment and the total cumulative dose of antipsychotic drugs administered to the patient increase. However, the syndrome can develop, although much less commonly, after relatively brief treatment periods at low doses.
There is no known treatment for established cases of tardive dyskinesia, although the syndrome may remit, partially or completely, if antipsychotic treatment is withdrawn. Antipsychotic treatment itself, however, may suppress (or partially suppress) the signs and symptoms of the syndrome and therapy may possibly mask the underlying disease process. The effect that symptomatic suppression has upon the long-term course of the syndrome is unknown.
Given these considerations, antipsychotics should be prescribed in a manner that is most likely to minimize the occurrence of tardive dyskinesia. Chronic antipsychotic treatment should generally be reserved for patients who suffer from a chronic illness that, 1) is known to respond to antipsychotic drugs, and, 2) for whom alternative, equally effective, but potentially less harmful treatments are
If signs and symptoms of tardive dyskinesia appear in a patient on antipsychotics, drug discontinuation should be considered. However, some patients may require treatment despite the presence of the syndrome.
For further information about the description of tardive dyskinesia and its clinical detection, please refer to the sections on PRECAUTIONSand ADVERSE REACTIONS.
The diagnostic evaluation of patients with this syndrome is complicated. In arriving at a diagnosis, it is important to identify cases where the clinical presentation includes both serious medical illness (e.g., pneumonia, systemic infection, etc.) and untreated or inadequately treated extrapyramidal signs and symptoms (EPS). Other important considerations in the differential diagnosis include central anticholinergic toxicity, heat stroke, drug fever and primary central nervous system (CNS) pathology.
The management of NMS should include 1) immediate discontinuation of antipsychotic drugs and other drugs not essential to concurrent therapy, 2) intensive symptomatic treatment and medical monitoring, and 3) treatment of any concomitant serious medical problems for which specific treatments are available. There is no general agreement about specific pharmacological treatment regimens for uncomplicated NMS.
If a patient requires antipsychotic drug treatment after recovery from NMS, the potential reintroduction of drug therapy should be carefully considered. The patient should be carefully monitored, since recurrences of NMS have been reported.
An encephalopathic syndrome (characterized by weakness, lethargy, fever, tremulousness and confusion, extrapyramidal symptoms, leukocytosis, elevated serum enzymes, BUN and FBS) has occurred in a few patients treated with lithium plus an antipsychotic. In some instances, the syndrome was followed by irreversible brain damage. Because of a possible causal relationship between these events and the concomitant administration of lithium and antipsychotics, patients receiving such combined therapy should be monitored closely for early evidence of neurologic toxicity and treatment discontinued promptly if such signs appear. This encephalopathic syndrome may be similar to or the same as neuroleptic malignant syndrome (NMS).
Patients with bone marrow depression or who have previously demonstrated a hypersensitivity reaction (e.g., blood dyscrasias, jaundice) with a phenothiazine, should not receive any phenothiazine, including chlorpromazine, unless in the judgment of the physician the potential benefits of treatment outweigh the possible hazard.
Chlorpromazine may impair mental and/or physical abilities, especially during the first few days of therapy. Therefore, caution patients about activities requiring alertness (e.g., operating vehicles or machinery).
The use of alcohol with this drug should be avoided due to possible additive effects and hypotension.
Chlorpromazine may counteract the antihypertensive effect of guanethidine and related compounds.
Chlorpromazine may cause somnolence, postural hypotension, motor and sensory instability, which may lead to falls and, consequently, fractures or other injuries. For patients with diseases, conditions, or medications that could exacerbate these effects, complete fall risk assessments when initiating antipsychotic treatment and recurrently for patients on long-term antipsychotic therapy.
Reproductive studies in rodents have demonstrated potential for embryotoxicity, increased neonatal mortality and nursing transfer of the drug. Tests in the offspring of the drug–treated rodents demonstrate decreased performance. The possibility of permanent neurological damage cannot be excluded.
Chlorpromazine Hydrochloride should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Cerebral edema has been reported.
Convulsive seizures (petit mal and grand mal) have been reported, particularly in patients with EEG abnormalities or history of such disorders.
Abnormality of the cerebrospinal fluid proteins has also been reported.
Contact dermatitis has been reported in nursing personnel; accordingly, the use of rubber gloves when administering chlorpromazine liquid or injectable is recommended.
In addition, asthma, laryngeal edema, angioneurotic edema and anaphylactoid reactions have been reported.
The pigmentary changes, restricted to exposed areas of the body, range from an almost imperceptible darkening of the skin to a slate gray color, sometimes with a violet hue. Histological examination reveals a pigment, chiefly in the dermis, which is probably a melanin-like complex. This pigmentation may fade following discontinuance of the drug.
Since the occurrence of eye changes seems to be related to dosage levels and/or duration of therapy, it is suggested that long-term patients on moderate to high dosage levels have periodic ocular examinations.
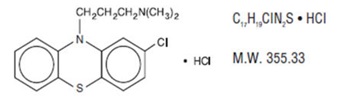
Chlorpromazine hydrochloride, a dimethylamine derivative of phenothiazine, has a chemical formula of 2-chloro-10-[3-(dimethylamino) propyl] phenothiazine monohydrochloride. It is available in tablets for oral administration. It has the following structural formula:
Chlorpromazine hydrochloride occurs as white or slightly creamy white, odorless, crystalline powder which darkens on prolonged exposure to light.
Each tablet for oral administration contains 10 mg, 25 mg, 50 mg, 100 mg, or 200 mg of chlorpromazine HCl, USP.
Inactive ingredients: lactose monohydrate, microcrystalline cellulose, croscarmellose sodium, povidone, colloidal silicon dioxide, and magnesium stearate, hypromellose, hydroxypropyl cellulose, titanium dioxide. For 10 mg and 25 mg tablets, FD&C Blue #2 aluminum lake. For 50 mg tablets, FD&C Yellow #6 aluminum lake, and ferric oxide red. For 100 mg and 200 mg tablets, D&C Red #7 lake and FD&C Blue #2 aluminum lake.