Furosemide
Furosemide Prescribing Information
Parenteral therapy should be reserved for patients unable to take oral medication or for patients in emergency clinical situations.
Furosemide is indicated as adjunctive therapy in acute pulmonary edema. The intravenous administration of furosemide is indicated when a rapid onset of diuresis is desired, e.g., in acute pulmonary edema.
If gastrointestinal absorption is impaired or oral medication is not practical for any reason, furosemide is indicated by the intravenous or intramuscular route. Parenteral use should be replaced with oral furosemide as soon as practical.
Parenteral therapy with Furosemide Injection should be used only in patients unable to take oral medication or in emergency situations and should be replaced with oral therapy as soon as practical.
The usual initial dose of furosemide is 20 to 40 mg given as a single-dose, injected intramuscularly or intravenously. The intravenous dose should be given slowly (1 to 2 minutes). Ordinarily a prompt diuresis ensues. If needed, another dose may be administered in the same manner 2 hours later or the dose may be increased. The dose may be raised by 20 mg and given not sooner than 2 hours after the previous dose until the desired diuretic effect has been obtained. This individually determined single-dose should then be given once or twice daily.
Therapy should be individualized according to patient response to gain maximal therapeutic response and to determine the minimal dose needed to maintain that response. Close medical supervision is necessary.
When furosemide is given for prolonged periods, careful clinical observation and laboratory monitoring are particularly advisable (see
If the physician elects to use high dose parenteral therapy, add the furosemide to either Sodium Chloride Injection USP, Lactated Ringer's Injection USP, or Dextrose (5%) Injection USP after pH has been adjusted to above 5.5, and administer as a controlled intravenous infusion at a rate not greater than 4 mg/min. Furosemide Injection is a buffered alkaline solution with a pH of about 9 and drug may precipitate at pH values below 7. Care must be taken to ensure that the pH of the prepared infusion solution is in the weakly alkaline to neutral range. Acid solutions, including other parenteral medications (e.g., labetalol, ciprofloxacin, amrinone, milrinone) must not be administered concurrently in the same infusion because they may cause precipitation of the furosemide. In addition, furosemide injection should not be added to a running intravenous line containing any of these acidic products.
The usual initial dose of furosemide is 40 mg injected slowly intravenously (over 1 to 2 minutes). If a satisfactory response does not occur within 1 hour, the dose may be increased to 80 mg injected slowly intravenously (over 1 to 2 minutes).
If necessary, additional therapy (e.g., digitalis, oxygen) may be administered concomitantly.
In general, dose selection for the elderly patient should be cautious, usually starting at the low end of the dosing range (see
Parenteral therapy should be used only in patients unable to take oral medication or in emergency situations and should be replaced with oral therapy as soon as practical.
The usual initial dose of Furosemide Injection (intravenously or intramuscularly) in pediatric patients is 1 mg/kg body weight and should be given slowly under close medical supervision. If the diuretic response to the initial dose is not satisfactory, dosage may be increased by 1 mg/kg not sooner than 2 hours after the previous dose, until the desired diuretic effect has been obtained. Doses greater than 6 mg/kg body weight are not recommended.
Literature reports suggest that the maximum dose for premature infants should not exceed 1 mg/kg/day (see
Furosemide Injection should be inspected visually for particulate matter and discoloration before administration.
Furosemide is contraindicated in patients with anuria and in patients with a history of hypersensitivity to furosemide.
Adverse reactions are categorized below by organ system and listed by decreasing severity.
- Hepatic encephalopathy in patients with hepatocellular insufficiency
- Pancreatitis
- Jaundice (intrahepatic cholestatic jaundice)
- Increased liver enzymes
- Anorexia
- Oral and gastric irritation
- Cramping
- Diarrhea
- Constipation
- Nausea
- Vomiting
- Severe anaphylactic or anaphylactoid reactions (e.g. with shock)
- Systemic vasculitis
- Interstitial nephritis
- Necrotizing angiitis
- Tinnitus and hearing loss
- Paresthesias
- Vertigo
- Dizziness
- Headache
- Blurred vision
- Xanthopsia
- Aplastic anemia
- Thrombocytopenia
- Agranulocytosis
- Hemolytic anemia
- Leukopenia
- Anemia
- Eosinophilia
- Exfoliative dermatitis
- Bullous pemphigoid
- Erythema multiforme
- Purpura
- Photosensitivity
- Urticaria
- Rash
- Pruritus
- Stevens-Johnson Syndrome
- Toxic epidermal necrolysis
- Orthostatic hypotension may occur and be aggravated by alcohol, barbiturates or narcotics.
- Increase in cholesterol and triglyceride serum levels.
- Hyperglycemia
- Glycosuria
- Hyperuricemia
- Muscle spasms
- Weakness
- Restlessness
- Urinary bladder spasm
- Thrombophlebitis
- Transient injection site pain following intramuscular injection
- Fever
Whenever adverse reactions are moderate or severe, furosemide dosage should be reduced or therapy withdrawn.
Furosemide may increase the ototoxic potential of aminoglycoside antibiotics, especially in the presence of impaired renal function. Except in life-threatening situations, avoid this combination.
Furosemide should not be used concomitantly with ethacrynic acid because of the possibility of ototoxicity. Patients receiving high doses of salicylates concomitantly with furosemide, as in rheumatic diseases, may experience salicylate toxicity at lower doses because of competitive renal excretory sites.
There is a risk of ototoxic effects if cisplatin and furosemide are given concomitantly. In addition, nephrotoxicity of nephrotoxic drugs such as cisplatin may be enhanced if furosemide is not given in lower doses and with positive fluid balance when used to achieve forced diuresis during cisplatin treatment.
Furosemide has a tendency to antagonize the skeletal muscle relaxing effect of tubocurarine and may potentiate the action of succinylcholine.
Lithium generally should not be given with diuretics because they reduce lithium's renal clearance and add a high risk of lithium toxicity.
Furosemide combined with angiotensin converting enzyme inhibitors or angiotensin II receptor blockers may lead to severe hypotension and deterioration in renal function, including renal failure. An interruption or reduction in the dosage of furosemide, angiotensin converting enzyme inhibitors, or angiotensin receptor blockers may be necessary.
Furosemide may add to or potentiate the therapeutic effect of other antihypertensive drugs. Potentiation occurs with ganglionic or peripheral adrenergic blocking drugs.
Furosemide may decrease arterial responsiveness to norepinephrine. However, norepinephrine may still be used effectively.
In isolated cases, intravenous administration of furosemide within 24 hours of taking chloral hydrate may lead to flushing, sweating attacks, restlessness, nausea, increase in blood pressure and tachycardia. Use of furosemide concomitantly with chloral hydrate is therefore not recommended.
Phenytoin interferes directly with renal action of furosemide.
Methotrexate and other drugs that, like furosemide, undergo significant renal tubular secretion may reduce the effect of furosemide. Conversely, furosemide may decrease renal elimination of other drugs that undergo tubular secretion. High-dose treatment of both furosemide and these other drugs may result in elevated serum levels of these drugs and may potentiate their toxicity as well as the toxicity of furosemide.
Furosemide can increase the risk of cephalosporin-induced nephrotoxicity even in the setting of minor or transient renal impairment.
Concomitant use of cyclosporine and furosemide is associated with increased risk of gouty arthritis secondary to furosemide-induced hyperuricemia and cyclosporine impairment of renal urate excretion.
One study in six subjects demonstrated that the combination of furosemide and acetylsalicylic acid temporarily reduced creatinine clearance in patients with chronic renal insufficiency. There are case reports of patients who developed increased BUN, serum creatinine and serum potassium levels and weight gain when furosemide was used in conjunction with NSAIDs.
Literature reports indicate that co-administration of indomethacin may reduce the natriuretic and antihypertensive effects of furosemide in some patients by inhibiting prostaglandin synthesis. Indomethacin may also affect plasma renin levels, aldosterone excretion and renin profile evaluation. Patients receiving both indomethacin and furosemide should be observed closely to determine if the desired diuretic and/or antihypertensive effect of furosemide is achieved.
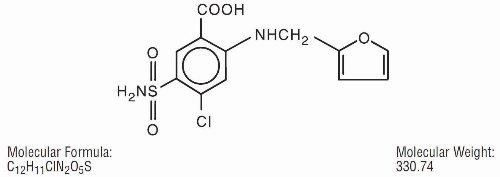
Furosemide is a diuretic which is an anthranilic acid derivative.
Chemically, it is 4-chloro-
Furosemide Injection, USP 10 mg/mL is a sterile, non-pyrogenic solution in vials for intravenous and intramuscular injection. Furosemide, USP is a white to slightly yellow, odorless, crystalline powder. It is practically insoluble in water; freely soluble in acetone, in dimethylformamide and in solutions of alkali hydroxides; soluble in methanol; sparingly soluble in alcohol; slightly soluble in ether; very slightly soluble in chloroform.
The structural formula is as follows:
Each mL contains: Furosemide, USP 10 mg, Sodium Hydroxide 1.3 mg, Water for Injection q.s., Sodium Chloride for isotonicity, additional Sodium Hydroxide (q.s.) and, if necessary, Hydrochloric Acid (q.s.) to adjust pH between 8.0 and 9.3.