Colchicine
Colchicine Prescribing Information
Colchicine tablets are an alkaloid indicated for:
- Familial Mediterranean fever (FMF) in adults and children 4 years or older ().
1.2 Familial Mediterranean Fever (FMF)Colchicine tablets are indicated in adults and children four years or older for treatment of familial Mediterranean fever (FMF).
The long-term use of colchicine is established for FMF.
The recommended dosage of colchicine tablets depends on the patient’s age, renal function, hepatic function and use of coadministered drugs
Coadministration of colchicine tablets with drugs known to inhibit CYP3A4 and/or P-glycoprotein (P-gp) increases the risk of colchicine-induced toxic effects
Strong CYP3A4 Inhibitors† | |||
Drug | Noted or Anticipated Outcome | FMF | |
Original Intended Dosage | Adjusted Dose | ||
| Atazanavir Clarithromycin Darunavir/ Ritonavir‡ Indinavir Itraconazole Ketoconazole Lopinavir/ Ritonavir‡ Nefazodone Nelfinavir Ritonavir Saquinavir Telithromycin Tipranavir/Ritonavir‡ | Significant increase in colchicine plasma levels*; fatal colchicine toxicity has been reported with clarithromycin, a strong CYP3A4 inhibitor. Similarly, significant increase in colchicine plasma levels is anticipated with other strong CYP3A4 inhibitors. | Maximum daily dose of 1.2 – 2.4 mg | Maximum daily dose of 0.6 mg (may be given as 0.3 mg twice a day) |
Moderate CYP3A4 Inhibitors | |||
FMF | |||
Drug | Noted or Anticipated Outcome | Original Intended Dosage | Adjusted Dose |
| Amprenavir‡ Aprepitant Diltiazem Erythromycin Fluconazole Fosamprenavir‡ (prodrug of Amprenavir) Grapefruit juice Verapamil | Significant increase in colchicine plasma concentration is anticipated. Neuromuscular toxicity has been reported with diltiazem and verapamil interactions. | Maximum daily dose of 1.2 – 2.4 mg | Maximum daily dose of 1.2 mg (may be given as 0.6 mg twice a day) |
P-gp Inhibitors† | |||
FMF | |||
Drug | Noted or Anticipated Outcome | Original Intended Dosage | Adjusted Dose |
| Cyclosporine Ranolazine | Significant increase in colchicine plasma levels*; fatal colchicine toxicity has been reported with cyclosporine, a P-gp inhibitor. Similarly, significant increase in colchicine plasma levels is anticipated with other P-gp inhibitors. | Maximum daily dose of 1.2 –2.4 mg | Maximum daily dose of 0.6 mg (may be given as 0.3 mg twice a day) |
*For magnitude of effect on colchicine plasma concentrations
†Patients with renal or hepatic impairment should not be given colchicine tablets in conjunction with strong CYP3A4 or P-gp inhibitors
‡When used in combination with Ritonavir, see dosing recommendations for strong CYP3A4 inhibitors
Protease Inhibitor | Clinical Comment | w/Colchicine-Treatment of FMF |
| Atazanavir sulfate (Reyataz) | Patients with renal or hepatic impairment should not be given colchicine with Reyataz. | Maximum daily dose of 0.6 mg (may be given as 0.3 mg twice a day) |
| Darunavir (Prezista) | Patients with renal or hepatic impairment should not be given colchicine with Prezista/ ritonavir. | Maximum daily dose of 0.6 mg (may be given as 0.3 mg twice a day) |
| Fosamprenavir (Lexiva) with Ritonavir | Patients with renal or hepatic impairment should not be given colchicine with Lexiva/ritonavir. | Maximum daily dose of 0.6 mg (may be given as 0.3 mg twice a day) |
| Fosamprenavir (Lexiva) | Patients with renal or hepatic impairment should not be given colchicine with Lexiva/ritonavir. | Maximum daily dose of 1.2 mg (may be given as 0.6 mg twice a day) |
| Indinavir (Crixivan) | Patients with renal or hepatic impairment should not be given colchicine with Crixivan. | Maximum daily dose of 0.6 mg (may be given as 0.3 mg twice a day) |
| Lopinavir/ Ritonavir (Kaletra) | Patients with renal or hepatic impairment should not be given colchicine with Kaletra. | Maximum daily dose of 0.6 mg (may be given as 0.3 mg twice a day) |
| Nelfinavir mesylate (Viracept) | Patients with renal or hepatic impairment should not be given colchicine with Viracept. | Maximum daily dose of 0.6 mg (may be given as 0.3 mg twice a day) |
| Ritonavir (Norvir) | Patients with renal or hepatic impairment should not be given colchicine with Norvir. | Maximum daily dose of 0.6 mg (may be given as 0.3 mg twice a day) |
| Saquinavir mesylate (Invirase) | Patients with renal or hepatic impairment should not be given colchicine with Invirase/ ritonavir. | Maximum daily dose of 0.6 mg (may be given as 0.3 mg twice a day) |
| Tipranavir (Aptivus) | Patients with renal or hepatic impairment should not be given colchicine with Aptivus/ritonavir. | Maximum daily dose of 0.6 mg (may be given as 0.3 mg twice a day) |
Colchicine dosing must be individualized according to the patient's renal function
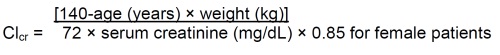
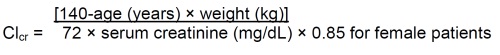
Clcr in mL/minute may be estimated from serum creatinine (mg/dL) determination using the following formula:
Patients with mild to moderate hepatic impairment should be monitored closely for adverse effects of colchicine. Dose reduction should be considered in patients with severe hepatic impairment
Colchicine tablets are administered orally without regard to meals.
Colchicine tablets are not an analgesic medication and should not be used to treat pain from other causes.
Tablets: 0.6 mg colchicine- Purple colored, capsule shaped, film coated tablets debossed with "C6" on one side and scored on the other side.
- In the presence of mild to moderate renal or hepatic impairment, adjustment of dosing is not required for treatment of FMF, but patients should be monitored closely ().
8.6 Renal ImpairmentColchicine is significantly excreted in urine in healthy subjects. Clearance of colchicine is decreased in patients with impaired renal function. Total body clearance of colchicine was reduced by 75% in patients with end-stage renal disease undergoing dialysis.
FMFAlthough, pharmacokinetics of colchicine in patients with mild (Clcr 50 to 80 mL/min) and moderate (Clcr 30 to 50 mL/min) renal impairment is not known, these patients should be monitored closely for adverse effects of colchicine. Dose reduction may be necessary. In patients with severe renal failure (Clcr less than 30 mL/min) and end-stage renal disease requiring dialysis, colchicine tablets may be started at the dose of 0.3 mg/day. Any increase in dose should be done with adequate monitoring of the patient for adverse effects of colchicine tablets
[see Clinical Pharmacology , Dosage and Administration ]. - In FMF patients, start with 0.3 mg/day, and any increase in dose should be done with close monitoring ().
8.6 Renal ImpairmentColchicine is significantly excreted in urine in healthy subjects. Clearance of colchicine is decreased in patients with impaired renal function. Total body clearance of colchicine was reduced by 75% in patients with end-stage renal disease undergoing dialysis.
FMFAlthough, pharmacokinetics of colchicine in patients with mild (Clcr 50 to 80 mL/min) and moderate (Clcr 30 to 50 mL/min) renal impairment is not known, these patients should be monitored closely for adverse effects of colchicine. Dose reduction may be necessary. In patients with severe renal failure (Clcr less than 30 mL/min) and end-stage renal disease requiring dialysis, colchicine tablets may be started at the dose of 0.3 mg/day. Any increase in dose should be done with adequate monitoring of the patient for adverse effects of colchicine tablets
[see Clinical Pharmacology , Dosage and Administration ]. - In patients with severe hepatic impairment, a dose reduction may be needed in FMF patients; (,
8.6 Renal ImpairmentColchicine is significantly excreted in urine in healthy subjects. Clearance of colchicine is decreased in patients with impaired renal function. Total body clearance of colchicine was reduced by 75% in patients with end-stage renal disease undergoing dialysis.
FMFAlthough, pharmacokinetics of colchicine in patients with mild (Clcr 50 to 80 mL/min) and moderate (Clcr 30 to 50 mL/min) renal impairment is not known, these patients should be monitored closely for adverse effects of colchicine. Dose reduction may be necessary. In patients with severe renal failure (Clcr less than 30 mL/min) and end-stage renal disease requiring dialysis, colchicine tablets may be started at the dose of 0.3 mg/day. Any increase in dose should be done with adequate monitoring of the patient for adverse effects of colchicine tablets
[see Clinical Pharmacology , Dosage and Administration ].).8.7 Hepatic ImpairmentThe clearance of colchicine may be significantly reduced and plasma half-life prolonged in patients with chronic hepatic impairment compared to healthy subjects
[see Clinical Pharmacology ].FMFIn patients with severe hepatic disease, dose reduction should be considered with careful monitoring
[see Clinical Pharmacology , Dosage and Administration ]. - For patients undergoing, dialysis, for FMF patients, the starting dose should be 0.3 mg/day and dosing can be increased with close monitoring ().
8.6 Renal ImpairmentColchicine is significantly excreted in urine in healthy subjects. Clearance of colchicine is decreased in patients with impaired renal function. Total body clearance of colchicine was reduced by 75% in patients with end-stage renal disease undergoing dialysis.
FMFAlthough, pharmacokinetics of colchicine in patients with mild (Clcr 50 to 80 mL/min) and moderate (Clcr 30 to 50 mL/min) renal impairment is not known, these patients should be monitored closely for adverse effects of colchicine. Dose reduction may be necessary. In patients with severe renal failure (Clcr less than 30 mL/min) and end-stage renal disease requiring dialysis, colchicine tablets may be started at the dose of 0.3 mg/day. Any increase in dose should be done with adequate monitoring of the patient for adverse effects of colchicine tablets
[see Clinical Pharmacology , Dosage and Administration ]. - Females and Males of Reproductive Potential: Advise males that colchicine may transiently impair fertility ()
8.3 Females and Males of Reproductive PotentialInfertilityCase reports and epidemiology studies in human male subjects on colchicine therapy indicated that infertility from colchicine is rare and may be reversible. A case report indicated that azoospermia was reversed when therapy was stopped. Case reports and epidemiology studies in female subjects on colchicine therapy have not established a clear relationship between colchicine use and female infertility. However, since the progression of FMF without treatment may result in infertility, the use of colchicine needs to be weighed against the potential risks
[see Nonclinical Toxicology ]. - Geriatric Use: The recommended dose of colchicine should be based on renal function ().
8.5 Geriatric UseClinical studies with colchicine for treatment of FMF did not include sufficient numbers of patients aged 65 years and older to determine whether they respond differently from younger patients. In general, dose selection for an elderly patient should be cautious, reflecting the greater frequency of decreased renal function, concomitant disease or other drug therapy
[see Dosage and Administration , Clinical Pharmacology ].
Patients with renal or hepatic impairment should not be given colchicine tablets in conjunction with P-gp or strong CYP3A4 inhibitors (this includes all protease inhibitors except fosamprenavir). In these patients, life-threatening and fatal colchicine toxicity has been reported with colchicine taken in therapeutic doses.
·
Fatal overdoses, both accidental and intentional, have been reported in adults and children who have ingested colchicine
The exact dose of colchicine that produces significant toxicity is unknown. Fatalities have occurred after ingestion of a dose as low as 7 mg over a four day period, while other patients have survived after ingesting more than 60 mg. A review of 150 patients who overdosed on colchicine found that those who ingested less than 0.5 mg/kg survived and tended to have milder toxicities such as gastrointestinal symptoms, whereas those who took 0.5 to 0.8 mg/kg had more severe reactions such as myelosuppression. There was 100% mortality in those who ingested more than 0.8 mg/kg. The first stage of acute colchicine toxicity typically begins within 24 hours of ingestion and includes gastrointestinal symptoms such as abdominal pain, nausea, vomiting, diarrhea and significant fluid loss, leading to volume depletion. Peripheral leukocytosis may also be seen. Life-threatening complications occur during the second stage, which occurs 24 to 72 hours after drug administration, attributed to multiorgan failure and its consequences. Death is usually a result of respiratory depression and cardiovascular collapse. If the patient survives, recovery of multiorgan injury may be accompanied by rebound leukocytosis and alopecia starting about one week after the initial ingestion.
Treatment of colchicine poisoning should begin with gastric lavage and measures to prevent shock. Otherwise, treatment is symptomatic and supportive. No specific antidote is known. Colchicine is not effectively removed by dialysis
·
Myelosuppression, leukopenia, granulocytopenia, thrombocytopenia, pancytopenia and aplastic anemia have been reported with colchicine used in therapeutic doses.
· Monitor for toxicity and if present consider temporary interruption or discontinuation of colchicine (
Myelosuppression, leukopenia, granulocytopenia, thrombocytopenia, pancytopenia and aplastic anemia have been reported with colchicine used in therapeutic doses.
Colchicine is a P-gp and CYP3A4 substrate. Life-threatening and fatal drug interactions have been reported in patients treated with colchicine given with P-gp and strong CYP3A4 inhibitors. If treatment with a P-gp or strong CYP3A4 inhibitor is required in patients with normal renal and hepatic function, the patient’s dose of colchicine may need to be reduced or interrupted
Colchicine-induced neuromuscular toxicity and rhabdomyolysis have been reported with chronic treatment in therapeutic doses. Patients with renal dysfunction and elderly patients, even those with normal renal and hepatic function, are at increased risk. Concomitant use of atorvastatin, simvastatin, pravastatin, fluvastatin, lovastatin, gemfibrozil, fenofibrate, fenofibric acid or benzafibrate (themselves associated with myotoxicity) or cyclosporine with colchicine tablets may potentiate the development of myopathy
Gastrointestinal tract adverse effects are the most frequent side effects in patients initiating colchicine tablets, usually presenting within 24 hours, and occurring in up to 20% of patients given therapeutic doses. Typical symptoms include cramping, nausea, diarrhea, abdominal pain and vomiting. These events should be viewed as dose-limiting if severe, as they can herald the onset of more significant toxicity.
- FMF:Most common adverse reactions (up to 20%) are abdominal pain, diarrhea, nausea and vomiting. These effects are usually mild, transient and reversible upon lowering the dose .
Serious toxic manifestations associated with colchicine include myelosuppression, disseminated intravascular coagulation and injury to cells in the renal, hepatic, circulatory and central nervous systems.
These most often occur with excessive accumulation or overdosage
The following adverse reactions have been identified with colchicine. These have been generally reversible upon temporarily interrupting treatment or lowering the dose of colchicine.
Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
The exact dose of colchicine that produces significant toxicity is unknown. Fatalities have occurred after ingestion of a dose as low as 7 mg over a four day period, while other patients have survived after ingesting more than 60 mg. A review of 150 patients who overdosed on colchicine found that those who ingested less than 0.5 mg/kg survived and tended to have milder toxicities such as gastrointestinal symptoms, whereas those who took 0.5 to 0.8 mg/kg had more severe reactions such as myelosuppression. There was 100% mortality in those who ingested more than 0.8 mg/kg. The first stage of acute colchicine toxicity typically begins within 24 hours of ingestion and includes gastrointestinal symptoms such as abdominal pain, nausea, vomiting, diarrhea and significant fluid loss, leading to volume depletion. Peripheral leukocytosis may also be seen. Life-threatening complications occur during the second stage, which occurs 24 to 72 hours after drug administration, attributed to multiorgan failure and its consequences. Death is usually a result of respiratory depression and cardiovascular collapse. If the patient survives, recovery of multiorgan injury may be accompanied by rebound leukocytosis and alopecia starting about one week after the initial ingestion.
Treatment of colchicine poisoning should begin with gastric lavage and measures to prevent shock. Otherwise, treatment is symptomatic and supportive. No specific antidote is known. Colchicine is not effectively removed by dialysis
·
Colchicine is a P-gp and CYP3A4 substrate. Life-threatening and fatal drug interactions have been reported in patients treated with colchicine given with P-gp and strong CYP3A4 inhibitors. If treatment with a P-gp or strong CYP3A4 inhibitor is required in patients with normal renal and hepatic function, the patient’s dose of colchicine may need to be reduced or interrupted
Colchicine is a substrate of the efflux transporter P-glycoprotein (P-gp). Of the cytochrome P450 enzymes tested, CYP3A4 was mainly involved in the metabolism of colchicine. If colchicine tablets is administered with drugs that inhibit P-gp, most of which also inhibit CYP3A4, increased concentrations of colchicine are likely. Fatal drug interactions have been reported. Physicians should ensure that patients are suitable candidates for treatment with colchicine tablets and remain alert for signs and symptoms of toxicities related to increased colchicine exposure as a result of a drug interaction. Signs and symptoms of colchicine tablets toxicity should be evaluated promptly and, if toxicity is suspected, colchicine tablets should be discontinued immediately. Table 4 provides recommendations as a result of other potentially significant drug interactions. Table 1 provides recommendations for strong and moderate CYP3A4 inhibitors and P-gp inhibitors.
Concomitant Drug Class or Food | Noted or Anticipated Outcome | Clinical Comment |
HMG-Co A Reductase Inhibitors: atorvastatin, fluvastatin, lovastatin, pravastatin, simvastatin | Pharmacokinetic and/or pharmacodynamic interaction: the addition of one drug to a stable long-term regimen of the other has resulted in myopathy and rhabdomyolysis (including a fatality) | Weigh the potential benefits and risks and carefully monitor patients for any signs or symptoms of muscle pain, tenderness, or weakness, particularly during initial therapy; monitoring CPK (creatine phosphokinase) will not necessarily prevent the occurrence of severe myopathy. |
Other Lipid-Lowering Drugs: fibrates, gemfibrozil | ||
Digitalis Glycosides: digoxin | P-gp substrate; rhabdomyolysis has been reported |
Coadministration of P-gp and/or CYP3A4 inhibitors (e.g., clarithromycin or cyclosporine) have been demonstrated to alter the concentration of colchicine. The potential for drug-drug interactions must be considered prior to and during therapy. See FPI for a complete list of reported and potential interactions .
·
Colchicine-induced neuromuscular toxicity and rhabdomyolysis have been reported with chronic treatment in therapeutic doses. Patients with renal dysfunction and elderly patients, even those with normal renal and hepatic function, are at increased risk. Concomitant use of atorvastatin, simvastatin, pravastatin, fluvastatin, lovastatin, gemfibrozil, fenofibrate, fenofibric acid or benzafibrate (themselves associated with myotoxicity) or cyclosporine with colchicine tablets may potentiate the development of myopathy
Colchicine is a substrate of the efflux transporter P-glycoprotein (P-gp). Of the cytochrome P450 enzymes tested, CYP3A4 was mainly involved in the metabolism of colchicine. If colchicine tablets is administered with drugs that inhibit P-gp, most of which also inhibit CYP3A4, increased concentrations of colchicine are likely. Fatal drug interactions have been reported. Physicians should ensure that patients are suitable candidates for treatment with colchicine tablets and remain alert for signs and symptoms of toxicities related to increased colchicine exposure as a result of a drug interaction. Signs and symptoms of colchicine tablets toxicity should be evaluated promptly and, if toxicity is suspected, colchicine tablets should be discontinued immediately. Table 4 provides recommendations as a result of other potentially significant drug interactions. Table 1 provides recommendations for strong and moderate CYP3A4 inhibitors and P-gp inhibitors.
Concomitant Drug Class or Food | Noted or Anticipated Outcome | Clinical Comment |
HMG-Co A Reductase Inhibitors: atorvastatin, fluvastatin, lovastatin, pravastatin, simvastatin | Pharmacokinetic and/or pharmacodynamic interaction: the addition of one drug to a stable long-term regimen of the other has resulted in myopathy and rhabdomyolysis (including a fatality) | Weigh the potential benefits and risks and carefully monitor patients for any signs or symptoms of muscle pain, tenderness, or weakness, particularly during initial therapy; monitoring CPK (creatine phosphokinase) will not necessarily prevent the occurrence of severe myopathy. |
Other Lipid-Lowering Drugs: fibrates, gemfibrozil | ||
Digitalis Glycosides: digoxin | P-gp substrate; rhabdomyolysis has been reported |
Coadministration of P-gp and/or CYP3A4 inhibitors (e.g., clarithromycin or cyclosporine) have been demonstrated to alter the concentration of colchicine. The potential for drug-drug interactions must be considered prior to and during therapy. See FPI for a complete list of reported and potential interactions .