Ipratropium Bromide
Ipratropium Bromide Prescribing Information
Ipratropium bromide nasal solution 0.03% is indicated for the symptomatic relief of rhinorrhea associated with allergic and nonallergic perennial rhinitis in adults and children age 6 years and older. Ipratropium bromide 0.03% does not relieve nasal congestion, sneezing, or postnasal drip associated with allergic or nonallergic perennial rhinitis.
The recommended dose of ipratropium bromide solution, 0.03% is two sprays (21 mcg) per nostril two or three times daily (total dose 168 to 252 mcg/day) for the symptomatic relief of rhinorrhea associated with allergic and nonallergic perennial rhinitis in adults and children age 6 years and older. Optimum dosage varies with the response of the individual patient.
Initial pump priming requires seven sprays of the pump. If used regularly as recommended, no further priming is required. If not used for more than 24 hours, the pump will require two sprays, or if not used for more than seven days, the pump will require seven sprays to reprime.
Ipratropium bromide nasal solution 0.03% is contraindicated in patients with a history of hypersensitivity to atropine or its derivatives, or to any of the other ingredients.
Adverse reaction information on ipratropium bromide nasal solution, 0.03% in patients with perennial rhinitis was derived from four multicenter, vehicle-controlled clinical trials involving 703 patients (356 patients on ipratropium bromide and 347 patients on vehicle), and a one-year, open-label, follow-up trial. In three of the trials, patients received ipratropium bromide 0.03% three times daily, for eight weeks. In the other trial, ipratropium bromide 0.03% was given to patients two times daily for four weeks. Of the 285 patients who entered the open-label, follow-up trial, 232 were treated for 3 months, 200 for 6 months, and 159 up to one year. The majority (>86%) of patients treated for one year were maintained on 42 mcg per nostril, two or three times daily, of ipratropium bromide 0.03%. Table 1 shows adverse events, and the frequency that these adverse events led to the discontinuation of treatment, reported for patients who received ipratropium bromide 0.03% at the recommended dose of 42 mcg per nostril, or vehicle two or three times daily for four or eight weeks. Only adverse events reported with an incidence of at least 2.0% in the ipratropium bromide group and higher in the ipratropium bromide group than in the vehicle group are shown.
Table 1 % of Patients Reporting Events* | ||||
Ipratropium Bromide 0.03% (n=356) | Vehicle Control (n=347) | |||
Incidence % | Discontinued % | Incidence % | Discontinued % | |
Headache | 9.8 | 0.6 | 9.2 | 0.0 |
Upper respiratory tract infection | 9.8 | 1.4 | 7.2 | 1.4 |
Epistaxis | 9.0 | 0.3 | 4.6 | 0.3 |
Rhinitis Nasal dryness | 5.1 | 0.0 | 0.9 | 0.3 |
Nasal Irritation | 2.0 | 0.0 | 1.7 | 0.6 |
Other nasal symptoms | 3.1 | 1.1 | 1.7 | 0.3 |
Pharyngitis | 8.1 | 0.3 | 4.6 | 0.0 |
Nausea | 2.2 | 0.3 | 0.9 | 0.0 |
+This table includes adverse events which occurred at an incidence rate of at least 2.0% in the Ipratropium Bromide group and more frequently in the Ipratropium Bromide group than in the vehicle group.
1Epistaxis reported by 7.0% of Ipratropium Bromide patients and 2.3% of vehicle patients, blood-tinged mucus by 2.0% of Ipratropium Bromide patients and 2.3% of vehicle patients.
2Nasal irritation includes reports of nasal itching, nasal burning, nasal irritation, and ulcerative rhinitis.
3Other nasal symptoms include reports of nasal congestion, increased rhinorrhea, increased rhinitis, posterior nasal drip, sneezing, nasal polyps, and nasal edema.
*All events are listed by their WHO term; rhinitis has been presented by descriptive terms for clarification.
Ipratropium bromide 0.03% was well tolerated by most patients. The most frequently reported nasal adverse events were transient episodes of nasal dryness or epistaxis. These adverse events were mild or moderate in nature, none was considered serious, none resulted in hospitalization and most resolved spontaneously or following a dose reduction. Treatment for nasal dryness and epistaxis was required infrequently (2% or less) and consisted of local application of pressure or a moisturizing agent (e.g., petroleum jelly or saline nasal spray). Patient discontinuation for epistaxis or nasal dryness was infrequent in both the controlled (0.3% or less) and one-year, open-label (2% or less) trials. There was no evidence of nasal rebound (i.e., a clinically significant increase in rhinorrhea, posterior nasal drip, sneezing or nasal congestion severity compared to baseline) upon discontinuation of double-blind therapy in these trials.
Adverse events reported by less than 2% of the patients receiving ipratropium bromide 0.03% during the controlled clinical trials or during the open-label follow-up trial, which are potentially related to Ipratropium Bromide’s local effects or systemic anticholinergic effects include: dry mouth/throat, dizziness, ocular irritation, blurred vision, conjunctivitis, hoarseness, cough, and taste perversion.
There were infrequent reports of skin rash in both the controlled and uncontrolled clinical studies.
Allergic type reactions such as skin rash, angioedema, including that of the throat, tongue, lips and face, generalized urticaria (including giant urticaria), laryngospasm, and anaphylactic reactions have been reported with ipratropium bromide 0.03% and for other ipratropium bromide-containing products, with positive rechallenge in some cases. Additional side effects identified from the published literature and/or post-marketing surveillance on the use of ipratropium bromide-containing products (singly or in combination with albuterol), include: urinary retention, prostatic disorders, mydriasis, cases of precipitation or worsening of narrow-angle glaucoma, acute eye pain, wheezing, dryness of the oropharynx, sinusitis, tachycardia, palpitations, pain, edema, gastrointestinal distress (diarrhea, nausea, vomiting), bowel obstruction, constipation, nasal discomfort, throat irritation, hypersensitivity, accommodation disorder, intraocular pressure increased, glaucoma, halo vision, conjunctival hyperaemia, corneal edema, heart rate increased, bronchospasm, pharyngeal edema, gastrointestinal motility disorder, mouth edema, stomatitis, and pruritus.
After oral inhalation of ipratropium bromide in patients suffering from COPD/Asthma supraventricular tachycardia and atrial fibrillation have been reported.
The active ingredient in Ipratropium Bromide Nasal Solution is ipratropium bromide (as the monohydrate). It is an anticholinergic agent chemically described as 8-azoniabicyclo (3.2.1) octane, 3-(3-hydroxy-1-oxo-2-phenylpropoxy)-8-methyl-8-(1-methylethyl)-, bromide monohydrate (3-endo, 8-syn)-: a synthetic quaternary ammonium compound, chemically related to atropine. The structural formula is:
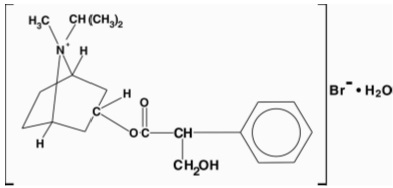
20H
30BrNO
3• H
2O Mol. Wt. 430.4
Ipratropium bromide is a white to off-white crystalline substance, freely soluble in water and methanol, sparingly soluble in ethanol, and insoluble in non-polar media. In aqueous solution, it exists in an ionized state as a quaternary ammonium compound.
Ipratropium Bromide Nasal Solution, 0.03% is a metered-dose, manual pump spray unit which delivers 21 mcg (70 mcL) ipratropium bromide per spray on an anhydrous basis in an isotonic, aqueous solution with pH adjusted to 4.7 with hydrochloric acid and/or sodium hydroxide (if needed). It also contains benzalkonium chloride, edetate disodium, purified water and sodium chloride. Each bottle contains 345 metered sprays.
Ipratropium bromide is an anticholinergic (parasympatholytic) agent which, based on animal studies, appears to inhibit vagally-mediated reflexes by antagonizing the action of acetylcholine, the transmitter agent released at the neuromuscular junctions in the lung. In humans, ipratropium bromide has anti-secretory properties and, when applied locally, inhibits secretions from the serous and seromucous glands lining the nasal mucosa Ipratropium bromide is a quaternary amine that minimally crosses the nasal and gastrointestinal membrane and the blood-brain barrier, resulting in a reduction of the systemic anticholinergic effects (e.g., neurologic, ophthalmic, cardiovascular, and gastrointestinal effects) that are seen with tertiary anticholinergic amines.
Ipratropium bromide is poorly absorbed into the systemic circulation following oral administration (2 to 3%). Less than 20% of an 84 mcg per nostril dose was absorbed from the nasal mucosa of normal volunteers, induced-cold patients, or perennial rhinitis patients.
Ipratropium bromide is minimally bound (0 to 9% in vitro) to plasma albumin and α1 -acid glycoprotein. Its blood/plasma concentration ratio was estimated to be about 0.89. Studies in rats have shown that ipratropium bromide does not penetrate the blood-brain barrier.
Ipratropium bromide is partially metabolized to ester hydrolysis products, tropic acid and tropane. These metabolites appear to be inactive based on in vitro receptor affinity studies using rat brain tissue homogenates.
After intravenous administration of 2 mg ipratropium bromide to 10 healthy volunteers, the terminal half-life of ipratropium was approximately 1.6 hours. The total body clearance and renal clearance were estimated to be 2,505 and 1,019 mL/min, respectively. The amount of the total dose excreted unchanged in the urine (Ae) within 24 hours was approximately one-half of the administered dose.
Following administration of 42 mcg of ipratropium bromide per nostril two or three times a day in perennial rhinitis patients 6 to 18 years old, the mean amounts of the total dose excreted unchanged in the urine (8.6 to 11.1%) were higher than those reported in adult volunteers or adult perennial rhinitis patients (3.7 to 5.6%). Plasma ipratropium concentrations were relatively low (ranging from undetectable up to 0.49 ng/mL). No correlation of the amount of the total dose excreted unchanged in the urine (Ae) with age or gender was observed in the pediatric population.
Gender does not appear to influence the absorption or excretion of nasally administered ipratropium bromide. The pharmacokinetics of ipratropium bromide have not been studied in patients with hepatic or renal insufficiency or in the elderly.
No specific pharmacokinetic studies were conducted to evaluate potential drug-drug interactions.
In two single-dose trials (n=17), doses up to 336 mcg of ipratropium bromide did not significantly affect pupillary diameter, heart rate, or systolic/diastolic blood pressure. Similarly, in patients with induced-colds, ipratropium bromide nasal spray 0.06% (84 mcg/nostril four times a day), had no significant effects on pupillary diameter, heart rate or systolic/ diastolic blood pressure.
Two nasal provocation trials in perennial rhinitis patients (n=44) using ipratropium bromide nasal spray showed a dose dependent increase in inhibition of methacholine induced nasal secretion with an onset of action within 15 minutes (time of first observation). Controlled clinical trials demonstrated that intranasal fluorocarbon-propelled ipratropium bromide does not alter physiologic nasal functions (e.g., sense of smell, ciliary beat frequency, mucociliary clearance, or the air conditioning capacity of the nose).
The clinical trials for ipratropium bromide 0.03% were conducted in patients with nonallergic perennial rhinitis (NAPR) and in patients with allergic perennial rhinitis (APR). APR patients were those who experienced symptoms of nasal hypersecretion and nasal congestion or sneezing when exposed to specific perennial allergens (e.g., dust mites, molds) and were skin test positive to these allergens. NAPR patients were those who experienced symptoms of nasal hypersecretion and nasal congestion or sneezing throughout the year but were skin test negative to common perennial allergens. In four controlled, four- and eight-week comparisons of ipratropium bromide 0.03% (42 mcg per nostril, two or three times daily) with its vehicle, in patients with allergic or nonallergic perennial rhinitis, there was a statistically significant decrease in the severity and duration of rhinorrhea in the ipratropium bromide group throughout the entire study period. An effect was seen as early as the first day of therapy. There was no effect of ipratropium bromide 0.03% on degree of nasal congestion, sneezing, or postnasal drip. The response to ipratropium bromide 0.03% did not appear to be affected by the type of perennial rhinitis (NAPR or APR), age, or gender. No controlled clinical trials directly compared the efficacy of BID versus TID treatment.