Dexamethasone Sodium Phosphate
Dexamethasone Sodium Phosphate Prescribing Information
When oral therapy is not feasible and the strength, dosage form, and route of administration of the drug reasonably lend the preparation to the treatment of the condition, those products labeled for intravenous or intramuscular use are indicated as follows:
1.
Primary or secondary adrenocortical insufficiency (hydrocortisone or cortisone is the drug of choice; synthetic analogs may be used in conjunction with mineralocorticoids where applicable; in infancy, mineralocorticoid supplementation is of particular importance).
Acute adrenocortical insufficiency (hydrocortisone or cortisone is the drug of choice; mineralocorticoid supplementation may be necessary, particularly when synthetic analogs are used).
Preoperatively, and in the event of serious trauma or illness, in patients with known adrenal insufficiency or when adrenocortical reserve is doubtful.
Shock unresponsive to conventional therapy if adrenocortical insufficiency exists or is suspected.
Congenital adrenal hyperplasia
Nonsuppurative thyroiditis
Hypercalcemia associated with cancer
2.
As adjunctive therapy for short-term administration (to tide the patient over an acute episode or exacerbation) in:
Post-traumatic osteoarthritis
Synovitis of osteoarthritis
Rheumatoid arthritis, including juvenile rheumatoid arthritis (selected cases may require low-dose maintenance therapy).
Acute and subacute bursitis
Epicondylitis
Acute nonspecific tenosynovitis
Acute gouty arthritis
Psoriatic arthritis
Ankylosing spondylitis
3.
During an exacerbation or as maintenance therapy in selected cases of:
Systemic lupus erythematosus
Acute rheumatic carditis
4
Pemphigus
Severe erythema multiforme (Stevens-Johnson syndrome)
Exfoliative dermatitis
Bullous dermatitis herpetiformis
Severe seborrheic dermatitis
Severe psoriasis
Mycosis fungoides
5.
Control of severe or incapacitating allergic conditions intractable to adequate trials of conventional treatment in:
Bronchial asthma
Contact dermatitis
Atopic dermatitis
Serum sickness
Seasonal or perennial allergic rhinitis
Drug hypersensitivity reactions
Urticarial transfusion reactions
Acute noninfectious laryngeal edema (epinephrine is the drug of first choice).
6.
Severe acute and chronic allergic and inflammatory processes involving the eye, such as:
Herpes zoster ophthalmicus
Iritis, iridocyclitis
Chorioretinitis
Diffuse posterior uveitis and choroiditis
Optic neuritis
Sympathetic ophthalmia
Anterior segment inflammation
Allergic conjunctivitis
Allergic corneal marginal ulcers
Keratitis
7
To tide the patient over a critical period of the disease in:
Ulcerative colitis (systemic therapy)
Regional enteritis (systemic therapy)
8.
Symptomatic sarcoidosis
Berylliosis
Fulminating or disseminated pulmonary tuberculosis when used concurrently with appropriate anti-tuberculous chemotherapy.
Loeffler's syndrome not manageable by other means.
Aspiration pneumonitis
9
Acquired (autoimmune) hemolytic anemia.
Idiopathic thrombocytopenic purpura in adults (IV only; IM administration is contraindicated).
Secondary thrombocytopenia in adults
Erythroblastopenia (RBC anemia)
Congenital (erythroid) hypoplastic anemia
10.
For palliative management of:
Leukemias and lymphomas in adults
Acute leukemia of childhood
11
To induce diuresis or remission of proteinuria in the nephrotic syndrome, without uremia, of the idiopathic type or that due to lupus erythematosus.
12.
Acute exacerbations of multiple sclerosis
13
Tuberculous meningitis with subarachnoid block or impending block when used concurrently with appropriate anti-tuberculosis chemotherapy.
Trichinosis with neurologic or myocardial involvement.
Diagnostic testing of adrenocortical hyperfunction.
Cerebral edema of diverse etiologies in conjunction with adequate neurological evaluation and management.
When the strength and dosage form of the drug lend the preparation to the treatment of the condition, those products labeled for intra-articular or soft tissue administration are indicated as adjunctive therapy for short-term administration (to tide the patient over an acute episode or exacerbation) in:
Synovitis of osteoarthritis.
Rheumatoid arthritis.
Acute and subacute bursitis.
Acute gouty arthritis.
Epicondylitis.
Acute nonspecific tenosynovitis.
Post-traumatic osteoarthritis.
When the strength and dosage form of the drug lend the preparation to the treatment of the condition, those products labeled for intralesional administration are indicated for:
Keloids.
Localized hypertrophic, infiltrated, inflammatory lesions of: lichen planus, psoriatic plaques,
granuloma annulare, and lichen simplex chronicus (neurodermatitis).
Discoid lupus erythematosus.
Necrobiosis lipoidica diabeticorum.
Alopecia areata.
They also may be useful in cystic tumors of an aponeurosis tendon (ganglia).
The initial dosage of dexamethasone sodium phosphate injection may vary from 0.50 mg/day to 9.0 mg/day depending on the specific disease entity being treated. In situations of less severity, lower doses will generally suffice, while in selected patients higher initial doses may be required. Usually the parenteral dosage ranges are one-third to one-half the oral dose given every 12 hours. However, in certain overwhelming, acute, life-threatening situations, administration of dosages exceeding the usual dosages may be justified and may be in multiples of the oral dosages.
For the treatment of unresponsive shock high pharmacologic doses of this product are currently
recommended. Reported regimens range from 1 to 6 mg/kg of body weight as a single intravenous injection to 40 mg initially followed by repeat intravenous injection every 2 to 6 hours while shock persists.
For the treatment of cerebral edema in adults an initial intravenous dose of 10 mg is recommended followed by 4 mg intramuscularly every six hours until maximum response has been noted. This regimen may be continued for several days postoperatively in patients requiring brain surgery. Oral dexamethasone, 1 to 3 mg t.i.d., should be given as soon as possible and dosage tapered off over a period of five to seven days. Nonoperative cases may require continuous therapy to remain free of symptoms of increased intracranial pressure. The smallest effective dose should be used in children, preferably orally. This may approximate 0.2 mg/kg/24 hours in divided doses.
In treatment of acute exacerbations of multiple sclerosis daily doses of 200 mg of prednisolone for a week followed by 80 mg every other day or 4–8 mg dexamethasone every other day for 1 month have been shown to be effective.
The initial dosage should be maintained or adjusted until a satisfactory response is noted. If after a reasonable period of time there is a lack of satisfactory clinical response, dexamethasone sodium phosphate injection should be discontinued and the patient transferred to other appropriate therapy. It should be emphasized that dosage requirements are variable and must be individualized on the basis of the disease under treatment and the response of the patient.
After a favorable response is noted, the proper maintenance dosage should be determined by decreasing the initial drug dosage in small decrements at appropriate time intervals until the lowest dosage which will maintain an adequate clinical response is reached. It should be kept in mind that constant monitoring is needed in regard to drug dosage. Included in the situations which may make dosage adjustments necessary are changes in clinical status secondary to remissions or exacerbations in the disease process, the patient's individual drug responsiveness and the effect of patient exposure to stressful situations not directly related to the disease entity under treatment. In this later situation it may be necessary to increase the dosage of dexamethasone sodium phosphate injection for a period of time consistent with the patient's condition. If after a long-term therapy the drug is to be stopped, it is recommended that it be withdrawn gradually rather than abruptly.
The dose for intrasynovial administration is usually 2 to 4 mg for large joints and 0.8 to 1 mg for small joints. For soft tissue and bursal injections a dose of 2 to 4 mg is recommended. Ganglia require a dose of 1 to 2 mg. A dose of 0.4 to 1 mg is used for injection into tendon sheaths. Injection into intervertebral joints should not be attempted at any time and hip joint injection cannot be recommended as an office procedure.
Intrasynovial and soft tissue injections should be employed only when affected areas are limited to 1 or 2 sites. It should be remembered that corticoids provide palliation only and that other conventional or curative methods of therapy should be employed when indicated.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever the solution and container permit.
Frequency of injection usually ranges from once every 3 to 5 days to once every 2 to 3 weeks. Frequent intra-articular injection may cause damage to joint tissue.
Systemic fungal infections.
Fluid and electrolyte disturbances:
Sodium retention
Fluid retention
Congestive heart failure in susceptible patients
Potassium loss
Hypokalemic alkalosis
Hypertension
Musculoskeletal:
Muscle weakness
Steroid myopathy
Loss of muscle mass
Osteoporosis
Vertebral compression fractures
Aseptic necrosis of femoral and humeral heads
Pathologic fracture of long bones
Gastrointestinal:
Peptic ulcer with possible subsequent perforation and hemorrhage
Pancreatitis
Abdominal distention
Ulcerative esophagitis
Dermatological:
Impaired wound healing
Thin fragile skin
Facial erythema
Increased sweating
May suppress reactions to skin tests
Petechiae and ecchymoses
Neurological:
Convulsions
Increased intracranial pressure with papilledema (pseudotumor cerebri) usually after treatment
Vertigo
Headache
Ophthalmic:
Posterior subcapsular cataracts
Increased intraocular pressure
Glaucoma
Endocrine:
Menstrual irregularities
Development of cushingoid state
Suppression of growth in children
Secondary adrenocortical and pituitary unresponsiveness, particularly in times of stress, as in trauma, surgery, or illness
Decreased carbohydrate tolerance
Manifestations of latent diabetes mellitus
Increased requirements for insulin or oral hypoglycemic agents in diabetics
Metabolic:
Negative nitrogen balance due to protein catabolism
Miscellaneous:
Hyperpigmentation or hypopigmentation
Subcutaneous and cutaneous atrophy
Sterile abscess
Post-injection flare, following intra-articular use
Charcot-like arthropathy
Itching, burning, tingling in the ano-genital region
Dexamethasone Sodium Phosphate Injection, USP, is a water-soluble inorganic ester of dexamethasone which produces a rapid response even when injected intramuscularly.
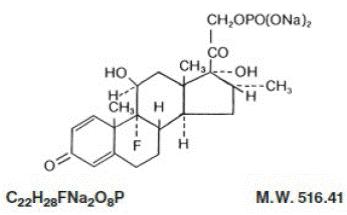
Dexamethasone Sodium Phosphate, USP chemically is Pregna-1,4-diene-3,20-dione, 9-fluoro- 11,17-dihydroxy-16-methyl-21-(phosphonooxy)-, disodium salt, (11ß, 16α).
It occurs as a white to practically white powder, is hygroscopic, is soluble in water and its solutions have a pH between 7.5 and 9.5. It has the following structural formula:
Each mL of Dexamethasone Sodium Phosphate Injection, USP
Dexamethasone Sodium Phosphate Injection, USP
70069-
The vial stopper closure is not made with natural rubber latex.
Store at 20° to 25°C (68° to 77°F) [see USP Controlled Room Temperature]. Sensitive to heat.
Do not autoclave.
Protect from freezing.