Gabapentin
Gabapentin Prescribing Information
Warnings and Precautions (5.5, 5.6) 4/2025
Warnings and Precautions, removal-
Sudden and Unexplained Death in Patients with Epilepsy (5.10) 4/2025
Gabapentin Capsules, USP are indicated for:
- Management of postherpetic neuralgia in adults
- Adjunctive therapy in the treatment of partial onset seizures, with and without secondary generalization, in adults and pediatric patients 3 years and older with epilepsy
In adults with postherpetic neuralgia, gabapentin may be initiated on Day 1 as a single 300 mg dose, on Day 2 as 600 mg/day (300 mg two times a day), and on Day 3 as 900 mg/day (300 mg three times a day). The dose can subsequently be titrated up as needed for pain relief to a dose of 1800 mg/day (600 mg three times a day). In clinical studies, efficacy was demonstrated over a range of doses from 1800 mg/day to 3600 mg/day with comparable effects across the dose range; however, in these clinical studies, the additional benefit of using doses greater than 1800 mg/day was not demonstrated.
The starting dose is 300 mg three times a day. The recommended maintenance dose of gabapentin is 300 mg to 600 mg three times a day. Dosages up to 2400 mg/day have been administered in long-term clinical studies. Doses of 3600 mg/day have also been administered to a small number of patients for a relatively short duration. Administer gabapentin capsules three times a day using 300 mg or 400 mg capsules. The maximum time between doses should not exceed 12 hours.
The starting dose range is 10 mg/kg/day to 15 mg/kg/day, given in three divided doses, and the recommended maintenance dose reached by upward titration over a period of approximately 3 days. The recommended maintenance dose of gabapentin in patients 3 to 4 years of age is 40 mg/kg/day, given in three divided doses. The recommended maintenance dose of gabapentin in patients 5 to 11 years of age is 25 mg/kg/day to 35 mg/kg/day, given in three divided doses. Gabapentin may be administered as capsule. Dosages up to 50 mg/kg/day have been administered in a long-term clinical study. The maximum time interval between doses should not exceed 12 hours.
Dosage adjustment in patients 12 years of age and older with renal impairment or undergoing hemodialysis is recommended, as follows (see dosing recommendations above for effective doses in each indication):
| Renal Function Total Daily Dose Regimen Creatinine Clearance Dose Range (mg) (mL/min) (mg/day) | ||
| ≥ 60 > 30 to 59 >15 to 29 15a | 900 to 3600 400 to 1400 200 to 700 100 to 300 | 300 TID 400 TID 600 TID 800 TID 1200 TID 200 BID 300 BID 400 BID 500 BID 700 BID 200 QD 300 QD 400 QD 500 QD 700 QD 100 QD 125 QD 150 QD 200 QD 300 QD |
| Post-Hemodialysis Supplemental Dose (mg)b | ||
| Hemodialysis | | 125b 150b 200b 250b 350b |
TID = Three times a day; BID = Two times a day; QD = Single daily dose
a For patients with creatinine clearance <15 mL/min, reduce daily dose in proportion to creatinine clearance (e.g., patients with a creatinine clearance of 7.5 mL/min should receive one-half the daily dose that patients with a creatinine clearance of 15 mL/min receive).
b Patients on hemodialysis should receive maintenance doses based on estimates of creatinine clearance as indicated in the upper portion of the table and a supplemental post-hemodialysis dose administered after each 4 hours of hemodialysis as indicated in the lower portion of the table.
Creatinine clearance (CLCr) is difficult to measure in outpatients. In patients with stable renal function, creatinine clearance can be reasonably well estimated using the equation of Cockcroft and Gault: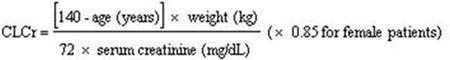
The use of gabapentin in patients less than 12 years of age with compromised renal function has not been studied.
Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and dose should be adjusted based on creatinine clearance values in these patients.
Administer gabapentin capsules orally with or without food.
Gabapentin capsules should be swallowed whole with water.
If the gabapentin dose is reduced, discontinued, or substituted with an alternative medication, this should be done gradually over a minimum of 1 week (a longer period may be needed at the discretion of the prescriber).
- 100 mg: white/white coloured size '3' hard gelatin capsules printed “103” on body of capsule containing white to off white granular powder
- 300 mg: yellow/yellow coloured size '1' hard gelatin capsules printed “104” on body of capsule containing white to off white granular powder
- 400 mg: orange/orange coloured size '0' hard gelatin capsules printed “105” on body of capsule containing white to off white granular powder
Pregnancy: Based on animal data, may cause fetal harm. (
There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to antiepileptic drugs (AEDs), such as Gabapentin, during pregnancy. Encourage women who are taking Gabapentin during pregnancy to enroll in the North American Antiepileptic Drug (NAAED) Pregnancy Registry by calling the toll free number 1-888-233-2334 or visiting http://www.aedpregnancyregistry.org/.
The totality of available data from published prospective and retrospective cohort studies pertaining to gabapentin use during pregnancy has not indicated an increased risk of major birth defects or miscarriage. There are important methodological limitations hindering interpretation of these studies [
Postmarketing data suggest that extended gabapentin use with opioids close to delivery may increase the risk of neonatal withdrawal versus opioids alone [
The background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Fetal/Neonatal Adverse Reactions
Neonatal withdrawal syndrome has been reported in newborns exposed to gabapentin in utero for an extended period of time when also exposed to opioids close to delivery. Neonatal withdrawal signs and symptoms reported have included tachypnea, vomiting, diarrhea, hypertonia, irritability, sneezing, poor feeding, hyperactivity, abnormal sleep pattern, and tremor. Reported signs and symptoms that may also be related to withdrawal include tongue thrusting, wandering eye movements while awake, back arching, and continuous extremity movements. Observe neonates exposed to gabapentin and opioids for signs and symptoms of neonatal withdrawal and manage accordingly.
An observational study based on routinely collected data from administrative and medical registers in Denmark, Finland, Norway, and Sweden, compared the prevalence of major congenital malformations in approximately 1,500 pregnancies exposed to gabapentin monotherapy in the first trimester to pregnancies unexposed to antiepileptics (n=2,995,816) and pregnancies exposed to lamotrigine monotherapy in the first trimester (n=7,582). The adjusted prevalence ratios in a pooled analysis were 1.00 (95% CI: 0.80-1.24) compared to pregnancies unexposed to antiepileptics and 1.29 (95% CI: 1.00-1.67) compared to pregnancies exposed to lamotrigine monotherapy in the first trimester.
Data from another observational study in the US based on Medicaid data, which compared the risk for major congenital malformations in more than 4,600 pregnancies exposed to gabapentin during the first trimester to unexposed pregnancies (n=1,753,865), estimated an adjusted relative risk of 1.07 (95% CI: 0.94-1.21).
Data from a cohort study of over 200,000 Medicaid-eligible pregnancies with prescription opioid exposure in the last 45 days of pregnancy found that the risk of neonatal drug withdrawal was greater in pregnancies with combined exposure to gabapentin and opioids compared to pregnancies with exposure to opioids alone.
The data from these observational studies should be interpreted with caution due to the potential for exposure misclassification, outcome misclassification, and residual confounding, including by underlying disease.
When pregnant mice received oral doses of gabapentin (500, 1000, or 3000 mg/kg/day) during the period of organogenesis, embryofetal toxicity (increased incidences of skeletal variations) was observed at the two highest doses. The no-effect dose for embryofetal developmental toxicity in mice (500 mg/kg/day) is less than the maximum recommended human dose (MRHD) of 3600 mg on a body surface area (mg/m2) basis.
In studies in which rats received oral doses of gabapentin (500 to 2000 mg/kg/day) during pregnancy, adverse effect on offspring development (increased incidences of hydroureter and/or hydronephrosis) were observed at all doses. The lowest dose tested is similar to the MRHD on a mg/m2basis.
When pregnant rabbits were treated with gabapentin during the period of organogenesis, an increase in embryofetal mortality was observed at all doses tested (60, 300, or 1500 mg/kg). The lowest dose tested is less than the MRHD on a mg/m2basis.
In a published study, gabapentin (400 mg/kg/day) was administered by intraperitoneal injection to neonatal mice during the first postnatal week, a period of synaptogenesis in rodents (corresponding to the last trimester of pregnancy in humans). Gabapentin caused a marked decrease in neuronal synapse formation in brains of intact mice and abnormal neuronal synapse formation in a mouse model of synaptic repair. Gabapentin has been shown
Gabapentin is contraindicated in patients who have demonstrated hypersensitivity to the drug or its ingredients.