Flecainide Acetate
Flecainide Acetate Prescribing Information
In patients without structural heart disease, flecainide is indicated for the prevention of
- paroxysmal supraventricular tachycardias (PSVT), including atrioventricular nodal reentrant tachycardia, atrioventricular reentrant tachycardia and other supraventricular tachycardias of unspecified mechanism associated with disabling symptoms
- paroxysmal atrial fibrillation/flutter (PAF) associated with disabling symptoms.
Flecainide is also indicated for the prevention of
- documented ventricular arrhythmias, such as
Use of flecainide for the treatment of sustained VT, like other antiarrhythmics, should be initiated in the hospital. The use of flecainide is not recommended in patients with less severe ventricular arrhythmias even if the patients are symptomatic.
Because of the proarrhythmic effects of flecainide, its use should be reserved for patients in whom, in the opinion of the physician, the benefits of treatment outweigh the risks.
Flecainide should not be used in patients with recent myocardial infarction (see
Use of flecainide in chronic atrial fibrillation has not been adequately studied and is not recommended (see
As is the case for other antiarrhythmic agents, there is no evidence from controlled trials that the use of flecainide favorably affects survival or the incidence of sudden death.
Flecainide has a long half-life (12 to 27 hours in patients). Steady-state plasma levels, in patients with normal renal and hepatic function, may not be achieved until the patient has received 3 to 5 days of therapy at a given dose. Therefore,
For patients with PSVT and patients with PAF the recommended starting dose is 50 mg every 12 hours. Flecainide acetate doses may be increased in increments of 50 mg bid every four days until efficacy is achieved. For PAF patients, a substantial increase in efficacy without a substantial increase in discontinuations for adverse experiences may be achieved by increasing the flecainide acetate dose from 50 to 100 mg bid. The maximum recommended dose for patients with paroxysmal supraventricular arrhythmias is 300 mg/day.
For
In patients with
Mortality Flecainide was included in the National Heart Lung and Blood Institute’s Cardiac Arrhythmia Suppression Trial (CAST), a long-term, multi center, randomized, double-blind study in patients with asymptomatic non-life-threatening ventricular arrhythmias who had a myocardial infarction more than six days, but less than two years previously. An excessive mortality or non-fatal cardiac arrest rate was seen in patients treated with flecainide compared with that seen in a carefully matched placebo-treated group. This rate was 16/315 (5.1%) for flecainide and 7/309 (2.3%) for the matched placebo. The average duration of treatment with flecainide in this study was 10 months. The applicability of the CAST results to other populations (e.g., those without recent myocardial infarction) is uncertain, but at present it is prudent to consider the risks of Class 1C agents (including flecainide), coupled with the lack of any evidence of improved survival, generally unacceptable in patients without life-threatening ventricular arrhythmias, even if the patients are experiencing unpleasant, but not life-threatening, symptoms or signs. Ventricular Proarrhythmic Effects in Patients with Atrial Fibrillation/Flutter A review of the world literature revealed reports of 568 patients treated with oral flecainide for paroxysmal atrial fibrillation/flutter (PAF). Ventricular tachycardia was experienced in 0.4% (2/568) of these patients. Of 19 patients in the literature with chronic atrial fibrillation (CAF), 10.5% (2) experienced VT or VF. FLECAINIDE IS NOT RECOMMENDED FOR USE IN PATIENTS WITH CHRONIC ATRIAL FIBRILLATION Case reports of ventricular proarrhythmic effects in patients treated with flecainide for atrial fibrillation/flutter have included increased PVCs, VT, ventricular fibrillation (VF) and death. As with other Class 1 agents, patients treated with flecainide for atrial flutter have been reported with 1:1 atrioventricular conduction due to slowing the atrial rate. A paradoxical increase in the ventricular rate also may occur in patients with atrial fibrillation who receive flecainide. Concomitant negative chronotropic therapy such as digoxin or beta-blockers may lower the risk of this complication. |
Flecainide slows cardiac conduction in most patients to produce dose-related increases in PR, QRS and QT intervals. PR interval increases on average about 25% (0.04 seconds) and as much as 118% in some patients. Approximately one-third of patients may develop new first-degree AV heart block (PR interval ≥0.20 seconds). The QRS complex increases on average about 25% (0.02 seconds) and as much as 150% in some patients. Many patients develop QRS complexes with a duration of 0.12 seconds or more. In one study, 4% of patients developed new bundle branch block while on flecainide. The degree of lengthening of PR and QRS intervals does not predict either efficacy or the development of cardiac adverse effects. In clinical trials, it was unusual for PR intervals to increase to 0.30 seconds or more, or for QRS intervals to increase to 0.18 seconds or more. Thus, caution should be used when such intervals occur, and dose reductions may be considered. The QT interval widens about 8%, but most of this widening (about 60% to 90%) is due to widening of the QRS duration. The JT interval (QT minus QRS) only widens about 4% on the average. Significant JT prolongation occurs in less than 2% of patients. There have been rare cases of Torsade de Pointes-type arrhythmia associated with flecainide therapy.
Clinically significant conduction changes have been observed at these rates: sinus node dysfunction such as sinus pause, sinus arrest and symptomatic bradycardia (1.2%), second degree AV block (0.5%) and third-degree AV block (0.4%). An attempt should be made to manage the patient on the lowest effective dose in an effort to minimize these effects (see
Flecainide should be used only with extreme caution in patients with sick sinus syndrome because it may cause sinus bradycardia, sinus pause, or sinus arrest.
Flecainide is known to increase endocardial pacing thresholds and may suppress ventricular escape rhythms. These effects are reversible if flecainide is discontinued. It should be used with caution in patients with permanent pacemakers or temporary pacing electrodes and should not be administered to patients with existing poor thresholds or nonprogrammable pacemakers unless suitable pacing rescue is available.
The pacing threshold in patients with pacemakers should be determined prior to instituting therapy with flecainide, again after one week of administration and at regular intervals thereafter. Generally, threshold changes are within the range of multiprogrammable pacemakers and, when these occur, a doubling of either voltage or pulse width is usually sufficient to regain capture.
Hypokalemia or hyperkalemia may alter the effects of Class I antiarrhythmic drugs. Preexisting hypokalemia or hyperkalemia should be corrected before administration of flecainide.
The safety and efficacy of flecainide in the fetus, infant, or child have not been established in double-blind, randomized, placebo-controlled trials. The proarrhythmic effects of flecainide as described previously, apply also to children. In pediatric patients with structural heart disease, flecainide has been associated with cardiac arrest and sudden death. Flecainide should be started in the hospital with rhythm monitoring. Any use of flecainide in children should be directly supervised by a cardiologist skilled in the treatment of arrhythmias in children.
Intravenous lidocaine has been used occasionally with flecainide while awaiting the therapeutic effect of flecainide. No adverse drug interactions were apparent. However, no formal studies have been performed to demonstrate the usefulness of this regimen.
An occasional patient not adequately controlled by (or intolerant to) a dose given at 12-hour intervals may be dosed at eight-hour intervals.
Once adequate control of the arrhythmia has been achieved, it may be possible in some patients to reduce the dose as necessary to minimize side effects or effects on conduction. In such patients, efficacy at the lower dose should be evaluated.
Flecainide should be used cautiously in patients with a history of CHF or myocardial dysfunction (see
Mortality Flecainide was included in the National Heart Lung and Blood Institute’s Cardiac Arrhythmia Suppression Trial (CAST), a long-term, multi center, randomized, double-blind study in patients with asymptomatic non-life-threatening ventricular arrhythmias who had a myocardial infarction more than six days, but less than two years previously. An excessive mortality or non-fatal cardiac arrest rate was seen in patients treated with flecainide compared with that seen in a carefully matched placebo-treated group. This rate was 16/315 (5.1%) for flecainide and 7/309 (2.3%) for the matched placebo. The average duration of treatment with flecainide in this study was 10 months. The applicability of the CAST results to other populations (e.g., those without recent myocardial infarction) is uncertain, but at present it is prudent to consider the risks of Class 1C agents (including flecainide), coupled with the lack of any evidence of improved survival, generally unacceptable in patients without life-threatening ventricular arrhythmias, even if the patients are experiencing unpleasant, but not life-threatening, symptoms or signs. Ventricular Proarrhythmic Effects in Patients with Atrial Fibrillation/Flutter A review of the world literature revealed reports of 568 patients treated with oral flecainide for paroxysmal atrial fibrillation/flutter (PAF). Ventricular tachycardia was experienced in 0.4% (2/568) of these patients. Of 19 patients in the literature with chronic atrial fibrillation (CAF), 10.5% (2) experienced VT or VF. FLECAINIDE IS NOT RECOMMENDED FOR USE IN PATIENTS WITH CHRONIC ATRIAL FIBRILLATION Case reports of ventricular proarrhythmic effects in patients treated with flecainide for atrial fibrillation/flutter have included increased PVCs, VT, ventricular fibrillation (VF) and death. As with other Class 1 agents, patients treated with flecainide for atrial flutter have been reported with 1:1 atrioventricular conduction due to slowing the atrial rate. A paradoxical increase in the ventricular rate also may occur in patients with atrial fibrillation who receive flecainide. Concomitant negative chronotropic therapy such as digoxin or beta-blockers may lower the risk of this complication. |
Flecainide slows cardiac conduction in most patients to produce dose-related increases in PR, QRS and QT intervals. PR interval increases on average about 25% (0.04 seconds) and as much as 118% in some patients. Approximately one-third of patients may develop new first-degree AV heart block (PR interval ≥0.20 seconds). The QRS complex increases on average about 25% (0.02 seconds) and as much as 150% in some patients. Many patients develop QRS complexes with a duration of 0.12 seconds or more. In one study, 4% of patients developed new bundle branch block while on flecainide. The degree of lengthening of PR and QRS intervals does not predict either efficacy or the development of cardiac adverse effects. In clinical trials, it was unusual for PR intervals to increase to 0.30 seconds or more, or for QRS intervals to increase to 0.18 seconds or more. Thus, caution should be used when such intervals occur, and dose reductions may be considered. The QT interval widens about 8%, but most of this widening (about 60% to 90%) is due to widening of the QRS duration. The JT interval (QT minus QRS) only widens about 4% on the average. Significant JT prolongation occurs in less than 2% of patients. There have been rare cases of Torsade de Pointes-type arrhythmia associated with flecainide therapy.
Clinically significant conduction changes have been observed at these rates: sinus node dysfunction such as sinus pause, sinus arrest and symptomatic bradycardia (1.2%), second degree AV block (0.5%) and third-degree AV block (0.4%). An attempt should be made to manage the patient on the lowest effective dose in an effort to minimize these effects (see
Flecainide should be used only with extreme caution in patients with sick sinus syndrome because it may cause sinus bradycardia, sinus pause, or sinus arrest.
Flecainide is known to increase endocardial pacing thresholds and may suppress ventricular escape rhythms. These effects are reversible if flecainide is discontinued. It should be used with caution in patients with permanent pacemakers or temporary pacing electrodes and should not be administered to patients with existing poor thresholds or nonprogrammable pacemakers unless suitable pacing rescue is available.
The pacing threshold in patients with pacemakers should be determined prior to instituting therapy with flecainide, again after one week of administration and at regular intervals thereafter. Generally, threshold changes are within the range of multiprogrammable pacemakers and, when these occur, a doubling of either voltage or pulse width is usually sufficient to regain capture.
Hypokalemia or hyperkalemia may alter the effects of Class I antiarrhythmic drugs. Preexisting hypokalemia or hyperkalemia should be corrected before administration of flecainide.
The safety and efficacy of flecainide in the fetus, infant, or child have not been established in double-blind, randomized, placebo-controlled trials. The proarrhythmic effects of flecainide as described previously, apply also to children. In pediatric patients with structural heart disease, flecainide has been associated with cardiac arrest and sudden death. Flecainide should be started in the hospital with rhythm monitoring. Any use of flecainide in children should be directly supervised by a cardiologist skilled in the treatment of arrhythmias in children.
Any use of flecainide in children should be directly supervised by a cardiologist skilled in the treatment of arrhythmias in children. Because of the evolving nature of information in this area, specialized literature should be consulted. Under six months of age, the initial starting dose of flecainide acetate in children is approximately 50 mg/M2 body surface area daily, divided into two or three equally spaced doses. Over six months of age, the initial starting dose may be increased to 100 mg/M2 per day. The maximum recommended dose is 200 mg/M2 per day. This dose should not be exceeded. In some children on higher doses, despite previously low plasma levels, the level has increased rapidly to far above therapeutic values while taking the same dose. Small changes in dose may also lead to disproportionate increases in plasma levels. Plasma trough (less than one hour pre-dose) flecainide levels and electrocardiograms should be obtained at presumed steady state (after at least five doses) either after initiation or change in flecainide dose, whether the dose was increased for lack of effectiveness, or increased growth of the patient. For the first year on therapy, whenever the patient is seen for reasons of clinical follow-up, it is suggested that a 12-lead electrocardiogram and plasma trough flecainide level are obtained. The usual therapeutic level of flecainide in children is 200 to 500 ng/mL. In some cases, levels as high as 800 ng/mL may be required for control.
In patients with severe renal impairment (creatinine clearance of 35 mL/min/1.73 square meters or less), the initial dosage should be 100 mg once daily (or 50 mg bid); when used in such patients, frequent plasma level monitoring is required to guide dosage adjustments (see
Based on theoretical considerations, rather than experimental data, the following suggestion is made: when transferring patients from another antiarrhythmic drug to flecainide allow at least two to four plasma half-lives to elapse for the drug being discontinued before starting flecainide at the usual dosage. In patients where withdrawal of a previous antiarrhythmic agent is likely to produce life-threatening arrhythmias, the physician should consider hospitalizing the patient.
When flecainide is given in the presence of amiodarone, reduce the usual flecainide dose by 50% and monitor the patient closely for adverse effects. Plasma level monitoring is strongly recommended to guide dosage with such combination therapy (see below).
Flecainide is contraindicated in patients with preexisting second- or third degree AV block, or with right bundle branch block when associated with a left hemiblock (bifascicular block), unless a pacemaker is present to sustain the cardiac rhythm should complete heart block occur. Flecainide is also contraindicated in the presence of cardiogenic shock or known hypersensitivity to the drug.
In post-myocardial infarction patients with asymptomatic PVCs and nonsustained ventricular tachycardia, flecainide therapy was found to be associated with a 5.1% rate of death and non-fatal cardiac arrest, compared with a 2.3% rate in a matched placebo group (see
Mortality Flecainide was included in the National Heart Lung and Blood Institute’s Cardiac Arrhythmia Suppression Trial (CAST), a long-term, multi center, randomized, double-blind study in patients with asymptomatic non-life-threatening ventricular arrhythmias who had a myocardial infarction more than six days, but less than two years previously. An excessive mortality or non-fatal cardiac arrest rate was seen in patients treated with flecainide compared with that seen in a carefully matched placebo-treated group. This rate was 16/315 (5.1%) for flecainide and 7/309 (2.3%) for the matched placebo. The average duration of treatment with flecainide in this study was 10 months. The applicability of the CAST results to other populations (e.g., those without recent myocardial infarction) is uncertain, but at present it is prudent to consider the risks of Class 1C agents (including flecainide), coupled with the lack of any evidence of improved survival, generally unacceptable in patients without life-threatening ventricular arrhythmias, even if the patients are experiencing unpleasant, but not life-threatening, symptoms or signs. Ventricular Proarrhythmic Effects in Patients with Atrial Fibrillation/Flutter A review of the world literature revealed reports of 568 patients treated with oral flecainide for paroxysmal atrial fibrillation/flutter (PAF). Ventricular tachycardia was experienced in 0.4% (2/568) of these patients. Of 19 patients in the literature with chronic atrial fibrillation (CAF), 10.5% (2) experienced VT or VF. FLECAINIDE IS NOT RECOMMENDED FOR USE IN PATIENTS WITH CHRONIC ATRIAL FIBRILLATION Case reports of ventricular proarrhythmic effects in patients treated with flecainide for atrial fibrillation/flutter have included increased PVCs, VT, ventricular fibrillation (VF) and death. As with other Class 1 agents, patients treated with flecainide for atrial flutter have been reported with 1:1 atrioventricular conduction due to slowing the atrial rate. A paradoxical increase in the ventricular rate also may occur in patients with atrial fibrillation who receive flecainide. Concomitant negative chronotropic therapy such as digoxin or beta-blockers may lower the risk of this complication. |
Flecainide slows cardiac conduction in most patients to produce dose-related increases in PR, QRS and QT intervals. PR interval increases on average about 25% (0.04 seconds) and as much as 118% in some patients. Approximately one-third of patients may develop new first-degree AV heart block (PR interval ≥0.20 seconds). The QRS complex increases on average about 25% (0.02 seconds) and as much as 150% in some patients. Many patients develop QRS complexes with a duration of 0.12 seconds or more. In one study, 4% of patients developed new bundle branch block while on flecainide. The degree of lengthening of PR and QRS intervals does not predict either efficacy or the development of cardiac adverse effects. In clinical trials, it was unusual for PR intervals to increase to 0.30 seconds or more, or for QRS intervals to increase to 0.18 seconds or more. Thus, caution should be used when such intervals occur, and dose reductions may be considered. The QT interval widens about 8%, but most of this widening (about 60% to 90%) is due to widening of the QRS duration. The JT interval (QT minus QRS) only widens about 4% on the average. Significant JT prolongation occurs in less than 2% of patients. There have been rare cases of Torsade de Pointes-type arrhythmia associated with flecainide therapy.
Clinically significant conduction changes have been observed at these rates: sinus node dysfunction such as sinus pause, sinus arrest and symptomatic bradycardia (1.2%), second degree AV block (0.5%) and third-degree AV block (0.4%). An attempt should be made to manage the patient on the lowest effective dose in an effort to minimize these effects (see
Flecainide should be used only with extreme caution in patients with sick sinus syndrome because it may cause sinus bradycardia, sinus pause, or sinus arrest.
Flecainide is known to increase endocardial pacing thresholds and may suppress ventricular escape rhythms. These effects are reversible if flecainide is discontinued. It should be used with caution in patients with permanent pacemakers or temporary pacing electrodes and should not be administered to patients with existing poor thresholds or nonprogrammable pacemakers unless suitable pacing rescue is available.
The pacing threshold in patients with pacemakers should be determined prior to instituting therapy with flecainide, again after one week of administration and at regular intervals thereafter. Generally, threshold changes are within the range of multiprogrammable pacemakers and, when these occur, a doubling of either voltage or pulse width is usually sufficient to regain capture.
Hypokalemia or hyperkalemia may alter the effects of Class I antiarrhythmic drugs. Preexisting hypokalemia or hyperkalemia should be corrected before administration of flecainide.
The safety and efficacy of flecainide in the fetus, infant, or child have not been established in double-blind, randomized, placebo-controlled trials. The proarrhythmic effects of flecainide as described previously, apply also to children. In pediatric patients with structural heart disease, flecainide has been associated with cardiac arrest and sudden death. Flecainide should be started in the hospital with rhythm monitoring. Any use of flecainide in children should be directly supervised by a cardiologist skilled in the treatment of arrhythmias in children.
Adverse effects reported for flecainide, described in detail in the
Mortality Flecainide was included in the National Heart Lung and Blood Institute’s Cardiac Arrhythmia Suppression Trial (CAST), a long-term, multi center, randomized, double-blind study in patients with asymptomatic non-life-threatening ventricular arrhythmias who had a myocardial infarction more than six days, but less than two years previously. An excessive mortality or non-fatal cardiac arrest rate was seen in patients treated with flecainide compared with that seen in a carefully matched placebo-treated group. This rate was 16/315 (5.1%) for flecainide and 7/309 (2.3%) for the matched placebo. The average duration of treatment with flecainide in this study was 10 months. The applicability of the CAST results to other populations (e.g., those without recent myocardial infarction) is uncertain, but at present it is prudent to consider the risks of Class 1C agents (including flecainide), coupled with the lack of any evidence of improved survival, generally unacceptable in patients without life-threatening ventricular arrhythmias, even if the patients are experiencing unpleasant, but not life-threatening, symptoms or signs. Ventricular Proarrhythmic Effects in Patients with Atrial Fibrillation/Flutter A review of the world literature revealed reports of 568 patients treated with oral flecainide for paroxysmal atrial fibrillation/flutter (PAF). Ventricular tachycardia was experienced in 0.4% (2/568) of these patients. Of 19 patients in the literature with chronic atrial fibrillation (CAF), 10.5% (2) experienced VT or VF. FLECAINIDE IS NOT RECOMMENDED FOR USE IN PATIENTS WITH CHRONIC ATRIAL FIBRILLATION Case reports of ventricular proarrhythmic effects in patients treated with flecainide for atrial fibrillation/flutter have included increased PVCs, VT, ventricular fibrillation (VF) and death. As with other Class 1 agents, patients treated with flecainide for atrial flutter have been reported with 1:1 atrioventricular conduction due to slowing the atrial rate. A paradoxical increase in the ventricular rate also may occur in patients with atrial fibrillation who receive flecainide. Concomitant negative chronotropic therapy such as digoxin or beta-blockers may lower the risk of this complication. |
Flecainide slows cardiac conduction in most patients to produce dose-related increases in PR, QRS and QT intervals. PR interval increases on average about 25% (0.04 seconds) and as much as 118% in some patients. Approximately one-third of patients may develop new first-degree AV heart block (PR interval ≥0.20 seconds). The QRS complex increases on average about 25% (0.02 seconds) and as much as 150% in some patients. Many patients develop QRS complexes with a duration of 0.12 seconds or more. In one study, 4% of patients developed new bundle branch block while on flecainide. The degree of lengthening of PR and QRS intervals does not predict either efficacy or the development of cardiac adverse effects. In clinical trials, it was unusual for PR intervals to increase to 0.30 seconds or more, or for QRS intervals to increase to 0.18 seconds or more. Thus, caution should be used when such intervals occur, and dose reductions may be considered. The QT interval widens about 8%, but most of this widening (about 60% to 90%) is due to widening of the QRS duration. The JT interval (QT minus QRS) only widens about 4% on the average. Significant JT prolongation occurs in less than 2% of patients. There have been rare cases of Torsade de Pointes-type arrhythmia associated with flecainide therapy.
Clinically significant conduction changes have been observed at these rates: sinus node dysfunction such as sinus pause, sinus arrest and symptomatic bradycardia (1.2%), second degree AV block (0.5%) and third-degree AV block (0.4%). An attempt should be made to manage the patient on the lowest effective dose in an effort to minimize these effects (see
Flecainide should be used only with extreme caution in patients with sick sinus syndrome because it may cause sinus bradycardia, sinus pause, or sinus arrest.
Flecainide is known to increase endocardial pacing thresholds and may suppress ventricular escape rhythms. These effects are reversible if flecainide is discontinued. It should be used with caution in patients with permanent pacemakers or temporary pacing electrodes and should not be administered to patients with existing poor thresholds or nonprogrammable pacemakers unless suitable pacing rescue is available.
The pacing threshold in patients with pacemakers should be determined prior to instituting therapy with flecainide, again after one week of administration and at regular intervals thereafter. Generally, threshold changes are within the range of multiprogrammable pacemakers and, when these occur, a doubling of either voltage or pulse width is usually sufficient to regain capture.
Hypokalemia or hyperkalemia may alter the effects of Class I antiarrhythmic drugs. Preexisting hypokalemia or hyperkalemia should be corrected before administration of flecainide.
The safety and efficacy of flecainide in the fetus, infant, or child have not been established in double-blind, randomized, placebo-controlled trials. The proarrhythmic effects of flecainide as described previously, apply also to children. In pediatric patients with structural heart disease, flecainide has been associated with cardiac arrest and sudden death. Flecainide should be started in the hospital with rhythm monitoring. Any use of flecainide in children should be directly supervised by a cardiologist skilled in the treatment of arrhythmias in children.
Mortality Flecainide was included in the National Heart Lung and Blood Institute’s Cardiac Arrhythmia Suppression Trial (CAST), a long-term, multi center, randomized, double-blind study in patients with asymptomatic non-life-threatening ventricular arrhythmias who had a myocardial infarction more than six days, but less than two years previously. An excessive mortality or non-fatal cardiac arrest rate was seen in patients treated with flecainide compared with that seen in a carefully matched placebo-treated group. This rate was 16/315 (5.1%) for flecainide and 7/309 (2.3%) for the matched placebo. The average duration of treatment with flecainide in this study was 10 months. The applicability of the CAST results to other populations (e.g., those without recent myocardial infarction) is uncertain, but at present it is prudent to consider the risks of Class 1C agents (including flecainide), coupled with the lack of any evidence of improved survival, generally unacceptable in patients without life-threatening ventricular arrhythmias, even if the patients are experiencing unpleasant, but not life-threatening, symptoms or signs. Ventricular Proarrhythmic Effects in Patients with Atrial Fibrillation/Flutter A review of the world literature revealed reports of 568 patients treated with oral flecainide for paroxysmal atrial fibrillation/flutter (PAF). Ventricular tachycardia was experienced in 0.4% (2/568) of these patients. Of 19 patients in the literature with chronic atrial fibrillation (CAF), 10.5% (2) experienced VT or VF. FLECAINIDE IS NOT RECOMMENDED FOR USE IN PATIENTS WITH CHRONIC ATRIAL FIBRILLATION Case reports of ventricular proarrhythmic effects in patients treated with flecainide for atrial fibrillation/flutter have included increased PVCs, VT, ventricular fibrillation (VF) and death. As with other Class 1 agents, patients treated with flecainide for atrial flutter have been reported with 1:1 atrioventricular conduction due to slowing the atrial rate. A paradoxical increase in the ventricular rate also may occur in patients with atrial fibrillation who receive flecainide. Concomitant negative chronotropic therapy such as digoxin or beta-blockers may lower the risk of this complication. |
Flecainide slows cardiac conduction in most patients to produce dose-related increases in PR, QRS and QT intervals. PR interval increases on average about 25% (0.04 seconds) and as much as 118% in some patients. Approximately one-third of patients may develop new first-degree AV heart block (PR interval ≥0.20 seconds). The QRS complex increases on average about 25% (0.02 seconds) and as much as 150% in some patients. Many patients develop QRS complexes with a duration of 0.12 seconds or more. In one study, 4% of patients developed new bundle branch block while on flecainide. The degree of lengthening of PR and QRS intervals does not predict either efficacy or the development of cardiac adverse effects. In clinical trials, it was unusual for PR intervals to increase to 0.30 seconds or more, or for QRS intervals to increase to 0.18 seconds or more. Thus, caution should be used when such intervals occur, and dose reductions may be considered. The QT interval widens about 8%, but most of this widening (about 60% to 90%) is due to widening of the QRS duration. The JT interval (QT minus QRS) only widens about 4% on the average. Significant JT prolongation occurs in less than 2% of patients. There have been rare cases of Torsade de Pointes-type arrhythmia associated with flecainide therapy.
Clinically significant conduction changes have been observed at these rates: sinus node dysfunction such as sinus pause, sinus arrest and symptomatic bradycardia (1.2%), second degree AV block (0.5%) and third-degree AV block (0.4%). An attempt should be made to manage the patient on the lowest effective dose in an effort to minimize these effects (see
Flecainide should be used only with extreme caution in patients with sick sinus syndrome because it may cause sinus bradycardia, sinus pause, or sinus arrest.
Flecainide is known to increase endocardial pacing thresholds and may suppress ventricular escape rhythms. These effects are reversible if flecainide is discontinued. It should be used with caution in patients with permanent pacemakers or temporary pacing electrodes and should not be administered to patients with existing poor thresholds or nonprogrammable pacemakers unless suitable pacing rescue is available.
The pacing threshold in patients with pacemakers should be determined prior to instituting therapy with flecainide, again after one week of administration and at regular intervals thereafter. Generally, threshold changes are within the range of multiprogrammable pacemakers and, when these occur, a doubling of either voltage or pulse width is usually sufficient to regain capture.
Hypokalemia or hyperkalemia may alter the effects of Class I antiarrhythmic drugs. Preexisting hypokalemia or hyperkalemia should be corrected before administration of flecainide.
The safety and efficacy of flecainide in the fetus, infant, or child have not been established in double-blind, randomized, placebo-controlled trials. The proarrhythmic effects of flecainide as described previously, apply also to children. In pediatric patients with structural heart disease, flecainide has been associated with cardiac arrest and sudden death. Flecainide should be started in the hospital with rhythm monitoring. Any use of flecainide in children should be directly supervised by a cardiologist skilled in the treatment of arrhythmias in children.
There have been rare reports of isolated elevations of serum alkaline phosphatase and isolated elevations of serum transaminase levels. These elevations have been asymptomatic and no cause and effect relationship with flecainide has been established. In foreign postmarketing surveillance studies, there have been rare reports of hepatic dysfunction including reports of cholestasis and hepatic failure, and extremely rare reports of blood dyscrasias. Although no cause and effect relationship has been established, it is advisable to discontinue flecainide in patients who develop unexplained jaundice or signs of hepatic dysfunction or blood dyscrasias in order to eliminate flecainide as the possible causative agent.
Incidence figures for other adverse effects in patients with ventricular arrhythmias are based on a multicenter efficacy study, utilizing starting doses of 200 mg/day with gradual upward titration to 400 mg/day. Patients were treated for an average of 4.7 months, with some receiving up to 22 months of therapy. In this trial, 5.4% of patients discontinued due to non-cardiac adverse effects.
Adverse Effect | Incidence All 429 Patients at Any Dose | Incidence by Dose During Upward Titration | ||
|---|---|---|---|---|
| 200 mg/Day (N=426) | 300 mg/Day (N=293) | 400 mg/Day (N=100) | ||
| Dizziness* | 18.9% | 11% | 10.6% | 13% |
| Visual Disturbances† | 15.9% | 5.4% | 12.3% | 18% |
| Dyspnea | 10.3% | 5.2% | 7.5% | 4% |
| Headache | 9.6% | 4.5% | 6.1% | 9% |
| Nausea | 8.9% | 4.9% | 4.8% | 6% |
| Fatigue | 7.7% | 4.5% | 4.4% | 3% |
| Palpitation | 6.1% | 3.5% | 2.4% | 7% |
| Chest Pain | 5.4% | 3.1% | 3.8% | 1% |
| Asthenia | 4.9% | 2.6% | 2% | 4% |
| Tremor | 4.7% | 2.4% | 3.4% | 2% |
| Constipation | 4.4% | 2.8% | 2.1% | 1% |
| Edema | 3.5% | 1.9% | 1.4% | 2% |
| Abdominal Pain | 3.3% | 1.9% | 2.4% | 1% |
* Dizziness includes reports of dizziness, lightheadedness, faintness, unsteadiness, near syncope, etc.
† Visual disturbance includes reports of blurred vision, difficulty in focusing, spots before eyes, etc.
The following additional adverse experiences, possibly related to flecainide therapy and occurring in 1% to less than 3% of patients, have been reported in acute and chronic studies:
The following additional adverse experiences, possibly related to flecainide, have been reported in less than 1% of patients:
For patients with supraventricular arrhythmias, the most commonly reported noncardiac adverse experiences remain consistent with those known for patients treated with flecainide for ventricular arrhythmias. Dizziness is possibly more frequent in PAF patients.
Flecainide acetate is an antiarrhythmic drug available in tablets of 50, 100, or 150 mg for oral administration.
Flecainide acetate is benzamide, N-(2-piperidinylmethyl)-2,5-bis(2,2,2-trifluoroethoxy)-, monoacetate. The structural formula is given below.
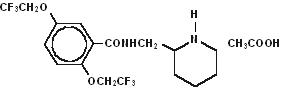
Molecular formula: C17H20F6N2O3•C2H4O2 Molecular weight: 474.40
Flecainide acetate, USP is a white crystalline substance with a pKa of 9.3. It has an aqueous solubility of 48.4 mg/mL at 37°C.
Flecainide acetate tablets, USP also contain the following inactive ingredients:
croscarmellose sodium, microcrystalline cellulose and magnesium stearate.
Flecainide has local anesthetic activity and belongs to the membrane stabilizing (Class 1) group of antiarrhythmic agents; it has electrophysiologic effects characteristic of the IC class of antiarrhythmics.
In man, flecainide produces a dose-related decrease in intracardiac conduction in all parts of the heart with the greatest effect on the His-Purkinje system (H-V conduction). Effects upon atrioventricular (AV) nodal conduction time and intra-atrial conduction times, although present, are less pronounced than those on ventricular conduction velocity. Significant effects on refractory periods were observed only in the ventricle. Sinus node recovery times (corrected) following pacing and spontaneous cycle lengths are somewhat increased. This latter effect may become significant in patients with sinus node dysfunction (see
Flecainide causes a dose-related and plasma-level related decrease in single and multiple PVCs and can suppress recurrence of ventricular tachycardia. In limited studies of patients with a history of ventricular tachycardia, flecainide has been successful 30% to 40% of the time in fully suppressing the inducibility of arrhythmias by programmed electrical stimulation. Based on PVC suppression, it appears that plasma levels of 0.2 to 1 mcg/mL may be needed to obtain the maximal therapeutic effect. It is more difficult to assess the dose needed to suppress serious arrhythmias, but trough plasma levels in patients successfully treated for recurrent ventricular tachycardia were between 0.2 and 1 mcg/mL. Plasma levels above 0.7 to 1 mcg/mL are associated with a higher rate of cardiac adverse experiences such as conduction defects or bradycardia. The relation of plasma levels to proarrhythmic events is not established, but dose reduction in clinical trials of patients with ventricular tachycardia appears to have led to a reduced frequency and severity of such events.
Flecainide does not usually alter heart rate, although bradycardia and tachycardia have been reported occasionally.
In animals and isolated myocardium, a negative inotropic effect of flecainide has been demonstrated. Decreases in ejection fraction, consistent with a negative inotropic effect, have been observed after single administration of 200 to 250 mg of the drug in man; both increases and decreases in ejection fraction have been encountered during multidose therapy in patients at usual therapeutic doses (see
Mortality Flecainide was included in the National Heart Lung and Blood Institute’s Cardiac Arrhythmia Suppression Trial (CAST), a long-term, multi center, randomized, double-blind study in patients with asymptomatic non-life-threatening ventricular arrhythmias who had a myocardial infarction more than six days, but less than two years previously. An excessive mortality or non-fatal cardiac arrest rate was seen in patients treated with flecainide compared with that seen in a carefully matched placebo-treated group. This rate was 16/315 (5.1%) for flecainide and 7/309 (2.3%) for the matched placebo. The average duration of treatment with flecainide in this study was 10 months. The applicability of the CAST results to other populations (e.g., those without recent myocardial infarction) is uncertain, but at present it is prudent to consider the risks of Class 1C agents (including flecainide), coupled with the lack of any evidence of improved survival, generally unacceptable in patients without life-threatening ventricular arrhythmias, even if the patients are experiencing unpleasant, but not life-threatening, symptoms or signs. Ventricular Proarrhythmic Effects in Patients with Atrial Fibrillation/Flutter A review of the world literature revealed reports of 568 patients treated with oral flecainide for paroxysmal atrial fibrillation/flutter (PAF). Ventricular tachycardia was experienced in 0.4% (2/568) of these patients. Of 19 patients in the literature with chronic atrial fibrillation (CAF), 10.5% (2) experienced VT or VF. FLECAINIDE IS NOT RECOMMENDED FOR USE IN PATIENTS WITH CHRONIC ATRIAL FIBRILLATION Case reports of ventricular proarrhythmic effects in patients treated with flecainide for atrial fibrillation/flutter have included increased PVCs, VT, ventricular fibrillation (VF) and death. As with other Class 1 agents, patients treated with flecainide for atrial flutter have been reported with 1:1 atrioventricular conduction due to slowing the atrial rate. A paradoxical increase in the ventricular rate also may occur in patients with atrial fibrillation who receive flecainide. Concomitant negative chronotropic therapy such as digoxin or beta-blockers may lower the risk of this complication. |
Flecainide slows cardiac conduction in most patients to produce dose-related increases in PR, QRS and QT intervals. PR interval increases on average about 25% (0.04 seconds) and as much as 118% in some patients. Approximately one-third of patients may develop new first-degree AV heart block (PR interval ≥0.20 seconds). The QRS complex increases on average about 25% (0.02 seconds) and as much as 150% in some patients. Many patients develop QRS complexes with a duration of 0.12 seconds or more. In one study, 4% of patients developed new bundle branch block while on flecainide. The degree of lengthening of PR and QRS intervals does not predict either efficacy or the development of cardiac adverse effects. In clinical trials, it was unusual for PR intervals to increase to 0.30 seconds or more, or for QRS intervals to increase to 0.18 seconds or more. Thus, caution should be used when such intervals occur, and dose reductions may be considered. The QT interval widens about 8%, but most of this widening (about 60% to 90%) is due to widening of the QRS duration. The JT interval (QT minus QRS) only widens about 4% on the average. Significant JT prolongation occurs in less than 2% of patients. There have been rare cases of Torsade de Pointes-type arrhythmia associated with flecainide therapy.
Clinically significant conduction changes have been observed at these rates: sinus node dysfunction such as sinus pause, sinus arrest and symptomatic bradycardia (1.2%), second degree AV block (0.5%) and third-degree AV block (0.4%). An attempt should be made to manage the patient on the lowest effective dose in an effort to minimize these effects (see
Flecainide should be used only with extreme caution in patients with sick sinus syndrome because it may cause sinus bradycardia, sinus pause, or sinus arrest.
Flecainide is known to increase endocardial pacing thresholds and may suppress ventricular escape rhythms. These effects are reversible if flecainide is discontinued. It should be used with caution in patients with permanent pacemakers or temporary pacing electrodes and should not be administered to patients with existing poor thresholds or nonprogrammable pacemakers unless suitable pacing rescue is available.
The pacing threshold in patients with pacemakers should be determined prior to instituting therapy with flecainide, again after one week of administration and at regular intervals thereafter. Generally, threshold changes are within the range of multiprogrammable pacemakers and, when these occur, a doubling of either voltage or pulse width is usually sufficient to regain capture.
Hypokalemia or hyperkalemia may alter the effects of Class I antiarrhythmic drugs. Preexisting hypokalemia or hyperkalemia should be corrected before administration of flecainide.
The safety and efficacy of flecainide in the fetus, infant, or child have not been established in double-blind, randomized, placebo-controlled trials. The proarrhythmic effects of flecainide as described previously, apply also to children. In pediatric patients with structural heart disease, flecainide has been associated with cardiac arrest and sudden death. Flecainide should be started in the hospital with rhythm monitoring. Any use of flecainide in children should be directly supervised by a cardiologist skilled in the treatment of arrhythmias in children.
Following oral administration, the absorption of flecainide is nearly complete. Peak plasma levels are attained at about three hours in most individuals (range, 1 to 6 hours). Flecainide does not undergo any consequential presystemic biotransformation (first-pass effect). Food or antacid do not affect absorption. Milk, however, may inhibit absorption in infants. A reduction in flecainide dosage should be considered when milk is removed from the diet of infants.
The apparent plasma half-life averages about 20 hours and is quite variable (range, 12 to 27 hours) after multiple oral doses in patients with premature ventricular contractions (PVCs). With multiple dosing, plasma levels increase because of its long half-life with steady-state levels approached in 3 to 5 days; once at steady-state, no additional (or unexpected) accumulation of drug in plasma occurs during chronic therapy. Over the usual therapeutic range, data suggest that plasma levels in an individual are approximately proportional to dose, deviating upwards from linearity only slightly (about 10% to 15% per 100 mg on average).
In healthy subjects, about 30% of a single oral dose (range, 10% to 50%) is excreted in urine as unchanged drug. The two major urinary metabolites are meta-0-dealkylated flecainide (active, but about one-fifth as potent) and the meta-0-dealkylated lactam of flecainide (non-active metabolite). These two metabolites (primarily conjugated) account for most of the remaining portion of the dose. Several minor metabolites (3% of the dose or less) are also found in urine; only 5% of an oral dose is excreted in feces. In patients, free (unconjugated) plasma levels of the two major metabolites are very low (less than 0.05 mcg/mL).
When urinary pH is very alkaline (8 or higher), as may occur in rare conditions (e.g., renal tubular acidosis, strict vegetarian diet), flecainide elimination from plasma is much slower.
The elimination of flecainide from the body depends on renal function (i.e., 10% to 50% appears in urine as unchanged drug). With increasing renal impairment, the extent of unchanged drug excretion in urine is reduced and the plasma half-life of flecainide is prolonged. Since flecainide is also extensively metabolized, there is no simple relationship between creatinine clearance and the rate of flecainide elimination from plasma (see
In patients with NYHA class III congestive heart failure (CHF), the rate of flecainide elimination from plasma (mean half-life, 19 hours) is moderately slower than for healthy subjects (mean half-life, 14 hours), but similar to the rate for patients with PVCs without CHF. The extent of excretion of unchanged drug in urine is also similar (see
Flecainide has a long half-life (12 to 27 hours in patients). Steady-state plasma levels, in patients with normal renal and hepatic function, may not be achieved until the patient has received 3 to 5 days of therapy at a given dose. Therefore,
For patients with PSVT and patients with PAF the recommended starting dose is 50 mg every 12 hours. Flecainide acetate doses may be increased in increments of 50 mg bid every four days until efficacy is achieved. For PAF patients, a substantial increase in efficacy without a substantial increase in discontinuations for adverse experiences may be achieved by increasing the flecainide acetate dose from 50 to 100 mg bid. The maximum recommended dose for patients with paroxysmal supraventricular arrhythmias is 300 mg/day.
For
In patients with
Intravenous lidocaine has been used occasionally with flecainide while awaiting the therapeutic effect of flecainide. No adverse drug interactions were apparent. However, no formal studies have been performed to demonstrate the usefulness of this regimen.
An occasional patient not adequately controlled by (or intolerant to) a dose given at 12-hour intervals may be dosed at eight-hour intervals.
Once adequate control of the arrhythmia has been achieved, it may be possible in some patients to reduce the dose as necessary to minimize side effects or effects on conduction. In such patients, efficacy at the lower dose should be evaluated.
Flecainide should be used cautiously in patients with a history of CHF or myocardial dysfunction (see
Any use of flecainide in children should be directly supervised by a cardiologist skilled in the treatment of arrhythmias in children. Because of the evolving nature of information in this area, specialized literature should be consulted. Under six months of age, the initial starting dose of flecainide acetate in children is approximately 50 mg/M2body surface area daily, divided into two or three equally spaced doses. Over six months of age, the initial starting dose may be increased to 100 mg/M2per day. The maximum recommended dose is 200 mg/M2per day. This dose should not be exceeded. In some children on higher doses, despite previously low plasma levels, the level has increased rapidly to far above therapeutic values while taking the same dose. Small changes in dose may also lead to disproportionate increases in plasma levels. Plasma trough (less than one hour pre-dose) flecainide levels and electrocardiograms should be obtained at presumed steady state (after at least five doses) either after initiation or change in flecainide dose, whether the dose was increased for lack of effectiveness, or increased growth of the patient. For the first year on therapy, whenever the patient is seen for reasons of clinical follow-up, it is suggested that a 12-lead electrocardiogram and plasma trough flecainide level are obtained. The usual therapeutic level of flecainide in children is 200 to 500 ng/mL. In some cases, levels as high as 800 ng/mL may be required for control.
In patients with severe renal impairment (creatinine clearance of 35 mL/min/1.73 square meters or less), the initial dosage should be 100 mg once daily (or 50 mg bid); when used in such patients, frequent plasma level monitoring is required to guide dosage adjustments (see
Based on theoretical considerations, rather than experimental data, the following suggestion is made: when transferring patients from another antiarrhythmic drug to flecainide allow at least two to four plasma half-lives to elapse for the drug being discontinued before starting flecainide at the usual dosage. In patients where withdrawal of a previous antiarrhythmic agent is likely to produce life-threatening arrhythmias, the physician should consider hospitalizing the patient.
When flecainide is given in the presence of amiodarone, reduce the usual flecainide dose by 50% and monitor the patient closely for adverse effects. Plasma level monitoring is strongly recommended to guide dosage with such combination therapy (see below).
The large majority of patients successfully treated with flecainide were found to have trough plasma levels between 0.2 and 1 mcg/mL. The probability of adverse experiences, especially cardiac, may increase with higher trough plasma levels, especially when these exceed 1 mcg/mL. Periodic monitoring of trough plasma levels may be useful in patient management. Plasma level monitoring is required in patients with severe renal failure or severe hepatic disease, since elimination of flecainide from plasma may be markedly slower. Monitoring of plasma levels is strongly recommended in patients on concurrent amiodarone therapy and may also be helpful in patients with CHF and in patients with moderate renal disease.
Under one year of age, current available data are limited but suggest that the half-life at birth may be as long as 29 hours, decreasing to 11 to 12 hours by three months of age and 6 hours by one year of age. The pharmacokinetics in hydropic infants have not been studied, but case reports suggest prolonged elimination. In children aged 1 year to 12 years the half-life is approximately 8 hours. In adolescents (age 12 to 15) the plasma elimination half-life is approximately 11 to 12 hours. Since milk may inhibit absorption in infants, a reduction in flecainide dosage should be considered when milk is removed from the diet (e.g., gastroenteritis, weaning). Plasma trough flecainide levels should be monitored during major changes in dietary milk intake.
From age 20 to 80, plasma levels are only slightly higher with advancing age; flecainide elimination from plasma is somewhat slower in elderly subjects than in younger subjects.
Patients up to age 80+ have been safely treated with usual dosages.
The extent of flecainide binding to human plasma proteins is about 40% and is independent of plasma drug level over the range of 0.015 to about 3.4 mcg/mL. Thus, clinically significant drug interactions based on protein binding effects would not be expected.
Hemodialysis removes only about 1% of an oral dose as unchanged flecainide.
Small increases in plasma digoxin levels are seen during coadministration of flecainide with digoxin. Small increases in both flecainide and propranolol plasma levels are seen during coadministration of these two drugs (see
In two randomized, crossover, placebo-controlled clinical trials of 16 weeks double-blind duration, 79% of patients with paroxysmal supraventricular tachycardia (PSVT) receiving flecainide were attack free, whereas 15% of patients receiving placebo remained attack free. The median time-before-recurrence of PSVT in patients receiving placebo was 11 to 12 days, whereas over 85% of patients receiving flecainide had no recurrence at 60 days.
In two randomized, crossover, placebo-controlled clinical trials of 16 weeks double-blind duration, 31% of patients with paroxysmal atrial fibrillation/flutter (PAF) receiving flecainide were attack free, whereas 8% receiving placebo remained attack free. The median time-before-recurrence of PAF in patients receiving placebo was about 2 to 3 days, whereas for those receiving flecainide the median time-before-recurrence was 15 days.