Fulvestrant
Fulvestrant Prescribing Information
Fulvestrant injection is indicated for the treatment of:
- Hormone receptor (HR)-positive, human epidermal growth factor receptor 2 (HER2)-negative advanced breast cancer in postmenopausal women not previously treated with endocrine therapy, or
- HR-positive advanced breast cancer in postmenopausal women with disease progression following endocrine therapy.
Fulvestrant injection is indicated for the treatment of:
- HR-positive, HER2-negative advanced or metastatic breast cancer in postmenopausal women in combination with ribociclib as initial endocrine based therapy or following disease progression on endocrine therapy.
- HR-positive, HER2-negative advanced or metastatic breast cancer in combination with palbociclib or abemaciclib in women with disease progression after endocrine therapy.
Fulvestrant injection, an injection for intramuscular administration, is supplied as 5-mL single-dose prefilled syringes containing 250 mg per 5 mL fulvestrant.
Fulvestrant is contraindicated in patients with a known hypersensitivity to the drug or to any of its components. Hypersensitivity reactions, including urticaria and angioedema, have been reported in association with fulvestrant
The following adverse reactions have been identified during post-approval use of fulvestrant. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
For fulvestrant 250 mg, other adverse reactions reported as drug-related and seen infrequently (<1%) include thromboembolic phenomena, myalgia, vertigo, leukopenia, and hypersensitivity reactions, including angioedema and urticaria.
Vaginal bleeding has been reported infrequently (<1%), mainly in patients during the first 6 weeks after changing from existing hormonal therapy to treatment with fulvestrant. If bleeding persists, further evaluation should be considered.
Elevation of bilirubin, elevation of gamma GT, hepatitis, and liver failure have been reported infrequently (<1%).
The following adverse reactions are discussed in more detail in other sections of the labeling:
- Risk of Bleeding [see]
5.1 Risk of BleedingBecause fulvestrant is administered intramuscularly, it should be used with caution in patients with bleeding diatheses, thrombocytopenia, or anticoagulant use.
- Increased Exposure in Patients with Hepatic Impairment [see]
5.2 Increased Exposure in Patients with Hepatic ImpairmentThe safety and pharmacokinetics of fulvestrant were evaluated in a study in seven subjects with moderate hepatic impairment (Child-Pugh class B) and seven subjects with normal hepatic function. Exposure was increased in patients with moderate hepatic impairment, therefore, a dose of 250 mg is recommended
[see Dosage and Administration (2.2)].Fulvestrant has not been studied in patients with severe hepatic impairment (Child-Pugh class C)
[see Use in Specific Populations (8.6)]. - Injection Site Reaction [see]
5.3 Injection Site ReactionInjection site related events including sciatica, neuralgia, neuropathic pain, and peripheral neuropathy have been reported with fulvestrant injection. Caution should be taken while administering fulvestrant at the dorsogluteal injection site due to the proximity of the underlying sciatic nerve
[see Dosage and Administration (2.3)and Adverse Reactions (6.1)]. - Embryo-Fetal Toxicity [see
5.4 Embryo-Fetal ToxicityBased on findings from animal studies and its mechanism of action, fulvestrant can cause fetal harm when administered to a pregnant woman. In animal reproduction studies, administration of fulvestrant to pregnant rats and rabbits during organogenesis resulted in embryo-fetal toxicity at daily doses that are significantly less than the maximum recommended human dose. Advise pregnant women of the potential risk to a fetus. Advise females of reproductive potential to use effective contraception during treatment with fulvestrant and for one year after the last dose
[see Use in Specific Populations (8.1), (8.3)and Clinical Pharmacology (12.1)].]
There are no known drug-drug interactions. Although, fulvestrant is metabolized by CYP 3A4
The single dose and multiple dose PK parameters for the 500 mg dosing regimen with an additional dose (AD) at Day 15 are reported in Table 11. The additional dose of fulvestrant given two weeks after the initial dose allows for steady state concentrations to be reached within the first month of dosing.
Cmax (ng/mL) | Cmin (ng/mL) | AUC (ng.hr/mL) | ||
|---|---|---|---|---|
500 mg + ADAdditional 500 mg dose given on Day 15 | Single dose | 25.1 (35.3) | 16.3 (25.9) | 11,400 (33.4) |
Multiple dose steady stateMonth 3 | 28 (27.9) | 12.2 (21.7) | 13,100 (23.4) | |
The apparent volume of distribution at steady state is approximately 3 to 5 L/kg. This suggests that distribution is largely extravascular. Fulvestrant is highly (99%) bound to plasma proteins; VLDL, LDL, and HDL lipoprotein fractions appear to be the major binding components. The role of sex hormone-binding globulin, if any, could not be determined.
Biotransformation and disposition of fulvestrant in humans have been determined following intramuscular and intravenous administration of14C-labeled fulvestrant. Metabolism of fulvestrant appears to involve combinations of a number of possible biotransformation pathways analogous to those of endogenous steroids, including oxidation, aromatic hydroxylation, conjugation with glucuronic acid and/or sulphate at the 2, 3, and 17 positions of the steroid nucleus, and oxidation of the side chain sulphoxide. Identified metabolites are either less active or exhibit similar activity to fulvestrant in antiestrogen models.
Studies using human liver preparations and recombinant human enzymes indicate that cytochrome P-450 3A4 (CYP 3A4) is the only P-450 isoenzyme involved in the oxidation of fulvestrant; however, the relative contribution of P-450 and non-P-450 routes
Fulvestrant was rapidly cleared by the hepatobiliary route with excretion primarily via the feces (approximately 90%). Renal elimination was negligible (less than 1%). After an intramuscular injection of 250 mg, the clearance (Mean ± SD) was 690 ± 226 mL/min with an apparent half-life about 40 days.
In patients with breast cancer, there was no difference in fulvestrant pharmacokinetic profile related to age (range 33 to 89 years).
Following administration of a single intravenous dose, there were no pharmacokinetic differences between men and women or between premenopausal and postmenopausal women. Similarly, there were no differences between men and postmenopausal women after intramuscular administration.
In the advanced breast cancer treatment trials, the potential for pharmacokinetic differences due to race have been evaluated in 294 women including 87.4% Caucasian, 7.8% Black, and 4.4% Hispanic. No differences in fulvestrant plasma pharmacokinetics were observed among these groups. In a separate trial, pharmacokinetic data from postmenopausal ethnic Japanese women were similar to those obtained in non-Japanese patients.
There are no known drug-drug interactions. Fulvestrant does not significantly inhibit any of the major CYP isoenzymes, including CYP 1A2, 2C9, 2C19, 2D6, and 3A4
Fulvestrant injection for intramuscular administration is an estrogen receptor antagonist. The chemical name is 7-alpha-[9-(4,4,5,5,5-penta fluoropentylsulphinyl) nonyl]estra-1,3,5-(10)- triene-3,17-beta-diol. The molecular formula is C32H47F5O3S and its structural formula is:
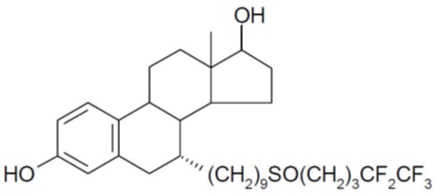
Fulvestrant is a white powder with a molecular weight of 606.77. The solution for injection is a sterile, clear, colorless to yellow, viscous liquid.
Each injection contains as inactive ingredients: 12% v/v alcohol, USP, 10% w/v benzyl alcohol, NF, and 15% w/v benzyl benzoate, USP, as co-solvents, and made up to 100% w/v with castor oil, USP as a co-solvent and release rate modifier.