Dabigatran Etexilate Prescribing Information
Premature discontinuation of any oral anticoagulant, including
Epidural or spinal hematomas may occur in patients treated with
• concomitant use of other drugs that affect hemostasis, such as non-steroidal anti-inflammatory drugs (NSAIDs), platelet inhibitors, other anticoagulants
• a history of traumatic or repeated epidural or spinal punctures
• a history of spinal deformity or spinal surgery
• optimal timing between the administration of
When neuraxial anesthesia (spinal/epidural anesthesia) or spinal puncture is employed, patients treated with anticoagulant agents are at risk of developing an epidural or spinal hematoma which can result in long-term or permanent paralysis
To reduce the potential risk of bleeding associated with the concurrent use of dabigatran etexilate capsules and epidural or spinal anesthesia/analgesia or spinal puncture, consider the pharmacokinetic profile of dabigatran
Should the physician decide to administer anticoagulation in the context of epidural or spinal anesthesia/analgesia or lumbar puncture, monitor frequently to detect any signs or symptoms of neurological impairment, such as midline back pain, sensory and motor deficits (numbness, tingling, or weakness in lower limbs), bowel and/or bladder dysfunction. Instruct patients to immediately report if they experience any of the above signs or symptoms. If signs or symptoms of spinal hematoma are suspected, initiate urgent diagnosis and treatment including consideration for spinal cord decompression even though such treatment may not prevent or reverse neurological sequelae.
When neuraxial anesthesia (spinal/epidural anesthesia) or spinal puncture is employed, patients treated with anticoagulant agents are at risk of developing an epidural or spinal hematoma which can result in long-term or permanent paralysis
To reduce the potential risk of bleeding associated with the concurrent use of dabigatran etexilate capsules and epidural or spinal anesthesia/analgesia or spinal puncture, consider the pharmacokinetic profile of dabigatran
Should the physician decide to administer anticoagulation in the context of epidural or spinal anesthesia/analgesia or lumbar puncture, monitor frequently to detect any signs or symptoms of neurological impairment, such as midline back pain, sensory and motor deficits (numbness, tingling, or weakness in lower limbs), bowel and/or bladder dysfunction. Instruct patients to immediately report if they experience any of the above signs or symptoms. If signs or symptoms of spinal hematoma are suspected, initiate urgent diagnosis and treatment including consideration for spinal cord decompression even though such treatment may not prevent or reverse neurological sequelae.
Consider the benefits and risks before neuraxial intervention in patients anticoagulated or to be anticoagulated
When neuraxial anesthesia (spinal/epidural anesthesia) or spinal puncture is employed, patients treated with anticoagulant agents are at risk of developing an epidural or spinal hematoma which can result in long-term or permanent paralysis
To reduce the potential risk of bleeding associated with the concurrent use of dabigatran etexilate capsules and epidural or spinal anesthesia/analgesia or spinal puncture, consider the pharmacokinetic profile of dabigatran
Should the physician decide to administer anticoagulation in the context of epidural or spinal anesthesia/analgesia or lumbar puncture, monitor frequently to detect any signs or symptoms of neurological impairment, such as midline back pain, sensory and motor deficits (numbness, tingling, or weakness in lower limbs), bowel and/or bladder dysfunction. Instruct patients to immediately report if they experience any of the above signs or symptoms. If signs or symptoms of spinal hematoma are suspected, initiate urgent diagnosis and treatment including consideration for spinal cord decompression even though such treatment may not prevent or reverse neurological sequelae.
Dabigatran etexilate capsules are direct thrombin inhibitor indicated:
- To reduce the risk of stroke and systemic embolism in adult patients with non-valvular atrial fibrillation ()
1.1 Reduction of Risk of Stroke and Systemic Embolism in Non-valvular Atrial Fibrillation in Adult PatientsDabigatran etexilate capsules are indicated to reduce the risk of stroke and systemic embolism in adult patients with non-valvular atrial fibrillation.
- For the treatment of deep venous thrombosis (DVT) and pulmonary embolism (PE) in adult patients who have been treated with a parenteral anticoagulant for 5 to 10 days ()1.2 Treatment of Deep Venous Thrombosis and Pulmonary Embolismin Adult Patients
Dabigatran etexilate capsules are indicated for the treatment of deep venous thrombosis and pulmonary embolism in adult patients who have been treated with a parenteral anticoagulant for 5 to 10 days.
- To reduce the risk of recurrence of DVT and PE in adult patients who have been previously treated ()1.3 Reduction in the Risk of Recurrence of Deep Venous Thrombosis and Pulmonary Embolismin Adult Patients
Dabigatran etexilate capsules are indicated to reduce the risk of recurrence of deep venous thrombosis and pulmonary embolism in adult patients who have been previously treated.
- For the prophylaxis of DVT and PE in adult patients who have undergone hip replacement surgery ()1.4 Prophylaxis of Deep Vein Thrombosis and Pulmonary Embolism in Adult Patients Following Hip Replacement Surgery
Dabigatran etexilate capsules are indicated for the prophylaxis of deep vein thrombosis and pulmonary embolism in adult patients who have undergone hip replacement surgery.
Pediatric use information is approved for Boehringer Ingelheim Pharmaceuticals, Inc.’s Pradaxa (dabigatran etexilate) capsules. However, due to Boehringer Ingelheim Pharmaceuticals, Inc.’s marketing exclusivity rights, this drug product is not labeled with that information.
- Non-valvular Atrial Fibrillation in Adult Patients:
For patients with CrCl >30 mL/min: 150 mg orally, twice daily (
)2.4 Dosage AdjustmentsAdult patients with renal impairmentAssess renal function prior to initiation of treatment with dabigatran etexilate capsules. Periodically assess renal function as clinically indicated (i.e., more frequently in clinical situations that may be associated with a decline in renal function) and adjust therapy accordingly. Discontinue dabigatran etexilate capsules in patients who develop acute renal failure while on dabigatran etexilate capsules and consider alternative anticoagulant therapy.
Generally, in adult patients, the extent of anticoagulation does not need to be assessed. When necessary, use aPTT or ECT, and not INR, to assess for anticoagulant activity in adult patients on dabigatran etexilate capsules
[see Warnings and Precautions (5.2)and Clinical Pharmacology (12.2)].Reduction of Risk of Stroke and Systemic Embolism in Non-valvular Atrial FibrillationIn patients with moderate renal impairment (CrCl 30 to 50 mL/min), concomitant use of the P-gp inhibitor dronedarone or systemic ketoconazole can be expected to produce dabigatran exposure similar to that observed in severe renal impairment. Reduce the dosage of dabigatran etexilate capsules to 75 mg twice daily
[see Warnings and Precautions (5.5), Drug Interactions (7.1)and Clinical Pharmacology (12.3)].Treatment and Reduction in the Risk of Recurrence of Deep Venous Thrombosis and Pulmonary EmbolismDosing recommendations for patients with CrCl ≤ 30 mL/min cannot be provided. Avoid use of concomitant P-gp inhibitors in patients with CrCl <50 mL/min
[see Warnings and Precautions , Drug Interactions (7.2) and Clinical Pharmacology].Prophylaxis of Deep Vein Thrombosis and Pulmonary Embolism Following Hip Replacement SurgeryDosing recommendations for patients with CrCl ≤ 30 mL/min or on dialysis cannot be provided. Avoid use of concomitant P-gp inhibitors in patients with CrCl <50 mL/min
[see Dosage and Administration , Warnings and Precautions (5.5), Drug Interactions (7.3) and Clinical Pharmacology (12.2, 12.3)].Pediatric patients with renal impairmentPediatric use information is approved for Boehringer Ingelheim Pharmaceuticals, Inc.’s Pradaxa (dabigatran etexilate) capsules. However, due to Boehringer Ingelheim Pharmaceuticals, Inc.’s marketing exclusivity rights, this drug product is not labeled with that information.
For patients with CrCl 15 to 30 mL/min: 75 mg orally, twice daily (
)2.4 Dosage AdjustmentsAdult patients with renal impairmentAssess renal function prior to initiation of treatment with dabigatran etexilate capsules. Periodically assess renal function as clinically indicated (i.e., more frequently in clinical situations that may be associated with a decline in renal function) and adjust therapy accordingly. Discontinue dabigatran etexilate capsules in patients who develop acute renal failure while on dabigatran etexilate capsules and consider alternative anticoagulant therapy.
Generally, in adult patients, the extent of anticoagulation does not need to be assessed. When necessary, use aPTT or ECT, and not INR, to assess for anticoagulant activity in adult patients on dabigatran etexilate capsules
[see Warnings and Precautions (5.2)and Clinical Pharmacology (12.2)].Reduction of Risk of Stroke and Systemic Embolism in Non-valvular Atrial FibrillationIn patients with moderate renal impairment (CrCl 30 to 50 mL/min), concomitant use of the P-gp inhibitor dronedarone or systemic ketoconazole can be expected to produce dabigatran exposure similar to that observed in severe renal impairment. Reduce the dosage of dabigatran etexilate capsules to 75 mg twice daily
[see Warnings and Precautions (5.5), Drug Interactions (7.1)and Clinical Pharmacology (12.3)].Treatment and Reduction in the Risk of Recurrence of Deep Venous Thrombosis and Pulmonary EmbolismDosing recommendations for patients with CrCl ≤ 30 mL/min cannot be provided. Avoid use of concomitant P-gp inhibitors in patients with CrCl <50 mL/min
[see Warnings and Precautions , Drug Interactions (7.2) and Clinical Pharmacology].Prophylaxis of Deep Vein Thrombosis and Pulmonary Embolism Following Hip Replacement SurgeryDosing recommendations for patients with CrCl ≤ 30 mL/min or on dialysis cannot be provided. Avoid use of concomitant P-gp inhibitors in patients with CrCl <50 mL/min
[see Dosage and Administration , Warnings and Precautions (5.5), Drug Interactions (7.3) and Clinical Pharmacology (12.2, 12.3)].Pediatric patients with renal impairmentPediatric use information is approved for Boehringer Ingelheim Pharmaceuticals, Inc.’s Pradaxa (dabigatran etexilate) capsules. However, due to Boehringer Ingelheim Pharmaceuticals, Inc.’s marketing exclusivity rights, this drug product is not labeled with that information.
- Treatment of DVT and PE in Adult Patients:
For patients with CrCl >30 mL/min: 150 mg orally, twice daily after 5 to10 days of parenteral anticoagulation (
)2.4 Dosage AdjustmentsAdult patients with renal impairmentAssess renal function prior to initiation of treatment with dabigatran etexilate capsules. Periodically assess renal function as clinically indicated (i.e., more frequently in clinical situations that may be associated with a decline in renal function) and adjust therapy accordingly. Discontinue dabigatran etexilate capsules in patients who develop acute renal failure while on dabigatran etexilate capsules and consider alternative anticoagulant therapy.
Generally, in adult patients, the extent of anticoagulation does not need to be assessed. When necessary, use aPTT or ECT, and not INR, to assess for anticoagulant activity in adult patients on dabigatran etexilate capsules
[see Warnings and Precautions (5.2)and Clinical Pharmacology (12.2)].Reduction of Risk of Stroke and Systemic Embolism in Non-valvular Atrial FibrillationIn patients with moderate renal impairment (CrCl 30 to 50 mL/min), concomitant use of the P-gp inhibitor dronedarone or systemic ketoconazole can be expected to produce dabigatran exposure similar to that observed in severe renal impairment. Reduce the dosage of dabigatran etexilate capsules to 75 mg twice daily
[see Warnings and Precautions (5.5), Drug Interactions (7.1)and Clinical Pharmacology (12.3)].Treatment and Reduction in the Risk of Recurrence of Deep Venous Thrombosis and Pulmonary EmbolismDosing recommendations for patients with CrCl ≤ 30 mL/min cannot be provided. Avoid use of concomitant P-gp inhibitors in patients with CrCl <50 mL/min
[see Warnings and Precautions , Drug Interactions (7.2) and Clinical Pharmacology].Prophylaxis of Deep Vein Thrombosis and Pulmonary Embolism Following Hip Replacement SurgeryDosing recommendations for patients with CrCl ≤ 30 mL/min or on dialysis cannot be provided. Avoid use of concomitant P-gp inhibitors in patients with CrCl <50 mL/min
[see Dosage and Administration , Warnings and Precautions (5.5), Drug Interactions (7.3) and Clinical Pharmacology (12.2, 12.3)].Pediatric patients with renal impairmentPediatric use information is approved for Boehringer Ingelheim Pharmaceuticals, Inc.’s Pradaxa (dabigatran etexilate) capsules. However, due to Boehringer Ingelheim Pharmaceuticals, Inc.’s marketing exclusivity rights, this drug product is not labeled with that information.
- Prophylaxis of DVT and PE Following Hip Replacement Surgery in Adult Patients:
For patients with CrCl >30 mL/min: 110 mg orally first day, then 220 mg once daily (
)2.2 Recommended Dabigatran Etexilate Capsules Dosage for AdultsIndicationDosageReduction in Risk of Stroke and Systemic Embolism in Non-valvular AFCrCl > 30 mL/min: 150 mg twice daily CrCl 15 to 30 mL/min: 75 mg twice daily CrCl < 15 mL/min or on dialysis: Dosing recommendations cannot be provided CrCl 30 to 50 mL/min with concomitant use of P-gp inhibitors: Reduce dosage to 75 mg twice daily if given with P-gp inhibitors dronedarone or systemic ketoconazole. CrCl < 30 mL/min with concomitant use of P-gp inhibitors: Avoid coadministration Treatment of DVT and PEReduction in the Risk of Recurrence of DVT and PECrCl > 30 mL/min: 150 mg twice daily CrCl ≤ 30 mL/min or on dialysis: Dosing recommendations cannot be provided CrCl <50 mL/min with concomitant use of P-gp inhibitors: Avoid coadministration Prophylaxis of DVT and PE FollowingHip Replacement SurgeryCrCl > 30 mL/min: CrCl ≤ 30 mL/min or on dialysis: 110 mg for first day, then 220 mg once daily Dosing recommendations cannot be provided CrCl < 50 mL/min with concomitant use of P-gp inhibitors: Avoid coadministration Reduction of Risk of Stroke and Systemic Embolism in Non-valvular Atrial Fibrillation in Adult PatientsFor patients with creatinine clearance (CrCl) >30 mL/min, the recommended dosage of dabigatran etexilate capsules is 150 mg taken orally, twice daily. For patients with severe renal impairment (CrCl 15 to 30 mL/min), the recommended dosage of dabigatran etexilate capsules is 75 mg twice daily
[see Use in Specific Populations (8.6)and Clinical Pharmacology (12.3)].Dosing recommendations for patients with a CrCl < 15 mL/min or on dialysis cannot be provided.Treatment of Deep Venous Thrombosis and Pulmonary Embolismin Adult PatientsFor patients with CrCl > 30 mL/min, the recommended dosage of dabigatran etexilate capsules is 150 mg taken orally, twice daily, after 5 to 10 days of parenteral anticoagulation. Dosing recommendations for patients with a CrCl ≤ 30 mL/min or on dialysis cannot be provided
[see Use in Specific Populations (8.6) and Clinical Pharmacology (12.3)].Reduction in the Risk of Recurrence of Deep Venous Thrombosis and Pulmonary Embolismin Adult PatientsFor patients with CrCl > 30 mL/min, the recommended dosage of dabigatran etexilate capsules is 150 mg taken orally, twice daily after previous treatment. Dosing recommendations for patients with a CrCl ≤30 mL/min or on dialysis cannot be provided
[see Use in Specific Populations (8.6) and Clinical Pharmacology (12.3)].Prophylaxis of Deep Vein Thrombosis and Pulmonary Embolism in Adult Patients Following Hip Replacement SurgeryFor patients with CrCl > 30 mL/min, the recommended dosage of dabigatran etexilate capsules is 110 mg taken orally 1 to 4 hours after surgery and after hemostasis has been achieved, then 220 mg taken once daily for 28 to 35 days. If dabigatran etexilate capsules is not started on the day of surgery, after hemostasis has been achieved initiate treatment with 220 mg once daily. Dosing recommendations for patients with a CrCl ≤30 mL/min or on dialysis cannot be provided
[see Dosage and Administration (2.4), Use in Specific Populations (8.6) and Clinical Pharmacology (12.2, 12.3)].Pediatric use information is approved for Boehringer Ingelheim Pharmaceuticals, Inc.’s Pradaxa (dabigatran etexilate) capsules. However, due to Boehringer Ingelheim Pharmaceuticals, Inc.’s marketing exclusivity rights, this drug product is not labeled with that information.
Dabigatran etexilate capsules are NOT substitutable on a milligram-to- milligram basis with other dabigatran etexilate dosage forms.
Review recommendations for converting to or from other oral or parenteral anticoagulants (
,2.8 Discontinuation for Surgery and Other InterventionsIf possible, discontinue dabigatran etexilate capsules in adults 1 to 2 days (CrCl ≥50 mL/min) or 3 to 5 days (CrCl <50 mL/min) before invasive or surgical procedures because of the increased risk of bleeding. Consider longer times for patients undergoing major surgery, spinal puncture, or placement of a spinal or epidural catheter or port, in whom complete hemostasis may be required
.[see Use in Specific Populations (8.6)and Clinical Pharmacology (12.3)]If surgery cannot be delayed, there is an increased risk of bleeding
[see Warnings and Precautions ].This risk of bleeding should be weighed against the urgency of intervention[see Warnings and Precautions ].Use a specific reversal agent (idarucizumab) in case of emergency surgery or urgent procedures when reversal of the anticoagulant effect of dabigatran is needed in adults. Efficacy and safety of idarucizumab have not been established in pediatric patients[see Warnings and Precautions ].Refer to the idarucizumab prescribing information for additional information. Restart dabigatran etexilate capsules as soon as medically appropriate.Pediatric use information is approved for Boehringer Ingelheim Pharmaceuticals, Inc.’s Pradaxa (dabigatran etexilate) capsules. However, due to Boehringer Ingelheim Pharmaceuticals, Inc.’s marketing exclusivity rights, this drug product is not labeled with that information.)2.7 Converting from or to Parenteral AnticoagulantsFor adult patients currently receiving a parenteral anticoagulant, start dabigatran etexilate capsules 0 to 2 hours before the time that the next dose of the parenteral drug was to have been administered or at the time of discontinuation of a continuously administered parenteral drug (e.g., intravenous unfractionated heparin).
For adult patients currently taking dabigatran etexilate capsules, wait 12 hours (CrCl ≥30 mL/min) or 24 hours (CrCl <30 mL/min) after the last dose of dabigatran etexilate capsules before initiating treatment with a parenteral anticoagulant
.[see Clinical Pharmacology (12.3)]Pediatric use information is approved for Boehringer Ingelheim Pharmaceuticals, Inc.’s Pradaxa (dabigatran etexilate) capsules. However, due to Boehringer Ingelheim Pharmaceuticals, Inc.’s marketing exclusivity rights, this drug product is not labeled with that information.Temporarily discontinue dabigatran etexilate capsules before invasive or surgical procedures when possible, then restart promptly (
)2.8 Discontinuation for Surgery and Other InterventionsIf possible, discontinue dabigatran etexilate capsules in adults 1 to 2 days (CrCl ≥50 mL/min) or 3 to 5 days (CrCl <50 mL/min) before invasive or surgical procedures because of the increased risk of bleeding. Consider longer times for patients undergoing major surgery, spinal puncture, or placement of a spinal or epidural catheter or port, in whom complete hemostasis may be required
.[see Use in Specific Populations (8.6)and Clinical Pharmacology (12.3)]If surgery cannot be delayed, there is an increased risk of bleeding
[see Warnings and Precautions ].This risk of bleeding should be weighed against the urgency of intervention[see Warnings and Precautions ].Use a specific reversal agent (idarucizumab) in case of emergency surgery or urgent procedures when reversal of the anticoagulant effect of dabigatran is needed in adults. Efficacy and safety of idarucizumab have not been established in pediatric patients[see Warnings and Precautions ].Refer to the idarucizumab prescribing information for additional information. Restart dabigatran etexilate capsules as soon as medically appropriate.Pediatric use information is approved for Boehringer Ingelheim Pharmaceuticals, Inc.’s Pradaxa (dabigatran etexilate) capsules. However, due to Boehringer Ingelheim Pharmaceuticals, Inc.’s marketing exclusivity rights, this drug product is not labeled with that information.
150 mg capsules consisting of hypromellose capsule shells with a buff opaque body, light blue opaque cap, imprinted "APO" on cap and "D150" on body in black ink. Filled with light yellow to yellow colored powder.
110 mg capsules consisting of hypromellose capsule shells with a buff opaque body, light blue opaque cap, imprinted "APO" on cap and "D110" on body in black ink. Filled with light yellow to yellow colored powder.
75 mg capsules consisting of hypromellose capsule shells with a buff opaque body, light blue opaque cap, imprinted "APO" on cap and "D75" on body in black ink. Filled with light yellow to yellow colored powder.
Lactation: Breastfeeding not recommended (
)8.2 LactationRisk SummaryThere are insufficient data to assess the presence of dabigatran in human milk. There are no data on the effects of dabigatran on the breastfed child, or on milk production. Dabigatran and/or its metabolites were present in rat milk. Breastfeeding is not recommended during treatment with dabigatran etexilate capsules.
- Geriatric Use: Risk of bleeding increases with age ()
8.5 Geriatric UseOf
the total number of patients in the RE-LY study, 82% were 65 and over,
while 40% were 75 and over. The risk of stroke and bleeding increases
with age, but the risk-benefit profile is favorable in all age groups[see Warnings and Precautions (5),.
Adverse Reactions (6.1), and Clinical
Studies (14.1)]
Dabigatran etexilate capsules are contraindicated in patients with:
- Active pathological bleeding [see Warnings and Precautionsand Adverse Reactions
5.2 Risk of BleedingDabigatran etexilate capsules increases the risk of bleeding and can cause significant and, sometimes, fatal bleeding. Promptly evaluate any signs or symptoms of blood loss (e.g., a drop in hemoglobin and/or hematocrit or hypotension). Discontinue dabigatran etexilate capsules in patients with active pathological bleeding
.[see Dosage and Administration (2.4)]Risk factors for bleeding include the concomitant use of other drugs that increase the risk of bleeding (e.g., anti-platelet agents, heparin, fibrinolytic therapy, and chronic use of NSAIDs). Dabigatran etexilate capsule’s anticoagulant activity and half-life are increased in patients with renal impairment
.[see Clinical Pharmacology (12.2)]Reversal of Anticoagulant Effect:In adults, a specific reversal agent (idarucizumab) for dabigatran etexilate capsules is available when reversal of the anticoagulant effect of dabigatran is needed:
- For emergency surgery/urgent procedures
- In life-threatening or uncontrolled bleeding
In pediatric patients, the efficacy and safety of idarucizumab have not been established.
Hemodialysis can remove dabigatran; however the clinical experience supporting the use of hemodialysis as a treatment for bleeding is limited
[see Overdosage ]. Prothrombin complex concentrates, or recombinant Factor VIIa may be considered but their use has not been evaluated in clinical trials. Protamine sulfate and vitamin K are not expected to affect the anticoagulant activity of dabigatran. Consider administration of platelet concentrates in cases where thrombocytopenia is present or long-acting antiplatelet drugs have been used.]6.1 Clinical Trials ExperienceBecause clinical trials are conducted under widely varying conditions, adverse reactions rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Adult TrialsReduction of Risk of Stroke and Systemic Embolism in Non-valvular Atrial FibrillationThe RE-LY (Randomized Evaluation of Long-term Anticoagulant Therapy) study provided safety information on the use of two doses of dabigatran etexilate capsules and warfarin
[see Clinical Studies (14.1)]. The numbers of patients and their exposures are described in Table 2. Limited information is presented on the 110 mg dosing arm because this dose is not approved.Table 2 Summary of Treatment Exposure in RE-LY Dabigatran etexilate capsules110 mg twice dailyDabigatran etexilate capsules150 mg twice dailyWarfarinTotal number treated 5,983 6,059 5,998 Exposure > 12 months 4,936 4,939 5,193 > 24 months 2,387 2,405 2,470 Mean exposure (months) 20.5 20.3 21.3 Total patient-years 10,242 10,261 10,659 Drug Discontinuation in RE-LYThe rates of adverse reactions leading to treatment discontinuation were 21% for dabigatran etexilate capsules 150 mg and 16% for warfarin. The most frequent adverse reactions leading to discontinuation of dabigatran etexilate capsules were bleeding and gastrointestinal events (i.e., dyspepsia, nausea, upper abdominal pain, gastrointestinal hemorrhage, and diarrhea).
Bleeding[see Warnings and Precautions (5.2)]Table 3 shows the number of adjudicated major bleeding events during the treatment period in the RE-LY study, with the bleeding rate per 100 subject-years (%). Major bleeding is defined as bleeding accompanied by one or more of the following: a decrease in hemoglobin of ≥2 g/dL, a transfusion of ≥2 units of packed red blood cells, bleeding at a critical site or with a fatal outcome. Intracranial hemorrhage included intracerebral (hemorrhagic stroke), subarachnoid, and subdural bleeds.
Table 3 Adjudicated Major Bleeding Events in Treated Patientsa aPatients during treatment or within 2 days of stopping study treatment. Major bleeding events within each subcategory were counted once per patient, but patients may have contributed events to multiple subcategories.
bAnnual event rate per 100 pt-years = 100 * number of subjects with event/subject-years. Subject-years is defined as cumulative number of days from first drug intake to event date, date of last drug intake + 2, death date (whatever occurred first) across all treated subjects divided by 365.25. In case of recurrent events of the same category, the first event was considered.
cDefined as bleeding accompanied by one or more of the following: a decrease in hemoglobin of ≥2 g/dL, a transfusion of 2 or more units of packed red blood cells, bleeding at a critical site or with fatal outcome.
dIntracranial bleed included intracerebral (hemorrhagic stroke), subarachnoid, and subdural bleeds.
eOn-treatment analysis based on the safety population, compared to ITT analysis presented in Section 14 Clinical Studies.
fFatal bleed: Adjudicated major bleed as defined above with investigator reported fatal outcome and adjudicated death with primary cause from bleeding.
gNon-intracranial fatal bleed: Adjudicated major bleed as defined above and adjudicated death with primary cause from bleeding but without symptomatic intracranial bleed based on investigator’s clinical assessment.
EventDabigatran etexilate capsules150 mg
N = 6,059
n (%/yearb)Warfarin
N = 5,998
n (%/yearb)Dabigatran etexilate capsules 150 mg
vs Warfarin
HR (95% CI)Major Bleedingc 350 (3.47) 374 (3.58) 0.97 (0.84, 1.12) Intracranial Hemorrhage (ICH)d 23 (0.22) 82 (0.77) 0.29 (0.18, 0.46) Hemorrhagic Strokee 6 (0.06) 40 (0.37) 0.16 (0.07, 0.37) Other ICH 17 (0.17) 46 (0.43) 0.38 (0.22, 0.67) Gastrointestinal 162 (1.59) 111 (1.05) 1.51 (1.19, 1.92) Fatal Bleedingf 7 (0.07) 16 (0.15) 0.45 (0.19, 1.10) ICH 3 (0.03) 9 (0.08) 0.35 (0.09, 1.28) Non-intracranialg 4 (0.04) 7 (0.07) 0.59 (0.17, 2.02) There was a higher rate of any gastrointestinal bleeds in patients receiving dabigatran etexilate capsules 150 mg than in patients receiving warfarin (6.6% vs 4.2%, respectively).
The risk of major bleeds was similar with dabigatran etexilate capsules 150 mg and warfarin across major subgroups defined by baseline characteristics (see Figure 1), with the exception of age, where there was a trend toward a higher incidence of major bleeding on dabigatran etexilate capsules (hazard ratio 1.2, 95% CI: 1 to 1.5) for patients ≥75 years of age.
Figure 1 Adjudicated Major Bleeding by Baseline Characteristics Including Hemorrhagic Stroke Treated Patients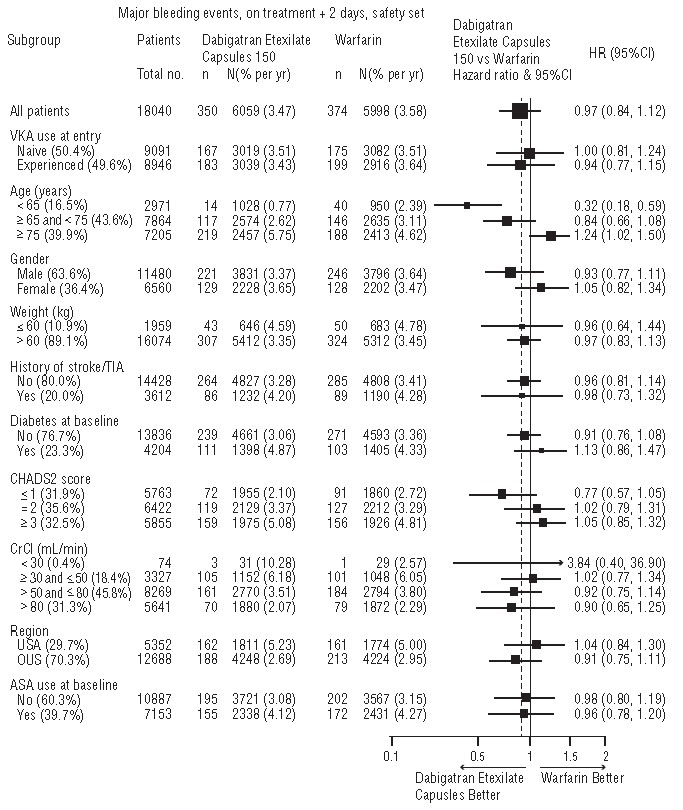
Note: The figure above presents effects in various subgroups all of which are baseline characteristics and all of which were pre-specified. The 95% confidence limits that are shown do not take into account how many comparisons were made, nor do they reflect the effect of a particular factor after adjustment for all other factors. Apparent homogeneity or heterogeneity among groups should not be over-interpreted.
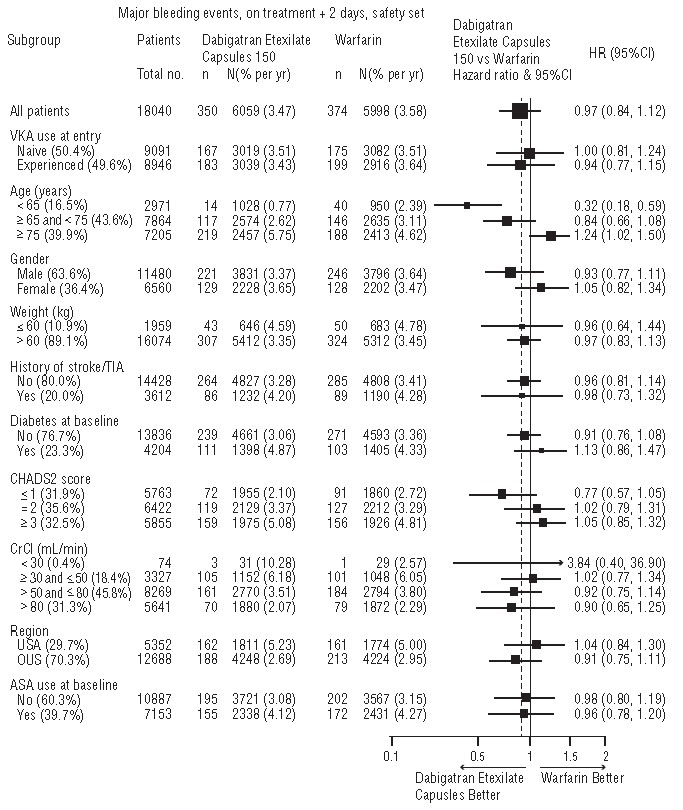
Figure 1 Gastrointestinal Adverse ReactionsPatients on dabigatran etexilate capsules 150 mg had an increased incidence of gastrointestinal adverse reactions (35% vs 24% on warfarin). These were commonly dyspepsia (including abdominal pain upper, abdominal pain, abdominal discomfort, and epigastric discomfort) and gastritis-like symptoms (including GERD, esophagitis, erosive gastritis, gastric hemorrhage, hemorrhagic gastritis, hemorrhagic erosive gastritis, and gastrointestinal ulcer).
Hypersensitivity ReactionsIn the RE-LY study, drug hypersensitivity (including urticaria, rash, and pruritus), allergic edema, anaphylactic reaction, and anaphylactic shock were reported in <0.1% of patients receiving dabigatran etexilate capsules.
Treatment and Reduction in the Risk of Recurrence of Deep Venous Thrombosis and Pulmonary EmbolismDabigatran etexilate capsules were studied in 4,387 patients in 4 pivotal, parallel, randomized, double-blind trials. Three of these trials were active-controlled (warfarin) (RE-COVER, RE-COVER II, and RE-MEDY), and one study (RE-SONATE) was placebo-controlled. The demographic characteristics were similar among the 4 pivotal studies and between the treatment groups within these studies. Approximately 60% of the treated patients were male, with a mean age of 55.1 years. The majority of the patients were white (87.7%), 10.3% were Asian, and 1.9% were black with a mean CrCl of 105.6 mL/min.
Bleeding events for the 4 pivotal studies were classified as major bleeding events if at least one of the following criteria applied: fatal bleeding, symptomatic bleeding in a critical area or organ (intraocular, intracranial, intraspinal or intramuscular with compartment syndrome, retroperitoneal bleeding, intra-articular bleeding, or pericardial bleeding), bleeding causing a fall in hemoglobin level of 2 g/dL (1.24 mmol/L or more, or leading to transfusion of 2 or more units of whole blood or red cells).
RE-COVER and RE-COVER II studies compared dabigatran etexilate capsules 150 mg twice daily and warfarin for the treatment of deep vein thrombosis and pulmonary embolism. Patients received 5 to 10 days of an approved parenteral anticoagulant therapy followed by 6 months, with mean exposure of 164 days, of oral only treatment; warfarin was overlapped with parenteral therapy. Table 4 shows the number of patients experiencing bleeding events in the pooled analysis of RE-COVER and RE-COVER II studies during the full treatment including parenteral and oral only treatment periods after randomization.
Table 4 Bleeding Events in RE-COVER and RE-COVER II Treated PatientsBleeding Events-Full Treatment Period Including Parenteral TreatmentDabigatran etexilate capsules
150 mg twice daily
N (%)Warfarin
N (%)Hazard Ratio
(95% CI)cPatientsN=2,553N=2,554Major bleeding eventa 37 (1.4) 51 (2.0) 0.73 (0.48, 1.11) Fatal bleeding 1 (0.04) 2 (0.1) Bleeding in a critical area or organ 7 (0.3) 15 (0.6) Fall in hemoglobin ≥2 g/dL or transfusion ≥2 units of whole blood or packed red blood cells 32 (1.3) 38 (1.5) Bleeding sites for MBEb Intracranial 2 (0.1) 5 (0.2) Retroperitoneal 2 (0.1) 1 (0.04) Intraarticular 2 (0.1) 4 (0.2) Intramuscular 2 (0.1) 6 (0.2) Gastrointestinal 15 (0.6) 14 (0.5) Urogenital 7 (0.3) 14 (0.5) Other 8 (0.3) 8 (0.3) Clinically relevant non-major bleeding 101 (4.0) 170 (6.7) 0.58 (0.46, 0.75) Any bleeding 411 (16.1) 567 (22.7) 0.70 (0.61, 0.79) Note: MBE can belong to more than one criterion.
aPatients with at least one MBE.
bBleeding site based on investigator assessment. Patients can have more than one site of bleeding.
cConfidence interval
The rate of any gastrointestinal bleeds in patients receiving dabigatran etexilate capsules 150 mg in the full treatment period was 3.1% (2.4% on warfarin).
The RE-MEDY and RE-SONATE studies provided safety information on the use of dabigatran etexilate capsules for the reduction in the risk of recurrence of deep vein thrombosis and pulmonary embolism.
RE-MEDY was an active-controlled study (warfarin) in which 1,430 patients received dabigatran etexilate capsules 150 mg twice daily following 3 to 12 months of oral anticoagulant regimen. Patients in the treatment studies who rolled over into the RE-MEDY study had a combined treatment duration of up to more than 3 years, with mean exposure of 473 days. Table 5 shows the number of patients experiencing bleeding events in the study.
Table 5 Bleeding Events in RE-MEDY Treated PatientsDabigatran etexilate capsules
150 mg twice daily
N (%)Warfarin
N (%)Hazard Ratio
(95% CI)cPatientsN=1,430N=1,426Major bleeding eventa 13 (0.9) 25 (1.8) 0.54 (0.25, 1.16) Fatal bleeding 0 1 (0.1) Bleeding in a critical area or organ 7 (0.5) 11 (0.8) Fall in hemoglobin ≥2 g/dL or transfusion ≥2 units of whole blood or packed red blood cells 7 (0.5) 16 (1.1) Bleeding sites for MBEb Intracranial 2 (0.1) 4 (0.3) Intraocular 4 (0.3) 2 (0.1) Retroperitoneal 0 1 (0.1) Intraarticular 0 2 (0.1) Intramuscular 0 4 (0.3) Gastrointestinal 4 (0.3) 8 (0.6) Urogenital 1 (0.1) 1 (0.1) Other 2 (0.1) 4 (0.3) Clinically relevant non-major bleeding 71 (5.0) 125 (8.8) 0.56 (0.42, 0.75) Any bleeding 278 (19.4) 373 (26.2) 0.71 (0.61, 0.83) Note: MBE can belong to more than one criterion.
aPatients with at least one MBE.
bBleeding site based on investigator assessment. Patients can have more than one site of bleeding.
cConfidence interval
In the RE-MEDY study, the rate of any gastrointestinal bleeds in patients receiving dabigatran etexilate capsules 150 mg was 3.1% (2.2% on warfarin).
RE-SONATE was a placebo-controlled study in which 684 patients received dabigatran etexilate capsules 150 mg twice daily following 6 to 18 months of oral anticoagulant regimen. Patients in the treatment studies who rolled over into the RE-SONATE study had combined treatment duration up to 9 months, with mean exposure of 165 days. Table 6 shows the number of patients experiencing bleeding events in the study.
Table 6 Bleeding Events in RE-SONATE Treated PatientsDabigatran etexilate capsules
150 mg twice daily
N (%)Placebo
N (%)Hazard Ratio
(95% CI)cPatientsN=684N=659Major bleeding eventa 2 (0.3) 0 Bleeding in a critical area or organ 0 0 Gastrointestinalb 2 (0.3) 0 Clinically relevant non-major bleeding 34 (5.0) 13 (2.0) 2.54 (1.34, 4.82) Any bleeding 72 (10.5) 40 (6.1) 1.77 (1.20, 2.61) Note: MBE can belong to more than one criterion.
aPatients with at least one MBE.
bBleeding site based on investigator assessment. Patients can have more than one site of bleeding.
cConfidence interval
In the RE-SONATE study, the rate of any gastrointestinal bleeds in patients receiving dabigatran etexilate capsules 150 mg was 0.7% (0.3% on placebo).
Clinical Myocardial Infarction EventsIn the active-controlled VTE studies, a higher rate of clinical myocardial infarction was reported in patients who received dabigatran etexilate capsules [20 (0.66 per 100 patient-years)] than in those who received warfarin [5 (0.17 per 100 patient-years)]. In the placebo-controlled study, a similar rate of nonfatal and fatal clinical myocardial infarction was reported in patients who received dabigatran etexilate capsules [1 (0.32 per 100 patient-years)] and in those who received placebo [1 (0.34 per 100 patient-years)].
Gastrointestinal Adverse ReactionsIn the four pivotal studies, patients on dabigatran etexilate capsules 150 mg had a similar incidence of gastrointestinal adverse reactions (24.7% vs 22.7% on warfarin). Dyspepsia (including abdominal pain upper, abdominal pain, abdominal discomfort, and epigastric discomfort) occurred in patients on dabigatran etexilate capsules 7.5% vs 5.5% on warfarin, and gastritis-like symptoms (including gastritis, GERD, esophagitis, erosive gastritis and gastric hemorrhage) occurred at 3% vs 1.7%, respectively.
Hypersensitivity ReactionsIn the 4 pivotal studies, drug hypersensitivity (including urticaria, rash, and pruritus), allergic edema, anaphylactic reaction, and anaphylactic shock were reported in 0.1% of patients receiving dabigatran etexilate capsules.Prophylaxis of Deep Vein Thrombosis and Pulmonary Embolism Following Hip Replacement SurgeryDabigatran etexilate capsules was studied in 5,476 patients, randomized and treated in two double-blind, active-controlled non-inferiority trials (RE-NOVATE and RE-NOVATE II). The demographic characteristics were similar across the two studies and between the treatment groups within these studies. Approximately 45.3% of the treated patients were male, with a mean age of 63.2 years. The majority of the patients were white (96.1%), 3.6% were Asian, and 0.3% were black with a mean CrCl of 92 mL/min.
Bleeding events for the RE-NOVATE and RE-NOVATE II studies were classified as major bleeding events if at least one of the following criteria applied: fatal bleeding, symptomatic bleeding in a critical area or organ (intraocular, intracranial, intraspinal or retroperitoneal bleeding), bleeding causing a fall in hemoglobin level of 2 g/dL (1.24 mmol/L) or more, or leading to transfusion of 2 or more units of whole blood or red cells, requiring treatment cessation or leading to re-operation.
The RE-NOVATE study compared dabigatran etexilate capsules 75 mg taken orally 1 to 4 hours after surgery followed by 150 mg once daily, dabigatran etexilate capsules 110 mg taken orally 1 to 4 hours after surgery followed by 220 mg once daily and subcutaneous enoxaparin 40 mg once daily initiated the evening before surgery for the prophylaxis of deep vein thrombosis and pulmonary embolism in patients who had undergone hip replacement surgery. The RE-NOVATE II study compared dabigatran etexilate capsules 110 mg taken orally 1 to 4 hours after surgery followed by 220 mg once daily and subcutaneous enoxaparin 40 mg once daily initiated the evening before surgery for the prophylaxis of deep vein thrombosis and pulmonary embolism in patients who had undergone hip replacement surgery. In the RE-NOVATE and RE-NOVATE II studies, patients received 28 to 35 days of dabigatran etexilate capsules or enoxaparin with median exposure of 33 days. Tables 7 and 8 show the number of patients experiencing bleeding events in the analysis of RE-NOVATE and RE-NOVATE II.
Table 7 Bleeding Events in RE-NOVATE Treated PatientsDabigatran Etexilate Capsules
220 mg
N (%)Enoxaparin
N (%)PatientsN=1,146N=1,154Major bleeding event 23 (2.0) 18 (1.6) Clinically relevant non-major bleeding 48 (4.2) 40 (3.5) Any bleeding 141 (12.3) 132 (11.4) Table 8 Bleeding Events in RE-NOVATE II Treated PatientsDabigatran Etexilate Capsules
220 mg
N (%)Enoxaparin
N (%)PatientsN=1,010N=1,003Major bleeding event 14 (1.4) 9 (0.9) Clinically relevant non-major bleeding 26 (2.6) 20 (2.0) Any bleeding 98 (9.7) 83 (8.3) In the two studies, the rate of major gastrointestinal bleeds in patients receiving dabigatran etexilate capsules and enoxaparin was the same (0.1%) and for any gastrointestinal bleeds was 1.4% for dabigatran etexilate capsules 220 mg and 0.9% for enoxaparin.
Gastrointestinal Adverse ReactionsIn the two studies, the incidence of gastrointestinal adverse reactions for patients on dabigatran etexilate capsules 220 mg and enoxaparin was 39.5% and 39.5%, respectively. Dyspepsia (including abdominal pain upper, abdominal pain, abdominal discomfort, and epigastric discomfort) occurred in patients on dabigatran etexilate capsules 220 mg in 4.1% vs. 3.8% on enoxaparin, and gastritis-like symptoms (including gastritis, GERD, esophagitis, erosive gastritis and gastric hemorrhage) occurred at 0.6% vs 1%, respectively.
Hypersensitivity ReactionsIn the two studies, drug hypersensitivity (such as urticaria, rash, and pruritus) was reported in 0.3% of patients receiving dabigatran etexilate capsules 220 mg.
Clinical Myocardial Infarction EventsIn the two studies, clinical myocardial infarction was reported in 2 (0.1%) of patients who received dabigatran etexilate capsules 220 mg and 6 (0.3%) of patients who received enoxaparin.
Pediatric use information is approved for Boehringer Ingelheim Pharmaceuticals, Inc.’s Pradaxa (dabigatran etexilate) capsules. However, due to Boehringer Ingelheim Pharmaceuticals, Inc.’s marketing exclusivity rights, this drug product is not labeled with that information. - History of a serious hypersensitivity reaction to dabigatran, dabigatran etexilate, or to one of the excipients of the product (e.g., anaphylactic reaction or anaphylactic shock) [see Adverse Reactions]
6.1 Clinical Trials ExperienceBecause clinical trials are conducted under widely varying conditions, adverse reactions rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Adult TrialsReduction of Risk of Stroke and Systemic Embolism in Non-valvular Atrial FibrillationThe RE-LY (Randomized Evaluation of Long-term Anticoagulant Therapy) study provided safety information on the use of two doses of dabigatran etexilate capsules and warfarin
[see Clinical Studies (14.1)]. The numbers of patients and their exposures are described in Table 2. Limited information is presented on the 110 mg dosing arm because this dose is not approved.Table 2 Summary of Treatment Exposure in RE-LY Dabigatran etexilate capsules110 mg twice dailyDabigatran etexilate capsules150 mg twice dailyWarfarinTotal number treated 5,983 6,059 5,998 Exposure > 12 months 4,936 4,939 5,193 > 24 months 2,387 2,405 2,470 Mean exposure (months) 20.5 20.3 21.3 Total patient-years 10,242 10,261 10,659 Drug Discontinuation in RE-LYThe rates of adverse reactions leading to treatment discontinuation were 21% for dabigatran etexilate capsules 150 mg and 16% for warfarin. The most frequent adverse reactions leading to discontinuation of dabigatran etexilate capsules were bleeding and gastrointestinal events (i.e., dyspepsia, nausea, upper abdominal pain, gastrointestinal hemorrhage, and diarrhea).
Bleeding[see Warnings and Precautions (5.2)]Table 3 shows the number of adjudicated major bleeding events during the treatment period in the RE-LY study, with the bleeding rate per 100 subject-years (%). Major bleeding is defined as bleeding accompanied by one or more of the following: a decrease in hemoglobin of ≥2 g/dL, a transfusion of ≥2 units of packed red blood cells, bleeding at a critical site or with a fatal outcome. Intracranial hemorrhage included intracerebral (hemorrhagic stroke), subarachnoid, and subdural bleeds.
Table 3 Adjudicated Major Bleeding Events in Treated Patientsa aPatients during treatment or within 2 days of stopping study treatment. Major bleeding events within each subcategory were counted once per patient, but patients may have contributed events to multiple subcategories.
bAnnual event rate per 100 pt-years = 100 * number of subjects with event/subject-years. Subject-years is defined as cumulative number of days from first drug intake to event date, date of last drug intake + 2, death date (whatever occurred first) across all treated subjects divided by 365.25. In case of recurrent events of the same category, the first event was considered.
cDefined as bleeding accompanied by one or more of the following: a decrease in hemoglobin of ≥2 g/dL, a transfusion of 2 or more units of packed red blood cells, bleeding at a critical site or with fatal outcome.
dIntracranial bleed included intracerebral (hemorrhagic stroke), subarachnoid, and subdural bleeds.
eOn-treatment analysis based on the safety population, compared to ITT analysis presented in Section 14 Clinical Studies.
fFatal bleed: Adjudicated major bleed as defined above with investigator reported fatal outcome and adjudicated death with primary cause from bleeding.
gNon-intracranial fatal bleed: Adjudicated major bleed as defined above and adjudicated death with primary cause from bleeding but without symptomatic intracranial bleed based on investigator’s clinical assessment.
EventDabigatran etexilate capsules150 mg
N = 6,059
n (%/yearb)Warfarin
N = 5,998
n (%/yearb)Dabigatran etexilate capsules 150 mg
vs Warfarin
HR (95% CI)Major Bleedingc 350 (3.47) 374 (3.58) 0.97 (0.84, 1.12) Intracranial Hemorrhage (ICH)d 23 (0.22) 82 (0.77) 0.29 (0.18, 0.46) Hemorrhagic Strokee 6 (0.06) 40 (0.37) 0.16 (0.07, 0.37) Other ICH 17 (0.17) 46 (0.43) 0.38 (0.22, 0.67) Gastrointestinal 162 (1.59) 111 (1.05) 1.51 (1.19, 1.92) Fatal Bleedingf 7 (0.07) 16 (0.15) 0.45 (0.19, 1.10) ICH 3 (0.03) 9 (0.08) 0.35 (0.09, 1.28) Non-intracranialg 4 (0.04) 7 (0.07) 0.59 (0.17, 2.02) There was a higher rate of any gastrointestinal bleeds in patients receiving dabigatran etexilate capsules 150 mg than in patients receiving warfarin (6.6% vs 4.2%, respectively).
The risk of major bleeds was similar with dabigatran etexilate capsules 150 mg and warfarin across major subgroups defined by baseline characteristics (see Figure 1), with the exception of age, where there was a trend toward a higher incidence of major bleeding on dabigatran etexilate capsules (hazard ratio 1.2, 95% CI: 1 to 1.5) for patients ≥75 years of age.
Figure 1 Adjudicated Major Bleeding by Baseline Characteristics Including Hemorrhagic Stroke Treated Patients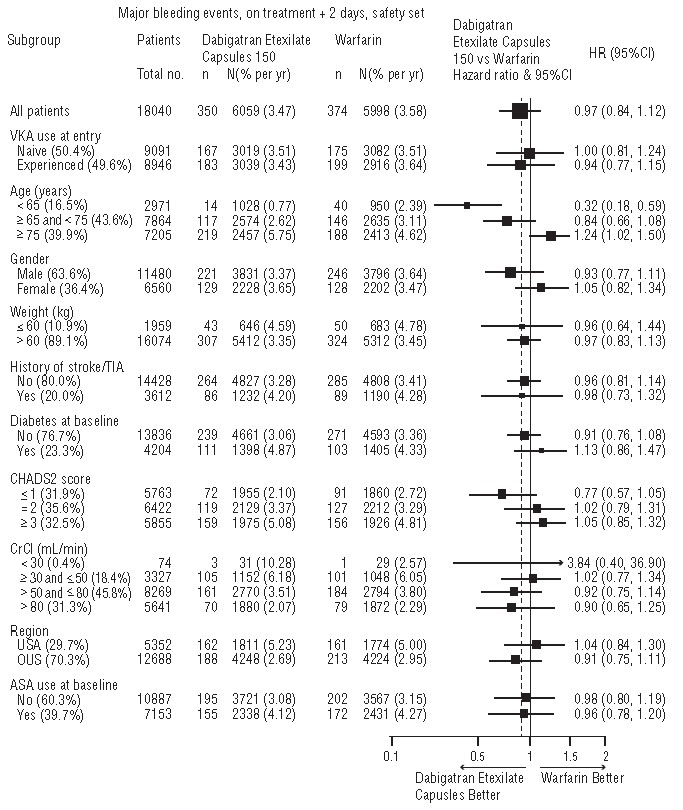
Note: The figure above presents effects in various subgroups all of which are baseline characteristics and all of which were pre-specified. The 95% confidence limits that are shown do not take into account how many comparisons were made, nor do they reflect the effect of a particular factor after adjustment for all other factors. Apparent homogeneity or heterogeneity among groups should not be over-interpreted.
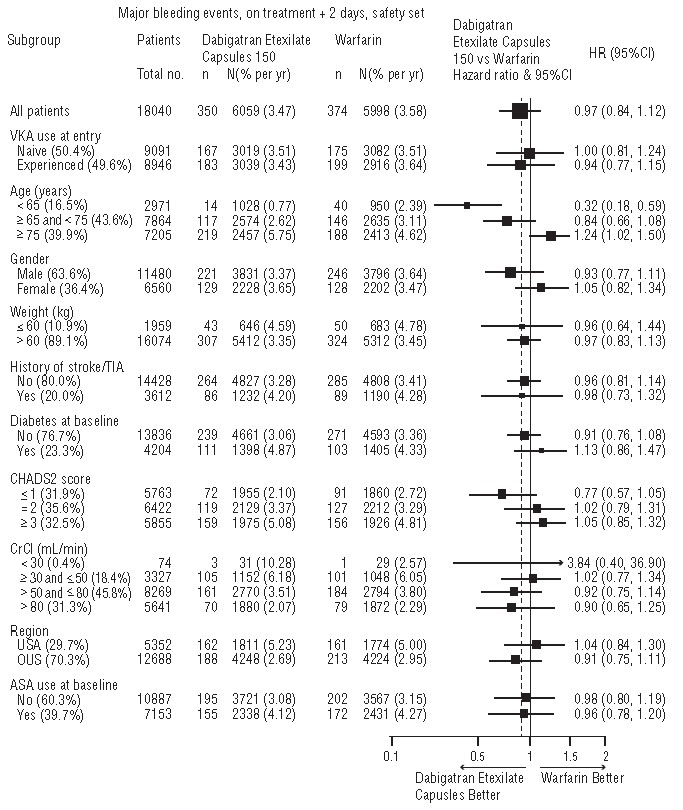
Figure 1 Gastrointestinal Adverse ReactionsPatients on dabigatran etexilate capsules 150 mg had an increased incidence of gastrointestinal adverse reactions (35% vs 24% on warfarin). These were commonly dyspepsia (including abdominal pain upper, abdominal pain, abdominal discomfort, and epigastric discomfort) and gastritis-like symptoms (including GERD, esophagitis, erosive gastritis, gastric hemorrhage, hemorrhagic gastritis, hemorrhagic erosive gastritis, and gastrointestinal ulcer).
Hypersensitivity ReactionsIn the RE-LY study, drug hypersensitivity (including urticaria, rash, and pruritus), allergic edema, anaphylactic reaction, and anaphylactic shock were reported in <0.1% of patients receiving dabigatran etexilate capsules.
Treatment and Reduction in the Risk of Recurrence of Deep Venous Thrombosis and Pulmonary EmbolismDabigatran etexilate capsules were studied in 4,387 patients in 4 pivotal, parallel, randomized, double-blind trials. Three of these trials were active-controlled (warfarin) (RE-COVER, RE-COVER II, and RE-MEDY), and one study (RE-SONATE) was placebo-controlled. The demographic characteristics were similar among the 4 pivotal studies and between the treatment groups within these studies. Approximately 60% of the treated patients were male, with a mean age of 55.1 years. The majority of the patients were white (87.7%), 10.3% were Asian, and 1.9% were black with a mean CrCl of 105.6 mL/min.
Bleeding events for the 4 pivotal studies were classified as major bleeding events if at least one of the following criteria applied: fatal bleeding, symptomatic bleeding in a critical area or organ (intraocular, intracranial, intraspinal or intramuscular with compartment syndrome, retroperitoneal bleeding, intra-articular bleeding, or pericardial bleeding), bleeding causing a fall in hemoglobin level of 2 g/dL (1.24 mmol/L or more, or leading to transfusion of 2 or more units of whole blood or red cells).
RE-COVER and RE-COVER II studies compared dabigatran etexilate capsules 150 mg twice daily and warfarin for the treatment of deep vein thrombosis and pulmonary embolism. Patients received 5 to 10 days of an approved parenteral anticoagulant therapy followed by 6 months, with mean exposure of 164 days, of oral only treatment; warfarin was overlapped with parenteral therapy. Table 4 shows the number of patients experiencing bleeding events in the pooled analysis of RE-COVER and RE-COVER II studies during the full treatment including parenteral and oral only treatment periods after randomization.
Table 4 Bleeding Events in RE-COVER and RE-COVER II Treated PatientsBleeding Events-Full Treatment Period Including Parenteral TreatmentDabigatran etexilate capsules
150 mg twice daily
N (%)Warfarin
N (%)Hazard Ratio
(95% CI)cPatientsN=2,553N=2,554Major bleeding eventa 37 (1.4) 51 (2.0) 0.73 (0.48, 1.11) Fatal bleeding 1 (0.04) 2 (0.1) Bleeding in a critical area or organ 7 (0.3) 15 (0.6) Fall in hemoglobin ≥2 g/dL or transfusion ≥2 units of whole blood or packed red blood cells 32 (1.3) 38 (1.5) Bleeding sites for MBEb Intracranial 2 (0.1) 5 (0.2) Retroperitoneal 2 (0.1) 1 (0.04) Intraarticular 2 (0.1) 4 (0.2) Intramuscular 2 (0.1) 6 (0.2) Gastrointestinal 15 (0.6) 14 (0.5) Urogenital 7 (0.3) 14 (0.5) Other 8 (0.3) 8 (0.3) Clinically relevant non-major bleeding 101 (4.0) 170 (6.7) 0.58 (0.46, 0.75) Any bleeding 411 (16.1) 567 (22.7) 0.70 (0.61, 0.79) Note: MBE can belong to more than one criterion.
aPatients with at least one MBE.
bBleeding site based on investigator assessment. Patients can have more than one site of bleeding.
cConfidence interval
The rate of any gastrointestinal bleeds in patients receiving dabigatran etexilate capsules 150 mg in the full treatment period was 3.1% (2.4% on warfarin).
The RE-MEDY and RE-SONATE studies provided safety information on the use of dabigatran etexilate capsules for the reduction in the risk of recurrence of deep vein thrombosis and pulmonary embolism.
RE-MEDY was an active-controlled study (warfarin) in which 1,430 patients received dabigatran etexilate capsules 150 mg twice daily following 3 to 12 months of oral anticoagulant regimen. Patients in the treatment studies who rolled over into the RE-MEDY study had a combined treatment duration of up to more than 3 years, with mean exposure of 473 days. Table 5 shows the number of patients experiencing bleeding events in the study.
Table 5 Bleeding Events in RE-MEDY Treated PatientsDabigatran etexilate capsules
150 mg twice daily
N (%)Warfarin
N (%)Hazard Ratio
(95% CI)cPatientsN=1,430N=1,426Major bleeding eventa 13 (0.9) 25 (1.8) 0.54 (0.25, 1.16) Fatal bleeding 0 1 (0.1) Bleeding in a critical area or organ 7 (0.5) 11 (0.8) Fall in hemoglobin ≥2 g/dL or transfusion ≥2 units of whole blood or packed red blood cells 7 (0.5) 16 (1.1) Bleeding sites for MBEb Intracranial 2 (0.1) 4 (0.3) Intraocular 4 (0.3) 2 (0.1) Retroperitoneal 0 1 (0.1) Intraarticular 0 2 (0.1) Intramuscular 0 4 (0.3) Gastrointestinal 4 (0.3) 8 (0.6) Urogenital 1 (0.1) 1 (0.1) Other 2 (0.1) 4 (0.3) Clinically relevant non-major bleeding 71 (5.0) 125 (8.8) 0.56 (0.42, 0.75) Any bleeding 278 (19.4) 373 (26.2) 0.71 (0.61, 0.83) Note: MBE can belong to more than one criterion.
aPatients with at least one MBE.
bBleeding site based on investigator assessment. Patients can have more than one site of bleeding.
cConfidence interval
In the RE-MEDY study, the rate of any gastrointestinal bleeds in patients receiving dabigatran etexilate capsules 150 mg was 3.1% (2.2% on warfarin).
RE-SONATE was a placebo-controlled study in which 684 patients received dabigatran etexilate capsules 150 mg twice daily following 6 to 18 months of oral anticoagulant regimen. Patients in the treatment studies who rolled over into the RE-SONATE study had combined treatment duration up to 9 months, with mean exposure of 165 days. Table 6 shows the number of patients experiencing bleeding events in the study.
Table 6 Bleeding Events in RE-SONATE Treated PatientsDabigatran etexilate capsules
150 mg twice daily
N (%)Placebo
N (%)Hazard Ratio
(95% CI)cPatientsN=684N=659Major bleeding eventa 2 (0.3) 0 Bleeding in a critical area or organ 0 0 Gastrointestinalb 2 (0.3) 0 Clinically relevant non-major bleeding 34 (5.0) 13 (2.0) 2.54 (1.34, 4.82) Any bleeding 72 (10.5) 40 (6.1) 1.77 (1.20, 2.61) Note: MBE can belong to more than one criterion.
aPatients with at least one MBE.
bBleeding site based on investigator assessment. Patients can have more than one site of bleeding.
cConfidence interval
In the RE-SONATE study, the rate of any gastrointestinal bleeds in patients receiving dabigatran etexilate capsules 150 mg was 0.7% (0.3% on placebo).
Clinical Myocardial Infarction EventsIn the active-controlled VTE studies, a higher rate of clinical myocardial infarction was reported in patients who received dabigatran etexilate capsules [20 (0.66 per 100 patient-years)] than in those who received warfarin [5 (0.17 per 100 patient-years)]. In the placebo-controlled study, a similar rate of nonfatal and fatal clinical myocardial infarction was reported in patients who received dabigatran etexilate capsules [1 (0.32 per 100 patient-years)] and in those who received placebo [1 (0.34 per 100 patient-years)].
Gastrointestinal Adverse ReactionsIn the four pivotal studies, patients on dabigatran etexilate capsules 150 mg had a similar incidence of gastrointestinal adverse reactions (24.7% vs 22.7% on warfarin). Dyspepsia (including abdominal pain upper, abdominal pain, abdominal discomfort, and epigastric discomfort) occurred in patients on dabigatran etexilate capsules 7.5% vs 5.5% on warfarin, and gastritis-like symptoms (including gastritis, GERD, esophagitis, erosive gastritis and gastric hemorrhage) occurred at 3% vs 1.7%, respectively.
Hypersensitivity ReactionsIn the 4 pivotal studies, drug hypersensitivity (including urticaria, rash, and pruritus), allergic edema, anaphylactic reaction, and anaphylactic shock were reported in 0.1% of patients receiving dabigatran etexilate capsules.Prophylaxis of Deep Vein Thrombosis and Pulmonary Embolism Following Hip Replacement SurgeryDabigatran etexilate capsules was studied in 5,476 patients, randomized and treated in two double-blind, active-controlled non-inferiority trials (RE-NOVATE and RE-NOVATE II). The demographic characteristics were similar across the two studies and between the treatment groups within these studies. Approximately 45.3% of the treated patients were male, with a mean age of 63.2 years. The majority of the patients were white (96.1%), 3.6% were Asian, and 0.3% were black with a mean CrCl of 92 mL/min.
Bleeding events for the RE-NOVATE and RE-NOVATE II studies were classified as major bleeding events if at least one of the following criteria applied: fatal bleeding, symptomatic bleeding in a critical area or organ (intraocular, intracranial, intraspinal or retroperitoneal bleeding), bleeding causing a fall in hemoglobin level of 2 g/dL (1.24 mmol/L) or more, or leading to transfusion of 2 or more units of whole blood or red cells, requiring treatment cessation or leading to re-operation.
The RE-NOVATE study compared dabigatran etexilate capsules 75 mg taken orally 1 to 4 hours after surgery followed by 150 mg once daily, dabigatran etexilate capsules 110 mg taken orally 1 to 4 hours after surgery followed by 220 mg once daily and subcutaneous enoxaparin 40 mg once daily initiated the evening before surgery for the prophylaxis of deep vein thrombosis and pulmonary embolism in patients who had undergone hip replacement surgery. The RE-NOVATE II study compared dabigatran etexilate capsules 110 mg taken orally 1 to 4 hours after surgery followed by 220 mg once daily and subcutaneous enoxaparin 40 mg once daily initiated the evening before surgery for the prophylaxis of deep vein thrombosis and pulmonary embolism in patients who had undergone hip replacement surgery. In the RE-NOVATE and RE-NOVATE II studies, patients received 28 to 35 days of dabigatran etexilate capsules or enoxaparin with median exposure of 33 days. Tables 7 and 8 show the number of patients experiencing bleeding events in the analysis of RE-NOVATE and RE-NOVATE II.
Table 7 Bleeding Events in RE-NOVATE Treated PatientsDabigatran Etexilate Capsules
220 mg
N (%)Enoxaparin
N (%)PatientsN=1,146N=1,154Major bleeding event 23 (2.0) 18 (1.6) Clinically relevant non-major bleeding 48 (4.2) 40 (3.5) Any bleeding 141 (12.3) 132 (11.4) Table 8 Bleeding Events in RE-NOVATE II Treated PatientsDabigatran Etexilate Capsules
220 mg
N (%)Enoxaparin
N (%)PatientsN=1,010N=1,003Major bleeding event 14 (1.4) 9 (0.9) Clinically relevant non-major bleeding 26 (2.6) 20 (2.0) Any bleeding 98 (9.7) 83 (8.3) In the two studies, the rate of major gastrointestinal bleeds in patients receiving dabigatran etexilate capsules and enoxaparin was the same (0.1%) and for any gastrointestinal bleeds was 1.4% for dabigatran etexilate capsules 220 mg and 0.9% for enoxaparin.
Gastrointestinal Adverse ReactionsIn the two studies, the incidence of gastrointestinal adverse reactions for patients on dabigatran etexilate capsules 220 mg and enoxaparin was 39.5% and 39.5%, respectively. Dyspepsia (including abdominal pain upper, abdominal pain, abdominal discomfort, and epigastric discomfort) occurred in patients on dabigatran etexilate capsules 220 mg in 4.1% vs. 3.8% on enoxaparin, and gastritis-like symptoms (including gastritis, GERD, esophagitis, erosive gastritis and gastric hemorrhage) occurred at 0.6% vs 1%, respectively.
Hypersensitivity ReactionsIn the two studies, drug hypersensitivity (such as urticaria, rash, and pruritus) was reported in 0.3% of patients receiving dabigatran etexilate capsules 220 mg.
Clinical Myocardial Infarction EventsIn the two studies, clinical myocardial infarction was reported in 2 (0.1%) of patients who received dabigatran etexilate capsules 220 mg and 6 (0.3%) of patients who received enoxaparin.
Pediatric use information is approved for Boehringer Ingelheim Pharmaceuticals, Inc.’s Pradaxa (dabigatran etexilate) capsules. However, due to Boehringer Ingelheim Pharmaceuticals, Inc.’s marketing exclusivity rights, this drug product is not labeled with that information. - Mechanical prosthetic heart valve [see Warnings and Precautions]
5.4 Thromboembolic and Bleeding Events in Patients with Prosthetic Heart ValvesThe safety and efficacy of dabigatran etexilate capsules in adult patients with bileaflet mechanical prosthetic heart valves was evaluated in the RE-ALIGN trial, in which patients with bileaflet mechanical prosthetic heart valves (recently implanted or implanted more than three months prior to enrollment) were randomized to dose-adjusted warfarin or 150 mg, 220 mg, or 300 mg of dabigatran etexilate capsules twice a day. RE-ALIGN was terminated early due to the occurrence of significantly more thromboembolic events (valve thrombosis, stroke, transient ischemic attack, and myocardial infarction) and an excess of major bleeding (predominantly post-operative pericardial effusions requiring intervention for hemodynamic compromise) in the dabigatran etexilate capsules treatment arm as compared to the warfarin treatment arm. These bleeding and thromboembolic events were seen both in patients who were initiated on dabigatran etexilate capsules postoperatively within three days of mechanical bileaflet valve implantation, as well as in patients whose valves had been implanted more than three months prior to enrollment. Therefore, the use of dabigatran etexilate capsules is contraindicated in all patients with mechanical prosthetic valves
[see Contraindications (4)].The use of dabigatran etexilate capsules for the prophylaxis of thromboembolic events in patients with atrial fibrillation in the setting of other forms of valvular heart disease, including the presence of a bioprosthetic heart valve, has not been studied and is not recommended.