Dapsone
Dapsone Prescribing Information
Dermatitis herpetiformis: (D.H.)
Leprosy: All forms of leprosy except for cases of proven Dapsone resistance.
The dosage should be individually titrated starting in adults with 50 mg daily and correspondingly smaller doses in children. If full control is not achieved within the range of 50 - 300 mg daily, higher doses may be tried. Dosage should be reduced to a minimum maintenance level as soon as possible. In responsive patients there is a prompt reduction in pruritus followed by clearance of skin lesions. There is no effect on the gastrointestinal component of the disease.
Dapsone levels are influenced by acetylation rates. Patients with high acetylation rates, or who are receiving treatment affecting acetylation may require an adjustment in dosage.
A strict gluten free diet is an option for the patient to elect, permitting many to reduce or eliminate the need for Dapsone; the average time for dosage reduction is 8 months with a range of 4 months to 2 1/2 years and for dosage elimination 29 months with a range of 6 months to 9 years.
In order to reduce secondary Dapsone resistance, the WHO Expert Committee on Leprosy and the USPHS at Carville, LA, recommended that Dapsone should be commenced in combination with one or more anti-leprosy drugs. In the multidrug program Dapsone should be maintained at the full dosage of 100 mg daily without interruption (with corresponding smaller doses for children) and provided to all patients who have sensitive organisms with new or recrudescent disease or who have not yet completed a two year course of Dapsone monotherapy. For advice and other drugs, the USPHS at Carville, LA (1- 800-642-2477) should be contacted. Before using other drugs consult appropriate product labeling.
In bacteriologically negative tuberculoid and indeterminate disease, the recommendation is the coadministration of Dapsone 100 mg daily with six months of Rifampin 600 mg daily. Under WHO, daily Rifampin may be replaced by 600 mg Rifampin monthly, if supervised. The Dapsone is continued until all signs of clinical activity are controlled usually after an additional six months. Then Dapsone should be continued for an additional three years for tuberculoid and indeterminate patients and for five years for borderline tuberculoid patients.
In lepromatous and borderline lepromatous patients, the recommendation is the co-administration of Dapsone 100 mg daily with two years of Rifampin 600 mg daily. Under WHO daily Rifampin may be replaced by 600 mg Rifampin monthly, if supervised. One may elect the concurrent administration of a third anti-leprosy drug, usually either Clofazamine 50-100 mg daily or Ethionamide 250-500 mg daily. Dapsone 100 mg daily is continued 3-10 years until all signs of clinical activity are controlled with skin scrapings and biopsies negative for one year. Dapsone should then be continued for an additional 10 years for borderline patients and for life for lepromatous patients.
Secondary Dapsone resistance should be suspected whenever a lepromatous or borderline lepromatous patient receiving Dapsone treatment relapses clinically and bacteriologically, solid staining bacilli being found in the smears taken from the new active lesions. If such cases show no response to regular and supervised Dapsone therapy within three to six months or good compliance for the past 3-6 months can be assured, Dapsone resistance should be considered confirmed clinically. Determination of drug sensitivity using the mouse footpad method is recommended and, after prior arrangement, is available without charge from the USPHS, Carville, LA. Patients with proven Dapsone resistance should be treated with other drugs.
Hypersensitivity to Dapsone and/or its derivatives.
In addition to the warnings listed above, the following syndromes and serious reactions have been reported in patients on Dapsone.
Dose-related hemolysis is the most common adverse effect and is seen in patients with or without G6PD deficiency. Almost all patients demonstrate the inter-related changes of a loss of 1-2g of hemoglobin, an increase in the reticulocytes (2-12%), a shortened red cell life span and a rise in methemoglobin. G6PD deficient patients have greater responses.
Peripheral neuropathy is a definite but unusual complication of Dapsone therapy in non-leprosy patients. Motor loss is predominant. If muscle weakness appears, Dapsone should be withdrawn. Recovery on withdrawal is usually substantially complete. The mechanism of recovery is reported by axonal regeneration. Some recovered patients have tolerated retreatment at reduced dosage. In leprosy this complication may be difficult to distinguish from a leprosy reactional state.
Falsely reduced HbA1c measurements have been reported with dapsone use. Alternate measures of glycemic control (e.g., fructosamine and/or more frequent blood glucose monitoring) are recommended when a discordance between HbA1c and blood glucose concentrations are observed or suspected. Falsely reduced HbA1c may occur without overt evidence of hemolysis or anemia.
In addition to the warnings and adverse effects reported above, additional adverse reactions include: nausea, vomiting, abdominal pains, pancreatitis, vertigo, blurred vision, tinnitus, insomnia, fever, headache, psychosis, phototoxicity, pulmonary eosinophilia, tachycardia, albuminuria, the nephrotic syndrome, hypoalbuminemia without proteinuria, renal papillary necrosis, male infertility, drug-induced Lupus erythematosus and an infectious mononucleosis-like syndrome. In general, with the exception of the complications of severe anoxia from overdosage (retinal and optic nerve damage, etc.) these adverse reactions have regressed off drug.
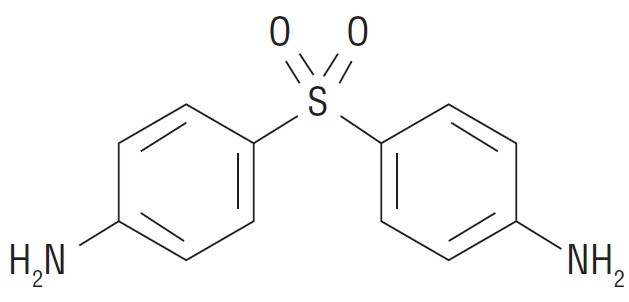
Dapsone-USP, 4,4’-sulfonyl dianiline, is a primary treatment for Dermatitis herpetiformis. It is an antibacterial drug for susceptible cases of leprosy. It is a white to creamy white crystalline powder, very slightly soluble in water, sparingly soluble in alcohol, soluble in acetone and dilute mineral acids.
Dapsone is issued on prescription in tablets of 25 mg and 100 mg for oral use.