Dasatinib
Dasatinib Prescribing Information
Dasatinib tablets are indicated for the treatment of adult patients with
• newly diagnosed Philadelphia chromosome-positive (Ph+) chronic myeloid leukemia (CML) in chronic phase.
• chronic, accelerated, or myeloid or lymphoid blast phase Ph+ CML with resistance or intolerance to prior therapy including imatinib.
• Philadelphia chromosome-positive acute lymphoblastic leukemia (Ph+ ALL) with resistance or intolerance to prior therapy.
Dasatinib tablets are indicated for the treatment of pediatric patients 1 year of age and older with
- Ph+ CML in chronic phase.
- newly diagnosed Ph+ ALL in combination with chemotherapy.
Dasatinib Tablets are available as 20 mg, 50 mg, 70 mg, 80 mg, 100 mg and 140 mg, white to off-white, biconvex, film-coated tablets.
None.
The following clinically significant adverse reactions are discussed in greater detail in other sections of the labeling:
- Myelosuppression[see Dosage and Administration (.) and Warnings and Precautions (
2.5 Dose Adjustment for Adverse ReactionsMyelosuppressionIn clinical studies, myelosuppression was managed by dose interruption, dose reduction, or discontinuation of study therapy. Hematopoietic growth factor has been used in patients with resistant myelosuppression. Guidelines for dose modifications for adult and pediatric patients are summarized in Tables 3 and 4, respectively.
Table 3: Dose Adjustments for Neutropenia and Thrombocytopenia in AdultsChronic Phase CML
(starting dose 100 mg once daily)ANC*< 0.5 X 109/L
or
Platelets < 50 x 109/L1. Stop dasatinib tablets until ANC ≥1.0 × 109/L and platelets ≥50 × 109/L.
2. Resume treatment with dasatinib tablets at the original starting dose if recovery occurs in ≤7 days.
3. If platelets <25 × 109/L or recurrence of ANC <0.5 × 109/L for >7 days, repeat Step 1 and resume dasatinib tablets at a reduced dose of 80 mg once daily for second episode. For third episode, further reduce dose to 50 mg once daily (for newly diagnosed patients) or discontinue dasatinib tablets (for patients resistant or intolerant to prior therapy including imatinib).Accelerated Phase CML, Blast Phase CML and Ph+ ALL (starting dose 140 mg once daily) ANC*< 0.5 X 109/L
or
Platelets <10 × 109/L1. Check if cytopenia is related to leukemia (marrow aspirate or biopsy).
2. If cytopenia is unrelated to leukemia, stop dasatinib tablets until ANC ≥1.0 × 109/L and platelets ≥20 × 109/L and resume at the original starting dose.
3. If recurrence of cytopenia, repeat Step 1 and resume dasatinib tablets at a reduced dose of 100 mg once daily (second episode) or 80 mg once daily (third episode).
4. If cytopenia is related to leukemia, consider dose escalation to 180 mg once daily.*ANC: absolute neutrophil count
Table4: Dose Adjustments for Neutropenia and Thrombocytopenia in Pediatric Patients with Ph+ CMLDose (maximum dose per day)1. If cytopenia persists for more than 3 weeks, check if cytopenia is related to leukemia (marrow aspirate or biopsy).
2. If cytopenia is unrelated to leukemia, stop dasatinib tablets until ANC* ≥1.0 × 109/L and platelets ≥75 × 109/L and resume at the original starting dose or at a reduced dose.
3. If cytopenia recurs, repeat marrow aspirate/biopsy and resume dasatinib tablets at a reduced dose.Original Starting DoseOne-Level Dose ReductionTwo-Level Dose ReductionTablets40 mg 20 mg ** 60 mg 40 mg 20 mg 70 mg 60 mg 50 mg 100 mg 80 mg 70 mg *ANC: absolute neutrophil count
** lower tablet dose not available
For pediatric patients with chronic phase CML, if Grade ≥ 3 neutropenia or thrombocytopenia recurs during complete hematologic response (CHR), interrupt dasatinib tablets and resume at a reduced dose. Implement temporary dose reductions for intermediate degrees of cytopenia and disease response as needed.
For pediatric patients with Ph+ ALL, if neutropenia and/or thrombocytopenia result in a delay of the next block of treatment by more than 14 days, interrupt dasatinib tablets and resume at the same dose level once the next block of treatment is started. If neutropenia and/or thrombocytopenia persist and the next block of treatment is delayed another 7 days, perform a bone marrow assessment to assess cellularity and percentage of blasts. If marrow cellularity is <10%, interrupt treatment with dasatinib tablets until ANC >500/microL (0.5 x 109/L), at which time treatment may be resumed at full dose. If marrow cellularity is >10%, resumption of treatment with dasatinib tablets may be considered.
Non-Hematologic Adverse ReactionsFor adults with Ph+ CML and ALL, and pediatric patients with Ph+ CML, if a severe non-hematologic adverse reaction develops with dasatinib use, treatment must be withheld until the adverse reaction has resolved or improved. Thereafter, treatment can be resumed as appropriate at a reduced dose depending on the severity and recurrence
[see Warnings and Precautions ].For pediatric patients with Ph+ ALL, interrupt treatment for cases of grade ≥3 non-hematologic adverse reactions with the exception of liver function test abnormalities, and resume at a reduced dose when resolved to grade ≤1. For elevated direct bilirubin over 5 times the institutional upper limit of normal (ULN), interrupt treatment until improvement to baseline or grade ≤1. For elevated AST/ALT over 15 times the institutional ULN, interrupt treatment until improvement to baseline or grade <1. For recurrent liver function test abnormalities as above, reduce the dose if this adverse reaction recurs after reinitiation of dasatinib tablets. Dose reduction recommendations are described in Table 5.
Table 5: Dose Adjustments for Non-Hematologic Toxicities in Pediatric PatientsDose (maximum dose per day) 1.If a non-hematologic toxicity grade 2 occurs, consider interrupting dasatinib tablets if no recovery despite symptomatic therapy; once recovered to grade ≤1, resume at the original starting dose. Resume dasatinib tablets at a reduced dose for recurrent events. TabletsOriginal Starting DoseOne-LevelDose ReductionTwo-LevelDose Reduction2. If a non-hematologic toxicity grade 3 occurs, stop dasatinib tablets until recovery to grade ≤1 and then resume at a reduced dose. 40 mg
60 mg
70 mg
100 mg20 mg
40 mg
60 mg
80 mg**
20 mg
50 mg
70 mg3. If direct bilirubin is >5 ULN or AST/ALT >15 ULN, interrupt dasatinib tablets until recovery to grade ≤1 and then resume dasatinib tablets at the original starting dose. Resume dasatinib tablets at a reduced dose for recurrent hepatotoxicity. ** lower tablet dose not available
)]5.1 MyelosuppressionTreatment with dasatinib is associated with severe (NCI CTCAE Grade 3 or 4) thrombocytopenia, neutropenia, and anemia, which occur earlier and more frequently in patients with advanced phase CML or Ph+ ALL than in patients with chronic phase CML
[see Adverse Reactions ].In patients with chronic phase CML, perform complete blood counts (CBCs) every 2 weeks for 12 weeks, then every 3 months thereafter, or as clinically indicated. In patients with advanced phase CML or Ph+ ALL, perform CBCs weekly for the first 2 months and then monthly thereafter, or as clinically indicated.
In pediatric patients with Ph+ ALL treated with dasatinib tablets in combination with chemotherapy, perform CBCs prior to the start of each block of chemotherapy and as clinically indicated. During the consolidation blocks of chemotherapy, perform CBCs every 2 days until recovery.
Myelosuppression is generally reversible and usually managed by withholding dasatinib temporarily and/or dose reduction
[see Dosage and Administration ]. Most bleeding events in clinical studies were associated with severe thrombocytopenia. In addition to causing thrombocytopenia in human subjects, dasatinib caused platelet dysfunction in vitro.Concomitant medications that inhibit platelet function or anticoagulants may increase the risk of hemorrhage.
- Fluid retention [see Warnings and Precautions (.)]
5.3 Fluid RetentionDasatinib may cause fluid retention[see Adverse Reactions ].After 5 years of follow-up in the adult randomized newly diagnosed chronic phase CML study (n=258), Grade 3 or 4 fluid retention was reported in 5% of patients, including 3% of patients with Grade 3 or 4 pleural effusion. In adult patients with newly diagnosed or imatinib-resistant or -intolerant chronic phase CML, Grade 3 or 4 fluid retention occurred in 6% of patients treated with dasatinib at the recommended dose (n=548). In adult patients with advanced phase CML or Ph+ ALL treated with dasatinib at the recommended dose (n=304), Grade 3 or 4 fluid retention was reported in 8% of patients, including Grade 3 or 4 pleural effusion reported in 7% of patients. In pediatric patients with chronic phase CML, cases of Grade 1 or 2 fluid retention were reported in 10.3% of patients.Evaluate
patients whodevelop symptoms of pleural effusion or other fluid retention, such as new or worsened dyspnea on exertion or at rest, pleuritic chest pain, or dry cough, promptly with a chest x-ray or additional diagnostic imaging as appropriate. Fluid retention events were typically managed by supportive care measures that may include diuretics or short courses of steroids. Severe pleural effusion may require thoracentesis and oxygen therapy. Consider dose reduction or treatment interruption[see Dosage and Administration ]. After 5 years of follow-up in the randomized newly diagnosed chronic phase CML trial in adults (n=258), the following cardiac adverse reactions occurred: cardiac ischemic events (3.9% dasatinib vs 1.6% imatinib), cardiac-related fluid retention (8.5% dasatinib vs 3.9% imatinib), and conduction system abnormalities, most commonly arrhythmia and palpitations (7% dasatinib vs 5% imatinib). Two cases (0.8%) of peripheral arterial occlusive disease occurred with imatinib and 2 (0.8%) transient ischemic attacks occurred with dasatinib. Monitor patients for signs or symptoms consistent with cardiac dysfunction and treat appropriately. - Pulmonary arterial hypertension [see Warnings and Precautions (.)]
5.5 Pulmonary Arterial HypertensionDasatinib may increase the risk of developing pulmonary arterial hypertension (PAH) in adult and pediatric patients which may occur any time after initiation, including after more than 1 year of treatment. Manifestations include dyspnea, fatigue, hypoxia, and fluid retention
[see Adverse Reactions].PAH may be reversible on discontinuation of dasatinib. Evaluate patients for signs and symptoms of underlying cardiopulmonary disease prior to initiating dasatinib and during treatment. If PAH is confirmed, dasatinib should be permanently discontinued. - QT prolongation [see Warnings and Precautions ()].
5.6 QT ProlongationDasatinib may increase the risk of prolongation of QTc in patients including those with hypokalemia or hypomagnesemia, patients with congenital long QT syndrome, patients taking antiarrhythmic medicines or other medicinal products that lead to QT prolongation, and cumulative high-dose anthracycline therapy[see Adverse Reactions (6.1)]. Correct hypokalemia or hypomagnesemia prior to and during dasatinib administration. - Severe dermatologic reactions [see Warnings and Precautions (.)]
5.7 Severe Dermatologic ReactionsCases of severe mucocutaneous dermatologic reactions, including Stevens-Johnson syndrome[see Adverse Reactions ]and erythema multiforme, have been reported in patients treated with dasatinib. Discontinue permanently in patients who experience a severe mucocutaneous reaction during treatment if no other etiology can be identified. - Tumor lysis syndrome [see Warnings and Precautions ()].
5.8 Tumor Lysis SyndromeTumor lysis syndrome has been reported in patients with resistance to prior imatinib therapy, primarily in advanced phase disease. Due to potential for tumor lysis syndrome, maintain adequate hydration, correct uric acid levels prior to initiating therapy with dasatinib, and monitor electrolyte levels. Patients with advanced stage disease and/or high tumor burden may be at increased risk and should be monitored more frequently
[see Adverse Reactions ]. - Effects on growth and development in pediatric patients [see Warnings and Precautions (.)]
5.10 Effects on Growth and Development in Pediatric PatientsIn pediatric trials of dasatinib in chronic phase CML after at least 2 years of treatment, adverse reactions associated with bone growth and development were reported in 5 (5.2%) patients, one of which was severe in intensity (Growth Retardation Grade 3). These 5 cases included cases of epiphyses delayed fusion, osteopenia, growth retardation, and gynecomastia
[see Adverse ReactionsandUse in Specific Populations]. Of these 5 cases, 1 case of osteopenia and 1 case of gynecomastia resolved during treatment.Monitor bone growth and development in pediatric patients.
- Hepatotoxicity [see Warnings and Precautions (.)]
5.11 HepatotoxicityDasatinib tablets may cause hepatotoxicity as measured by elevations in bilirubin, aspartate aminotransferase (AST), alanine aminotransferase (ALT), and alkaline phosphatase
[see Adverse Reactions ]. Monitor transaminases at baseline and monthly or as clinically indicated during treatment. Reduce dose, withhold, or permanently discontinue dasatinib tablets based on severity[see Dosage and Administration ]. When dasatinib tablets are administered in combination with chemotherapy, liver toxicity in the form of transaminase elevation and hyperbilirubinemia has been observed. Monitor hepatic function when dasatinib tablets are used in combination with chemotherapy.
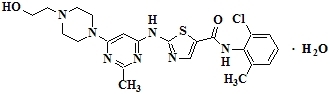
Dasatinib is a kinase inhibitor. The chemical name for dasatinib is N-(2-chloro-6-methylphenyl)-2-[[6-[4-(2-hydroxyethyl)-1-piperazinyl]-2-methyl-4-pyrimidinyl]amino]-5-thiazolecarboxamide, monohydrate. The molecular formula is C22H26ClN7O2S•H2O, which corresponds to a formula weight of 506.02 (monohydrate). The anhydrous free base has a molecular weight of 488.01. Dasatinib has the following chemical structure:
Dasatinib is a white to off-white powder. The drug substance is insoluble in water and slightly soluble in ethanol, methanol, polyethylene glycol 400 and propylene glycol; very slightly soluble in acetone and acetonitrile; and practically insoluble in corn oil.
Dasatinib tablets are white to off-white, biconvex, film-coated tablets containing dasatinib, with the following inactive ingredients: colloidal silicon dioxide, croscarmellose sodium, lactose monohydrate, magnesium stearate and microcrystalline cellulose. The tablet coating consists of hydroxypropyl cellulose, hypromellose, titanium dioxide and triethyl citrate. Dasatinib tablets are supplied for oral administration.
Dasatinib, at nanomolar concentrations, inhibits the following kinases: BCR-ABL, SRC family (SRC, LCK, YES, FYN), c-KIT, EPHA2, and PDGFRβ. Based on modeling studies, dasatinib is predicted to bind to multiple conformations of the ABL kinase.