Fluocinolone Acetonide - Fluocinolone Acetonide cream
(Fluocinolone Acetonide)Fluocinolone Acetonide - Fluocinolone Acetonide cream Prescribing Information
Topical corticosteroids are indicated for the relief of the inflammatory and pruritic manifestations of corticosteroid-responsive dermatoses.
Topical corticosteroids are generally applied to the affected area as a thin film from two to four times daily depending on the severity of the condition. In hairy sites, the hair should be parted to allow direct contact with the lesion.
Occlusive dressings may be used for the management of psoriasis or recalcitrant conditions. Some plastic films may be flammable and due care should be exercised in their use. Similarly, caution should be employed when such films are used on children or left in their proximity, to avoid the possibility of accidental suffocation.
If an infection develops, the use of occlusive dressings should be discontinued and appropriate antimicrobial therapy instituted.
Topical corticosteroids are contraindicated in those patients with a history of hypersensitivity to any of the components of the preparation.
The following local adverse reactions are reported infrequently with topical corticosteroids, but may occur more frequently with the use of occlusive dressings. These reactions are listed in an approximate decreasing order of occurrence: Burning, Itching, Irritation, Dryness, Folliculitis, Hypertrichosis, Acneiform eruptions, Hypopigmentation, Perioral dermatitis, Allergic contact dermatitis, Maceration of the skin, Secondary infection, Skin atrophy, Striae and Miliaria.
The topical corticosteroids constitute a class of primarily synthetic steroids used as anti-inflammatory and anti-pruritic agents. Fluocinolone Acetonide is included in this class of synthetic corticosteroids.
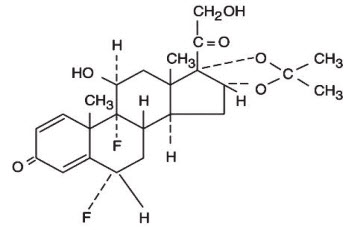
Chemically Fluocinolone Acetonide is Pregna-1,4-diene-3,20-dione, 6,9-difluoro-11,21-dihydroxy-16,17-[(1-methylethylidene)bis(oxy)]-, (6α, 11β, 6α)-), with the molecular formula C
24H
30F
20
6, a molecular weight of 452.49 and the following structural formula:
Each gram of Fluocinolone Acetonide Cream, USP 0.01% contains 0.1 mg fluocinolone acetonide USP in a water washable cream base consisting of mineral oil (and) lanolin alcohols, isopropyl palmitate NF, propylene glycol stearate, cetyl alcohol NF, sorbitan monostearate NF, polysorbate 60 NF, sorbic acid NF, polyoxyl (40) stearate NF, purified water USP, propylene glycol USP with propylparaben NF and methylparaben NF as preservatives.
Each gram of Fluocinolone Acetonide Ointment, USP 0.025% contains 0.25 mg of fluocinolone acetonide USP in an ointment base consisting of light mineral oil NF and white petrolatum USP.
Topical corticosteroids share anti-inflammatory, anti-pruritic and vasoconstrictive actions.
The mechanism of anti-inflammatory activity of the topical corticosteroids is unclear. Various laboratory methods, including vasoconstrictor assays, are used to compare and predict potencies and/or clinical efficacies of the topical corticosteroids. There is some evidence to suggest that a recognizable correlation exists between vasoconstrictor potency and therapeutic efficacy in man.
Topical corticosteroids can be absorbed from normal intact skin. Inflammation and/or other disease processes in the skin increase percutaneous absorption. Occlusive dressings substantially increase the percutaneous absorption of topical corticosteroids. Thus, occlusive dressings may be a valuable therapeutic adjunct for treatment of resistant dermatoses, (See
Topical corticosteroids are generally applied to the affected area as a thin film from two to four times daily depending on the severity of the condition. In hairy sites, the hair should be parted to allow direct contact with the lesion.
Occlusive dressings may be used for the management of psoriasis or recalcitrant conditions. Some plastic films may be flammable and due care should be exercised in their use. Similarly, caution should be employed when such films are used on children or left in their proximity, to avoid the possibility of accidental suffocation.
If an infection develops, the use of occlusive dressings should be discontinued and appropriate antimicrobial therapy instituted.
Once absorbed through the skin, topical corticosteroids are handled through pharmacokinetic pathways similar to systemically administered corticosteroids. Corticosteroids are bound to plasma proteins in varying degrees. Corticosteroids are metabolized primarily in the liver and are then excreted by the kidneys. Some of the topical corticosteroids and their metabolites are also excreted in the bile.