Cimetidine
Cimetidine Prescribing Information
Cimetidine tablets are indicated in:
Clinical studies have indicated that suppression of nocturnal acid is the most important factor in duodenal ulcer healing (see
In a U.S. dose-ranging study of 400 mg at bedtime, 800 mg at bedtime and 1,600 mg at bedtime, a continuous dose-response relationship for ulcer healing was demonstrated.
However, 800 mg at bedtime is the dose of choice for most patients, as it provides a high healing rate (the difference between 800 mg at bedtime and 1,600 mg at bedtime being small), maximal pain relief, a decreased potential for drug interactions (see
It has been shown that patients who both have an endoscopically demonstrated ulcer larger than 1 cm and are also heavy smokers (i.e., smoke 1 pack of cigarettes or more per day) are more difficult to heal. There is some evidence which suggests that more rapid healing can be achieved in this subpopulation with 1,600 mg of cimetidine tablets at bedtime. While early pain relief with either 800 mg at bedtime or 1,600 mg at bedtime is equivalent in all patients, 1,600 mg at bedtime provides an appropriate alternative when it is important to ensure healing within 4 weeks for this subpopulation. Alternatively, approximately 94% of all patients will also heal in 8 weeks with 800 mg of cimetidine tablets at bedtime.
Other regimens of cimetidine tablets in the United States which have been shown to be effective are: 300 mg 4 times daily, with meals and at bedtime, the original regimen with which U.S. physicians have the most experience, and 400 mg twice daily, in the morning and at bedtime (see
Concomitant antacids should be given as needed for relief of pain. However, simultaneous administration of cimetidine tablets and antacids is not recommended, since antacids have been reported to interfere with the absorption of cimetidine.
While healing with cimetidine tablets often occurs during the first week or two, treatment should be continued for 4 weeks to 6 weeks unless healing has been demonstrated by endoscopic examination.
In those patients requiring maintenance therapy, the recommended adult oral dose is 400 mg at bedtime.
The recommended adult oral dosage for short-term treatment of active benign gastric ulcer is 800 mg at bedtime, or 300 mg 4 times a day with meals and at bedtime. Controlled clinical studies were limited to 6 weeks of treatment (see
The recommended adult oral dosage for the treatment of erosive esophagitis that has been diagnosed by endoscopy is 1,600 mg daily in divided doses (800 mg twice daily or 400 mg 4 times daily) for 12 weeks. The use of cimetidine tablets beyond 12 weeks has not been established.
Recommended adult oral dosage: 300 mg 4 times a day with meals and at bedtime. In some patients it may be necessary to administer higher doses more frequently. Doses should be adjusted to individual patient needs, but should not usually exceed 2,400 mg per day and should continue as long as clinically indicated.
Patients with severely impaired renal function have been treated with cimetidine tablets. However, such usage has been very limited. On the basis of this experience the recommended dosage is 300 mg every 12 hours orally. Should the patient’s condition require, the frequency of dosing may be increased to every 8 hours or even further with caution. In severe renal failure, accumulation may occur and the lowest frequency of dosing compatible with an adequate patient response should be used. When liver impairment is also present, further reductions in dosage may be necessary. Hemodialysis reduces the level of circulating cimetidine tablets. Ideally, the dosage schedule should be adjusted so that the timing of a scheduled dose coincides with the end of hemodialysis.
The recommended adult oral dosage for the treatment of erosive esophagitis that has been diagnosed by endoscopy is 1,600 mg daily in divided doses (800 mg twice daily or 400 mg 4 times daily) for 12 weeks. The use of cimetidine tablets beyond 12 weeks has not been established.
Clinical studies have indicated that suppression of nocturnal acid is the most important factor in duodenal ulcer healing (see
An 800 mg oral dose of cimetidine at bedtime reduces mean hourly H+activity by greater than 85% over an 8-hour period in duodenal ulcer patients, with no effect on daytime acid secretion. A 1,600 mg oral dose of cimetidine at bedtime produces 100% inhibition of mean hourly H+activity over an 8-hour period in duodenal ulcer patients, but also reduces H+activity by 35% for an additional 5 hours into the following morning. Cimetidine given as 400 mg twice daily and 300 mg 4 times daily decreases nocturnal acid secretion in a dose-related manner, i.e., 47% to 83% over a 6-hour to 8-hour period and 54% over a 9-hour period, respectively.
During the first hour after a standard experimental meal, a 300 mg oral dose of cimetidine inhibited gastric acid secretion in duodenal ulcer patients by at least 50%. During the subsequent 2 hours cimetidine inhibited gastric acid secretion by at least 75%.
The effect of a 300 mg breakfast dose of cimetidine continued for at least 4 hours and there was partial suppression of the rise in gastric acid secretion following the luncheon meal in duodenal ulcer patients. This suppression of gastric acid output was enhanced and could be maintained by another 300 mg dose of cimetidine given with lunch.
In another study, a 300 mg dose of cimetidine given with the meal increased gastric pH as compared with placebo.
Cimetidine | Placebo | |
1 hour | 3.5 | 2.6 |
2 hours | 3.1 | 1.6 |
3 hours | 3.8 | 1.9 |
4 hours | 6.1 | 2.2 |
Cimetidine dosed at 800 mg at bedtime, 400 mg twice daily, and 300 mg 4 times daily, all provide a similar, moderate (less than 60%) level of 24-hour acid suppression. However, the 800 mg bedtime dose regimen exerts its entire effect on nocturnal acid, and does not affect daytime gastric physiology.
Cimetidine administered orally significantly inhibited gastric acid secretion stimulated by betazole (an isomer of histamine), pentagastrin, caffeine and insulin as follows:
Stimulant | Stimulant Dose | Cimetidine | % Inhibition |
Betazole | 1.5 mg/kg (sc) | 300 mg (po) | 85% at 2 1/2 hours |
Pentagastrin | 6 mcg/kg/hr (iv) | 100 mg/hr (iv) | 60% at 1 hour |
Caffeine | 5 mg/kg/hr (iv) | 300 mg (po) | 100% at 1 hour |
Insulin | 0.03 units/kg/hr (iv) | 100 mg/hr (iv) | 82% at 1 hour |
When food and betazole were used to stimulate secretion, inhibition of hydrogen ion concentration usually ranged from 45% to 75% and the inhibition of volume ranged from 30% to 65%.
300 mg of cimetidine taken orally reduced total pepsin output as a result of the decrease in volume of gastric juice.
Intrinsic factor secretion was studied with betazole as a stimulant. Cimetidine dosed at 300 mg orally inhibited the rise in intrinsic factor concentration produced by betazole, but some intrinsic factor was secreted at all times.
Cimetidine has been shown to be effective in the treatment of active duodenal ulcer and, at reduced dosage, in maintenance therapy following healing of active ulcers.
Cimetidine accelerates the rate of duodenal ulcer healing. Healing rates reported in U.S. and foreign controlled trials with cimetidine are summarized below, beginning with the regimen providing the lowest nocturnal dose.
Regimen | 300 mg 4 times daily | 400 mg twice daily | 800 mg at bedtime | 1,600 mg at bedtime |
Week 4 | 68% | 73% | 80% | 86% |
Week 6 | 80% | 80% | 89% | - |
Week 8 | - | 92% | 94% | - |
A U.S., double-blind, placebo-controlled, dose-ranging study demonstrated that all once-daily at bedtime regimens of cimetidine was superior to placebo in ulcer healing and that 800 mg of cimetidine at bedtime healed 75% of patients at 4 weeks. The healing rate with 800 mg at bedtime was significantly superior to 400 mg at bedtime (66%) and not significantly different from 1,600 mg at bedtime (81%).
In the U.S. dose-ranging trial, over 80% of patients receiving 800 mg of cimetidine at bedtime experienced nocturnal pain relief after one day. Relief from daytime pain was reported in approximately 70% of patients after 2 days. As with ulcer healing, the 800 mg dose at bedtime was superior to 400 mg at bedtime and not different from 1,600 mg at bedtime.
In foreign, double-blind studies with 800 mg of cimetidine at bedtime, 79% to 85% of patients were healed at 4 weeks.
While short-term treatment with cimetidine can result in complete healing of the duodenal ulcer, acute therapy will not prevent ulcer recurrence after cimetidine has been discontinued. Some follow-up studies have reported that the rate of recurrence once therapy was discontinued was slightly higher for patients healed on cimetidine than for patients healed on other forms of therapy; however, the patients treated with cimetidine generally had more severe disease.
Treatment with a reduced dose of cimetidine has been proven effective as maintenance therapy following healing of active duodenal ulcers.
In numerous placebo-controlled studies conducted worldwide, the percent of patients with observed ulcers at the end of 1 year’s therapy with 400 mg of cimetidine at bedtime was significantly lower (10% to 45%) than in patients receiving placebo (44% to 70%). Thus, from 55% to 90% of patients were maintained free of observed ulcers at the end of 1 year with 400 mg of cimetidine at bedtime.
Factors such as smoking, duration and severity of disease, gender, and genetic traits may contribute to variations in actual percentages.
Trials of other anti-ulcer therapy, whether placebo-controlled, positive-controlled or open, have demonstrated a range of results similar to that seen with cimetidine.
In a U.S. dose-ranging study of 400 mg at bedtime, 800 mg at bedtime and 1,600 mg at bedtime, a continuous dose-response relationship for ulcer healing was demonstrated.
However, 800 mg at bedtime is the dose of choice for most patients, as it provides a high healing rate (the difference between 800 mg at bedtime and 1,600 mg at bedtime being small), maximal pain relief, a decreased potential for drug interactions (see
Cimetidine, apparently through an effect on certain microsomal enzyme systems, has been reported to reduce the hepatic metabolism of warfarin-type anticoagulants, phenytoin, propranolol, nifedipine, chlordiazepoxide, diazepam, certain tricyclic antidepressants, lidocaine, theophylline, and metronidazole, thereby delaying elimination and increasing blood levels of these drugs.
Clinically significant effects have been reported with the warfarin anticoagulants; therefore, close monitoring of prothrombin time is recommended, and adjustment of the anticoagulant dose may be necessary when cimetidine is administered concomitantly. Interaction with phenytoin, lidocaine, and theophylline has also been reported to produce adverse clinical effects.
However, a crossover study in healthy subjects receiving either 300 mg 4 times daily or 800 mg at bedtime of cimetidine concomitantly with a 300 mg twice-daily dose of theophylline extended-release tablets demonstrated less alteration in steady-state theophylline peak serum levels with the 800 mg at bedtime regimen, particularly in subjects aged 54 years and older. Data beyond 10 days are not available. (Note: All patients receiving theophylline should be monitored appropriately, regardless of concomitant drug therapy.)
Dosage of the drugs mentioned above and other similarly metabolized drugs, particularly those of low therapeutic ratio or in patients with renal and/or hepatic impairment, may require adjustment when starting or stopping the concomitant administration of cimetidine to maintain optimum therapeutic blood levels.
Alteration of pH may affect absorption of certain drugs (e.g., ketoconazole). If these products are needed, they should be given at least 2 hours before cimetidine administration.
Additional clinical experience may reveal other drugs affected by the concomitant administration of cimetidine.
It has been shown that patients who both have an endoscopically demonstrated ulcer larger than 1 cm and are also heavy smokers (i.e., smoke 1 pack of cigarettes or more per day) are more difficult to heal. There is some evidence which suggests that more rapid healing can be achieved in this subpopulation with 1,600 mg of cimetidine tablets at bedtime. While early pain relief with either 800 mg at bedtime or 1,600 mg at bedtime is equivalent in all patients, 1,600 mg at bedtime provides an appropriate alternative when it is important to ensure healing within 4 weeks for this subpopulation. Alternatively, approximately 94% of all patients will also heal in 8 weeks with 800 mg of cimetidine tablets at bedtime.
Other regimens of cimetidine tablets in the United States which have been shown to be effective are: 300 mg 4 times daily, with meals and at bedtime, the original regimen with which U.S. physicians have the most experience, and 400 mg twice daily, in the morning and at bedtime (see
Cimetidine has been shown to be effective in the treatment of active duodenal ulcer and, at reduced dosage, in maintenance therapy following healing of active ulcers.
Cimetidine accelerates the rate of duodenal ulcer healing. Healing rates reported in U.S. and foreign controlled trials with cimetidine are summarized below, beginning with the regimen providing the lowest nocturnal dose.
Regimen | 300 mg 4 times daily | 400 mg twice daily | 800 mg at bedtime | 1,600 mg at bedtime |
Week 4 | 68% | 73% | 80% | 86% |
Week 6 | 80% | 80% | 89% | - |
Week 8 | - | 92% | 94% | - |
A U.S., double-blind, placebo-controlled, dose-ranging study demonstrated that all once-daily at bedtime regimens of cimetidine was superior to placebo in ulcer healing and that 800 mg of cimetidine at bedtime healed 75% of patients at 4 weeks. The healing rate with 800 mg at bedtime was significantly superior to 400 mg at bedtime (66%) and not significantly different from 1,600 mg at bedtime (81%).
In the U.S. dose-ranging trial, over 80% of patients receiving 800 mg of cimetidine at bedtime experienced nocturnal pain relief after one day. Relief from daytime pain was reported in approximately 70% of patients after 2 days. As with ulcer healing, the 800 mg dose at bedtime was superior to 400 mg at bedtime and not different from 1,600 mg at bedtime.
In foreign, double-blind studies with 800 mg of cimetidine at bedtime, 79% to 85% of patients were healed at 4 weeks.
While short-term treatment with cimetidine can result in complete healing of the duodenal ulcer, acute therapy will not prevent ulcer recurrence after cimetidine has been discontinued. Some follow-up studies have reported that the rate of recurrence once therapy was discontinued was slightly higher for patients healed on cimetidine than for patients healed on other forms of therapy; however, the patients treated with cimetidine generally had more severe disease.
Treatment with a reduced dose of cimetidine has been proven effective as maintenance therapy following healing of active duodenal ulcers.
In numerous placebo-controlled studies conducted worldwide, the percent of patients with observed ulcers at the end of 1 year’s therapy with 400 mg of cimetidine at bedtime was significantly lower (10% to 45%) than in patients receiving placebo (44% to 70%). Thus, from 55% to 90% of patients were maintained free of observed ulcers at the end of 1 year with 400 mg of cimetidine at bedtime.
Factors such as smoking, duration and severity of disease, gender, and genetic traits may contribute to variations in actual percentages.
Trials of other anti-ulcer therapy, whether placebo-controlled, positive-controlled or open, have demonstrated a range of results similar to that seen with cimetidine.
Concomitant antacids should be given as needed for relief of pain. However, simultaneous administration of cimetidine tablets and antacids is not recommended, since antacids have been reported to interfere with the absorption of cimetidine.
While healing with cimetidine tablets often occurs during the first week or two, treatment should be continued for 4 weeks to 6 weeks unless healing has been demonstrated by endoscopic examination.
Cimetidine tablets are contraindicated for patients known to have hypersensitivity to the product.
Adverse effects reported in patients taking cimetidine is described as follows by body system. Incidence figures of 1 in 100 and greater are generally derived from controlled clinical studies.
Cimetidine, apparently through an effect on certain microsomal enzyme systems, has been reported to reduce the hepatic metabolism of warfarin-type anticoagulants, phenytoin, propranolol, nifedipine, chlordiazepoxide, diazepam, certain tricyclic antidepressants, lidocaine, theophylline, and metronidazole, thereby delaying elimination and increasing blood levels of these drugs.
Clinically significant effects have been reported with the warfarin anticoagulants; therefore, close monitoring of prothrombin time is recommended, and adjustment of the anticoagulant dose may be necessary when cimetidine is administered concomitantly. Interaction with phenytoin, lidocaine, and theophylline has also been reported to produce adverse clinical effects.
However, a crossover study in healthy subjects receiving either 300 mg 4 times daily or 800 mg at bedtime of cimetidine concomitantly with a 300 mg twice-daily dose of theophylline extended-release tablets demonstrated less alteration in steady-state theophylline peak serum levels with the 800 mg at bedtime regimen, particularly in subjects aged 54 years and older. Data beyond 10 days are not available. (Note: All patients receiving theophylline should be monitored appropriately, regardless of concomitant drug therapy.)
Dosage of the drugs mentioned above and other similarly metabolized drugs, particularly those of low therapeutic ratio or in patients with renal and/or hepatic impairment, may require adjustment when starting or stopping the concomitant administration of cimetidine to maintain optimum therapeutic blood levels.
Alteration of pH may affect absorption of certain drugs (e.g., ketoconazole). If these products are needed, they should be given at least 2 hours before cimetidine administration.
Additional clinical experience may reveal other drugs affected by the concomitant administration of cimetidine.
Cimetidine is a histamine H
2-receptor antagonist. Chemically it is
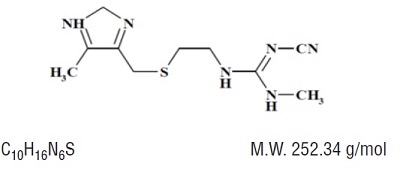
Cimetidine contains an imidazole ring, and is chemically related to histamine.
Cimetidine, USP is a white to off-white, crystalline powder.