Ivermectin
Ivermectin Prescribing Information
Ivermectin is indicated for the treatment of the following infections:
The recommended dosage of ivermectin tablets for the treatment of strongyloidiasis is a single oral dose designed to provide approximately 200 mcg of ivermectin per kg of body weight. See
Body Weight (kg) | Single Oral Dose Number of 3-mg Tablets |
| 15-24 | 1 tablet |
| 25-35 | 2 tablets |
| 36-50 | 3 tablets |
| 51-65 | 4 tablets |
| 66-79 | 5 tablets |
| ≥ 80 | 200 mcg/kg |
Following oral administration of ivermectin, plasma concentrations are approximately proportional to the dose. In two studies, after single 12-mg doses of ivermectin tablets in fasting healthy volunteers (representing a mean dose of 165 mcg/kg), the mean peak plasma concentrations of the major component (H2B1a) were 46.6 (±21.9) (range: 16.4 - 101.1) and 30.6 (±15.6) (range: 13.9 - 68.4) ng/mL, respectively, at approximately 4 hours after dosing. Ivermectin is metabolized in the liver, and ivermectin and/or its metabolites are excreted almost exclusively in the feces over an estimated 12 days, with less than 1% of the administered dose excreted in the urine. The plasma half-life of ivermectin in man is approximately 18 hours following oral administration.
The safety and pharmacokinetic properties of ivermectin were further assessed in a multiple-dose clinical pharmacokinetic study involving healthy volunteers. Subjects received oral doses of 30 to 120 mg (333 to 2000 mcg/kg) ivermectin in a fasted state or 30 mg (333 to 600 mcg/kg) ivermectin following a standard high-fat (48.6 g of fat) meal. Administration of 30 mg ivermectin following a high-fat meal resulted in an approximate 2.5-fold increase in bioavailability relative to administration of 30 mg ivermectin in the fasted state.
Two controlled clinical studies using albendazole as the comparative agent were carried out in international sites where albendazole is approved for the treatment of strongyloidiasis of the gastrointestinal tract, and three controlled studies were carried out in the U.S. and internationally using thiabendazole as the comparative agent. Efficacy, as measured by cure rate, was defined as the absence of larvae in at least two follow-up stool examinations 3 to 4 weeks post-therapy. Based on this criterion, efficacy was significantly greater for ivermectin (a single dose of 170 to 200 mcg/kg) than for albendazole (200 mg b.i.d. for 3 days). Ivermectin tablets administered as a single dose of 200 mcg/kg for 1 day was as efficacious as thiabendazole administered at 25 mg/kg b.i.d. for 3 days.
Summary of Cure Rates for Ivermectin Versus Comparative Agents in the Treatment of Strongyloidiasis
| Cure Rate* (%) | ||
| Ivermectin† | Comparative Agent | |
| Albendazole‡Comparative | ||
| International Study | 24/26 (92) | 12/22 (55) |
| WHO Study | 126/152 (83) | 67/149 (45) |
| Thiabendazole§Comparative | ||
| International Study | 9/14 (64) | 13/15 (87) |
| US Studies | 14/14 (100) | 16/17 (94) |
*Number and % of evaluable patients
†170-200 mcg/kg
‡200 mg b.i.d. for 3 days
§25 mg/kg b.i.d. for 3 days
In one study conducted in France, a non-endemic area where there was no possibility of reinfection, several patients were observed to have recrudescence of Strongyloides larvae in their stool as long as 106 days following ivermectin therapy. Therefore, at least three stool examinations should be conducted over the three months following treatment to ensure eradication. If recrudescence of larvae is observed, retreatment with ivermectin is indicated. Concentration techniques (such as using a Baermann apparatus) should be employed when performing these stool examinations, as the number of Strongyloides larvae per gram of feces may be very low.
The evaluation of ivermectin in the treatment of onchocerciasis is based on the results of clinical studies involving 1278 patients. In a double-blind, placebo-controlled study involving adult patients with moderate to severe onchocercal infection, patients who received a single dose of 150 mcg/kg ivermectin tablets experienced an 83.2% and 99.5% decrease in skin microfilariae count (geometric mean) 3 days and 3 months after the dose, respectively. A marked reduction of >90% was maintained for up to 12 months after the single dose. As with other microfilaricidal drugs, there was an increase in the microfilariae count in the anterior chamber of the eye at day 3 after treatment in some patients. However, at 3 and 6 months after the dose, a significantly greater percentage of patients treated with ivermectin had decreases in microfilariae count in the anterior chamber than patients treated with placebo.
In a separate open study involving pediatric patients ages 6 to 13 (n=103; weight range: 17-41 kg), similar decreases in skin microfilariae counts were observed for up to 12 months after dosing.
Body Weight (kg) | Single Oral Dose Number of 3-mg Tablets |
| 15-24 | 1 tablet |
| 25-35 | 2 tablets |
| 36-50 | 3 tablets |
| 51-65 | 4 tablets |
| 66-79 | 5 tablets |
| ≥ 80 | 200 mcg/kg |
Ivermectin tablets are contraindicated in patients who are hypersensitive to any component of this product.
In four clinical studies involving a total of 109 patients given either one or two doses of 170 to 200 mcg/kg of ivermectin, the following adverse reactions were reported as possibly, probably, or definitely related to ivermectin:
In comparative trials, patients treated with ivermectin experienced more abdominal distention and chest discomfort than patients treated with albendazole. However, ivermectin was better tolerated than thiabendazole in comparative studies involving 37 patients treated with thiabendazole.
The Mazzotti-type and ophthalmologic reactions associated with the treatment of onchocerciasis or the disease itself would not be expected to occur in strongyloidiasis patients treated with ivermectin (See
In clinical trials involving 963 adult patients treated with 100 to 200 mcg/kg ivermectin tablets, worsening of the following Mazzotti reactions during the first 4 days post-treatment were reported: arthralgia/synovitis (9.3%), axillary lymph node enlargement and tenderness (11.0% and 4.4%, respectively), cervical lymph node enlargement and tenderness (5.3% and 1.2%, respectively), inguinal lymph node enlargement and tenderness (12.6% and 13.9%, respectively), other lymph node enlargement and tenderness (3.0% and 1.9%, respectively), pruritus (27.5%), skin involvement including edema, papular and pustular or frank urticarial rash (22.7%), and fever (22.6%) (See WARNINGS).
In clinical trials, ophthalmological conditions were examined in 963 adult patients before treatment, at day 3, and months 3 and 6 after treatment with 100 to 200 mcg/kg ivermectin. Changes observed were primarily deterioration from baseline 3 days post-treatment. Most changes either returned to baseline condition or improved over baseline severity at the month 3 and 6 visits. The percentages of patients with worsening of the following conditions at day 3, month 3 and 6, respectively, were: limbitis: 5.5%, 4.8%, and 3.5% and punctate opacity: 1.8%, 1.8%, and 1.4%. The corresponding percentages for patients treated with placebo were: limbitis: 6.2%, 9.9%, and 9.4% and punctate opacity: 2.0%, 6.4%, and 7.2% (See WARNINGS).
In clinical trials involving 963 adult patients who received 100 to 200 mcg/kg ivermectin, the following clinical adverse reactions were reported as possibly, probably, or definitely related to the drug in ≥ 1% of the patients: facial edema (1.2%), peripheral edema (3.2%), orthostatic hypotension (1.1%), and tachycardia (3.5%). Drug-related headache and myalgia occurred in < 1% of patients (0.2% and 0.4%, respectively). However, these were the most common adverse experiences reported overall during these trials regardless of causality (22.3% and 19.7%, respectively).
A similar safety profile was observed in an open study in pediatric patients ages 6 to 13.
The following ophthalmological side effects do occur due to the disease itself but have also been reported after treatment with ivermectin: abnormal sensation in the eyes, eyelid edema, anterior uveitis, conjunctivitis, limbitis, keratitis, and chorioretinitis or choroiditis. These have rarely been severe or associated with loss of vision and have generally resolved without corticosteroid treatment.
In controlled clinical trials, the following laboratory adverse experiences were reported as possibly, probably, or definitely related to the drug in ≥ 1% of the patients: eosinophilia (3%) and hemoglobin increase (1%).
Post-marketing reports of increased INR (International Normalized Ratio) have been rarely reported when ivermectin was co-administered with warfarin.
Ivermectin is a semisynthetic, anthelmintic agent for oral administration. Ivermectin is derived from the avermectins, a class of highly active broad-spectrum, anti-parasitic agents isolated from the fermentation products of
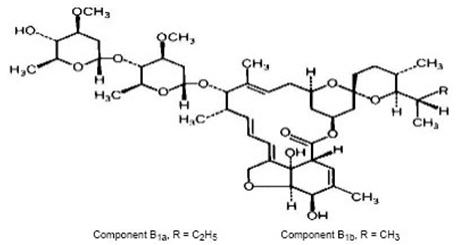
Ivermectin is a white to yellowish-white, nonhygroscopic, crystalline powder with a melting point of about 155°C. It is insoluble in water but is freely soluble in methanol and soluble in 95% ethanol.
Ivermectin tablets are available as 3-mg tablets containing the following inactive ingredients: colloidal silicon dioxide, croscarmellose sodium, magnesium stearate, microcrystalline cellulose, and pregelatinized starch.