Emsam Prescribing Information
In pooled analyses of placebo-controlled trials of antidepressant drugs (SSRIs and other antidepressant classes) that included approximately 77,000 adult patients and over 4,400 pediatric patients, the incidence of suicidal thoughts and behaviors in pediatric and young adult patients was greater in antidepressant-treated patients than in placebo-treated patients. The drug-placebo differences in the number of cases of suicidal thoughts and behaviors per 1000 patients treated are provided in Table 1.
No suicides occurred in any of the pediatric studies. There were suicides in the adult studies, but the number was not sufficient to reach any conclusion about antidepressant drug effect on suicide.
Age Range (years) | Drug-Placebo Difference in Number of Patients of Suicidal Thoughts or Behaviors per 1000 Patients Treated |
Increases Compared to Placebo | |
<18 | 14 additional patients |
18-24 | 5 additional patients |
Decreases Compared to Placebo | |
25-64 | 1 fewer patient |
≥65 | 6 fewer patients |
It is unknown whether the risk of suicidal thoughts and behaviors in pediatric and young adult patients extends to longer-term use, i.e., beyond four months. However, there is substantial evidence from placebo-controlled maintenance trials in adults with MDD that antidepressants delay the recurrence of depression.
Monitor all antidepressant-treated patients for clinical worsening and emergence of suicidal thoughts and behaviors, especially during the initial few months of drug therapy and at times of dosage changes. Counsel family members or caregivers of patients to monitor for changes in behavior and to alert the healthcare provider. Consider changing the therapeutic regimen, including possibly discontinuing EMSAM, in patients whose depression is persistently worse, or who are experiencing emergent suicidal thoughts or behaviors.
• EMSAM (selegiline transdermal system) is contraindicated with selective serotonin reuptake inhibitors (SSRIs, e.g., fluoxetine, sertraline, and paroxetine); serotonin and norepinephrine reuptake inhibitors (SNRIs, e.g., venlafaxine and duloxetine); the tricyclic antidepressants clomipramine and imipramine, the opiate analgesics meperidine, tramadol, methadone, pentazocine, and propoxyphene; and the antitussive agent dextromethorphan because of a risk of serotonin syndrome when EMSAM is used with these agents[see Warnings and Precautions (5.2)and Drug Interactions (7.1)].• Carbamazepine is contraindicated with EMSAM because of a possible increased risk of hypertensive crisis[see Warnings and Precautions (5.3)and Clinical Pharmacology (12.3)].• After stopping treatment with drugs contraindicated with EMSAM, a time period equal to 4 to 5 half-lives (approximately one week) of the drug or any active metabolite should elapse before starting therapy with EMSAM. Because of the long half-life of fluoxetine and its active metabolite, at least 5 weeks should elapse between discontinuation of fluoxetine and initiation of treatment with EMSAM.• At least 2 weeks should elapse after stopping EMSAM before starting therapy with any drug that is contraindicated with EMSAM.• EMSAM is contraindicated in patients less than 12 years of age because of the potential for a hypertensive crisis[see Use in Specific Populations (8.4)and Clinical Pharmacology (12.3)].• EMSAM is contraindicated in patients with pheochromocytoma because MAOIs may precipitate a hypertensive crisis in such patients.
• Serotonergic drugs: selective serotonin reuptake inhibitors (SSRIs), serotonin and norepinephrine reuptake inhibitors (SNRIs), clomipramine and imipramine, meperidine, tramadol, methadone, pentazocine, and propoxyphene; and the antitussive agent dextromethorphan should not be used with EMSAM because of a risk of serotonin syndrome .• Carbamazepine should not be used with EMSAM .• After stopping treatment with contraindicated medication, a time period equal to 4 to 5 half-lives (approximately one week) of the drug or any active metabolite should elapse before starting therapy with EMSAM. Because of the long half-life of fluoxetine and its active metabolite, at least 5 weeks should elapse between discontinuation of fluoxetine and initiation of treatment with EMSAM .• At least 2 weeks should elapse after stopping EMSAM before starting therapy with a drug that is contraindicated with EMSAM .• EMSAM is contraindicated in patients less than 12 years of age .• Pheochromocytoma .
Use of EMSAM in patients less than 12 years of age is contraindicated because of the potential for a hypertensive crisis
Limited pharmacokinetic data with doses lower than in the commercially available formulations suggest that children under age 12 may be exposed to increased levels of selegiline compared to adolescents and adults, administered with and without dietary modifications, therefore, there may be an increased risk of hypertensive crisis, even at the lowest dose of EMSAM.
Efficacy has not been established in pediatric patients ages 12 to 17 years with MDD and EMSAM is not recommended for use in this age range
A multi-center, randomized, double-blind, placebo-controlled, flexible-dose trial in 308 adolescents (ages 12 to 17 years) with MDD failed to demonstrate the efficacy of EMSAM. Diagnosis of major depressive disorder (single episode or recurrent, moderate to severe) was based on according DSM-IV criteria and Kiddie Schedule for Affective Disorders and Schizophrenia for School Aged Children (K-SADS). Enrolled patients had a Children’s Depression Rating Scale-Revised of ≥ 45 at the screening visit. Trial participants were randomized 1:1 to either EMSAM or matching placebo without forced titration for a period of 12 weeks. Active treatment consisted of EMSAM transdermal system at a dose of 6 mg per 24 hours, 9 mg per 24 hours, or 12 mg per 24 hours. The primary efficacy endpoint was the difference in total score on the Children’s Depression Rating Scale-Revised (CDRS-R) from baseline to the end of study (EOS) (Week 12). There was no observed difference in effect on CDRS-R Total Score at Week 12 (EOS) between treatments. The mean reduction in CDRS-R Total Score was 21.4 in the EMSAM-treated subjects and 21.5 in those receiving placebo treatment. Safety endpoints included physical examination, 12-lead electrocardiogram, respiration rate, temperature, supine and standing blood pressure and heart rate, application site assessments, and adverse events. Overall, safety findings were similar to those observed in EMSAM trials conducted in adults. Treatment-emergent adverse events reported by at least 5% of EMSAM-treated patients at a rate at least twice the placebo rate were insomnia (6%, 3%) and upper respiratory tract infection (7%, 3%).
EMSAM (selegiline transdermal system) is a monoamine oxidase inhibitor (MAOI) indicated for the treatment of adults with major depressive disorder (MDD)
The efficacy of EMSAM as a treatment for major depressive disorder was established in two placebo-controlled studies of 6 and 8 weeks duration in adult outpatients (ages 18 to 70 years) meeting DSM-IV criteria for major depressive disorder. In both studies, patients were randomized to double-blind treatment with EMSAM or placebo. The 6-week trial (N = 176) showed that EMSAM 6 mg per 24 hours was statistically significantly more effective than placebo on the 17-item Hamilton Depression Rating Scale (HAM-D) total score (Study 1 in Table 7). In an 8-week dose titration trial, depressed patients (N = 265), who received EMSAM or placebo at a starting dose of 6 mg per 24 hours, with possible increases to 9 mg per 24 hours or 12 mg per 24 hours based on clinical response, showed significant improvement compared with placebo on the primary outcome measure, the 28-item HAM-D total score (Study 2 in Table 7).
| SD: standard deviation; SE: standard error; LS Mean: least-squares mean; CI: confidence interval. | |||||
Study Number [Primary Measure] | Treatment Group | Number of Patients | Mean Baseline Score (SD) | LS Mean Change from Baseline (SE) | Placebo-subtracted Difference Difference (drug minus placebo) in least-squares mean change from baseline(95% CI) |
Study 1 | EMSAM (6 mg) | 89 | 22.9 (2.1) | -9.0 (0.8) | -2.5 |
[HAMD-17] | Placebo | 88 | 23.3 (2.9) | -6.5 (0.8) | (-4.6, -0.4) |
Study 2 | EMSAM | 132 | 28.3 (3.7) | -10.9 (0.8) | -2.4 |
[HAMD-28] | Placebo | 133 | 28.5 (3.9) | -8.6 (0.8) | (-4.5, -0.3) |
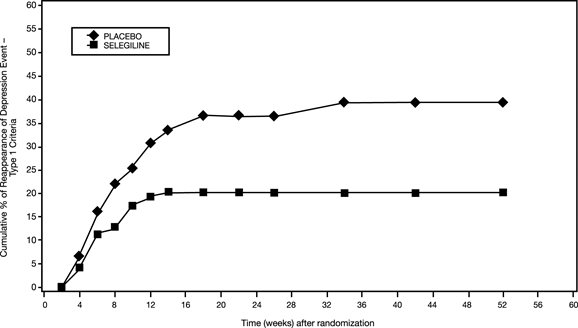
In another trial (Study 3), 322 patients meeting DSM-IV criteria for major depressive disorder who had responded during an initial 10-week open-label treatment phase for about 25 days, on average, to EMSAM 6 mg per 24 hours were randomized either to continuation of EMSAM at the same dose (N = 159) or to placebo (N = 163) under double-blind conditions for observation of relapse. About 52% of the EMSAM-treated patients, as well as about 52% of the placebo-treated patients, had discontinued treatment by week 12 of the double-blind phase. Response during the open-label phase was defined as 17-item HAM-D total score less than 10 at either week 8 or 9 and at week 10 of the open-label phase. Relapse during the double-blind phase was defined as follows: (1) a 17-item HAM-D score of 14 or greater, (2) a CGI-S score of 3 or greater (with at least a 2-point increase from double-blind baseline), and (3) meeting DSM-IV criteria for major depressive disorder on two consecutive visits at least 11 days apart. In the double-blind phase, patients receiving continued EMSAM experienced a significantly longer time to relapse (Figure 2).
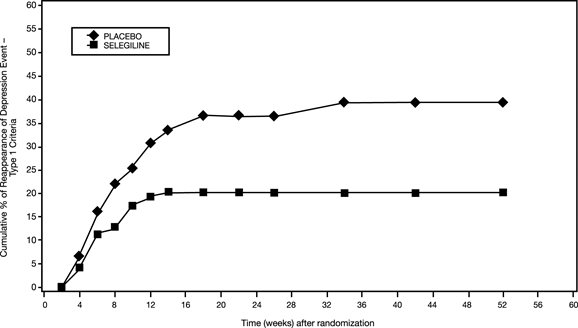
Figure 2. Kaplan-Meier Estimates of Cumulative Percent of Patients with Relapse (Study 3)
An examination of population subgroups did not reveal any clear evidence of differential responsiveness on the basis of age, gender, or race.
EMSAM should be applied to dry, intact skin on the upper torso (below the neck and above the waist), upper thigh or the outer surface of the upper arm once every 24 hours (
EMSAM should be applied to dry, intact skin on the upper torso (below the neck and above the waist), upper thigh or the outer surface of the upper arm once every 24 hours. The recommended starting dose and target dose for EMSAM is 6 mg per 24 hours. EMSAM
has been systematically evaluated and shown to be effective in a dose range of 6 mg per 24 hours to 12 mg per 24 hours. However, the trials were not designed to assess if higher doses are more effective than the lowest effective dose of 6 mg per 24 hours. Based on clinical judgment, if dose increases are indicated for individual patients, they should occur in dose increments of 3 mg per 24 hours (up to a maximum dose of 12 mg per 24 hours) at intervals of no less than 2 weeks. Full antidepressant effect may be delayed.Patients should be informed that tyramine-rich foods and beverages should be avoided beginning on the first day of EMSAM 9 mg per 24 hours or 12 mg per 24 hours treatment and should continue to be avoided for 2 weeks after a dose reduction to EMSAM 6 mg per 24 hours or following the discontinuation of EMSAM 9 mg per 24 hours or 12 mg per 24 hours
• Initial Treatment: The recommended starting dose and target dose for EMSAM is 6 mg per 24 hours ().2.1 Initial TreatmentEMSAM should be applied to dry, intact skin on the upper torso (below the neck and above the waist), upper thigh or the outer surface of the upper arm once every 24 hours. The recommended starting dose and target dose for EMSAM is 6 mg per 24 hours. EMSAM
has been systematically evaluated and shown to be effective in a dose range of 6 mg per 24 hours to 12 mg per 24 hours. However, the trials were not designed to assess if higher doses are more effective than the lowest effective dose of 6 mg per 24 hours. Based on clinical judgment, if dose increases are indicated for individual patients, they should occur in dose increments of 3 mg per 24 hours (up to a maximum dose of 12 mg per 24 hours) at intervals of no less than 2 weeks. Full antidepressant effect may be delayed.Patients should be informed that tyramine-rich foods and beverages should be avoided beginning on the first day of EMSAM 9 mg per 24 hours or 12 mg per 24 hours treatment and should continue to be avoided for 2 weeks after a dose reduction to EMSAM 6 mg per 24 hours or following the discontinuation of EMSAM 9 mg per 24 hours or 12 mg per 24 hours
[see Warnings and Precautions (5.3)].2.1 Initial TreatmentEMSAM should be applied to dry, intact skin on the upper torso (below the neck and above the waist), upper thigh or the outer surface of the upper arm once every 24 hours. The recommended starting dose and target dose for EMSAM is 6 mg per 24 hours. EMSAM
has been systematically evaluated and shown to be effective in a dose range of 6 mg per 24 hours to 12 mg per 24 hours. However, the trials were not designed to assess if higher doses are more effective than the lowest effective dose of 6 mg per 24 hours. Based on clinical judgment, if dose increases are indicated for individual patients, they should occur in dose increments of 3 mg per 24 hours (up to a maximum dose of 12 mg per 24 hours) at intervals of no less than 2 weeks. Full antidepressant effect may be delayed.Patients should be informed that tyramine-rich foods and beverages should be avoided beginning on the first day of EMSAM 9 mg per 24 hours or 12 mg per 24 hours treatment and should continue to be avoided for 2 weeks after a dose reduction to EMSAM 6 mg per 24 hours or following the discontinuation of EMSAM 9 mg per 24 hours or 12 mg per 24 hours
[see Warnings and Precautions (5.3)].• Geriatric Use: The recommended dose for elderly patients (65 years and older) is EMSAM 6 mg per 24 hours daily ().8.5 Geriatric UseThe recommended dose of EMSAM for elderly patients (65 years and older) is 6 mg per 24 hours daily. The effect of age on the pharmacokinetics or metabolism of selegiline after administration of EMSAM has not been systematically evaluated. One hundred ninety-eight (198) elderly (65 years of age and older) patients participated in clinical studies with EMSAM 6 mg per 24 hours to 12 mg per 24 hours. There were no overall differences in effectiveness between elderly and younger patients. In short-term, placebo-controlled depression trials, patients age 50 and older appeared to be at higher risk for rash (4.4% EMSAM vs. 0% placebo) than younger patients (3.4% EMSAM vs. 2.4% placebo).
• Dietary Modifications with EMSAM 9 mg per 24 hours and 12 mg per 24 hours: Tyramine-rich foods and beverages should be avoided beginning on the first day of EMSAM 9 mg per 24 hours or 12 mg per 24 hours treatment, and should continue to be avoided for 2 weeks after a dose reduction to EMSAM 6 mg per 24 hours or following the discontinuation of EMSAM 9 mg per 24 hours or 12 mg per 24 hours ().2.3 Dietary Modifications Required for Patients Taking EMSAM 9 mg per 24 hours and 12 mg per 24 hoursEMSAM (selegiline transdermal system) contains a monoamine oxidase inhibitor (MAOI). MAOIs including EMSAM combined with a high tyramine diet may cause a hypertensive crisis. A hypertensive crisis can be a life-threatening condition
[see Warnings and Precautions (5.3)].The foods and beverages listed in Table 5 should be avoided beginning on the first day of EMSAM 9 mg per 24 hours or 12 mg per 24 hours treatment, and should continue to be avoided for 2 weeks after a dose reduction to EMSAM 6 mg per 24 hours or following the discontinuation of EMSAM 9 mg per 24 hours or 12 mg per 24 hours
[see Drug Interactions (7.2)].
EMSAM (selegiline transdermal system) is supplied as 6 mg per 24 hours (20 mg per 20 cm2), 9 mg per 24 hours (30 mg per 30 cm2) and 12 mg per 24 hours (40 mg per 40 cm2) transdermal systems (TDS).
EMSAM
• Pregnancy: May cause fetal harm ().8.1 PregnancyRisk SummaryThe available data on EMSAM use in pregnant women are not sufficient to inform a drug-associated risk of adverse pregnancy-related outcomes. In animal embryo-fetal development studies, transdermal administration of selegiline to rats and rabbits at doses up to 60 and 64 times the maximum recommended human dose (MRHD) respectively, produced slight increases in malformations in both rats and rabbits, and decreased fetal weight, delayed ossification, and embryo-fetal post-implantation loss in rats. Most of these effects were seen at the high dose in both rats and rabbits. These effects were not seen at 8 times and 16 times the MRHD in rats and rabbits, respectively. In a pre-natal and post-natal development study, transdermal administration of selegiline in rats at doses 8, 24, and 60 times MRHD produced a decrease in pup weight and survival at the medium and high doses, an increase in the number of stillborn pups at the high dose, and delayed neurobehavioral and sexual development in pups
at all doses. A persistent effect on reproductive performance of pups born to mothers treated at the high dose was evident (see Data). When treating a pregnant woman with EMSAM, the physician should carefully consider both the potential risks of taking an MAOI, particularly the risk of hypertensive crisis during pregnancy, along with the established benefits of treating depression with an antidepressant.
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Clinical ConsiderationsDisease-associated maternal and embryo/fetal riskA prospective longitudinal study was conducted of 201 pregnant women with a history of major depression, who were either on antidepressants or had received antidepressants less than 12 weeks prior to their last menstrual period, and were in remission. Women who discontinued antidepressant medication during pregnancy showed a significant increase in relapse of their major depression compared to those women who remained on antidepressant medication throughout pregnancy.
DataAnimal DataIn an embryofetal development study, rats were treated with transdermal selegiline during the period of organogenesis at doses of 10, 30, and 75 mg/kg/day (8, 24, and 60 times the MRHD of EMSAM [12 mg/24 hours] on a mg/m2basis). At the highest dose there was a decrease in fetal weight and slight increases in malformations, delayed ossification (also seen at the mid dose), and embryofetal post-implantation loss. Concentrations of selegiline and its metabolites in fetal plasma were generally similar to those in maternal plasma.
In an embryofetal development study, rabbits were treated with transdermal selegiline during the period of organogenesis at doses of 2.5, 10, and 40 mg/kg/day (4, 16, and 64 times the MRHD on a mg/m2basis). A slight increase in visceral malformations was seen at the high dose.
In a prenatal and postnatal development study, rats were treated with transdermal selegiline at doses of 10, 30, and 75 mg/kg/day (8, 24, and 60 times the MRHD on a mg/m2basis) on days 6 to 21 of gestation and days 1 to 21 of the lactation period. An increase in post-implantation loss was seen at the mid and high doses, and an increase in stillborn pups was seen at the high dose. Decreases in pup weight (throughout lactation and postweaning periods) and survival (throughout lactation period), delayed pup physical development, and pup epididymal and testicular hypoplasia, were seen at the mid and high doses. Delayed neurobehavioral and sexual development was seen at all doses. Adverse effects on pup reproductive performance, as evidenced by decreases in implantations and litter size, were seen at the high dose. These findings suggest persistent effects on the offspring of treated dams. A no-effect dose was not established in this study for developmental toxicity.
• Lactation: Breastfeeding is not recommended ().8.2 LactationRisk SummaryThere is no information regarding the presence of selegiline in human milk, or on its effects on milk production or the breastfed infant. Selegiline and its metabolites are present in the milk of lactating rats (
see Data).Because of the potential for serious adverse reactions in breastfed infants from EMSAM, including the potential for hypertensive crisis, advise a woman that breastfeeding is not recommended during treatment with EMSAM and for 5 days after the final dose.
DataIn a prenatal and postnatal development study where rats were treated with transdermal selegiline at doses approximately 8, 24, and 60 times the MRHD on days 6 to 21 of gestation and days 1 to 21 of the lactation period, concentrations of selegiline and its metabolites in milk were approximately 15 and 5 times, respectively, the concentrations in maternal plasma.
• Pediatrics: EMSAM is contraindicated in patients under age 12 years and is not recommended in patients 12 to 17 years of age (,4 CONTRAINDICATIONS• EMSAM (selegiline transdermal system) is contraindicated with selective serotonin reuptake inhibitors (SSRIs, e.g., fluoxetine, sertraline, and paroxetine); serotonin and norepinephrine reuptake inhibitors (SNRIs, e.g., venlafaxine and duloxetine); the tricyclic antidepressants clomipramine and imipramine, the opiate analgesics meperidine, tramadol, methadone, pentazocine, and propoxyphene; and the antitussive agent dextromethorphan because of a risk of serotonin syndrome when EMSAM is used with these agents[see Warnings and Precautions (5.2)and Drug Interactions (7.1)].• Carbamazepine is contraindicated with EMSAM because of a possible increased risk of hypertensive crisis[see Warnings and Precautions (5.3)and Clinical Pharmacology (12.3)].• After stopping treatment with drugs contraindicated with EMSAM, a time period equal to 4 to 5 half-lives (approximately one week) of the drug or any active metabolite should elapse before starting therapy with EMSAM. Because of the long half-life of fluoxetine and its active metabolite, at least 5 weeks should elapse between discontinuation of fluoxetine and initiation of treatment with EMSAM.• At least 2 weeks should elapse after stopping EMSAM before starting therapy with any drug that is contraindicated with EMSAM.• EMSAM is contraindicated in patients less than 12 years of age because of the potential for a hypertensive crisis[see Use in Specific Populations (8.4)and Clinical Pharmacology (12.3)].• EMSAM is contraindicated in patients with pheochromocytoma because MAOIs may precipitate a hypertensive crisis in such patients.
• Serotonergic drugs: selective serotonin reuptake inhibitors (SSRIs), serotonin and norepinephrine reuptake inhibitors (SNRIs), clomipramine and imipramine, meperidine, tramadol, methadone, pentazocine, and propoxyphene; and the antitussive agent dextromethorphan should not be used with EMSAM because of a risk of serotonin syndrome .• Carbamazepine should not be used with EMSAM .• After stopping treatment with contraindicated medication, a time period equal to 4 to 5 half-lives (approximately one week) of the drug or any active metabolite should elapse before starting therapy with EMSAM. Because of the long half-life of fluoxetine and its active metabolite, at least 5 weeks should elapse between discontinuation of fluoxetine and initiation of treatment with EMSAM .• At least 2 weeks should elapse after stopping EMSAM before starting therapy with a drug that is contraindicated with EMSAM .• EMSAM is contraindicated in patients less than 12 years of age .• Pheochromocytoma .
).8.4 Pediatric UseUse of EMSAM in patients less than 12 years of age is contraindicated because of the potential for a hypertensive crisis
[see Contraindications (4)].Limited pharmacokinetic data with doses lower than in the commercially available formulations suggest that children under age 12 may be exposed to increased levels of selegiline compared to adolescents and adults, administered with and without dietary modifications, therefore, there may be an increased risk of hypertensive crisis, even at the lowest dose of EMSAM.
Efficacy has not been established in pediatric patients ages 12 to 17 years with MDD and EMSAM is not recommended for use in this age range
[see Clinical Pharmacology (12.3)].A multi-center, randomized, double-blind, placebo-controlled, flexible-dose trial in 308 adolescents (ages 12 to 17 years) with MDD failed to demonstrate the efficacy of EMSAM. Diagnosis of major depressive disorder (single episode or recurrent, moderate to severe) was based on according DSM-IV criteria and Kiddie Schedule for Affective Disorders and Schizophrenia for School Aged Children (K-SADS). Enrolled patients had a Children’s Depression Rating Scale-Revised of ≥ 45 at the screening visit. Trial participants were randomized 1:1 to either EMSAM or matching placebo without forced titration for a period of 12 weeks. Active treatment consisted of EMSAM transdermal system at a dose of 6 mg per 24 hours, 9 mg per 24 hours, or 12 mg per 24 hours. The primary efficacy endpoint was the difference in total score on the Children’s Depression Rating Scale-Revised (CDRS-R) from baseline to the end of study (EOS) (Week 12). There was no observed difference in effect on CDRS-R Total Score at Week 12 (EOS) between treatments. The mean reduction in CDRS-R Total Score was 21.4 in the EMSAM-treated subjects and 21.5 in those receiving placebo treatment. Safety endpoints included physical examination, 12-lead electrocardiogram, respiration rate, temperature, supine and standing blood pressure and heart rate, application site assessments, and adverse events. Overall, safety findings were similar to those observed in EMSAM trials conducted in adults. Treatment-emergent adverse events reported by at least 5% of EMSAM-treated patients at a rate at least twice the placebo rate were insomnia (6%, 3%) and upper respiratory tract infection (7%, 3%).
• EMSAM (selegiline transdermal system) is contraindicated with selective serotonin reuptake inhibitors (SSRIs, e.g., fluoxetine, sertraline, and paroxetine); serotonin and norepinephrine reuptake inhibitors (SNRIs, e.g., venlafaxine and duloxetine); the tricyclic antidepressants clomipramine and imipramine, the opiate analgesics meperidine, tramadol, methadone, pentazocine, and propoxyphene; and the antitussive agent dextromethorphan because of a risk of serotonin syndrome when EMSAM is used with these agents[see.and5.2 Serotonin SyndromeThe development of a potentially life-threatening serotonin syndrome has been reported with concomitant use of MAOIs, such as EMSAM, with serotonergic drugs. These reactions have also been reported in patients who have discontinued serotonergic drugs and then subsequently started an MAOI
[see Contraindications (4)].Serotonin syndrome symptoms may include mental status changes (e.g., agitation, hallucinations, delirium, and coma), autonomic instability (e.g., tachycardia, labile blood pressure, dizziness, diaphoresis, flushing, hyperthermia), neuromuscular changes (e.g., tremor, rigidity, myoclonus, hyperreflexia, incoordination), seizures, and/or gastrointestinal symptoms (e.g., nausea, vomiting, diarrhea).
Patients should be monitored for the emergence of serotonin syndrome. Treatment with EMSAM and any concomitant serotonergic agents should be discontinued immediately if the above events occur and supportive treatment should be initiated.
]7.1 Serotonergic DrugsSerious, sometimes fatal, central nervous system (CNS) toxicity referred to as the “serotonin syndrome” has been reported with the combination of nonselective MAOIs and serotonergic drugs. Use of EMSAM with these drugs is contraindicated
[see Contraindications (4)and Warnings and Precautions (5.2)].• Carbamazepine is contraindicated with EMSAM because of a possible increased risk of hypertensive crisis[see.and5.3 Blood Pressure ElevationTyramine-Induced Hypertensive CrisisEMSAM inhibits the catabolism of dietary amines, such as tyramine, and has the potential to produce a hypertensive crisis following the ingestion of tyramine-rich foods or beverages
[see Drug Interactions (7.2)and Clinical Pharmacology (12.2)].Hypertensive crises, which in some cases may be fatal, are characterized by some or all of the following symptoms: occipital headache which may radiate frontally, palpitation, neck stiffness or soreness, nausea, vomiting, sweating (sometimes with fever and sometimes with cold, clammy skin), dilated pupils, and photophobia. Either tachycardia or bradycardia may be present and can be associated with constricting chest pain. Intracranial bleeding has been reported in association with the increase in blood pressure. Patients should be instructed as to the signs and symptoms of severe hypertension and advised to seek immediate medical attention if these signs or symptoms are present.
If a hypertensive crisis occurs, EMSAM should be discontinued immediately and therapy to lower blood pressure should be instituted immediately. Fever should be managed by means of external cooling. Patients must be closely monitored until symptoms have stabilized. To prevent a hypertensive crisis, patients receiving treatment with EMSAM 9 mg per 24 hours or EMSAM 12 mg per 24 hours should follow the advice regarding a low tyramine diet described in Table 5 under Dietary Modifications Required for Patients Taking EMSAM 9 mg per 24 hours and 12 mg per 24 hours
[see Drug Interactions (7.2)].Blood Pressure Elevation Related to Concomitant MedicationCarbamazepine is contraindicated with EMSAM because carbamazepine has been shown to significantly elevate selegiline levels, which may increase the risk of a hypertensive crisis
[see Contraindications (4)and Drug Interactions (7.4)].The use of EMSAM with adrenergic drugs or buspirone may produce substantial increases in blood pressure. Therefore, monitor blood pressure if EMSAM is used with any of the following drugs: buspirone, amphetamines, or cold products or weight-reducing preparations that contain sympathomimetic amines (e.g., pseudoephedrine, phenylephrine, phenylpropanolamine, and ephedrine).
]12.3 PharmacokineticsAbsorptionFollowing dermal application of EMSAM to humans, 25% to 30% of the
selegilinecontent on average is delivered systemically over 24 hours (range approximately 10% to 40%). Consequently, the degree of drug absorption may be 1/3 higher than the average amounts of 6 mg to 12 mg per 24 hours. Transdermal dosing results in significantly higher exposure to selegiline with significantly lower exposure for all metabolites when compared to oral dosing, due to extensive first-pass metabolism. In a 10-day study with daily administration of EMSAM to healthy male and female volunteers, steady-state selegiline plasma concentrations indicated selegiline concentration-time profiles were comparable when EMSAM is applied to the upper torso or upper thigh, and absorption from these two sites of administration was equivalent.DistributionFollowing dermal application of radiolabeled selegiline to laboratory animals, selegiline is rapidly distributed to all body tissues. Selegiline rapidly penetrates the blood-brain barrier.
In humans, selegiline is approximately 90% bound to plasma protein over a 2 to 500 ng per mL concentration range. Selegiline does not accumulate in the skin.
In vivo MetabolismTransdermally absorbed selegiline (via EMSAM) is not metabolized in human skin and does not undergo extensive first-pass metabolism. Selegiline is extensively metabolized by several CYP450-dependent enzyme systems (
see In vitro Metabolism). Selegiline is metabolized initially via N-dealkylation or N-depropargylation to form N-desmethylselegiline or R(-)-methamphetamine, respectively. Both of these metabolites can be further metabolized to R(-)-amphetamine. These metabolites are all levorotatory (l-)enantiomers and no racemic biotransformation to the dextrorotatory form (i.e., S(+)-amphetamine or S(+)-methamphetamine) occurs. R(-)-methamphetamine and R(-)-amphetamine are mainly excreted unchanged in urine.In vitro MetabolismIn vitrostudies utilizing human liver microsomes demonstrated that several CYP450-dependent enzymes are involved in the metabolism of selegiline and its metabolites. CYP2B6, CYP2C9, CYP3A4 and CYP3A5 appeared to be the major contributing enzymes in the formation of R(-)-methamphetamine from selegiline, with CYP2A6 having a minor role. CYP2A6, CYP2B6, CYP3A4 and CYP3A5 appeared to contribute to the formation of R(-)-amphetamine from N-desmethylselegiline.The potential for selegiline or N-desmethylselegiline to inhibit individual CYP450-dependent enzyme pathways was also examined
in vitrowith human liver microsomes. Each substrate was examined over a concentration range of 2.5 to 250 mcM. Consistent with competitive inhibition, both selegiline and N-desmethylselegiline caused a concentration dependent inhibition of CYP2D6 at 10 to 250 mcM and CYP3A4 and CYP3A5 at 25 to 250 mcM. CYP2C19 and CYP2B6 were also inhibited at concentrations of 100 mcM or greater. All inhibitory effects of selegiline and N-desmethylselegiline occurred at concentrations that are several orders of magnitude higher than concentrations seen clinically (highest predose concentration observed at a dose of 12 mg per 24 hours at steady-state was 0.046 mcM)[see Drug Interactions (7)].ExcretionApproximately 10% and 2% of a radiolabeled dose applied dermally, as a DMSO solution, was recovered in urine and feces respectively, with at least 63% of the dose remaining unabsorbed. The remaining 25% of the dose was unaccounted for. Urinary excretion of unchanged selegiline accounted for 0.1% of the applied dose with the remainder of the dose recovered in urine being metabolites.
The systemic clearance of selegiline after intravenous administration was 1.4 L per min, and the mean half-lives of selegiline and its three metabolites, R(-)-N-desmethylselegiline, R(-)-amphetamine, and R(-)-methamphetamine, ranged from 18 to 25 hours.
Population SubgroupsAgeEMSAM should not be used in patients less than 18 years of age
[see Use in Specific Populations (8.4)].Stratification of exposure data following treatment with EMSAM indicated that pre-dose (trough) selegiline plasma concentrations at steady state appeared higher (p = 0.12) in children aged < 12 years old, compared to adolescents aged ≥ 12 years as shown in Table 6.
Table 6. Steady State Selegiline Trough Concentrations Associated with Administration of EMSAM 15 mg/15 cm2Daily for 7 Days Trough Concentration, pg/mL6 to 11 year old age group12 to 14 year old age group(N = 6)
(N = 4)
Mean (SD)2,562 (974)
1,821 (146)
Drug-Drug InteractionsAlcoholThe pharmacokinetics and pharmacodynamics of alcohol (0.75 mg per kg) alone or in combination with EMSAM 6 mg per 24 hours for 7 days of treatment was examined in 16 healthy volunteers. No clinically significant differences were observed in the pharmacokinetics or pharmacodynamics of alcohol or the pharmacokinetics of selegiline during co-administration. Although EMSAM has not been shown to increase the impairment of mental and motor skills caused by alcohol (0.75 mg per kg) and failed to alter the pharmacokinetic properties of alcohol, patients should be advised that the use of alcohol is not recommended while taking EMSAM
[see Drug Interactions (7.4)and (7.5)].AlprazolamIn subjects who had received EMSAM 6 mg per 24 hours for 7 days, co-administration with alprazolam (15 mg per day), a CYP3A4 and CYP3A5 substrate, did not affect the pharmacokinetics of alprazolam or selegiline
[see Drug Interactions (7.4)and (7.5)].CarbamazepineCarbamazepine is an enzyme inducer and typically causes decreases in drug exposure; however, approximately 2-fold increased systemic exposure of selegiline and its metabolites, L-amphetamine and L-methamphetamine were seen after single application of EMSAM 6 mg per 24 hours in subjects who had received carbamazepine (400 mg per day) for 14 days. Changes in plasma selegiline concentrations were nearly 2-fold and variable across the subject population. Such increases may increase the risk of a hypertensive crisis when carbamazepine is used with EMSAM at any dose
[see Contraindications (4), Warnings and Precautions (5.3)and Drug Interaction (7.4)].IbuprofenIn subjects who had received EMSAM 6 mg per 24 hours for 11 days, combined administration with the CYP2C9 substrate ibuprofen (800 mg single dose) did not affect the pharmacokinetics of either selegiline or ibuprofen
[see Drug Interactions (7.4)and (7.5)].KetoconazoleSeven-day treatment with ketoconazole (200 mg per day), a potent inhibitor of CYP3A4, did not affect the steady-state pharmacokinetics of selegiline in subjects who received EMSAM 6 mg per 24 hours for 7 days and no differences in the pharmacokinetics of ketoconazole were observed
[see Drug Interactions (7.4)and (7.5)].LevothyroxineIn healthy subjects who had received EMSAM 6 mg per 24 hours for 10 days, single dose administration with levothyroxine (150 mcg) did not alter the pharmacokinetics of either selegiline or levothyroxine
[see Drug Interactions (7.4)and (7.5)].OlanzapineIn subjects who had received EMSAM 6 mg per 24 hours for 10 days, co-administration with olanzapine, a substrate for CYP1A2, CYP2D6, and possibly CYP2A6, did not affect the pharmacokinetics of selegiline or olanzapine
[see Drug Interactions (7.4)and (7.5)].Phenylpropanolamine (PPA)In subjects who had received EMSAM 6 mg per 24 hours for 9 days, co-administration with PPA (25 mg every 4 hours for 24 hours) did not affect the pharmacokinetics of PPA. There was a higher incidence of significant blood pressure elevations with the co-administration of EMSAM and PPA than with PPA alone, suggesting a possible pharmacodynamic interaction
[see Drug Interactions (7.4)and (7.5)].PseudoephedrineEMSAM 6 mg per 24 hours for 10 days, co-administered with pseudoephedrine (60 mg, 3 times a day) did not affect the pharmacokinetics of pseudoephedrine. There were no clinically significant changes in blood pressure during pseudoephedrine administration alone, or in combination with EMSAM
[see Drug Interactions (7.4)and (7.5)].RisperidoneIn subjects who had received EMSAM 6 mg per 24 hours for 10 days, co-administration with risperidone (2 mg per day for 7 days), a substrate for CYP2D6, did not affect the pharmacokinetics of selegiline or risperidone
[see Drug Interactions (7.4)and (7.5)].WarfarinWarfarin is a substrate for CYP2C9 and CYP3A4 metabolism pathways. In healthy volunteers titrated with Coumadin®(warfarin sodium) to clinical levels of anticoagulation (INR of 1.5 to 2), co-administration with EMSAM 6 mg per 24 hours for 7 days did not affect the pharmacokinetics of the individual warfarin enantiomers. EMSAM did not alter the clinical pharmacodynamic effects of warfarin as measured by INR, Factor VII or Factor X levels
[see Drug Interactions (7.4)and (7.5)].• After stopping treatment with drugs contraindicated with EMSAM, a time period equal to 4 to 5 half-lives (approximately one week) of the drug or any active metabolite should elapse before starting therapy with EMSAM. Because of the long half-life of fluoxetine and its active metabolite, at least 5 weeks should elapse between discontinuation of fluoxetine and initiation of treatment with EMSAM.• At least 2 weeks should elapse after stopping EMSAM before starting therapy with any drug that is contraindicated with EMSAM.• EMSAM is contraindicated in patients less than 12 years of age because of the potential for a hypertensive crisis[see.and8.4 Pediatric UseUse of EMSAM in patients less than 12 years of age is contraindicated because of the potential for a hypertensive crisis
[see Contraindications (4)].Limited pharmacokinetic data with doses lower than in the commercially available formulations suggest that children under age 12 may be exposed to increased levels of selegiline compared to adolescents and adults, administered with and without dietary modifications, therefore, there may be an increased risk of hypertensive crisis, even at the lowest dose of EMSAM.
Efficacy has not been established in pediatric patients ages 12 to 17 years with MDD and EMSAM is not recommended for use in this age range
[see Clinical Pharmacology (12.3)].A multi-center, randomized, double-blind, placebo-controlled, flexible-dose trial in 308 adolescents (ages 12 to 17 years) with MDD failed to demonstrate the efficacy of EMSAM. Diagnosis of major depressive disorder (single episode or recurrent, moderate to severe) was based on according DSM-IV criteria and Kiddie Schedule for Affective Disorders and Schizophrenia for School Aged Children (K-SADS). Enrolled patients had a Children’s Depression Rating Scale-Revised of ≥ 45 at the screening visit. Trial participants were randomized 1:1 to either EMSAM or matching placebo without forced titration for a period of 12 weeks. Active treatment consisted of EMSAM transdermal system at a dose of 6 mg per 24 hours, 9 mg per 24 hours, or 12 mg per 24 hours. The primary efficacy endpoint was the difference in total score on the Children’s Depression Rating Scale-Revised (CDRS-R) from baseline to the end of study (EOS) (Week 12). There was no observed difference in effect on CDRS-R Total Score at Week 12 (EOS) between treatments. The mean reduction in CDRS-R Total Score was 21.4 in the EMSAM-treated subjects and 21.5 in those receiving placebo treatment. Safety endpoints included physical examination, 12-lead electrocardiogram, respiration rate, temperature, supine and standing blood pressure and heart rate, application site assessments, and adverse events. Overall, safety findings were similar to those observed in EMSAM trials conducted in adults. Treatment-emergent adverse events reported by at least 5% of EMSAM-treated patients at a rate at least twice the placebo rate were insomnia (6%, 3%) and upper respiratory tract infection (7%, 3%).
]12.3 PharmacokineticsAbsorptionFollowing dermal application of EMSAM to humans, 25% to 30% of the
selegilinecontent on average is delivered systemically over 24 hours (range approximately 10% to 40%). Consequently, the degree of drug absorption may be 1/3 higher than the average amounts of 6 mg to 12 mg per 24 hours. Transdermal dosing results in significantly higher exposure to selegiline with significantly lower exposure for all metabolites when compared to oral dosing, due to extensive first-pass metabolism. In a 10-day study with daily administration of EMSAM to healthy male and female volunteers, steady-state selegiline plasma concentrations indicated selegiline concentration-time profiles were comparable when EMSAM is applied to the upper torso or upper thigh, and absorption from these two sites of administration was equivalent.DistributionFollowing dermal application of radiolabeled selegiline to laboratory animals, selegiline is rapidly distributed to all body tissues. Selegiline rapidly penetrates the blood-brain barrier.
In humans, selegiline is approximately 90% bound to plasma protein over a 2 to 500 ng per mL concentration range. Selegiline does not accumulate in the skin.
In vivo MetabolismTransdermally absorbed selegiline (via EMSAM) is not metabolized in human skin and does not undergo extensive first-pass metabolism. Selegiline is extensively metabolized by several CYP450-dependent enzyme systems (
see In vitro Metabolism). Selegiline is metabolized initially via N-dealkylation or N-depropargylation to form N-desmethylselegiline or R(-)-methamphetamine, respectively. Both of these metabolites can be further metabolized to R(-)-amphetamine. These metabolites are all levorotatory (l-)enantiomers and no racemic biotransformation to the dextrorotatory form (i.e., S(+)-amphetamine or S(+)-methamphetamine) occurs. R(-)-methamphetamine and R(-)-amphetamine are mainly excreted unchanged in urine.In vitro MetabolismIn vitrostudies utilizing human liver microsomes demonstrated that several CYP450-dependent enzymes are involved in the metabolism of selegiline and its metabolites. CYP2B6, CYP2C9, CYP3A4 and CYP3A5 appeared to be the major contributing enzymes in the formation of R(-)-methamphetamine from selegiline, with CYP2A6 having a minor role. CYP2A6, CYP2B6, CYP3A4 and CYP3A5 appeared to contribute to the formation of R(-)-amphetamine from N-desmethylselegiline.The potential for selegiline or N-desmethylselegiline to inhibit individual CYP450-dependent enzyme pathways was also examined
in vitrowith human liver microsomes. Each substrate was examined over a concentration range of 2.5 to 250 mcM. Consistent with competitive inhibition, both selegiline and N-desmethylselegiline caused a concentration dependent inhibition of CYP2D6 at 10 to 250 mcM and CYP3A4 and CYP3A5 at 25 to 250 mcM. CYP2C19 and CYP2B6 were also inhibited at concentrations of 100 mcM or greater. All inhibitory effects of selegiline and N-desmethylselegiline occurred at concentrations that are several orders of magnitude higher than concentrations seen clinically (highest predose concentration observed at a dose of 12 mg per 24 hours at steady-state was 0.046 mcM)[see Drug Interactions (7)].ExcretionApproximately 10% and 2% of a radiolabeled dose applied dermally, as a DMSO solution, was recovered in urine and feces respectively, with at least 63% of the dose remaining unabsorbed. The remaining 25% of the dose was unaccounted for. Urinary excretion of unchanged selegiline accounted for 0.1% of the applied dose with the remainder of the dose recovered in urine being metabolites.
The systemic clearance of selegiline after intravenous administration was 1.4 L per min, and the mean half-lives of selegiline and its three metabolites, R(-)-N-desmethylselegiline, R(-)-amphetamine, and R(-)-methamphetamine, ranged from 18 to 25 hours.
Population SubgroupsAgeEMSAM should not be used in patients less than 18 years of age
[see Use in Specific Populations (8.4)].Stratification of exposure data following treatment with EMSAM indicated that pre-dose (trough) selegiline plasma concentrations at steady state appeared higher (p = 0.12) in children aged < 12 years old, compared to adolescents aged ≥ 12 years as shown in Table 6.
Table 6. Steady State Selegiline Trough Concentrations Associated with Administration of EMSAM 15 mg/15 cm2Daily for 7 Days Trough Concentration, pg/mL6 to 11 year old age group12 to 14 year old age group(N = 6)
(N = 4)
Mean (SD)2,562 (974)
1,821 (146)
Drug-Drug InteractionsAlcoholThe pharmacokinetics and pharmacodynamics of alcohol (0.75 mg per kg) alone or in combination with EMSAM 6 mg per 24 hours for 7 days of treatment was examined in 16 healthy volunteers. No clinically significant differences were observed in the pharmacokinetics or pharmacodynamics of alcohol or the pharmacokinetics of selegiline during co-administration. Although EMSAM has not been shown to increase the impairment of mental and motor skills caused by alcohol (0.75 mg per kg) and failed to alter the pharmacokinetic properties of alcohol, patients should be advised that the use of alcohol is not recommended while taking EMSAM
[see Drug Interactions (7.4)and (7.5)].AlprazolamIn subjects who had received EMSAM 6 mg per 24 hours for 7 days, co-administration with alprazolam (15 mg per day), a CYP3A4 and CYP3A5 substrate, did not affect the pharmacokinetics of alprazolam or selegiline
[see Drug Interactions (7.4)and (7.5)].CarbamazepineCarbamazepine is an enzyme inducer and typically causes decreases in drug exposure; however, approximately 2-fold increased systemic exposure of selegiline and its metabolites, L-amphetamine and L-methamphetamine were seen after single application of EMSAM 6 mg per 24 hours in subjects who had received carbamazepine (400 mg per day) for 14 days. Changes in plasma selegiline concentrations were nearly 2-fold and variable across the subject population. Such increases may increase the risk of a hypertensive crisis when carbamazepine is used with EMSAM at any dose
[see Contraindications (4), Warnings and Precautions (5.3)and Drug Interaction (7.4)].IbuprofenIn subjects who had received EMSAM 6 mg per 24 hours for 11 days, combined administration with the CYP2C9 substrate ibuprofen (800 mg single dose) did not affect the pharmacokinetics of either selegiline or ibuprofen
[see Drug Interactions (7.4)and (7.5)].KetoconazoleSeven-day treatment with ketoconazole (200 mg per day), a potent inhibitor of CYP3A4, did not affect the steady-state pharmacokinetics of selegiline in subjects who received EMSAM 6 mg per 24 hours for 7 days and no differences in the pharmacokinetics of ketoconazole were observed
[see Drug Interactions (7.4)and (7.5)].LevothyroxineIn healthy subjects who had received EMSAM 6 mg per 24 hours for 10 days, single dose administration with levothyroxine (150 mcg) did not alter the pharmacokinetics of either selegiline or levothyroxine
[see Drug Interactions (7.4)and (7.5)].OlanzapineIn subjects who had received EMSAM 6 mg per 24 hours for 10 days, co-administration with olanzapine, a substrate for CYP1A2, CYP2D6, and possibly CYP2A6, did not affect the pharmacokinetics of selegiline or olanzapine
[see Drug Interactions (7.4)and (7.5)].Phenylpropanolamine (PPA)In subjects who had received EMSAM 6 mg per 24 hours for 9 days, co-administration with PPA (25 mg every 4 hours for 24 hours) did not affect the pharmacokinetics of PPA. There was a higher incidence of significant blood pressure elevations with the co-administration of EMSAM and PPA than with PPA alone, suggesting a possible pharmacodynamic interaction
[see Drug Interactions (7.4)and (7.5)].PseudoephedrineEMSAM 6 mg per 24 hours for 10 days, co-administered with pseudoephedrine (60 mg, 3 times a day) did not affect the pharmacokinetics of pseudoephedrine. There were no clinically significant changes in blood pressure during pseudoephedrine administration alone, or in combination with EMSAM
[see Drug Interactions (7.4)and (7.5)].RisperidoneIn subjects who had received EMSAM 6 mg per 24 hours for 10 days, co-administration with risperidone (2 mg per day for 7 days), a substrate for CYP2D6, did not affect the pharmacokinetics of selegiline or risperidone
[see Drug Interactions (7.4)and (7.5)].WarfarinWarfarin is a substrate for CYP2C9 and CYP3A4 metabolism pathways. In healthy volunteers titrated with Coumadin®(warfarin sodium) to clinical levels of anticoagulation (INR of 1.5 to 2), co-administration with EMSAM 6 mg per 24 hours for 7 days did not affect the pharmacokinetics of the individual warfarin enantiomers. EMSAM did not alter the clinical pharmacodynamic effects of warfarin as measured by INR, Factor VII or Factor X levels
[see Drug Interactions (7.4)and (7.5)].• EMSAM is contraindicated in patients with pheochromocytoma because MAOIs may precipitate a hypertensive crisis in such patients.