Clonazepam Prescribing Information
- Concomitant use of benzodiazepines and opioids may result in profound sedation, respiratory depression, coma, and death. Reserve concomitant prescribing of these drugs for patients for whom alternative treatment options are inadequate. Limit dosages and durations to the minimum required. Follow patients for signs and symptoms of respiratory depression and sedation (seeand
WARNINGSRisks from Concomitant Use with OpioidsConcomitant use of benzodiazepines, including clonazepam, and opioids may result in profound sedation, respiratory depression, coma, and death. Because of these risks, reserve concomitant prescribing of benzodiazepines and opioids for patients for whom alternative treatment options are inadequate.
Observational studies have demonstrated that concomitant use of opioid analgesics and benzodiazepines increases the risk of drug-related mortality compared to use of opioids alone. If a decision is made to prescribe clonazepam concomitantly with opioids, prescribe the lowest effective dosages and minimum durations of concomitant use, and follow patients closely for signs and symptoms of respiratory depression and sedation. Advise both patients and caregivers about the risks of respiratory depression and sedation when clonazepam is used with opioids (see
PRECAUTIONS: Information for PatientsandPRECAUTIONS: Drug Interactions)Abuse, Misuse, and AddictionThe use of benzodiazepines, including clonazepam, exposes users to the risks of abuse, misuse, and addiction, which can lead to overdose or death. Abuse and misuse of benzodiazepines often (but not always) involve the use of doses greater than the maximum recommended dosage and commonly involve concomitant use of other medications, alcohol, and/or illicit substances, which is associated with an increased frequency of serious adverse outcomes, including respiratory depression, overdose, or death (see
DRUG ABUSE AND DEPENDENCE: Abuse).Before prescribing clonazepam and throughout treatment, assess each patient’s risk for abuse, misuse, and addiction (e.g., using a standardized screening tool). Use of clonazepam, particularly in patients at elevated risk, necessitates counseling about the risks and proper use of clonazepam along with monitoring for signs and symptoms of abuse, misuse, and addiction. Prescribe the lowest effective dosage; avoid or minimize concomitant use of CNS depressants and other substances associated with abuse, misuse, and addiction (e.g., opioid analgesics, stimulants); and advise patients on the proper disposal of unused drug. If a substance use disorder is suspected, evaluate the patient and institute (or refer them for) early treatment, as appropriate.
Dependence and Withdrawal ReactionsTo reduce the risk of withdrawal reactions, use a gradual taper to discontinue clonazepam or reduce the dosage (a patient-specific plan should be used to taper the dose) (see
DOSAGE AND ADMINISTRATION: Discontinuation or Dosage Reduction of Clonazepam).Patients at an increased risk of withdrawal adverse reactions after benzodiazepine discontinuation or rapid dosage reduction include those who take higher dosages, and those who have had longer durations of use.
Acute Withdrawal ReactionsThe continued use of benzodiazepines, including clonazepam, may lead to clinically significant physical dependence. Abrupt discontinuation or rapid dosage reduction of clonazepam after continued use, or administration of flumazenil (a benzodiazepine antagonist) may precipitate acute withdrawal reactions, which can be life-threatening (e.g., seizures) (see
DRUG ABUSE AND DEPENDENCE: Dependence).Protracted Withdrawal SyndromeIn some cases, benzodiazepine users have developed a protracted withdrawal syndrome with withdrawal symptoms lasting weeks to more than 12 months (see
DRUG ABUSE AND DEPENDENCE: Dependence).Interference with Cognitive and Motor PerformanceSince clonazepam produces CNS depression, patients receiving this drug should be cautioned against engaging in hazardous occupations requiring mental alertness, such as operating machinery or driving a motor vehicle. They should also be warned about the concomitant use of alcohol or other CNS-depressant drugs during clonazepam therapy (see
PRECAUTIONS: Drug InteractionsandPRECAUTIONS: Information for Patients).Suicidal Behavior and IdeationAntiepileptic drugs (AEDs), including clonazepam, increase the risk of suicidal thoughts or behavior in patients taking these drugs for any indication. Patients treated with any AED for any indication should be monitored for the emergence or worsening of depression, suicidal thoughts or behavior, and/or any unusual changes in mood or behavior.
Pooled analyses of 199 placebo-controlled clinical trials (mono- and adjunctive therapy) of 11 different AEDs showed that patients randomized to one of the AEDs had approximately twice the risk (adjusted Relative Risk 1.8, 95% CI:1.2, 2.7) of suicidal thinking or behavior compared to patients randomized to placebo. In these trials, which had a median treatment duration of 12 weeks, the estimated incidence rate of suicidal behavior or ideation among 27,863 AED-treated patients was 0.43% compared to 0.24% among 16,029 placebo-treated patients, representing an increase of approximately one case of suicidal thinking or behavior for every 530 patients treated. There were four suicides in drug-treated patients in the trials and none in placebo-treated patients, but the number is too small to allow any conclusion about drug effect on suicide.
The increased risk of suicidal thoughts or behavior with AEDs was observed as early as one week after starting drug treatment with AEDs and persisted for the duration of treatment assessed. Because most trials included in the analysis did not extend beyond 24 weeks, the risk of suicidal thoughts or behavior beyond 24 weeks could not be assessed.
The risk of suicidal thoughts or behavior was generally consistent among drugs in the data analyzed. The finding of increased risk with AEDs of varying mechanisms of action and across a range of indications suggests that the risk applies to all AEDs used for any indication. The risk did not vary substantially by age (5 to 100 years) in the clinical trials analyzed.
Table 1shows absolute and relative risk by indication for all evaluated AEDs.Table 1 Risk by Indication for Antiepileptic Drugs in the Pooled AnalysisIndicationPlacebo Patients with Events Per 1000 PatientsDrug Patients with Events Per 1000 PatientsRelative Risk: Incidence of Events in Drug Patients/Incidence in Placebo PatientsRisk Difference: Additional Drug Patients with Events per 1000 PatientsEpilepsy
Psychiatric
Other
Total
1.0
5.7
1.0
2.4
3.4
8.5
1.8
4.3
3.5
1.5
1.9
1.8
2.4
2.9
0.9
1.9
The relative risk for suicidal thoughts or behavior was higher in clinical trials for epilepsy than in clinical trials for psychiatric or other conditions, but the absolute risk differences were similar for the epilepsy and psychiatric indications.
Anyone considering prescribing clonazepam or any other AED must balance the risk of suicidal thoughts or behavior with the risk of untreated illness. Epilepsy and many other illnesses for which AEDs are prescribed are themselves associated with morbidity and mortality and with an increased risk of suicidal thoughts and behavior. Should suicidal thoughts and behavior emerge during treatment, the prescriber needs to consider whether the emergence of these symptoms in any given patient may be related to the illness being treated.
Patients, their caregivers, and families should be informed that AEDs increase the risk of suicidal thoughts and behavior and should be advised of the need to be alert for the emergence or worsening of the signs and symptoms of depression, any unusual changes in mood or behavior, or the emergence of suicidal thoughts, behavior, or thoughts about self-harm. Behaviors of concern should be reported immediately to healthcare providers.
Neonatal Sedation and Withdrawal SyndromeUse of clonazepam late in pregnancy can result in sedation (respiratory depression, lethargy, hypotonia) and/or withdrawal symptoms (hyperreflexia, irritability, restlessness, tremors, inconsolable crying, and feeding difficulties) in the neonate (see
PRECAUTIONS: Pregnancy). Monitor neonates exposed to clonazepam during pregnancy or labor for signs of sedation and monitor neonates exposed to clonazepam during pregnancy for signs of withdrawal; manage these neonates accordingly.).PRECAUTIONSGeneralWorsening of SeizuresWhen used in patients in whom several different types of seizure disorders coexist, clonazepam may increase the incidence or precipitate the onset of generalized tonic-clonic seizures (grand mal). This may require the addition of appropriate anticonvulsants or an increase in their dosages. The concomitant use of valproic acid and clonazepam may produce absence status.
Loss of EffectIn some studies, up to 30% of patients who initially responded have shown a loss of anticonvulsant activity, often within 3 months of administration. In some cases, dosage adjustment may reestablish efficacy.
Laboratory Testing During Long-Term TherapyPeriodic blood counts and liver function tests are advisable during long-term therapy with clonazepam.
Psychiatric and Paradoxical ReactionsParadoxical reactions, such as agitation, irritability, aggression, anxiety, anger, nightmares, hallucinations, and psychoses are known to occur when using benzodiazepines (see
ADVERSE REACTIONS: Psychiatric). Should this occur, the use of the drug should be discontinued gradually (seeWARNINGS: Dependence and Withdrawal ReactionsandDRUG ABUSE AND DEPENDENCE: Dependence). Paradoxical reactions are more likely to occur in children and in the elderly.Caution in Renally Impaired PatientsMetabolites of clonazepam are excreted by the kidneys; to avoid their excess accumulation, caution should be exercised in the administration of the drug to patients with impaired renal function.
HypersalivationClonazepam may produce an increase in salivation. This should be considered before giving the drug to patients who have difficulty handling secretions.
Respiratory DepressionClonazepam may cause respiratory depression and should be used with caution in patients with compromised respiratory function (e.g., chronic obstructive pulmonary disease, sleep apnea).
PorphyriaClonazepam may have a porphyrogenic effect and should be used with care in patients with porphyria.
Information for PatientsA clonazepam Medication Guide must be given to the patient each time clonazepam is dispensed, as required by law. Patients should be instructed to take clonazepam only as prescribed. Physicians are advised to discuss the following issues with patients for whom they prescribe clonazepam:
Risks from Concomitant Use with OpioidsInform patients and caregivers that potentially fatal additive effects may occur if clonazepam is used with opioids and not to use such drugs concomitantly unless supervised by a health care provider (see
WARNINGS: Risks from Concomitant Use with OpioidsandPRECAUTIONS: Drug Interactions).Abuse, Misuse, and AddictionInform patients that the use of clonazepam, even at recommended dosages, exposes users to risks of abuse, misuse, and addiction, which can lead to overdose and death, especially when used in combination with other medications (e.g., opioid analgesics), alcohol, and/or illicit substances. Inform patients about the signs and symptoms of benzodiazepine abuse, misuse, and addiction; to seek medical help if they develop these signs and/or symptoms; and on the proper disposal of unused drug (see
WARNINGS: Abuse, Misuse, and AddictionandDRUG ABUSE AND DEPENDENCE).Withdrawal ReactionsInform patients that the continued use of clonazepam may lead to clinically significant physical dependence and that abrupt discontinuation or rapid dosage reduction of clonazepam may precipitate acute withdrawal reactions, which can be life-threatening. Inform patients that in some cases, patients taking benzodiazepines have developed a protracted withdrawal syndrome with withdrawal symptoms lasting weeks to more than 12 months. Instruct patients that discontinuation or dosage reduction of clonazepam may require a slow taper (see
WARNINGS: Dependence and Withdrawal ReactionsandDRUG ABUSE AND DEPENDENCE).Interference With Cognitive and Motor PerformanceBecause benzodiazepines have the potential to impair judgment, thinking or motor skills, patients should be cautioned about operating hazardous machinery, including automobiles, until they are reasonably certain that clonazepam therapy does not affect them adversely.
Suicidal Thinking and BehaviorPatients, their caregivers, and families should be counseled that AEDs, including clonazepam, may increase the risk of suicidal thoughts and behavior and should be advised of the need to be alert for the emergence or worsening of symptoms of depression, any unusual changes in mood or behavior, or the emergence of suicidal thoughts, behavior, or thoughts about self-harm. Behaviors of concern should be reported immediately to healthcare providers.
PregnancyAdvise pregnant females that use of clonazepam late in pregnancy can result in sedation (respiratory depression, lethargy, hypotonia) and/or withdrawal symptoms (hyperreflexia, irritability, restlessness, tremors, inconsolable crying, and feeding difficulties) in newborns (see
WARNINGS: Neonatal Sedation and Withdrawal SyndromeandPRECAUTIONS: Pregnancy). Instruct patients to inform their healthcare provider if they are pregnant. Encourage patients to enroll in the North American Antiepileptic Drug (NAAED) Pregnancy Registry if they become pregnant while taking clonazepam. This registry is collecting information about the safety of antiepileptic drugs during pregnancy (seePRECAUTIONS: Pregnancy).NursingInstruct patients to inform their healthcare provider if they are breastfeeding or intend to breastfeed. Instruct breastfeeding patients who take clonazepam to monitor their infants for excessive sedation, poor feeding and poor weight gain, and to seek medical attention if they notice these signs (see
PRECAUTIONS: Nursing Mothers).Concomitant MedicationPatients should be advised to inform their physicians if they are taking, or plan to take, any prescription or over-the-counter drugs, since there is a potential for interactions.
AlcoholPatients should be advised to avoid alcohol while taking clonazepam.
Drug InteractionsEffect of Concomitant Use of Benzodiazepines and OpioidsThe concomitant use of benzodiazepines and opioids increases the risk of respiratory depression because of actions at different receptor sites in the CNS that control respiration. Benzodiazepines interact at GABAAsites, and opioids interact primarily at mu receptors. When benzodiazepines and opioids are combined, the potential for benzodiazepines to significantly worsen opioid-related respiratory depression exists. Limit dosage and duration of concomitant use of benzodiazepines and opioids, and follow patients closely for respiratory depression and sedation.
Effect of Clonazepam on the Pharmacokinetics of Other DrugsClonazepam does not appear to alter the pharmacokinetics of carbamazepine or phenobarbital. Clonazepam has the potential to influence concentrations of phenytoin. Monitoring of phenytoin concentration is recommended when clonazepam is co-administrated with phenytoin. The effect of clonazepam on the metabolism of other drugs has not been investigated.
Effect of Other Drugs on the Pharmacokinetics of ClonazepamLiterature reports suggest that ranitidine, an agent that decreases stomach acidity, does not greatly alter clonazepam pharmacokinetics.
In a study in which the 2 mg clonazepam orally disintegrating tablet was administered with and without propantheline (an anticholinergic agent with multiple effects on the GI tract) to healthy volunteers, the AUC of clonazepam was 10% lower and the Cmaxof clonazepam was 20% lower when the orally disintegrating tablet was given with propantheline compared to when it was given alone.
The selective serotonin reuptake inhibitors sertraline (weak CYP3A4 inducer) and fluoxetine (CYP2D6 inhibitor), and the anti-epileptic drug felbamate (CYP2C19 inhibitor and CYP3A4 inducer) do not affect the pharmacokinetics of clonazepam. Cytochrome P-450 inducers, such as phenytoin, carbamazepine, lamotrigine, and phenobarbital, induce clonazepam metabolism, causing an approximately 38% decrease in plasma clonazepam levels. Although clinical studies have not been performed, based on the involvement of the cytochrome P-450 3A family in clonazepam metabolism, inhibitors of this enzyme system, notably oral antifungal agents (e.g., fluconazole), should be used cautiously in patients receiving clonazepam because they may impair the metabolism of clonazepam leading to exaggerated concentrations and effects.
Pharmacodynamic InteractionsThe CNS-depressant action of the benzodiazepine class of drugs may be potentiated by alcohol, narcotics, barbiturates, nonbarbiturate hypnotics, antianxiety agents, the phenothiazines, thioxanthene and butyrophenone classes of antipsychotic agents, monoamine oxidase inhibitors and the tricyclic antidepressants, and by other anticonvulsant drugs.
Carcinogenesis, Mutagenesis, Impairment of FertilityCarcinogenesisCarcinogenicity studies have not been conducted with clonazepam.
MutagenesisThe data currently available are not sufficient to determine the genotoxic potential of clonazepam.
Impairment of FertilityIn a two-generation fertility study in which clonazepam was given orally to rats at 10 and 100 mg/kg/day, there was a decrease in the number of pregnancies and in the number of offspring surviving until weaning. The lowest dose tested is approximately 5 and 24 times the maximum recommended human dose (MRHD) of 20 mg/day for seizure disorders and 4 mg/day for panic disorder, respectively, on a body surface area (mg/m2) basis.
PregnancyPregnancy Exposure RegistryThere is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to AEDs, such as clonazepam, during pregnancy. Healthcare providers are encouraged to recommend that pregnant women taking clonazepam enroll in the NAAED Pregnancy Registry by calling 1-888-233-2334 or online at http://www.aedpregnancyregistry.org/.
Risk SummaryNeonates born to mothers using benzodiazepines late in pregnancy have been reported to experience symptoms of sedation and/or neonatal withdrawal (see
WARNINGS: Neonatal Sedation and Withdrawal Syndrome, and Clinical Considerations). Available data from published observational studies of pregnant women exposed to benzodiazepines do not report a clear association with benzodiazepines and major birth defects (seeData).Administration of clonazepam to pregnant rabbits during the period of organogenesis resulted in developmental toxicity, including increased incidences of fetal malformations, at doses similar to or below therapeutic doses in patients (see
Animal Data). Data for other benzodiazepines suggest the possibility of long-term effects on neurobehavioral and immunological function in animals following prenatal exposure to benzodiazepines at clinically relevant doses.The background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated risk of major birth defects and of miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Clinical ConsiderationsFetal/Neonatal Adverse ReactionsBenzodiazepines cross the placenta and may produce respiratory depression, hypotonia and sedation in neonates. Monitor neonates exposed to clonazepam during pregnancy or labor for signs of sedation, respiratory depression, hypotonia, and feeding problems. Monitor neonates exposed to clonazepam during pregnancy for signs of withdrawal. Manage these neonates accordingly (see
WARNINGS: Neonatal Sedation and Withdrawal Syndrome).DataHuman DataPublished data from observational studies on the use of benzodiazepines during pregnancy do not report a clear association with benzodiazepines and major birth defects.
Although early studies reported an increased risk of congenital malformations with diazepam and chlordiazepoxide, there was no consistent pattern noted. In addition, the majority of more recent case-control and cohort studies of benzodiazepine use during pregnancy, which were adjusted for confounding exposures to alcohol, tobacco and other medications, have not confirmed these findings.
Animal DataIn three studies in which clonazepam was administered orally to pregnant rabbits at doses of 0.2, 1, 5, or 10 mg/kg/day during the period of organogenesis, a similar pattern of malformations (cleft palate, open eyelid, fused sternebrae and limb defects) was observed at all doses, in a low, non-dose-related incidence. The lowest dose tested is less than the maximum recommended human dose (MRHD) of 20 mg/day for seizure disorders and similar to the MRHD of 4 mg/day for panic disorder, on a mg/m2basis. Reductions in maternal weight gain occurred at doses of 5 mg/kg/day or greater and reduction in embryofetal growth occurred in one study at a dose of 10 mg/kg/day.
No adverse maternal or embryofetal effects were observed in mice or rats following oral administration of clonazepam during organogenesis of doses up to 15 or 40 mg/kg/day, respectively (4 and 20 times the MRHD of 20 mg/day for seizure disorders and 20 and 100 times the MRHD of 4 mg/day for panic disorder, respectively, on a mg/m2basis).
Data for other benzodiazepines suggest the possibility of adverse developmental effects (long-term effects on neurobehavioral and immunological function) in animals following prenatal exposure to benzodiazepines.
Nursing MothersRisk SummaryClonazepam is excreted in human milk. There are reports of sedation, poor feeding and poor weight gain in infants exposed to benzodiazepines through breast milk. There are no data on the effects of clonazepam on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for clonazepam and any potential adverse effects on the breastfed infant from clonazepam or from the underlying maternal condition.
Clinical ConsiderationsInfants exposed to clonazepam through breast milk should be monitored for sedation, poor feeding and poor weight gain.
Pediatric UseBecause of the possibility that adverse effects on physical or mental development could become apparent only after many years, a benefit-risk consideration of the long-term use of clonazepam is important in pediatric patients being treated for seizure disorder (see
INDICATIONS AND USAGEandDOSAGE AND ADMINISTRATION).Safety and effectiveness in pediatric patients with panic disorder below the age of 18 have not been established.
Geriatric UseClinical studies of clonazepam did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
Because clonazepam undergoes hepatic metabolism, it is possible that liver disease will impair clonazepam elimination. Metabolites of clonazepam are excreted by the kidneys; to avoid their excess accumulation, caution should be exercised in the administration of the drug to patients with impaired renal function. Because elderly patients are more likely to have decreased hepatic and/or renal function, care should be taken in dose selection, and it may be useful to assess hepatic and/or renal function at the time of dose selection.
Sedating drugs may cause confusion and over-sedation in the elderly; elderly patients generally should be started on low doses of clonazepam and observed closely.
- The use of benzodiazepines, including clonazepam, exposes users to risks of abuse, misuse, and addiction, which can lead to overdose or death. Abuse and misuse of benzodiazepines commonly involve concomitant use of other medications, alcohol, and/or illicit substances, which is associated with an increased frequency of serious adverse outcomes. Before prescribing clonazepam and throughout treatment, assess each patient’s risk for abuse, misuse, and addiction (see).
WARNINGSRisks from Concomitant Use with OpioidsConcomitant use of benzodiazepines, including clonazepam, and opioids may result in profound sedation, respiratory depression, coma, and death. Because of these risks, reserve concomitant prescribing of benzodiazepines and opioids for patients for whom alternative treatment options are inadequate.
Observational studies have demonstrated that concomitant use of opioid analgesics and benzodiazepines increases the risk of drug-related mortality compared to use of opioids alone. If a decision is made to prescribe clonazepam concomitantly with opioids, prescribe the lowest effective dosages and minimum durations of concomitant use, and follow patients closely for signs and symptoms of respiratory depression and sedation. Advise both patients and caregivers about the risks of respiratory depression and sedation when clonazepam is used with opioids (see
PRECAUTIONS: Information for PatientsandPRECAUTIONS: Drug Interactions)Abuse, Misuse, and AddictionThe use of benzodiazepines, including clonazepam, exposes users to the risks of abuse, misuse, and addiction, which can lead to overdose or death. Abuse and misuse of benzodiazepines often (but not always) involve the use of doses greater than the maximum recommended dosage and commonly involve concomitant use of other medications, alcohol, and/or illicit substances, which is associated with an increased frequency of serious adverse outcomes, including respiratory depression, overdose, or death (see
DRUG ABUSE AND DEPENDENCE: Abuse).Before prescribing clonazepam and throughout treatment, assess each patient’s risk for abuse, misuse, and addiction (e.g., using a standardized screening tool). Use of clonazepam, particularly in patients at elevated risk, necessitates counseling about the risks and proper use of clonazepam along with monitoring for signs and symptoms of abuse, misuse, and addiction. Prescribe the lowest effective dosage; avoid or minimize concomitant use of CNS depressants and other substances associated with abuse, misuse, and addiction (e.g., opioid analgesics, stimulants); and advise patients on the proper disposal of unused drug. If a substance use disorder is suspected, evaluate the patient and institute (or refer them for) early treatment, as appropriate.
Dependence and Withdrawal ReactionsTo reduce the risk of withdrawal reactions, use a gradual taper to discontinue clonazepam or reduce the dosage (a patient-specific plan should be used to taper the dose) (see
DOSAGE AND ADMINISTRATION: Discontinuation or Dosage Reduction of Clonazepam).Patients at an increased risk of withdrawal adverse reactions after benzodiazepine discontinuation or rapid dosage reduction include those who take higher dosages, and those who have had longer durations of use.
Acute Withdrawal ReactionsThe continued use of benzodiazepines, including clonazepam, may lead to clinically significant physical dependence. Abrupt discontinuation or rapid dosage reduction of clonazepam after continued use, or administration of flumazenil (a benzodiazepine antagonist) may precipitate acute withdrawal reactions, which can be life-threatening (e.g., seizures) (see
DRUG ABUSE AND DEPENDENCE: Dependence).Protracted Withdrawal SyndromeIn some cases, benzodiazepine users have developed a protracted withdrawal syndrome with withdrawal symptoms lasting weeks to more than 12 months (see
DRUG ABUSE AND DEPENDENCE: Dependence).Interference with Cognitive and Motor PerformanceSince clonazepam produces CNS depression, patients receiving this drug should be cautioned against engaging in hazardous occupations requiring mental alertness, such as operating machinery or driving a motor vehicle. They should also be warned about the concomitant use of alcohol or other CNS-depressant drugs during clonazepam therapy (see
PRECAUTIONS: Drug InteractionsandPRECAUTIONS: Information for Patients).Suicidal Behavior and IdeationAntiepileptic drugs (AEDs), including clonazepam, increase the risk of suicidal thoughts or behavior in patients taking these drugs for any indication. Patients treated with any AED for any indication should be monitored for the emergence or worsening of depression, suicidal thoughts or behavior, and/or any unusual changes in mood or behavior.
Pooled analyses of 199 placebo-controlled clinical trials (mono- and adjunctive therapy) of 11 different AEDs showed that patients randomized to one of the AEDs had approximately twice the risk (adjusted Relative Risk 1.8, 95% CI:1.2, 2.7) of suicidal thinking or behavior compared to patients randomized to placebo. In these trials, which had a median treatment duration of 12 weeks, the estimated incidence rate of suicidal behavior or ideation among 27,863 AED-treated patients was 0.43% compared to 0.24% among 16,029 placebo-treated patients, representing an increase of approximately one case of suicidal thinking or behavior for every 530 patients treated. There were four suicides in drug-treated patients in the trials and none in placebo-treated patients, but the number is too small to allow any conclusion about drug effect on suicide.
The increased risk of suicidal thoughts or behavior with AEDs was observed as early as one week after starting drug treatment with AEDs and persisted for the duration of treatment assessed. Because most trials included in the analysis did not extend beyond 24 weeks, the risk of suicidal thoughts or behavior beyond 24 weeks could not be assessed.
The risk of suicidal thoughts or behavior was generally consistent among drugs in the data analyzed. The finding of increased risk with AEDs of varying mechanisms of action and across a range of indications suggests that the risk applies to all AEDs used for any indication. The risk did not vary substantially by age (5 to 100 years) in the clinical trials analyzed.
Table 1shows absolute and relative risk by indication for all evaluated AEDs.Table 1 Risk by Indication for Antiepileptic Drugs in the Pooled AnalysisIndicationPlacebo Patients with Events Per 1000 PatientsDrug Patients with Events Per 1000 PatientsRelative Risk: Incidence of Events in Drug Patients/Incidence in Placebo PatientsRisk Difference: Additional Drug Patients with Events per 1000 PatientsEpilepsy
Psychiatric
Other
Total
1.0
5.7
1.0
2.4
3.4
8.5
1.8
4.3
3.5
1.5
1.9
1.8
2.4
2.9
0.9
1.9
The relative risk for suicidal thoughts or behavior was higher in clinical trials for epilepsy than in clinical trials for psychiatric or other conditions, but the absolute risk differences were similar for the epilepsy and psychiatric indications.
Anyone considering prescribing clonazepam or any other AED must balance the risk of suicidal thoughts or behavior with the risk of untreated illness. Epilepsy and many other illnesses for which AEDs are prescribed are themselves associated with morbidity and mortality and with an increased risk of suicidal thoughts and behavior. Should suicidal thoughts and behavior emerge during treatment, the prescriber needs to consider whether the emergence of these symptoms in any given patient may be related to the illness being treated.
Patients, their caregivers, and families should be informed that AEDs increase the risk of suicidal thoughts and behavior and should be advised of the need to be alert for the emergence or worsening of the signs and symptoms of depression, any unusual changes in mood or behavior, or the emergence of suicidal thoughts, behavior, or thoughts about self-harm. Behaviors of concern should be reported immediately to healthcare providers.
Neonatal Sedation and Withdrawal SyndromeUse of clonazepam late in pregnancy can result in sedation (respiratory depression, lethargy, hypotonia) and/or withdrawal symptoms (hyperreflexia, irritability, restlessness, tremors, inconsolable crying, and feeding difficulties) in the neonate (see
PRECAUTIONS: Pregnancy). Monitor neonates exposed to clonazepam during pregnancy or labor for signs of sedation and monitor neonates exposed to clonazepam during pregnancy for signs of withdrawal; manage these neonates accordingly. - The continued use of benzodiazepines, including clonazepam, may lead to clinically significant physical dependence. The risks of dependence and withdrawal increase with longer treatment duration and higher daily dose. Abrupt discontinuation or rapid dosage reduction of clonazepam after continued use may precipitate acute withdrawal reactions, which can be life-threatening. To reduce the risk of withdrawal reactions, use a gradual taper to discontinue clonazepam or reduce the dosage (seeand
DOSAGE AND ADMINISTRATIONClonazepam is available as a tablet. The tablets should be administered with water by swallowing the tablet whole.
Seizure DisordersThe use of multiple anticonvulsants may result in an increase of CNS depressant adverse effects. This should be considered before adding clonazepam to an existing anticonvulsant regimen.
AdultsThe initial dose for adults with seizure disorders should not exceed 1.5 mg/day divided into three doses. Dosage may be increased in increments of 0.5 to 1 mg every 3 days until seizures are adequately controlled or until side effects preclude any further increase. Maintenance dosage must be individualized for each patient depending upon response. Maximum recommended daily dose is 20 mg.
Pediatric PatientsClonazepam tablets are administered orally. In order to minimize drowsiness, the initial dose for infants and children (up to 10 years of age or 30 kg of body weight) should be between 0.01 and 0.03 mg/kg/day but not to exceed 0.05 mg/kg/day given in two or three divided doses. Dosage should be increased by no more than 0.25 to 0.5 mg every third day until a daily maintenance dose of 0.1 to 0.2 mg/kg of body weight has been reached, unless seizures are controlled or side effects preclude further increase. Whenever possible, the daily dose should be divided into three equal doses. If doses are not equally divided, the largest dose should be given before retiring.
Geriatric PatientsThere is no clinical trial experience with clonazepam tablets in seizure disorder patients 65 years of age and older. In general, elderly patients should be started on low doses of clonazepam tablets and observed closely (see
PRECAUTIONS: Geriatric Use).Panic DisorderAdultsThe initial dose for adults with panic disorder is 0.25 mg twice daily. An increase to the target dose for most patients of 1 mg/day may be made after 3 days. The recommended dose of 1 mg/day is based on the results from a fixed dose study in which the optimal effect was seen at 1 mg/day. Higher doses of 2, 3 and 4 mg/day in that study were less effective than the 1 mg/day dose and were associated with more adverse effects. Nevertheless, it is possible that some individual patients may benefit from doses of up to a maximum dose of 4 mg/day, and in those instances, the dose may be increased in increments of 0.125 to 0.25 mg twice daily every 3 days until panic disorder is controlled or until side effects make further increases undesired. To reduce the inconvenience of somnolence, administration of one dose at bedtime may be desirable.
Treatment should be discontinued gradually, with a decrease of 0.125 mg twice daily every 3 days, until the drug is completely withdrawn.
There is no body of evidence available to answer the question of how long the patient treated with clonazepam should remain on it. Therefore, the physician who elects to use clonazepam tablets for extended periods should periodically reevaluate the long-term usefulness of the drug for the individual patient.
Pediatric PatientsThere is no clinical trial experience with clonazepam tablets in panic disorder patients under 18 years of age.
Geriatric PatientsThere is no clinical trial experience with clonazepam tablets in panic disorder patients 65 years of age and older. In general, elderly patients should be started on low doses of clonazepam tablets and observed closely (see
PRECAUTIONS: Geriatric Use).Discontinuation or Dosage Reduction of ClonazepamTo reduce the risk of withdrawal reactions, increased seizure frequency, and status epilepticus, use a gradual taper to discontinue clonazepam or reduce the dosage. If a patient develops withdrawal reactions, consider pausing the taper or increasing the dosage to the previous tapered dosage level. Subsequently decrease the dosage more slowly (see
WARNINGS: Dependence and Withdrawal ReactionsandDRUG ABUSE AND DEPENDENCE: Dependence).).WARNINGSRisks from Concomitant Use with OpioidsConcomitant use of benzodiazepines, including clonazepam, and opioids may result in profound sedation, respiratory depression, coma, and death. Because of these risks, reserve concomitant prescribing of benzodiazepines and opioids for patients for whom alternative treatment options are inadequate.
Observational studies have demonstrated that concomitant use of opioid analgesics and benzodiazepines increases the risk of drug-related mortality compared to use of opioids alone. If a decision is made to prescribe clonazepam concomitantly with opioids, prescribe the lowest effective dosages and minimum durations of concomitant use, and follow patients closely for signs and symptoms of respiratory depression and sedation. Advise both patients and caregivers about the risks of respiratory depression and sedation when clonazepam is used with opioids (see
PRECAUTIONS: Information for PatientsandPRECAUTIONS: Drug Interactions)Abuse, Misuse, and AddictionThe use of benzodiazepines, including clonazepam, exposes users to the risks of abuse, misuse, and addiction, which can lead to overdose or death. Abuse and misuse of benzodiazepines often (but not always) involve the use of doses greater than the maximum recommended dosage and commonly involve concomitant use of other medications, alcohol, and/or illicit substances, which is associated with an increased frequency of serious adverse outcomes, including respiratory depression, overdose, or death (see
DRUG ABUSE AND DEPENDENCE: Abuse).Before prescribing clonazepam and throughout treatment, assess each patient’s risk for abuse, misuse, and addiction (e.g., using a standardized screening tool). Use of clonazepam, particularly in patients at elevated risk, necessitates counseling about the risks and proper use of clonazepam along with monitoring for signs and symptoms of abuse, misuse, and addiction. Prescribe the lowest effective dosage; avoid or minimize concomitant use of CNS depressants and other substances associated with abuse, misuse, and addiction (e.g., opioid analgesics, stimulants); and advise patients on the proper disposal of unused drug. If a substance use disorder is suspected, evaluate the patient and institute (or refer them for) early treatment, as appropriate.
Dependence and Withdrawal ReactionsTo reduce the risk of withdrawal reactions, use a gradual taper to discontinue clonazepam or reduce the dosage (a patient-specific plan should be used to taper the dose) (see
DOSAGE AND ADMINISTRATION: Discontinuation or Dosage Reduction of Clonazepam).Patients at an increased risk of withdrawal adverse reactions after benzodiazepine discontinuation or rapid dosage reduction include those who take higher dosages, and those who have had longer durations of use.
Acute Withdrawal ReactionsThe continued use of benzodiazepines, including clonazepam, may lead to clinically significant physical dependence. Abrupt discontinuation or rapid dosage reduction of clonazepam after continued use, or administration of flumazenil (a benzodiazepine antagonist) may precipitate acute withdrawal reactions, which can be life-threatening (e.g., seizures) (see
DRUG ABUSE AND DEPENDENCE: Dependence).Protracted Withdrawal SyndromeIn some cases, benzodiazepine users have developed a protracted withdrawal syndrome with withdrawal symptoms lasting weeks to more than 12 months (see
DRUG ABUSE AND DEPENDENCE: Dependence).Interference with Cognitive and Motor PerformanceSince clonazepam produces CNS depression, patients receiving this drug should be cautioned against engaging in hazardous occupations requiring mental alertness, such as operating machinery or driving a motor vehicle. They should also be warned about the concomitant use of alcohol or other CNS-depressant drugs during clonazepam therapy (see
PRECAUTIONS: Drug InteractionsandPRECAUTIONS: Information for Patients).Suicidal Behavior and IdeationAntiepileptic drugs (AEDs), including clonazepam, increase the risk of suicidal thoughts or behavior in patients taking these drugs for any indication. Patients treated with any AED for any indication should be monitored for the emergence or worsening of depression, suicidal thoughts or behavior, and/or any unusual changes in mood or behavior.
Pooled analyses of 199 placebo-controlled clinical trials (mono- and adjunctive therapy) of 11 different AEDs showed that patients randomized to one of the AEDs had approximately twice the risk (adjusted Relative Risk 1.8, 95% CI:1.2, 2.7) of suicidal thinking or behavior compared to patients randomized to placebo. In these trials, which had a median treatment duration of 12 weeks, the estimated incidence rate of suicidal behavior or ideation among 27,863 AED-treated patients was 0.43% compared to 0.24% among 16,029 placebo-treated patients, representing an increase of approximately one case of suicidal thinking or behavior for every 530 patients treated. There were four suicides in drug-treated patients in the trials and none in placebo-treated patients, but the number is too small to allow any conclusion about drug effect on suicide.
The increased risk of suicidal thoughts or behavior with AEDs was observed as early as one week after starting drug treatment with AEDs and persisted for the duration of treatment assessed. Because most trials included in the analysis did not extend beyond 24 weeks, the risk of suicidal thoughts or behavior beyond 24 weeks could not be assessed.
The risk of suicidal thoughts or behavior was generally consistent among drugs in the data analyzed. The finding of increased risk with AEDs of varying mechanisms of action and across a range of indications suggests that the risk applies to all AEDs used for any indication. The risk did not vary substantially by age (5 to 100 years) in the clinical trials analyzed.
Table 1shows absolute and relative risk by indication for all evaluated AEDs.Table 1 Risk by Indication for Antiepileptic Drugs in the Pooled AnalysisIndicationPlacebo Patients with Events Per 1000 PatientsDrug Patients with Events Per 1000 PatientsRelative Risk: Incidence of Events in Drug Patients/Incidence in Placebo PatientsRisk Difference: Additional Drug Patients with Events per 1000 PatientsEpilepsy
Psychiatric
Other
Total
1.0
5.7
1.0
2.4
3.4
8.5
1.8
4.3
3.5
1.5
1.9
1.8
2.4
2.9
0.9
1.9
The relative risk for suicidal thoughts or behavior was higher in clinical trials for epilepsy than in clinical trials for psychiatric or other conditions, but the absolute risk differences were similar for the epilepsy and psychiatric indications.
Anyone considering prescribing clonazepam or any other AED must balance the risk of suicidal thoughts or behavior with the risk of untreated illness. Epilepsy and many other illnesses for which AEDs are prescribed are themselves associated with morbidity and mortality and with an increased risk of suicidal thoughts and behavior. Should suicidal thoughts and behavior emerge during treatment, the prescriber needs to consider whether the emergence of these symptoms in any given patient may be related to the illness being treated.
Patients, their caregivers, and families should be informed that AEDs increase the risk of suicidal thoughts and behavior and should be advised of the need to be alert for the emergence or worsening of the signs and symptoms of depression, any unusual changes in mood or behavior, or the emergence of suicidal thoughts, behavior, or thoughts about self-harm. Behaviors of concern should be reported immediately to healthcare providers.
Neonatal Sedation and Withdrawal SyndromeUse of clonazepam late in pregnancy can result in sedation (respiratory depression, lethargy, hypotonia) and/or withdrawal symptoms (hyperreflexia, irritability, restlessness, tremors, inconsolable crying, and feeding difficulties) in the neonate (see
PRECAUTIONS: Pregnancy). Monitor neonates exposed to clonazepam during pregnancy or labor for signs of sedation and monitor neonates exposed to clonazepam during pregnancy for signs of withdrawal; manage these neonates accordingly.
Clonazepam tablets, are useful alone or as an adjunct in the treatment of the Lennox-Gastaut syndrome (petit mal variant), akinetic and myoclonic seizures. In patients with absence seizures (petit mal) who have failed to respond to succinimides, clonazepam tablets, may be useful.
Some loss of effect may occur during the course of clonazepam treatment (see
When used in patients in whom several different types of seizure disorders coexist, clonazepam may increase the incidence or precipitate the onset of generalized tonic-clonic seizures (grand mal). This may require the addition of appropriate anticonvulsants or an increase in their dosages. The concomitant use of valproic acid and clonazepam may produce absence status.
In some studies, up to 30% of patients who initially responded have shown a loss of anticonvulsant activity, often within 3 months of administration. In some cases, dosage adjustment may reestablish efficacy.
Periodic blood counts and liver function tests are advisable during long-term therapy with clonazepam.
Paradoxical reactions, such as agitation, irritability, aggression, anxiety, anger, nightmares, hallucinations, and psychoses are known to occur when using benzodiazepines (see
Metabolites of clonazepam are excreted by the kidneys; to avoid their excess accumulation, caution should be exercised in the administration of the drug to patients with impaired renal function.
Clonazepam may produce an increase in salivation. This should be considered before giving the drug to patients who have difficulty handling secretions.
Clonazepam may cause respiratory depression and should be used with caution in patients with compromised respiratory function (e.g., chronic obstructive pulmonary disease, sleep apnea).
Clonazepam may have a porphyrogenic effect and should be used with care in patients with porphyria.
A clonazepam Medication Guide must be given to the patient each time clonazepam is dispensed, as required by law. Patients should be instructed to take clonazepam only as prescribed. Physicians are advised to discuss the following issues with patients for whom they prescribe clonazepam:
Inform patients and caregivers that potentially fatal additive effects may occur if clonazepam is used with opioids and not to use such drugs concomitantly unless supervised by a health care provider (see
Inform patients that the use of clonazepam, even at recommended dosages, exposes users to risks of abuse, misuse, and addiction, which can lead to overdose and death, especially when used in combination with other medications (e.g., opioid analgesics), alcohol, and/or illicit substances. Inform patients about the signs and symptoms of benzodiazepine abuse, misuse, and addiction; to seek medical help if they develop these signs and/or symptoms; and on the proper disposal of unused drug (see
Inform patients that the continued use of clonazepam may lead to clinically significant physical dependence and that abrupt discontinuation or rapid dosage reduction of clonazepam may precipitate acute withdrawal reactions, which can be life-threatening. Inform patients that in some cases, patients taking benzodiazepines have developed a protracted withdrawal syndrome with withdrawal symptoms lasting weeks to more than 12 months. Instruct patients that discontinuation or dosage reduction of clonazepam may require a slow taper (see
Because benzodiazepines have the potential to impair judgment, thinking or motor skills, patients should be cautioned about operating hazardous machinery, including automobiles, until they are reasonably certain that clonazepam therapy does not affect them adversely.
Patients, their caregivers, and families should be counseled that AEDs, including clonazepam, may increase the risk of suicidal thoughts and behavior and should be advised of the need to be alert for the emergence or worsening of symptoms of depression, any unusual changes in mood or behavior, or the emergence of suicidal thoughts, behavior, or thoughts about self-harm. Behaviors of concern should be reported immediately to healthcare providers.
Advise pregnant females that use of clonazepam late in pregnancy can result in sedation (respiratory depression, lethargy, hypotonia) and/or withdrawal symptoms (hyperreflexia, irritability, restlessness, tremors, inconsolable crying, and feeding difficulties) in newborns (see
Instruct patients to inform their healthcare provider if they are breastfeeding or intend to breastfeed. Instruct breastfeeding patients who take clonazepam to monitor their infants for excessive sedation, poor feeding and poor weight gain, and to seek medical attention if they notice these signs (see
Patients should be advised to inform their physicians if they are taking, or plan to take, any prescription or over-the-counter drugs, since there is a potential for interactions.
Patients should be advised to avoid alcohol while taking clonazepam.
The concomitant use of benzodiazepines and opioids increases the risk of respiratory depression because of actions at different receptor sites in the CNS that control respiration. Benzodiazepines interact at GABAAsites, and opioids interact primarily at mu receptors. When benzodiazepines and opioids are combined, the potential for benzodiazepines to significantly worsen opioid-related respiratory depression exists. Limit dosage and duration of concomitant use of benzodiazepines and opioids, and follow patients closely for respiratory depression and sedation.
Clonazepam does not appear to alter the pharmacokinetics of carbamazepine or phenobarbital. Clonazepam has the potential to influence concentrations of phenytoin. Monitoring of phenytoin concentration is recommended when clonazepam is co-administrated with phenytoin. The effect of clonazepam on the metabolism of other drugs has not been investigated.
Literature reports suggest that ranitidine, an agent that decreases stomach acidity, does not greatly alter clonazepam pharmacokinetics.
In a study in which the 2 mg clonazepam orally disintegrating tablet was administered with and without propantheline (an anticholinergic agent with multiple effects on the GI tract) to healthy volunteers, the AUC of clonazepam was 10% lower and the Cmaxof clonazepam was 20% lower when the orally disintegrating tablet was given with propantheline compared to when it was given alone.
The selective serotonin reuptake inhibitors sertraline (weak CYP3A4 inducer) and fluoxetine (CYP2D6 inhibitor), and the anti-epileptic drug felbamate (CYP2C19 inhibitor and CYP3A4 inducer) do not affect the pharmacokinetics of clonazepam. Cytochrome P-450 inducers, such as phenytoin, carbamazepine, lamotrigine, and phenobarbital, induce clonazepam metabolism, causing an approximately 38% decrease in plasma clonazepam levels. Although clinical studies have not been performed, based on the involvement of the cytochrome P-450 3A family in clonazepam metabolism, inhibitors of this enzyme system, notably oral antifungal agents (e.g., fluconazole), should be used cautiously in patients receiving clonazepam because they may impair the metabolism of clonazepam leading to exaggerated concentrations and effects.
The CNS-depressant action of the benzodiazepine class of drugs may be potentiated by alcohol, narcotics, barbiturates, nonbarbiturate hypnotics, antianxiety agents, the phenothiazines, thioxanthene and butyrophenone classes of antipsychotic agents, monoamine oxidase inhibitors and the tricyclic antidepressants, and by other anticonvulsant drugs.
Carcinogenicity studies have not been conducted with clonazepam.
The data currently available are not sufficient to determine the genotoxic potential of clonazepam.
In a two-generation fertility study in which clonazepam was given orally to rats at 10 and 100 mg/kg/day, there was a decrease in the number of pregnancies and in the number of offspring surviving until weaning. The lowest dose tested is approximately 5 and 24 times the maximum recommended human dose (MRHD) of 20 mg/day for seizure disorders and 4 mg/day for panic disorder, respectively, on a body surface area (mg/m2) basis.
There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to AEDs, such as clonazepam, during pregnancy. Healthcare providers are encouraged to recommend that pregnant women taking clonazepam enroll in the NAAED Pregnancy Registry by calling 1-888-233-2334 or online at http://www.aedpregnancyregistry.org/.
Neonates born to mothers using benzodiazepines late in pregnancy have been reported to experience symptoms of sedation and/or neonatal withdrawal (see
Administration of clonazepam to pregnant rabbits during the period of organogenesis resulted in developmental toxicity, including increased incidences of fetal malformations, at doses similar to or below therapeutic doses in patients (see
The background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated risk of major birth defects and of miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Benzodiazepines cross the placenta and may produce respiratory depression, hypotonia and sedation in neonates. Monitor neonates exposed to clonazepam during pregnancy or labor for signs of sedation, respiratory depression, hypotonia, and feeding problems. Monitor neonates exposed to clonazepam during pregnancy for signs of withdrawal. Manage these neonates accordingly (see
Published data from observational studies on the use of benzodiazepines during pregnancy do not report a clear association with benzodiazepines and major birth defects.
Although early studies reported an increased risk of congenital malformations with diazepam and chlordiazepoxide, there was no consistent pattern noted. In addition, the majority of more recent case-control and cohort studies of benzodiazepine use during pregnancy, which were adjusted for confounding exposures to alcohol, tobacco and other medications, have not confirmed these findings.
In three studies in which clonazepam was administered orally to pregnant rabbits at doses of 0.2, 1, 5, or 10 mg/kg/day during the period of organogenesis, a similar pattern of malformations (cleft palate, open eyelid, fused sternebrae and limb defects) was observed at all doses, in a low, non-dose-related incidence. The lowest dose tested is less than the maximum recommended human dose (MRHD) of 20 mg/day for seizure disorders and similar to the MRHD of 4 mg/day for panic disorder, on a mg/m2basis. Reductions in maternal weight gain occurred at doses of 5 mg/kg/day or greater and reduction in embryofetal growth occurred in one study at a dose of 10 mg/kg/day.
No adverse maternal or embryofetal effects were observed in mice or rats following oral administration of clonazepam during organogenesis of doses up to 15 or 40 mg/kg/day, respectively (4 and 20 times the MRHD of 20 mg/day for seizure disorders and 20 and 100 times the MRHD of 4 mg/day for panic disorder, respectively, on a mg/m2basis).
Data for other benzodiazepines suggest the possibility of adverse developmental effects (long-term effects on neurobehavioral and immunological function) in animals following prenatal exposure to benzodiazepines.
Clonazepam is excreted in human milk. There are reports of sedation, poor feeding and poor weight gain in infants exposed to benzodiazepines through breast milk. There are no data on the effects of clonazepam on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for clonazepam and any potential adverse effects on the breastfed infant from clonazepam or from the underlying maternal condition.
Infants exposed to clonazepam through breast milk should be monitored for sedation, poor feeding and poor weight gain.
Because of the possibility that adverse effects on physical or mental development could become apparent only after many years, a benefit-risk consideration of the long-term use of clonazepam is important in pediatric patients being treated for seizure disorder (see
Safety and effectiveness in pediatric patients with panic disorder below the age of 18 have not been established.
Clinical studies of clonazepam did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
Because clonazepam undergoes hepatic metabolism, it is possible that liver disease will impair clonazepam elimination. Metabolites of clonazepam are excreted by the kidneys; to avoid their excess accumulation, caution should be exercised in the administration of the drug to patients with impaired renal function. Because elderly patients are more likely to have decreased hepatic and/or renal function, care should be taken in dose selection, and it may be useful to assess hepatic and/or renal function at the time of dose selection.
Sedating drugs may cause confusion and over-sedation in the elderly; elderly patients generally should be started on low doses of clonazepam and observed closely.
Clonazepam tablets, are indicated for the treatment of panic disorder, with or without agoraphobia, as defined in DSM-V. Panic disorder is characterized by the occurrence of unexpected panic attacks and associated concern about having additional attacks, worry about the implications or consequences of the attacks, and/or a significant change in behavior related to the attacks.
The efficacy of clonazepam tablets, was established in two 6- to 9-week trials in panic disorder patients whose diagnoses corresponded to the DSM-IIIR category of panic disorder (see
Panic disorder (DSM-V) is characterized by recurrent unexpected panic attacks, i.e., a discrete period of intense fear or discomfort in which four (or more) of the following symptoms develop abruptly and reach a peak within 10 minutes: (1) palpitations, pounding heart or accelerated heart rate; (2) sweating; (3) trembling or shaking; (4) sensations of shortness of breath or smothering; (5) feeling of choking; (6) chest pain or discomfort; (7) nausea or abdominal distress; (8) feeling dizzy, unsteady, lightheaded or faint; (9) derealization (feelings of unreality) or depersonalization (being detached from oneself); (10) fear of losing control; (11) fear of dying; (12) paresthesias (numbness or tingling sensations); (13) chills or hot flushes.
The effectiveness of clonazepam tablets, in long-term use, that is, for more than 9 weeks, has not been systematically studied in controlled clinical trials. The physician who elects to use clonazepam tablets, for extended periods should periodically reevaluate the long-term usefulness of the drug for the individual patient (see
Clonazepam is available as a tablet. The tablets should be administered with water by swallowing the tablet whole.
The use of multiple anticonvulsants may result in an increase of CNS depressant adverse effects. This should be considered before adding clonazepam to an existing anticonvulsant regimen.
The initial dose for adults with seizure disorders should not exceed 1.5 mg/day divided into three doses. Dosage may be increased in increments of 0.5 to 1 mg every 3 days until seizures are adequately controlled or until side effects preclude any further increase. Maintenance dosage must be individualized for each patient depending upon response. Maximum recommended daily dose is 20 mg.
Clonazepam tablets are administered orally. In order to minimize drowsiness, the initial dose for infants and children (up to 10 years of age or 30 kg of body weight) should be between 0.01 and 0.03 mg/kg/day but not to exceed 0.05 mg/kg/day given in two or three divided doses. Dosage should be increased by no more than 0.25 to 0.5 mg every third day until a daily maintenance dose of 0.1 to 0.2 mg/kg of body weight has been reached, unless seizures are controlled or side effects preclude further increase. Whenever possible, the daily dose should be divided into three equal doses. If doses are not equally divided, the largest dose should be given before retiring.
There is no clinical trial experience with clonazepam tablets in seizure disorder patients 65 years of age and older. In general, elderly patients should be started on low doses of clonazepam tablets and observed closely (see
The initial dose for adults with panic disorder is 0.25 mg twice daily. An increase to the target dose for most patients of 1 mg/day may be made after 3 days. The recommended dose of 1 mg/day is based on the results from a fixed dose study in which the optimal effect was seen at 1 mg/day. Higher doses of 2, 3 and 4 mg/day in that study were less effective than the 1 mg/day dose and were associated with more adverse effects. Nevertheless, it is possible that some individual patients may benefit from doses of up to a maximum dose of 4 mg/day, and in those instances, the dose may be increased in increments of 0.125 to 0.25 mg twice daily every 3 days until panic disorder is controlled or until side effects make further increases undesired. To reduce the inconvenience of somnolence, administration of one dose at bedtime may be desirable.
Treatment should be discontinued gradually, with a decrease of 0.125 mg twice daily every 3 days, until the drug is completely withdrawn.
There is no body of evidence available to answer the question of how long the patient treated with clonazepam should remain on it. Therefore, the physician who elects to use clonazepam tablets for extended periods should periodically reevaluate the long-term usefulness of the drug for the individual patient.
There is no clinical trial experience with clonazepam tablets in panic disorder patients under 18 years of age.
There is no clinical trial experience with clonazepam tablets in panic disorder patients 65 years of age and older. In general, elderly patients should be started on low doses of clonazepam tablets and observed closely (see
To reduce the risk of withdrawal reactions, increased seizure frequency, and status epilepticus, use a gradual taper to discontinue clonazepam or reduce the dosage. If a patient develops withdrawal reactions, consider pausing the taper or increasing the dosage to the previous tapered dosage level. Subsequently decrease the dosage more slowly (see
Clonazepam is available as a tablet. The tablets should be administered with water by swallowing the tablet whole.
The use of multiple anticonvulsants may result in an increase of CNS depressant adverse effects. This should be considered before adding clonazepam to an existing anticonvulsant regimen.
The initial dose for adults with seizure disorders should not exceed 1.5 mg/day divided into three doses. Dosage may be increased in increments of 0.5 to 1 mg every 3 days until seizures are adequately controlled or until side effects preclude any further increase. Maintenance dosage must be individualized for each patient depending upon response. Maximum recommended daily dose is 20 mg.
Clonazepam tablets are administered orally. In order to minimize drowsiness, the initial dose for infants and children (up to 10 years of age or 30 kg of body weight) should be between 0.01 and 0.03 mg/kg/day but not to exceed 0.05 mg/kg/day given in two or three divided doses. Dosage should be increased by no more than 0.25 to 0.5 mg every third day until a daily maintenance dose of 0.1 to 0.2 mg/kg of body weight has been reached, unless seizures are controlled or side effects preclude further increase. Whenever possible, the daily dose should be divided into three equal doses. If doses are not equally divided, the largest dose should be given before retiring.
There is no clinical trial experience with clonazepam tablets in seizure disorder patients 65 years of age and older. In general, elderly patients should be started on low doses of clonazepam tablets and observed closely (see
The initial dose for adults with panic disorder is 0.25 mg twice daily. An increase to the target dose for most patients of 1 mg/day may be made after 3 days. The recommended dose of 1 mg/day is based on the results from a fixed dose study in which the optimal effect was seen at 1 mg/day. Higher doses of 2, 3 and 4 mg/day in that study were less effective than the 1 mg/day dose and were associated with more adverse effects. Nevertheless, it is possible that some individual patients may benefit from doses of up to a maximum dose of 4 mg/day, and in those instances, the dose may be increased in increments of 0.125 to 0.25 mg twice daily every 3 days until panic disorder is controlled or until side effects make further increases undesired. To reduce the inconvenience of somnolence, administration of one dose at bedtime may be desirable.
Treatment should be discontinued gradually, with a decrease of 0.125 mg twice daily every 3 days, until the drug is completely withdrawn.
There is no body of evidence available to answer the question of how long the patient treated with clonazepam should remain on it. Therefore, the physician who elects to use clonazepam tablets for extended periods should periodically reevaluate the long-term usefulness of the drug for the individual patient.
There is no clinical trial experience with clonazepam tablets in panic disorder patients under 18 years of age.
There is no clinical trial experience with clonazepam tablets in panic disorder patients 65 years of age and older. In general, elderly patients should be started on low doses of clonazepam tablets and observed closely (see
To reduce the risk of withdrawal reactions, increased seizure frequency, and status epilepticus, use a gradual taper to discontinue clonazepam or reduce the dosage. If a patient develops withdrawal reactions, consider pausing the taper or increasing the dosage to the previous tapered dosage level. Subsequently decrease the dosage more slowly (see
Clonazepam is contraindicated in patients with the following conditions:
- History of sensitivity to benzodiazepines
- Clinical or biochemical evidence of significant liver disease
- Acute narrow angle glaucoma (it may be used in patients with open angle glaucoma who are receiving appropriate therapy).
The adverse experiences for clonazepam are provided separately for patients with seizure disorders and with panic disorder.
The most frequently occurring side effects of clonazepam are referable to CNS depression. Experience in treatment of seizures has shown that drowsiness has occurred in approximately 50% of patients and ataxia in approximately 30%. In some cases, these may diminish with time; behavior problems have been noted in approximately 25% of patients. Others, listed by system, including those identified during postapproval use of clonazepam are:
The following paradoxical reactions have been observed: irritability, aggression, agitation, nervousness, hostility, anxiety, sleep disturbances, nightmares, abnormal dreams, hallucinations.
The stated frequencies of adverse events represent the proportion of individuals who experienced, at least once, a treatment-emergent adverse event of the type listed. An event was considered treatment-emergent if it occurred for the first time or worsened while receiving therapy following baseline evaluation.
Adverse Events Associated
Overall, the incidence of discontinuation due to adverse events was 17% in clonazepam compared to 9% for placebo in the combined data of two 6- to 9-week trials. The most common events (≥1%) associated with discontinuation and a dropout rate twice or greater for clonazepam than that of placebo included the following:
Adverse Event | Clonazepam (N=574) | Placebo (N=294) |
Somnolence | 7% | 1% |
Depression | 4% | 1% |
Dizziness | 1% | <1% |
Nervousness | 1% | 0% |
Ataxia | 1% | 0% |
Intellectual Ability Reduced | 1% | 0% |
The prescriber should be aware that the figures in
*
Clonazepam Maximum Daily Dose | ||||||
Adverse Event by Body System | < 1 mg n=96 % | 1- < 2 mg n=129 % | 2- < 3 mg n=113 % | ≥ 3 mg n=235 % | All Clonazepam Groups N=574 % | Placebo N=294 % |
Central & Peripheral Nervous System | ||||||
Somnolence | 26 | 35 | 50 | 36 | 37 | 10 |
Dizziness | 5 | 5 | 12 | 8 | 8 | 4 |
Coordination Abnormal | 1 | 2 | 7 | 9 | 6 | 0 |
Ataxia | 2 | 1 | 8 | 8 | 5 | 0 |
Dysarthria | 0 | 0 | 4 | 3 | 2 | 0 |
Psychiatric | ||||||
Depression | 7 | 6 | 8 | 8 | 7 | 1 |
Memory Disturbance | 2 | 5 | 2 | 5 | 4 | 2 |
Nervousness | 1 | 4 | 3 | 4 | 3 | 2 |
Intellectual Ability Reduced | 0 | 2 | 4 | 3 | 2 | 0 |
Emotional Lability | 0 | 1 | 2 | 2 | 1 | 1 |
Libido Decreased | 0 | 1 | 3 | 1 | 1 | 0 |
Confusion | 0 | 2 | 2 | 1 | 1 | 0 |
Respiratory System | ||||||
Upper Respiratory Tract Infection | 10 | 10 | 7 | 6 | 8 | 4 |
Sinusitis | 4 | 2 | 8 | 4 | 4 | 3 |
Rhinitis | 3 | 2 | 4 | 2 | 2 | 1 |
Coughing | 2 | 2 | 4 | 0 | 2 | 0 |
Pharyngitis | 1 | 1 | 3 | 2 | 2 | 1 |
Bronchitis | 1 | 0 | 2 | 2 | 1 | 1 |
Gastrointestinal System | ||||||
Constipation | 0 | 1 | 5 | 3 | 2 | 2 |
Appetite Decreased | 1 | 1 | 0 | 3 | 1 | 1 |
Abdominal Pain | 2 | 2 | 2 | 0 | 1 | 1 |
Body as a Whole | ||||||
Fatigue | 9 | 6 | 7 | 7 | 7 | 4 |
Allergic Reaction | 3 | 1 | 4 | 2 | 2 | 1 |
Musculoskeletal | ||||||
Myalgia | 2 | 1 | 4 | 0 | 1 | 1 |
Resistance Mechanism Disorders | ||||||
Influenza | 3 | 2 | 5 | 5 | 4 | 3 |
Urinary System | ||||||
Micturition Frequency | 1 | 2 | 2 | 1 | 1 | 0 |
Urinary Tract Infection | 0 | 0 | 2 | 2 | 1 | 0 |
Vision Disorders | ||||||
Blurred Vision | 1 | 2 | 3 | 0 | 1 | 1 |
Reproductive Disorders ‡ | ||||||
Female | ||||||
Dysmenorrhea | 0 | 6 | 5 | 2 | 3 | 2 |
Colpitis | 4 | 0 | 2 | 1 | 1 | 1 |
Male | ||||||
Ejaculation Delayed | 0 | 0 | 2 | 2 | 1 | 0 |
Impotence | 3 | 0 | 2 | 1 | 1 | 0 |
* Events reported by at least 1% of patients treated with clonazepam and for which the incidence was greater than that for placebo.
†Indicates that the p-value for the dose-trend test (Cochran-Mantel-Haenszel) for adverse event incidence was ≤0.10.
‡Denominators for events in gender-specific systems are: n=240 (clonazepam), 102 (placebo) for male, and 334 (clonazepam), 192 (placebo) for female.
*in Acute Therapy in Pool of 6- to 9-Week Trials
Adverse Event | Clonazepam (N=574) | Placebo (N=294) |
Somnolence | 37% | 10% |
Depression | 7% | 1% |
Coordination Abnormal | 6% | 0% |
Ataxia | 5% | 0% |
* Treatment-emergent events for which the incidence in the clonazepam patients was ≥5% and at least twice that in the placebo patients.
In the pool of two short-term placebo-controlled trials, adverse events classified under the preferred term "depression" were reported in 7% of clonazepam-treated patients compared to 1% of placebo-treated patients, without any clear pattern of dose relatedness. In these same trials, adverse events classified under the preferred term "depression" were reported as leading to discontinuation in 4% of clonazepam-treated patients compared to 1% of placebo-treated patients. While these findings are noteworthy, Hamilton Depression Rating Scale (HAM-D) data collected in these trials revealed a larger decline in HAM-D scores in the clonazepam group than the placebo group suggesting that clonazepam-treated patients were not experiencing a worsening or emergence of clinical depression.
Following is a list of modified CIGY terms that reflect treatment-emergent adverse events reported by patients treated with clonazepam at multiple doses during clinical trials. All reported events are included except those already listed in
Events are further categorized by body system and listed in order of decreasing frequency. These adverse events were reported infrequently, which is defined as occurring in 1/100 to 1/1000 patients.
Clonazepam Tablets, USP, a benzodiazepine, are available as round scored tablets containing 0.5 mg, 1 mg, or 2 mg clonazepam and microcrystalline cellulose, lactose monohydrate, corn starch, and magnesium stearate
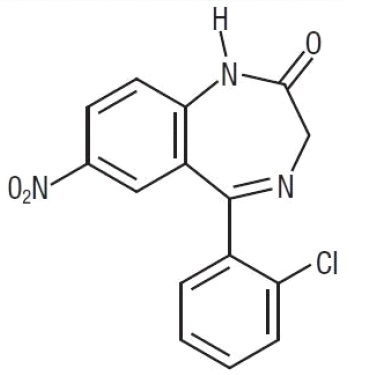
Chemically, clonazepam is 5-(2-chlorophenyl)-1, 3-dihydro-7-nitro-2