Guanfacine
Guanfacine Prescribing Information
Guanfacine tablets, USP are indicated in the management of hypertension. Guanfacine tablets, USP may be given alone or in combination with other antihypertensive agents, especially thiazide-type diuretics.
The recommended initial dose of guanfacine tablets when given alone or in combination with another antihypertensive drug is 1 mg daily given at bedtime to minimize somnolence. If after 3 weeks to 4 weeks of therapy 1 mg does not give a satisfactory result, a dose of 2 mg may be given, although most of the effect of guanfacine tablets are seen at 1 mg (see
Guanfacine hydrochloride is an orally active antihypertensive agent whose principal mechanism of action appears to be stimulation of central α2-adrenergic receptors. By stimulating these receptors, guanfacine reduces sympathetic nerve impulses from the vasomotor center to the heart and blood vessels. This results in a decrease in peripheral vascular resistance and a reduction in heart rate.
The dose-response relationship for blood pressure and adverse effects of guanfacine given once a day as monotherapy has been evaluated in patients with mild to moderate hypertension. In this study patients were randomized to placebo or to 0.5 mg, 1 mg, 2 mg, 3 mg, or 5 mg of guanfacine tablets. Results are shown in the following table. A useful effect was not observed overall until doses of 2 mg were reached, although responses in white patients were seen at 1 mg; 24 hour effectiveness of 1 mg to 3 mg doses was documented using 24 hour ambulatory monitoring. While the 5 mg dose added an increment of effectiveness, it caused an unacceptable increase in adverse reactions.
| *S/D = Systolic/diastolic blood pressure | |||||||||||||||||||||||
Mean change S/D* Seated | n = (range) | Placebo | 0.5 mg | 1 mg | 2 mg | 3 mg | 5 mg | ||||||||||||||||
| White Patients | 11 to 30 | -1/-5 | -6/-8 | -8/-9 | -12/-11 | -15/-12 | -18/-16 | ||||||||||||||||
| Black Patients | 8 to 28 | -3/-5 | 0/-2 | -3/-5 | -7/-7 | -8/-9 | -19/-15 | ||||||||||||||||
Controlled clinical trials in patients with mild to moderate hypertension who were receiving a thiazide-type diuretic have defined the dose-response relationship for blood pressure response and adverse reactions of guanfacine given at bedtime and have shown that the blood pressure response to guanfacine can persist for 24 hours after a single dose. In the 12-week placebo-controlled dose-response study, patients were randomized to placebo or to doses of 0.5 mg, 1 mg, 2 mg, and 3 mg of guanfacine, in addition to 25 mg chlorthalidone, each given at bedtime. The observed mean changes from baseline, tabulated below, indicate the similarity of response for placebo and the 0.5 mg dose. Doses of 1 mg, 2 mg, and 3 mg resulted in decreased blood pressure in the sitting position with no real differences among the three doses. In the standing position, there was some increase in response with dose.
| *S/D = Systolic/diastolic blood pressure | ||||||||||||||||||||||||||
Mean Change | n = | Placebo 63 | 0.5 mg 63 | 1 mg 64 | 2 mg 58 | 3 mg 59 | ||||||||||||||||||||
| SD*Seated | -5/-7 | -5/-6 | -14/-13 | -12/-13 | -16/-13 | |||||||||||||||||||||
| SD Standing | -3/-5 | -5/-4 | -11/-9 | -9/-10 | -15/-12 | |||||||||||||||||||||
While most of the effectiveness of guanfacine in combination (and as monotherapy in white patients) was present at 1 mg, adverse reactions at this dose were not clearly distinguishable from those associated with placebo. Adverse reactions were clearly present at 2 mg and 3 mg (see
In a second 12-week placebo-controlled study of 1 mg, 2 mg or 3 mg of guanfacine hydrochloride administered with 25 mg of chlorthalidone once daily, a significant decrease in blood pressure was maintained for a full 24 hours after dosing. While there was no significant difference between the 12 hour and 24 hour blood pressure readings, the fall in blood pressure at 24 hours was numerically smaller, suggesting possible escape of blood pressure in some patients and the need for individualization of therapy.
In a double-blind, randomized trial, either guanfacine or clonidine was given at recommended doses with 25 mg chlorthalidone for 24 weeks and then abruptly discontinued. Results showed equal degrees of blood pressure reduction with the two drugs and there was no tendency for blood pressures to increase despite maintenance of the same daily dose of the two drugs. Signs and symptoms of rebound phenomena were infrequent upon discontinuation of either drug. Abrupt withdrawal of clonidine produced a rapid return of diastolic and especially systolic blood pressure to approximately pretreatment levels, with occasional values significantly greater than baseline, whereas guanfacine withdrawal produced a more gradual increase to pretreatment levels, but also with occasional values significantly greater than baseline.
Hemodynamic studies in man showed that the decrease in blood pressure observed after single-dose or long-term oral treatment with guanfacine was accompanied by a significant decrease in peripheral resistance and a slight reduction in heart rate (5 beats/min). Cardiac output under conditions of rest or exercise was not altered by guanfacine.
Guanfacine hydrochloride lowered elevated plasma renin activity and plasma catecholamine levels in hypertensive patients, but this does not correlate with individual blood-pressure responses.
Growth hormone secretion was stimulated with single oral doses of 2 mg and 4 mg of guanfacine. Long-term use of guanfacine tablets had no effect on growth hormone levels.
Guanfacine had no effect on plasma aldosterone. A slight but insignificant decrease in plasma volume occurred after one month of guanfacine therapy. There were no changes in mean body weight or electrolytes.
Relative to an intravenous dose of 3 mg, the absolute oral bioavailability of guanfacine is about 80 %. Peak plasma concentrations occur from 1 hour to 4 hours with an average of 2.6 hours after single oral doses or at steady state.
The area under the concentration-time curve (AUC) increases linearly with the dose.
In individuals with normal renal function, the average elimination half-life is approximately 17 hours (range 10 hours to 30 hours). Younger patients tend to have shorter elimination half-lives (13 hours to 14 hours) while older patients tend to have half-lives at the upper end of the range. Steady state blood levels were attained within 4 days in most subjects.
In individuals with normal renal function, guanfacine and its metabolites are excreted primarily in the urine. Approximately 50 % (40 % to 75 %) of the dose is eliminated in the urine as unchanged drug; the remainder is eliminated mostly as conjugates of metabolites produced by oxidative metabolism of the aromatic ring.
The guanfacine-to-creatinine clearance ratio is greater than 1.0, which would suggest that tubular secretion of drug occurs.
The drug is approximately 70 % bound to plasma proteins, independent of drug concentration.
The whole body volume of distribution is high (a mean of 6.3 L/kg), which suggests a high distribution of drug to the tissues.
The clearance of guanfacine in patients with varying degrees of renal insufficiency is reduced, but plasma levels of drug are only slightly increased compared to patients with normal renal function. When prescribing for patients with renal impairment, the low end of the dosing range should be used. Patients on dialysis also can be given usual doses of guanfacine hydrochloride as the drug is poorly dialyzed.
The frequency of rebound hypertension is low, but it can occur. When rebound occurs, it does so after 2 days to 4 days, which is delayed compared with clonidine hydrochloride. This is consistent with the longer half-life of guanfacine. In most cases, after abrupt withdrawal of guanfacine, blood pressure returns to pretreatment levels slowly (within 2 days to 4 days) without ill effects.
Guanfacine tablets are contraindicated in patients with known hypersensitivity to guanfacine hydrochloride.
Adverse reactions noted with guanfacine hydrochloride are similar to those of other drugs of the central α2-adrenoreceptor agonist class: dry mouth, sedation (somnolence), weakness (asthenia), dizziness, constipation, and impotence. While the reactions are common, most are mild and tend to disappear on continued dosing.
Skin rash with exfoliation has been reported in a few cases; although clear cause and effect relationships to guanfacine tablets could not be established, should a rash occur, guanfacine tablets should be discontinued and the patient monitored appropriately.
In the dose-response monotherapy study described under
Guanfacine hydrochloride is an orally active antihypertensive agent whose principal mechanism of action appears to be stimulation of central α2-adrenergic receptors. By stimulating these receptors, guanfacine reduces sympathetic nerve impulses from the vasomotor center to the heart and blood vessels. This results in a decrease in peripheral vascular resistance and a reduction in heart rate.
The dose-response relationship for blood pressure and adverse effects of guanfacine given once a day as monotherapy has been evaluated in patients with mild to moderate hypertension. In this study patients were randomized to placebo or to 0.5 mg, 1 mg, 2 mg, 3 mg, or 5 mg of guanfacine tablets. Results are shown in the following table. A useful effect was not observed overall until doses of 2 mg were reached, although responses in white patients were seen at 1 mg; 24 hour effectiveness of 1 mg to 3 mg doses was documented using 24 hour ambulatory monitoring. While the 5 mg dose added an increment of effectiveness, it caused an unacceptable increase in adverse reactions.
| *S/D = Systolic/diastolic blood pressure | |||||||||||||||||||||||
Mean change S/D* Seated | n = (range) | Placebo | 0.5 mg | 1 mg | 2 mg | 3 mg | 5 mg | ||||||||||||||||
| White Patients | 11 to 30 | -1/-5 | -6/-8 | -8/-9 | -12/-11 | -15/-12 | -18/-16 | ||||||||||||||||
| Black Patients | 8 to 28 | -3/-5 | 0/-2 | -3/-5 | -7/-7 | -8/-9 | -19/-15 | ||||||||||||||||
Controlled clinical trials in patients with mild to moderate hypertension who were receiving a thiazide-type diuretic have defined the dose-response relationship for blood pressure response and adverse reactions of guanfacine given at bedtime and have shown that the blood pressure response to guanfacine can persist for 24 hours after a single dose. In the 12-week placebo-controlled dose-response study, patients were randomized to placebo or to doses of 0.5 mg, 1 mg, 2 mg, and 3 mg of guanfacine, in addition to 25 mg chlorthalidone, each given at bedtime. The observed mean changes from baseline, tabulated below, indicate the similarity of response for placebo and the 0.5 mg dose. Doses of 1 mg, 2 mg, and 3 mg resulted in decreased blood pressure in the sitting position with no real differences among the three doses. In the standing position, there was some increase in response with dose.
| *S/D = Systolic/diastolic blood pressure | ||||||||||||||||||||||||||
Mean Change | n = | Placebo 63 | 0.5 mg 63 | 1 mg 64 | 2 mg 58 | 3 mg 59 | ||||||||||||||||||||
| SD*Seated | -5/-7 | -5/-6 | -14/-13 | -12/-13 | -16/-13 | |||||||||||||||||||||
| SD Standing | -3/-5 | -5/-4 | -11/-9 | -9/-10 | -15/-12 | |||||||||||||||||||||
While most of the effectiveness of guanfacine in combination (and as monotherapy in white patients) was present at 1 mg, adverse reactions at this dose were not clearly distinguishable from those associated with placebo. Adverse reactions were clearly present at 2 mg and 3 mg (see
In a second 12-week placebo-controlled study of 1 mg, 2 mg or 3 mg of guanfacine hydrochloride administered with 25 mg of chlorthalidone once daily, a significant decrease in blood pressure was maintained for a full 24 hours after dosing. While there was no significant difference between the 12 hour and 24 hour blood pressure readings, the fall in blood pressure at 24 hours was numerically smaller, suggesting possible escape of blood pressure in some patients and the need for individualization of therapy.
In a double-blind, randomized trial, either guanfacine or clonidine was given at recommended doses with 25 mg chlorthalidone for 24 weeks and then abruptly discontinued. Results showed equal degrees of blood pressure reduction with the two drugs and there was no tendency for blood pressures to increase despite maintenance of the same daily dose of the two drugs. Signs and symptoms of rebound phenomena were infrequent upon discontinuation of either drug. Abrupt withdrawal of clonidine produced a rapid return of diastolic and especially systolic blood pressure to approximately pretreatment levels, with occasional values significantly greater than baseline, whereas guanfacine withdrawal produced a more gradual increase to pretreatment levels, but also with occasional values significantly greater than baseline.
Hemodynamic studies in man showed that the decrease in blood pressure observed after single-dose or long-term oral treatment with guanfacine was accompanied by a significant decrease in peripheral resistance and a slight reduction in heart rate (5 beats/min). Cardiac output under conditions of rest or exercise was not altered by guanfacine.
Guanfacine hydrochloride lowered elevated plasma renin activity and plasma catecholamine levels in hypertensive patients, but this does not correlate with individual blood-pressure responses.
Growth hormone secretion was stimulated with single oral doses of 2 mg and 4 mg of guanfacine. Long-term use of guanfacine tablets had no effect on growth hormone levels.
Guanfacine had no effect on plasma aldosterone. A slight but insignificant decrease in plasma volume occurred after one month of guanfacine therapy. There were no changes in mean body weight or electrolytes.
Relative to an intravenous dose of 3 mg, the absolute oral bioavailability of guanfacine is about 80 %. Peak plasma concentrations occur from 1 hour to 4 hours with an average of 2.6 hours after single oral doses or at steady state.
The area under the concentration-time curve (AUC) increases linearly with the dose.
In individuals with normal renal function, the average elimination half-life is approximately 17 hours (range 10 hours to 30 hours). Younger patients tend to have shorter elimination half-lives (13 hours to 14 hours) while older patients tend to have half-lives at the upper end of the range. Steady state blood levels were attained within 4 days in most subjects.
In individuals with normal renal function, guanfacine and its metabolites are excreted primarily in the urine. Approximately 50 % (40 % to 75 %) of the dose is eliminated in the urine as unchanged drug; the remainder is eliminated mostly as conjugates of metabolites produced by oxidative metabolism of the aromatic ring.
The guanfacine-to-creatinine clearance ratio is greater than 1.0, which would suggest that tubular secretion of drug occurs.
The drug is approximately 70 % bound to plasma proteins, independent of drug concentration.
The whole body volume of distribution is high (a mean of 6.3 L/kg), which suggests a high distribution of drug to the tissues.
The clearance of guanfacine in patients with varying degrees of renal insufficiency is reduced, but plasma levels of drug are only slightly increased compared to patients with normal renal function. When prescribing for patients with renal impairment, the low end of the dosing range should be used. Patients on dialysis also can be given usual doses of guanfacine hydrochloride as the drug is poorly dialyzed.
| Adverse Reaction | Placebo n = 59 | 0.5 mg n = 60 | 1 mg n = 61 | 2 mg n = 60 | 3 mg n = 59 |
| Dry Mouth | 0 % | 10 % | 10 % | 42 % | 54 % |
| Somnolence | 8 % | 5 % | 10 % | 13 % | 39 % |
| Asthenia | 0 % | 2 % | 3 % | 7 % | 3 % |
| Dizziness | 8 % | 12 % | 2 % | 8 % | 15 % |
| Headache | 8 % | 13 % | 7 % | 5 % | 3 % |
| Impotence | 0 % | 0 % | 0 % | 7 % | 3 % |
| Constipation | 0 % | 2 % | 0 % | 5 % | 15 % |
| Fatigue | 2 % | 2 % | 5 % | 8 % | 10 % |
The percent of patients who dropped out because of adverse reactions are shown below for each dosage group.
| | Placebo | 0.5 mg | 1 mg | 2 mg | 3 mg |
| Percent dropouts | 0 % | 2.0 % | 5.0 % | 13 % | 32 % |
The most common reasons for dropouts among patients who received guanfacine were dry mouth, somnolence, dizziness, fatigue, weakness, and constipation.
In the 12-week, placebo-controlled, dose-response study of guanfacine administered with 25 mg chlorthalidone at bedtime, the frequency of the most commonly observed adverse reactions showed a clear dose relationship from 0.5 mg to 3 mg as follows:
| Adverse Reaction | Placebo n = 73 | 0.5 mg n = 72 | 1 mg n = 72 | 2 mg n = 72 | 3 mg n = 72 |
| Dry Mouth | 5 (7 %) | 4 (5 %) | 6 (8 %) | 8 (11 %) | 20 (28 %) |
| Somnolence | 1 (1 %) | 3 (4 %) | 0 (0 %) | 1 (1 %) | 10 (14 %) |
| Asthenia | 0 (0 %) | 2 (3 %) | 0 (0 %) | 2 (2 %) | 7 (10 %) |
| Dizziness | 2 (2 %) | 1 (1 %) | 3 (4 %) | 6 (8 %) | 3 (4 %) |
| Headache | 3 (4 %) | 4 (3 %) | 3 (4 %) | 1 (1 %) | 2 (2 %) |
| Impotence | 1 (1 %) | 1 (0 %) | 0 (0 %) | 1 (1 %) | 3 (4 %) |
| Constipation | 0 (0 %) | 0 (0 %) | 0 (0 %) | 1 (1 %) | 1 (1 %) |
| Fatigue | 3 (3 %) | 2 (3 %) | 2 (3 %) | 5 (6 %) | 3 (4 %) |
There were 41 premature terminations because of adverse reactions in this study. The percent of patients who dropped out and the dose at which the dropout occurred were as follows:
| Dose | Placebo | 0.5 mg | 1 mg | 2 mg | 3 mg |
| Percent dropouts | 6.9 % | 4.2 % | 3.2 % | 6.9 % | 8.3 % |
Reasons for dropouts among patients who received guanfacine were: somnolence, headache, weakness, dry mouth, dizziness, impotence, insomnia, constipation, syncope, urinary incontinence, conjunctivitis, paresthesia, and dermatitis.
In a second 12-week placebo-controlled combination therapy study in which the dose could be adjusted upward to 3 mg per day in 1-mg increments at 3-week intervals, i.e., a setting more similar to ordinary clinical use, the most commonly recorded reactions were: dry mouth, 47 %; constipation, 16 %; fatigue, 12 %; somnolence, 10 %; asthenia, 6 %; dizziness, 6 %; headache, 4 %; and insomnia, 4 %.
Reasons for dropouts among patients who received guanfacine were: somnolence, dry mouth, dizziness, impotence, constipation, confusion, depression, and palpitations.
In the clonidine/guanfacine comparison described in
Guanfacine hydrochloride is an orally active antihypertensive agent whose principal mechanism of action appears to be stimulation of central α2-adrenergic receptors. By stimulating these receptors, guanfacine reduces sympathetic nerve impulses from the vasomotor center to the heart and blood vessels. This results in a decrease in peripheral vascular resistance and a reduction in heart rate.
The dose-response relationship for blood pressure and adverse effects of guanfacine given once a day as monotherapy has been evaluated in patients with mild to moderate hypertension. In this study patients were randomized to placebo or to 0.5 mg, 1 mg, 2 mg, 3 mg, or 5 mg of guanfacine tablets. Results are shown in the following table. A useful effect was not observed overall until doses of 2 mg were reached, although responses in white patients were seen at 1 mg; 24 hour effectiveness of 1 mg to 3 mg doses was documented using 24 hour ambulatory monitoring. While the 5 mg dose added an increment of effectiveness, it caused an unacceptable increase in adverse reactions.
| *S/D = Systolic/diastolic blood pressure | |||||||||||||||||||||||
Mean change S/D* Seated | n = (range) | Placebo | 0.5 mg | 1 mg | 2 mg | 3 mg | 5 mg | ||||||||||||||||
| White Patients | 11 to 30 | -1/-5 | -6/-8 | -8/-9 | -12/-11 | -15/-12 | -18/-16 | ||||||||||||||||
| Black Patients | 8 to 28 | -3/-5 | 0/-2 | -3/-5 | -7/-7 | -8/-9 | -19/-15 | ||||||||||||||||
Controlled clinical trials in patients with mild to moderate hypertension who were receiving a thiazide-type diuretic have defined the dose-response relationship for blood pressure response and adverse reactions of guanfacine given at bedtime and have shown that the blood pressure response to guanfacine can persist for 24 hours after a single dose. In the 12-week placebo-controlled dose-response study, patients were randomized to placebo or to doses of 0.5 mg, 1 mg, 2 mg, and 3 mg of guanfacine, in addition to 25 mg chlorthalidone, each given at bedtime. The observed mean changes from baseline, tabulated below, indicate the similarity of response for placebo and the 0.5 mg dose. Doses of 1 mg, 2 mg, and 3 mg resulted in decreased blood pressure in the sitting position with no real differences among the three doses. In the standing position, there was some increase in response with dose.
| *S/D = Systolic/diastolic blood pressure | ||||||||||||||||||||||||||
Mean Change | n = | Placebo 63 | 0.5 mg 63 | 1 mg 64 | 2 mg 58 | 3 mg 59 | ||||||||||||||||||||
| SD*Seated | -5/-7 | -5/-6 | -14/-13 | -12/-13 | -16/-13 | |||||||||||||||||||||
| SD Standing | -3/-5 | -5/-4 | -11/-9 | -9/-10 | -15/-12 | |||||||||||||||||||||
While most of the effectiveness of guanfacine in combination (and as monotherapy in white patients) was present at 1 mg, adverse reactions at this dose were not clearly distinguishable from those associated with placebo. Adverse reactions were clearly present at 2 mg and 3 mg (see
In a second 12-week placebo-controlled study of 1 mg, 2 mg or 3 mg of guanfacine hydrochloride administered with 25 mg of chlorthalidone once daily, a significant decrease in blood pressure was maintained for a full 24 hours after dosing. While there was no significant difference between the 12 hour and 24 hour blood pressure readings, the fall in blood pressure at 24 hours was numerically smaller, suggesting possible escape of blood pressure in some patients and the need for individualization of therapy.
In a double-blind, randomized trial, either guanfacine or clonidine was given at recommended doses with 25 mg chlorthalidone for 24 weeks and then abruptly discontinued. Results showed equal degrees of blood pressure reduction with the two drugs and there was no tendency for blood pressures to increase despite maintenance of the same daily dose of the two drugs. Signs and symptoms of rebound phenomena were infrequent upon discontinuation of either drug. Abrupt withdrawal of clonidine produced a rapid return of diastolic and especially systolic blood pressure to approximately pretreatment levels, with occasional values significantly greater than baseline, whereas guanfacine withdrawal produced a more gradual increase to pretreatment levels, but also with occasional values significantly greater than baseline.
Hemodynamic studies in man showed that the decrease in blood pressure observed after single-dose or long-term oral treatment with guanfacine was accompanied by a significant decrease in peripheral resistance and a slight reduction in heart rate (5 beats/min). Cardiac output under conditions of rest or exercise was not altered by guanfacine.
Guanfacine hydrochloride lowered elevated plasma renin activity and plasma catecholamine levels in hypertensive patients, but this does not correlate with individual blood-pressure responses.
Growth hormone secretion was stimulated with single oral doses of 2 mg and 4 mg of guanfacine. Long-term use of guanfacine tablets had no effect on growth hormone levels.
Guanfacine had no effect on plasma aldosterone. A slight but insignificant decrease in plasma volume occurred after one month of guanfacine therapy. There were no changes in mean body weight or electrolytes.
Relative to an intravenous dose of 3 mg, the absolute oral bioavailability of guanfacine is about 80 %. Peak plasma concentrations occur from 1 hour to 4 hours with an average of 2.6 hours after single oral doses or at steady state.
The area under the concentration-time curve (AUC) increases linearly with the dose.
In individuals with normal renal function, the average elimination half-life is approximately 17 hours (range 10 hours to 30 hours). Younger patients tend to have shorter elimination half-lives (13 hours to 14 hours) while older patients tend to have half-lives at the upper end of the range. Steady state blood levels were attained within 4 days in most subjects.
In individuals with normal renal function, guanfacine and its metabolites are excreted primarily in the urine. Approximately 50 % (40 % to 75 %) of the dose is eliminated in the urine as unchanged drug; the remainder is eliminated mostly as conjugates of metabolites produced by oxidative metabolism of the aromatic ring.
The guanfacine-to-creatinine clearance ratio is greater than 1.0, which would suggest that tubular secretion of drug occurs.
The drug is approximately 70 % bound to plasma proteins, independent of drug concentration.
The whole body volume of distribution is high (a mean of 6.3 L/kg), which suggests a high distribution of drug to the tissues.
The clearance of guanfacine in patients with varying degrees of renal insufficiency is reduced, but plasma levels of drug are only slightly increased compared to patients with normal renal function. When prescribing for patients with renal impairment, the low end of the dosing range should be used. Patients on dialysis also can be given usual doses of guanfacine hydrochloride as the drug is poorly dialyzed.
| Adverse Reactions | Guanfacine (n = 279) | Clonidine (n = 278) |
| Dry Mouth | 30 % | 37 % |
| Somnolence | 21 % | 35 % |
| Dizziness | 11 % | 8 % |
| Constipation | 10 % | 5 % |
| Fatigue | 9 % | 8 % |
| Headache | 4 % | 4 % |
| Insomnia | 4 % | 3 % |
Adverse reactions occurring in 3 % or less of patients in the three controlled trials of guanfacine hydrochloride with a diuretic were:
Cardiovascular- bradycardia, palpitations, substernal pain
Gastrointestinal- abdominal pain, diarrhea, dyspepsia, dysphagia, nausea
CNS- amnesia, confusion, depression, insomnia, libido decrease
ENT disorders- rhinitis, taste perversion, tinnitus
Eye disorders- conjunctivitis, iritis, vision disturbance
Musculoskeletal- leg cramps, hypokinesia
Respiratory- dyspnea
Dermatologic- dermatitis, pruritus, purpura, sweating
Urogenital- testicular disorder, urinary incontinence
Other- malaise, paresthesia, paresis
Adverse reaction reports tend to decrease over time. In an open-label trial of one year's duration, 580 hypertensive subjects were given guanfacine, titrated to achieve goal blood pressure, alone (51 %), with diuretic (38 %), with beta blocker (3 %), with diuretic plus beta blocker (6 %), or with diuretic plus vasodilator (2 %). The mean daily dose of guanfacine reached was 4.7 mg.
| Adverse Reaction | Incidence of adverse reactions at any time during the study n = 580 | Incidence of adverse reactions at end of one year n = 580 |
| Dry Mouth | 60 % | 15 % |
| Drowsiness | 33 % | 6 % |
| Dizziness | 15 % | 1 % |
| Constipation | 14 % | 3 % |
| Weakness | 5 % | 1 % |
| Headache | 4 % | 0.2 % |
| Insomnia | 5 % | 0 % |
There were 52 (8.9 %) dropouts due to adverse effects in this 1-year trial. The causes were: dry mouth (n = 20), weakness (n = 12), constipation (n = 7), somnolence (n = 3), nausea (n = 3), orthostatic hypotension (n = 2), insomnia (n = 1), rash (n = 1), nightmares (n = 1), headache (n = 1), and depression (n = 1).
An open-label postmarketing study involving 21,718 patients was conducted to assess the safety of guanfacine hydrochloride 1 mg/day given at bedtime for 28 days. Guanfacine tablets were administered with or without other antihypertensive agents. Adverse events reported in the postmarketing study at an incidence greater than 1 % included dry mouth, dizziness, somnolence, fatigue, headache and nausea. The most commonly reported adverse events in this study were the same as those observed in controlled clinical trials.
Less frequent, possibly guanfacine tablets-related events observed in the postmarketing study and/or reported spontaneously include:
BODY AS A WHOLE asthenia, chest pain, edema, malaise, tremor
CARDIOVASCULAR bradycardia, palpitations, syncope, tachycardia
CENTRAL NERVOUS SYSTEM paresthesias, vertigo
EYE DISORDERS blurred vision
GASTROINTESTINAL SYSTEM abdominal pain, constipation, diarrhea, dyspepsia
LIVER AND BILLIARY SYSTEM abnormal liver function tests
MUSCULO-SKELETAL SYSTEM arthralgia, leg cramps, leg pain, myalgia
PSYCHIATRIC agitation, anxiety, confusion, depression, insomnia, nervousness
REPRODUCTIVE SYSTEM, Male- impotence
RESPIRATORY SYSTEM dyspnea
SKIN AND APPENDAGES alopecia, dermatitis, exfoliative dermatitis, pruritus, rash
SPECIAL SENSES alterations in taste
URINARY SYSTEM nocturia, urinary frequency
Rare, serious disorders with no definitive cause and effect relationship to guanfacine tablets have been reported spontaneously and/or in the postmarketing study. These events include acute renal failure, cardiac fibrillation, cerebrovascular accident, congestive heart failure, heart block, and myocardial infarction.
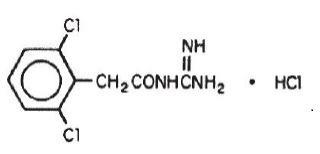
Guanfacine hydrochloride, USP is a centrally acting antihypertensive with α2-adrenoceptor agonist properties in tablet form for oral administration.
The chemical name of guanfacine hydrochloride, USP is
Guanfacine hydrochloride, USP is a white to off-white powder; sparingly soluble in water and alcohol and very slightly soluble in acetone. The tablets contain the following inactive ingredients:
1 mg—Anhydrous citric acid, microcrystalline cellulose, pregelatinized starch, stearic acid.
2 mg—Anhydrous citric acid, microcrystalline cellulose, pregelatinized starch, stearic acid.
Guanfacine tablets meets USP Dissolution Test 2.
Guanfacine hydrochloride is an orally active antihypertensive agent whose principal mechanism of action appears to be stimulation of central α2-adrenergic receptors. By stimulating these receptors, guanfacine reduces sympathetic nerve impulses from the vasomotor center to the heart and blood vessels. This results in a decrease in peripheral vascular resistance and a reduction in heart rate.
The dose-response relationship for blood pressure and adverse effects of guanfacine given once a day as monotherapy has been evaluated in patients with mild to moderate hypertension. In this study patients were randomized to placebo or to 0.5 mg, 1 mg, 2 mg, 3 mg, or 5 mg of guanfacine tablets. Results are shown in the following table. A useful effect was not observed overall until doses of 2 mg were reached, although responses in white patients were seen at 1 mg; 24 hour effectiveness of 1 mg to 3 mg doses was documented using 24 hour ambulatory monitoring. While the 5 mg dose added an increment of effectiveness, it caused an unacceptable increase in adverse reactions.
| * S/D = Systolic/diastolic blood pressure | |||||||||||||||||||||||
| Mean change S/D* Seated | n = (range) | Placebo | 0.5 mg | 1 mg | 2 mg | 3 mg | 5 mg | ||||||||||||||||
| White Patients | 11 to 30 | -1/-5 | -6/-8 | -8/-9 | -12/-11 | -15/-12 | -18/-16 | ||||||||||||||||
| Black Patients | 8 to 28 | -3/-5 | 0/-2 | -3/-5 | -7/-7 | -8/-9 | -19/-15 | ||||||||||||||||
Controlled clinical trials in patients with mild to moderate hypertension who were receiving a thiazide-type diuretic have defined the dose-response relationship for blood pressure response and adverse reactions of guanfacine given at bedtime and have shown that the blood pressure response to guanfacine can persist for 24 hours after a single dose. In the 12-week placebo-controlled dose-response study, patients were randomized to placebo or to doses of 0.5 mg, 1 mg, 2 mg, and 3 mg of guanfacine, in addition to 25 mg chlorthalidone, each given at bedtime. The observed mean changes from baseline, tabulated below, indicate the similarity of response for placebo and the 0.5 mg dose. Doses of 1 mg, 2 mg, and 3 mg resulted in decreased blood pressure in the sitting position with no real differences among the three doses. In the standing position, there was some increase in response with dose.
| * S/D = Systolic/diastolic blood pressure | ||||||||||||||||||||||||||
| Mean Change | n = | Placebo 63 | 0.5 mg 63 | 1 mg 64 | 2 mg 58 | 3 mg 59 | ||||||||||||||||||||
| SD* Seated | | -5/-7 | -5/-6 | -14/-13 | -12/-13 | -16/-13 | ||||||||||||||||||||
| SD Standing | -3/-5 | -5/-4 | -11/-9 | -9/-10 | -15/-12 | |||||||||||||||||||||
While most of the effectiveness of guanfacine in combination (and as monotherapy in white patients) was present at 1 mg, adverse reactions at this dose were not clearly distinguishable from those associated with placebo. Adverse reactions were clearly present at 2 mg and 3 mg (see
Adverse reactions noted with guanfacine hydrochloride are similar to those of other drugs of the central α2-adrenoreceptor agonist class: dry mouth, sedation (somnolence), weakness (asthenia), dizziness, constipation, and impotence. While the reactions are common, most are mild and tend to disappear on continued dosing.
Skin rash with exfoliation has been reported in a few cases; although clear cause and effect relationships to guanfacine tablets could not be established, should a rash occur, guanfacine tablets should be discontinued and the patient monitored appropriately.
In the dose-response monotherapy study described under
Adverse Reaction | Placebo n = 59 | 0.5 mg n = 60 | 1 mg n = 61 | 2 mg n = 60 | 3 mg n = 59 |
| Dry Mouth | 0 % | 10 % | 10 % | 42 % | 54 % |
| Somnolence | 8 % | 5 % | 10 % | 13 % | 39 % |
| Asthenia | 0 % | 2 % | 3 % | 7 % | 3 % |
| Dizziness | 8 % | 12 % | 2 % | 8 % | 15 % |
| Headache | 8 % | 13 % | 7 % | 5 % | 3 % |
| Impotence | 0 % | 0 % | 0 % | 7 % | 3 % |
| Constipation | 0 % | 2 % | 0 % | 5 % | 15 % |
| Fatigue | 2 % | 2 % | 5 % | 8 % | 10 % |
The percent of patients who dropped out because of adverse reactions are shown below for each dosage group.
Placebo | 0.5 mg | 1 mg | 2 mg | 3 mg | |
| Percent dropouts | 0 % | 2.0 % | 5.0 % | 13 % | 32 % |
The most common reasons for dropouts among patients who received guanfacine were dry mouth, somnolence, dizziness, fatigue, weakness, and constipation.
In the 12-week, placebo-controlled, dose-response study of guanfacine administered with 25 mg chlorthalidone at bedtime, the frequency of the most commonly observed adverse reactions showed a clear dose relationship from 0.5 mg to 3 mg as follows:
Adverse Reaction | Placebo n = 73 | 0.5 mg n = 72 | 1 mg n = 72 | 2 mg n = 72 | 3 mg n = 72 |
| Dry Mouth | 5 (7 %) | 4 (5 %) | 6 (8 %) | 8 (11 %) | 20 (28 %) |
| Somnolence | 1 (1 %) | 3 (4 %) | 0 (0 %) | 1 (1 %) | 10 (14 %) |
| Asthenia | 0 (0 %) | 2 (3 %) | 0 (0 %) | 2 (2 %) | 7 (10 %) |
| Dizziness | 2 (2 %) | 1 (1 %) | 3 (4 %) | 6 (8 %) | 3 (4 %) |
| Headache | 3 (4 %) | 4 (3 %) | 3 (4 %) | 1 (1 %) | 2 (2 %) |
| Impotence | 1 (1 %) | 1 (0 %) | 0 (0 %) | 1 (1 %) | 3 (4 %) |
| Constipation | 0 (0 %) | 0 (0 %) | 0 (0 %) | 1 (1 %) | 1 (1 %) |
| Fatigue | 3 (3 %) | 2 (3 %) | 2 (3 %) | 5 (6 %) | 3 (4 %) |
There were 41 premature terminations because of adverse reactions in this study. The percent of patients who dropped out and the dose at which the dropout occurred were as follows:
Dose | Placebo | 0.5 mg | 1 mg | 2 mg | 3 mg |
| Percent dropouts | 6.9 % | 4.2 % | 3.2 % | 6.9 % | 8.3 % |
Reasons for dropouts among patients who received guanfacine were: somnolence, headache, weakness, dry mouth, dizziness, impotence, insomnia, constipation, syncope, urinary incontinence, conjunctivitis, paresthesia, and dermatitis.
In a second 12-week placebo-controlled combination therapy study in which the dose could be adjusted upward to 3 mg per day in 1-mg increments at 3-week intervals, i.e., a setting more similar to ordinary clinical use, the most commonly recorded reactions were: dry mouth, 47 %; constipation, 16 %; fatigue, 12 %; somnolence, 10 %; asthenia, 6 %; dizziness, 6 %; headache, 4 %; and insomnia, 4 %.
Reasons for dropouts among patients who received guanfacine were: somnolence, dry mouth, dizziness, impotence, constipation, confusion, depression, and palpitations.
In the clonidine/guanfacine comparison described in
Adverse Reactions | Guanfacine (n = 279) | Clonidine (n = 278) |
| Dry Mouth | 30 % | 37 % |
| Somnolence | 21 % | 35 % |
| Dizziness | 11 % | 8 % |
| Constipation | 10 % | 5 % |
| Fatigue | 9 % | 8 % |
| Headache | 4 % | 4 % |
| Insomnia | 4 % | 3 % |
Adverse reactions occurring in 3 % or less of patients in the three controlled trials of guanfacine hydrochloride with a diuretic were:
Cardiovascular- bradycardia, palpitations, substernal pain
Gastrointestinal- abdominal pain, diarrhea, dyspepsia, dysphagia, nausea
CNS- amnesia, confusion, depression, insomnia, libido decrease
ENT disorders- rhinitis, taste perversion, tinnitus
Eye disorders- conjunctivitis, iritis, vision disturbance
Musculoskeletal- leg cramps, hypokinesia
Respiratory- dyspnea
Dermatologic- dermatitis, pruritus, purpura, sweating
Urogenital- testicular disorder, urinary incontinence
Other- malaise, paresthesia, paresis
Adverse reaction reports tend to decrease over time. In an open-label trial of one year's duration, 580 hypertensive subjects were given guanfacine, titrated to achieve goal blood pressure, alone (51 %), with diuretic (38 %), with beta blocker (3 %), with diuretic plus beta blocker (6 %), or with diuretic plus vasodilator (2 %). The mean daily dose of guanfacine reached was 4.7 mg.
Adverse Reaction | Incidence of adverse reactions at any time during the study n = 580 | Incidence of adverse reactions at end of one year n = 580 |
| Dry Mouth | 60 % | 15 % |
| Drowsiness | 33 % | 6 % |
| Dizziness | 15 % | 1 % |
| Constipation | 14 % | 3 % |
| Weakness | 5 % | 1 % |
| Headache | 4 % | 0.2 % |
| Insomnia | 5 % | 0 % |
There were 52 (8.9 %) dropouts due to adverse effects in this 1-year trial. The causes were: dry mouth (n = 20), weakness (n = 12), constipation (n = 7), somnolence (n = 3), nausea (n = 3), orthostatic hypotension (n = 2), insomnia (n = 1), rash (n = 1), nightmares (n = 1), headache (n = 1), and depression (n = 1).
An open-label postmarketing study involving 21,718 patients was conducted to assess the safety of guanfacine hydrochloride 1 mg/day given at bedtime for 28 days. Guanfacine tablets were administered with or without other antihypertensive agents. Adverse events reported in the postmarketing study at an incidence greater than 1 % included dry mouth, dizziness, somnolence, fatigue, headache and nausea. The most commonly reported adverse events in this study were the same as those observed in controlled clinical trials.
Less frequent, possibly guanfacine tablets-related events observed in the postmarketing study and/or reported spontaneously include:
BODY AS A WHOLE asthenia, chest pain, edema, malaise, tremor
CARDIOVASCULAR bradycardia, palpitations, syncope, tachycardia
CENTRAL NERVOUS SYSTEM paresthesias, vertigo
EYE DISORDERS blurred vision
GASTROINTESTINAL SYSTEM abdominal pain, constipation, diarrhea, dyspepsia
LIVER AND BILLIARY SYSTEM abnormal liver function tests
MUSCULO-SKELETAL SYSTEM arthralgia, leg cramps, leg pain, myalgia
PSYCHIATRIC agitation, anxiety, confusion, depression, insomnia, nervousness
REPRODUCTIVE SYSTEM, Male- impotence
RESPIRATORY SYSTEM dyspnea
SKIN AND APPENDAGES alopecia, dermatitis, exfoliative dermatitis, pruritus, rash
SPECIAL SENSES alterations in taste
URINARY SYSTEM nocturia, urinary frequency
Rare, serious disorders with no definitive cause and effect relationship to guanfacine tablets have been reported spontaneously and/or in the postmarketing study. These events include acute renal failure, cardiac fibrillation, cerebrovascular accident, congestive heart failure, heart block, and myocardial infarction.
In a second 12-week placebo-controlled study of 1 mg, 2 mg or 3 mg of guanfacine hydrochloride administered with 25 mg of chlorthalidone once daily, a significant decrease in blood pressure was maintained for a full 24 hours after dosing. While there was no significant difference between the 12 hour and 24 hour blood pressure readings, the fall in blood pressure at 24 hours was numerically smaller, suggesting possible escape of blood pressure in some patients and the need for individualization of therapy.
In a double-blind, randomized trial, either guanfacine or clonidine was given at recommended doses with 25 mg chlorthalidone for 24 weeks and then abruptly discontinued. Results showed equal degrees of blood pressure reduction with the two drugs and there was no tendency for blood pressures to increase despite maintenance of the same daily dose of the two drugs. Signs and symptoms of rebound phenomena were infrequent upon discontinuation of either drug. Abrupt withdrawal of clonidine produced a rapid return of diastolic and especially systolic blood pressure to approximately pretreatment levels, with occasional values significantly greater than baseline, whereas guanfacine withdrawal produced a more gradual increase to pretreatment levels, but also with occasional values significantly greater than baseline.
Hemodynamic studies in man showed that the decrease in blood pressure observed after single-dose or long-term oral treatment with guanfacine was accompanied by a significant decrease in peripheral resistance and a slight reduction in heart rate (5 beats/min). Cardiac output under conditions of rest or exercise was not altered by guanfacine.
Guanfacine hydrochloride lowered elevated plasma renin activity and plasma catecholamine levels in hypertensive patients, but this does not correlate with individual blood-pressure responses.
Growth hormone secretion was stimulated with single oral doses of 2 mg and 4 mg of guanfacine. Long-term use of guanfacine tablets had no effect on growth hormone levels.
Guanfacine had no effect on plasma aldosterone. A slight but insignificant decrease in plasma volume occurred after one month of guanfacine therapy. There were no changes in mean body weight or electrolytes.
Relative to an intravenous dose of 3 mg, the absolute oral bioavailability of guanfacine is about 80 %. Peak plasma concentrations occur from 1 hour to 4 hours with an average of 2.6 hours after single oral doses or at steady state.
The area under the concentration-time curve (AUC) increases linearly with the dose.
In individuals with normal renal function, the average elimination half-life is approximately 17 hours (range 10 hours to 30 hours). Younger patients tend to have shorter elimination half-lives (13 hours to 14 hours) while older patients tend to have half-lives at the upper end of the range. Steady state blood levels were attained within 4 days in most subjects.
In individuals with normal renal function, guanfacine and its metabolites are excreted primarily in the urine. Approximately 50 % (40 % to 75 %) of the dose is eliminated in the urine as unchanged drug; the remainder is eliminated mostly as conjugates of metabolites produced by oxidative metabolism of the aromatic ring.
The guanfacine-to-creatinine clearance ratio is greater than 1.0, which would suggest that tubular secretion of drug occurs.
The drug is approximately 70 % bound to plasma proteins, independent of drug concentration.
The whole body volume of distribution is high (a mean of 6.3 L/kg), which suggests a high distribution of drug to the tissues.
The clearance of guanfacine in patients with varying degrees of renal insufficiency is reduced, but plasma levels of drug are only slightly increased compared to patients with normal renal function. When prescribing for patients with renal impairment, the low end of the dosing range should be used. Patients on dialysis also can be given usual doses of guanfacine hydrochloride as the drug is poorly dialyzed.