Lenalidomide Prescribing Information
Lenalidomide is a thalidomide analogue and is contraindicated for use during pregnancy. Thalidomide is a known human teratogen that causes life-threatening human birth defects or embryo-fetal death
Lenalidomide is only available through the
Females of reproductive potential must avoid pregnancy for at least 4 weeks before beginning lenalidomide therapy, during therapy, during dose interruptions and for at least 4 weeks after completing therapy.
Females must commit either to abstain continuously from heterosexual sexual intercourse or to use two methods of reliable birth control, beginning 4 weeks prior to initiating treatment with lenalidomide, during therapy, during dose interruptions and continuing for 4 weeks following discontinuation of lenalidomide therapy.
Two negative pregnancy tests must be obtained prior to initiating therapy. The first test should be performed within 10 to 14 days and the second test within 24 hours prior to prescribing lenalidomide therapy and then weekly during the first month, then monthly thereafter in females with regular menstrual cycles or every 2 weeks in females with irregular menstrual cycles
Lenalidomide is present in the semen of patients receiving the drug. Therefore, males must always use a latex or synthetic condom during any sexual contact with females of reproductive potential while taking lenalidomide and for up to 4 weeks after discontinuing lenalidomide, even if they have undergone a successful vasectomy. Male patients taking lenalidomide must not donate sperm and for up to 4 weeks after discontinuing lenalidomide
Patients must not donate blood during treatment with lenalidomide and for 4 weeks following discontinuation of the drug because the blood might be given to a pregnant female patient whose fetus must not be exposed to lenalidomide.
Advise patients that lenalidomide is contraindicated in pregnancy
Advise females of reproductive potential that they must avoid pregnancy while taking lenalidomide and for at least 4 weeks after completing therapy.
Initiate lenalidomide treatment in females of reproductive potential only following a negative pregnancy test.
Advise females of reproductive potential of the importance of monthly pregnancy tests and the need to use 2 different forms of contraception including at least 1 highly effective form, simultaneously during lenalidomide therapy, during dose interruption and for 4 weeks after she has completely finished taking lenalidomide. Highly effective forms of contraception other than tubal ligation include IUD and hormonal (birth control pills, injections, patch or implants) and a partner's vasectomy. Additional effective contraceptive methods include latex or synthetic condom, diaphragm and cervical cap.
Instruct patient to immediately stop taking lenalidomide and contact her healthcare provider if she becomes pregnant while taking this drug, if she misses her menstrual period, or experiences unusual menstrual bleeding, if she stops taking birth control, or if she thinks FOR ANY REASON that she may be pregnant.
Advise patient that if her healthcare provider is not available, she should call the REMS Call Center at 1-888-423-5436
[see Warnings and Precautions (5.1)and Use in Specific Populations (8.3)].Advise males to always use a latex or synthetic condom during any sexual contact with females of reproductive potential while taking lenalidomide and for up to 4 weeks after discontinuing lenalidomide, even if they have undergone a successful vasectomy.
Advise male patients taking lenalidomide that they must not donate sperm and for up to 4 weeks after discontinuation lenalidomide
[see Warnings and Precautions (5.1)and Use in Specific Populations (8.3)].All patients must be instructed to not donate blood while taking lenalidomide, during dose interruptions and for 4 weeks following discontinuation of lenalidomide
[see Warnings and Precautions (5.1)].
Because of the risk of embryo-fetal toxicity, lenalidomide is only available through a restricted program called the Lenalidomide REMS program
Patients must sign a Patient-Physician agreement form and comply with the requirements to receive lenalidomide. In particular, females of reproductive potential must comply with the pregnancy testing, contraception requirements and participate in monthly telephone surveys. Males must comply with the contraception requirements
[see Use in Specific Populations (8.3)].Lenalidomide is available only from pharmacies that are certified in the Lenalidomide REMS program. Provide patients with the telephone number and website for information on how to obtain the product.
Pregnancy Exposure Registry
Inform females there is a Pregnancy Exposure Registry that monitors pregnancy outcomes in females exposed to lenalidomide during pregnancy and that they can contact the Pregnancy Exposure Registry by calling 1-888-423-5436 [
Inform patients that lenalidomide is associated with significant neutropenia and thrombocytopenia
Inform patients of the risk of thrombosis including DVT, PE, MI, and stroke and to report immediately any signs and symptoms suggestive of these events for evaluation [
Inform patients that lenalidomide had increased mortality in patients with CLL and serious adverse cardiovascular reactions, including atrial fibrillation, myocardial infarction, and cardiac failure
Inform patients of the potential risk of developing second primary malignancies during treatment with lenalidomide
Inform patients of the risk of hepatotoxicity, including hepatic failure and death, and to report any signs and symptoms associated with this event to their healthcare provider for evaluation
Inform patients of the potential risk for severe skin reactions such as SJS, TEN, and DRESS and report any signs and symptoms associated with these reactions to their healthcare provider for evaluation. Patients with a prior history of Grade 4 rash associated with thalidomide treatment should not receive lenalidomide
Inform patients of the potential risk of tumor lysis syndrome and to report any signs and symptoms associated with this event to their healthcare provider for evaluation
Inform patients of the potential risk of tumor flare reaction and to report any signs and symptoms associated with this event to their healthcare provider for evaluation
Inform patients with MCL of the potential for early death
Inform patients of the potential for severe hypersensitivity reactions such as angioedema and anaphylaxis to lenalidomide. Instruct patients to contact their healthcare provider right away for signs and symptoms of these reactions. Advise patients to seek emergency medical attention for signs or symptoms of severe hypersensitivity reactions
Inform patients how to take lenalidomide
Lenalidomide should be taken once daily at about the same time each day,
Lenalidomide may be taken either with or without food.
The capsules should not be opened, broken, or chewed. Lenalidomide should be swallowed whole with water.
Instruct patients that if they miss a dose of lenalidomide, they may still take it up to 12 hours after the time they would normally take it. If more than 12 hours have elapsed, they should be instructed to skip the dose for that day. The next day, they should take lenalidomide at the usual time. Warn patients to not take 2 doses to make up for the one that they missed.
Biocon Pharma Limited
Bengaluru, India – 560099
Biocon Pharma Inc.,
Iselin, New Jersey, 08830-3009
United States of America
Because of the embryo-fetal risk
Required components of the
Prescribers must be certified with the
Lenalidomide REMSprogram by enrolling and complying with the REMS requirements.Patients must sign a Patient-Physician agreement form and comply with the REMS requirements. In particular, female patients of reproductive potential who are not pregnant must comply with the pregnancy testing and contraception requirements
[see Use in Specific Populations (8.3)]and males must comply with contraception requirements[see Use in Specific Populations (8.3)].Pharmacies must be certified with the
Lenalidomide REMSprogram, must only dispense to patients who are authorized to receive lenalidomide and comply with REMS requirements.
Further information about the
The recommended starting dose of lenalidomide is 10 mg daily. Treatment is continued or modified based upon clinical and laboratory findings. Continue treatment until disease progression or unacceptable toxicity.
Patients who are dosed initially at 10 mg and who experience thrombocytopenia should have their dosage adjusted as follows:
If thrombocytopenia develops WITHIN 4 weeks of starting treatment at 10 mg daily in MDS
If baseline is at least 100,000/mcL | |
When Platelets | Recommended Course |
| Fall below 50,000/mcL | Interrupt lenalidomide treatment |
| Return to at least 50,000/mcL | Resume lenalidomide at 5 mg daily |
If baseline is below 100,000/mcL | |
When Platelets | Recommended Course |
Fall to 50% of the baseline value If baseline is at least 60,000/mcL and returns to at least 50,000/mcL If baseline is below 60,000/mcL and returns to at least 30,000/mcL | Interrupt lenalidomide treatment Resume lenalidomide at 5 mg daily Resume lenalidomide at 5 mg daily |
If thrombocytopenia develops AFTER 4 weeks of starting treatment at 10 mg daily in MDS
When Platelets | Recommended Course |
| Fall below 30,000/mcL or below 50,000/mcL with platelet transfusions | Interrupt lenalidomide treatment |
| Return to at least 30,000/mcL (without hemostatic failure) | Resume lenalidomide at 5 mg daily |
Patients who experience thrombocytopenia at 5 mg daily should have their dosage adjusted as follows:
If thrombocytopenia develops during treatment at 5 mg daily in MDS
When Platelets | Recommended Course |
| Fall below 30,000/mcL or below 50,000/mcL with platelet transfusions | Interrupt lenalidomide treatment |
| Return to at least 30,000/mcL (without hemostatic failure) | Resume lenalidomide at 2.5 mg daily |
Patients who are dosed initially at 10 mg and experience neutropenia should have their dosage adjusted as follows:
If neutropenia develops WITHIN 4 weeks of starting treatment at 10 mg daily in MDS
If baseline ANC is at least 1,000/mcL | |
When Neutrophils | Recommended Course |
| Fall below 750/mcL | Interrupt lenalidomide treatment |
| Return to at least 1,000/mcL | Resume lenalidomide at 5 mg daily |
If baseline ANC is below 1,000/mcL | |
When Neutrophils | Recommended Course |
| Fall below 500/mcL | Interrupt lenalidomide treatment |
| Return to at least 500/mcL | Resume lenalidomide at 5 mg daily |
If neutropenia develops AFTER 4 weeks of starting treatment at 10 mg daily in MDS
When Platelets | Recommended Course |
| Fall below 500/mcL for at least 7 days or below 500/mcL associated with fever (at least 38.5°C) | Interrupt lenalidomide treatment |
| Return to at least 500/mcL | Resume lenalidomide at 5 mg daily |
Patients who experience neutropenia at 5 mg daily should have their dosage adjusted as follows:
If neutropenia develops during treatment at 5 mg daily in MDS
When Platelets | Recommended Course |
| Fall below 500/mcL for at least 7 days or below 500/mcL associated with fever (at least 38.5°C) | Interrupt lenalidomide treatment |
| Return to at least 500/mcL | Resume lenalidomide at 2.5 mg daily |
Venous thromboembolic events (VTE [DVT and PE]) and arterial thromboembolic events (ATE, myocardial infarction and stroke) are increased in patients treated with lenalidomide.
A significantly increased risk of DVT (7.4%) and of PE (3.7%) occurred in patients with MM after at least one prior therapy who were treated with lenalidomide and dexamethasone therapy compared to patients treated in the placebo and dexamethasone group (3.1% and 0.9%) in clinical trials with varying use of anticoagulant therapies. In the newly diagnosed multiple myeloma (NDMM) study in which nearly all patients received antithrombotic prophylaxis, DVT was reported as a serious adverse reaction (3.6%, 2.0%, and 1.7%) in the Rd Continuous, Rd18, and MPT Arms, respectively. The frequency of serious adverse reactions of PE was similar between the Rd Continuous, Rd18, and MPT Arms (3.8%, 2.8%, and 3.7%, respectively)
Myocardial infarction (1.7%) and stroke (CVA) (2.3%) are increased in patients with MM after at least one prior therapy who were treated with lenalidomide and dexamethasone therapy compared to patients treated with placebo and dexamethasone (0.6%, and 0.9%) in clinical trials. In the NDMM study, myocardial infarction (including acute) was reported as a serious adverse reaction (2.3%, 0.6%, and 1.1%) in the Rd Continuous, Rd18, and MPT Arms, respectively. The frequency of serious adverse reactions of CVA was similar between the Rd Continuous, Rd18, and MPT Arms (0.8%, 0.6 %, and 0.6%, respectively)
Patients with known risk factors, including prior thrombosis, may be at greater risk and actions should be taken to try to minimize all modifiable factors (e.g. hyperlipidemia, hypertension, smoking).
In controlled clinical trials that did not use concomitant thromboprophylaxis, 21.5% overall thrombotic events (Standardized MedDRA Query Embolic and Thrombotic events) occurred in patients with refractory and relapsed MM who were treated with lenalidomide and dexamethasone compared to 8.3% thrombosis in patients treated with placebo and dexamethasone. The median time to first thrombosis event was 2.8 months. In the NDMM study in which nearly all patients received antithrombotic prophylaxis, the overall frequency of thrombotic events was 17.4% in patients in the combined Rd Continuous and Rd18 Arms, and was 11.6% in the MPT Arm. The median time to first thrombosis event was 4.3 months in the combined Rd Continuous and Rd18 Arms.
In the AUGMENT trial, the incidence of VTE (including DVT and PE) in FL or MZL patients was 3.4% in the lenalidomide /rituximab arm
Thromboprophylaxis is recommended. The regimen of thromboprophylaxis should be based on an assessment of the patient's underlying risks. Instruct patients to report immediately any signs and symptoms suggestive of thrombotic events. ESAs and estrogens may further increase the risk of thrombosis and their use should be based on a benefit-risk decision in patients receiving lenalidomide
Warnings and Precautions ( Lenalidomide is a thalidomide analogue and is contraindicated for use during pregnancy. Thalidomide is a known human teratogen that causes life-threatening human birth defects or embryo-fetal death [see Use in Specific Populations (8.1)] . An embryo-fetal development study in monkeys indicates that lenalidomide produced malformations in the offspring of female monkeys who received the drug during pregnancy, similar to birth defects observed in humans following exposure to thalidomide during pregnancy.Lenalidomide is only available through the Lenalidomide REMS program[see Warnings and Precautions (5.2)] .Females of Reproductive Potential Females of reproductive potential must avoid pregnancy for at least 4 weeks before beginning lenalidomide therapy, during therapy, during dose interruptions and for at least 4 weeks after completing therapy. Females must commit either to abstain continuously from heterosexual sexual intercourse or to use two methods of reliable birth control, beginning 4 weeks prior to initiating treatment with lenalidomide, during therapy, during dose interruptions and continuing for 4 weeks following discontinuation of lenalidomide therapy. Two negative pregnancy tests must be obtained prior to initiating therapy. The first test should be performed within 10 to 14 days and the second test within 24 hours prior to prescribing lenalidomide therapy and then weekly during the first month, then monthly thereafter in females with regular menstrual cycles or every 2 weeks in females with irregular menstrual cycles [see Use in Specific Populations (8.3)] .Males Lenalidomide is present in the semen of patients receiving the drug. Therefore, males must always use a latex or synthetic condom during any sexual contact with females of reproductive potential while taking lenalidomide and for up to 4 weeks after discontinuing lenalidomide, even if they have undergone a successful vasectomy. Male patients taking lenalidomide must not donate sperm and for up to 4 weeks after discontinuing lenalidomide [see Use in Specific Populations (8.3)]. Blood Donation Patients must not donate blood during treatment with lenalidomide and for 4 weeks following discontinuation of the drug because the blood might be given to a pregnant female patient whose fetus must not be exposed to lenalidomide. Tumor flare reaction (TFR), including fatal reactions, have occurred during investigational use of lenalidomide for CLL and lymphoma, and is characterized by tender lymph node swelling, low grade fever, pain and rash. Lenalidomide is not indicated and not recommended for use in CLL outside of controlled clinical trials. Monitoring and evaluation for TFR is recommended in patients with MCL, FL, or MZL. Tumor flare reaction may mimic progression of disease (PD). In the MCL trial, 13/134 (10%) of subjects experienced TFR; all reports were Grade 1 or 2 in severity. All of the events occurred in Cycle 1 and one patient developed TFR again in Cycle 11. In the AUGMENT trial in FL or MZL patients, TFR was reported in 19/176 (10.8%) of patients in lenalidomide with rituximab arm; one patient in the lenalidomide /rituximab arm experienced a Grade 3 TFR. In the MAGNIFY trial, 9/222 (4.1%) of patients experienced TFR; all reports were Grade 1 or 2 in severity and 1 event was considered as serious. In a separate MCL phase 2 trial, one case of TFR resulted in a fatal outcome. Lenalidomide may be continued in patients with Grade 1 and 2 TFR without interruption or modification, at the physician's discretion. Patients with Grade 1 and 2 TFR may also be treated with corticosteroids, non-steroidal anti-inflammatory drugs (NSAIDs) and/or narcotic analgesics for management of TFR symptoms. In patients with Grade 3 or 4 TFR, it is recommended to withhold treatment with lenalidomide until TFR resolves to ≤ Grade 1. Patients with Grade 3 or 4 TFR may be treated for management of symptoms per the guidance for treatment of Grade 1 and 2 TFR. | 5/2022 |
Lenalidomide is a thalidomide analogue indicated for the treatment of adult patients with:
Multiple myeloma (MM), in combination with dexamethasone (
).1.1 Multiple MyelomaLenalidomide in combination with dexamethasone is indicated for the treatment of adult patients with multiple myeloma (MM).
Lenalidomide is indicated as maintenance therapy in adult patients with MM following autologous hematopoietic stem cell transplantation (auto-HSCT).
MM, as maintenance following autologous hematopoietic stem cell transplantation (auto-HSCT) (
).1.1 Multiple MyelomaLenalidomide in combination with dexamethasone is indicated for the treatment of adult patients with multiple myeloma (MM).
Lenalidomide is indicated as maintenance therapy in adult patients with MM following autologous hematopoietic stem cell transplantation (auto-HSCT).
Transfusion-dependent anemia due to low- or intermediate-1-risk myelodysplastic syndromes (MDS) associated with a deletion 5q abnormality with or without additional cytogenetic abnormalities (
).1.2 Myelodysplastic SyndromesLenalidomide is indicated for the treatment of adult patients with transfusion-dependent anemia due to low- or intermediate-1-risk myelodysplastic syndromes (MDS) associated with a deletion 5q cytogenetic abnormality with or without additional cytogenetic abnormalities.
Mantle cell lymphoma (MCL) whose disease has relapsed or progressed after two prior therapies, one of which included bortezomib (
).1.3 Mantle Cell LymphomaLenalidomideis indicated for the treatment of adult patients with mantle cell lymphoma (MCL) whose disease has relapsed or progressed after two prior therapies, one of which included bortezomib.
Previously treated follicular lymphoma (FL), in combination with a rituximab product (
).1.4 Follicular LymphomaLenalidomidein combination with a rituximab product, is indicated for the treatment of adult patients with previously treated follicular lymphoma (FL).
Previously treated marginal zone lymphoma (MZL), in combination with a rituximab product (
).1.5 Marginal Zone LymphomaLenalidomide in combination with a rituximab product, is indicated for the treatment of adult patients with previously treated marginal zone lymphoma (MZL).
Lenalidomide is not indicated and is not recommended for the treatment of patients with chronic lymphocytic leukemia (CLL) outside of controlled clinical trials (
).1.4 Follicular LymphomaLenalidomidein combination with a rituximab product, is indicated for the treatment of adult patients with previously treated follicular lymphoma (FL).
MM combination therapy: 25 mg once daily orally on Days 1 to 21 of repeated 28-day cycles. (
).2.1 Recommended Dosage for Multiple MyelomaLenalidomide Combination TherapyThe recommended starting dose of lenalidomide is 25 mg orally once daily on Days 1 to 21 of repeated 28-day cycles in combination with dexamethasone. Refer to Section 14.1 for specific dexamethasone dosing. For patients greater than 75 years old, the starting dose of dexamethasone may be reduced
[see Clinical Studies (14.1)]. Treatment should be continued until disease progression or unacceptable toxicity.In patients who are not eligible for auto-HSCT, treatment should continue until disease progression or unacceptable toxicity. For patients who are auto-HSCT-eligible, hematopoietic stem cell mobilization should occur within 4 cycles of a lenalidomide-containing therapy
[see Warnings and Precautions (5.12)].Dose Adjustments for Hematologic Toxicities During MM TreatmentDose modification guidelines, as summarized in Table 1 below, are recommended to manage Grade 3 or 4 neutropenia or thrombocytopenia or other Grade 3 or 4 toxicity judged to be related to lenalidomide.
Table 1: Dose Adjustments for Hematologic Toxicities for MMPlatelet countsThrombocytopenia in MMWhen PlateletsRecommended Course Days 1 to 21 of repeated 28-day cycleFall below 30,000/mcL Interrupt lenalidomide treatment, follow CBC weekly Return to at least 30,000/mcL Resume lenalidomide at next lower dose. Do not dose below 2.5 mg daily For each subsequent drop below 30,000/mcL Interrupt lenalidomide treatment Return to at least 30,000/mcL Resume lenalidomide at next lower dose. Do not dose below 2.5 mg daily Absolute Neutrophil counts (ANC)Neutropenia in MMWhen NeutrophilsRecommended Course Days 1 to 21 of repeated 28-day cycleFall below 1,000/mcL Interrupt lenalidomide treatment, follow CBC weekly Return to at least 1,000/mcL and neutropenia is the only toxicity Resume lenalidomide at 25 mg daily or initial starting dose Return to at least 1,000/mcL and if other toxicity Resume lenalidomide at next lower dose. Do not dose below 2.5 mg daily For each subsequent drop below 1,000/mcL Interrupt lenalidomide treatment Return to at least 1,000/mcL Resume lenalidomide at next lower dose. Do not dose below 2.5 mg daily Lenalidomide Maintenance Therapy Following Auto-HSCTFollowing auto-HSCT, initiate lenalidomide maintenance therapy after adequate hematologic recovery (ANC at least 1,000/mcL and/or platelet counts at least 75,000/mcL). The recommended starting dose of lenalidomide is 10 mg once daily continuously (Days 1 to 28 of repeated 28-day cycles) until disease progression or unacceptable toxicity. After 3 cycles of maintenance therapy, the dose can be increased to 15 mg once daily if tolerated.
Dose Adjustments for Hematologic Toxicities During MM TreatmentDose modification guidelines, as summarized in Table 2 below, are recommended to manage Grade 3 or 4 neutropenia or thrombocytopenia or other Grade 3 or 4 toxicity judged to be related to lenalidomide.
Table 2: Dose Adjustments for Hematologic Toxicities for MMPlatelet countsThrombocytopenia in MMWhen PlateletsRecommended CourseFall below 30,000/mcL
Return to at least 30,000/mcL
Interrupt lenalidomide treatment, follow CBC weekly
Resume lenalidomide at next lower dose, continuously for Days 1 to 28 of repeated 28-day cycle
If at the 5 mg daily dose,
For a subsequent drop below 30,000/mcL
Return to at least 30,000/mcL
Interrupt lenalidomide treatment. Do not dose below 5 mg daily for Day 1 to 21 of 28 day cycle
Resume lenalidomide at 5 mg daily for Days 1 to 21 of 28-day cycle. Do not dose below 5 mg daily for Day 1 to 21 of 28 day cycle
Absolute Neutrophil counts (ANC)Neutropenia in MMWhen NeutrophilsRecommended CourseFall below 500/mcL
Return to at least 500/mcL
Interrupt lenalidomide treatment, follow CBC weekly
Resume lenalidomide at next lower dose, continuously for Days 1 to 28 of repeated 28-day cycle
If at 5 mg daily dose,
For a subsequent drop below 500/mcL
Return to at least 500/mcL
Interrupt lenalidomide treatment. Do not dose below 5 mg daily for Day 1 to 21 of 28-day cycle
Resume lenalidomide at 5 mg daily for Days 1 to 21 of 28-day cycle. Do not dose below 5 mg daily for Day 1 to 21 of 28-day cycle
MM maintenance therapy following auto-HSCT: 10 mg once daily continuously on Days 1 to 28 of repeated 28-day cycles (
).2.1 Recommended Dosage for Multiple MyelomaLenalidomide Combination TherapyThe recommended starting dose of lenalidomide is 25 mg orally once daily on Days 1 to 21 of repeated 28-day cycles in combination with dexamethasone. Refer to Section 14.1 for specific dexamethasone dosing. For patients greater than 75 years old, the starting dose of dexamethasone may be reduced
[see Clinical Studies (14.1)]. Treatment should be continued until disease progression or unacceptable toxicity.In patients who are not eligible for auto-HSCT, treatment should continue until disease progression or unacceptable toxicity. For patients who are auto-HSCT-eligible, hematopoietic stem cell mobilization should occur within 4 cycles of a lenalidomide-containing therapy
[see Warnings and Precautions (5.12)].Dose Adjustments for Hematologic Toxicities During MM TreatmentDose modification guidelines, as summarized in Table 1 below, are recommended to manage Grade 3 or 4 neutropenia or thrombocytopenia or other Grade 3 or 4 toxicity judged to be related to lenalidomide.
Table 1: Dose Adjustments for Hematologic Toxicities for MMPlatelet countsThrombocytopenia in MMWhen PlateletsRecommended Course Days 1 to 21 of repeated 28-day cycleFall below 30,000/mcL Interrupt lenalidomide treatment, follow CBC weekly Return to at least 30,000/mcL Resume lenalidomide at next lower dose. Do not dose below 2.5 mg daily For each subsequent drop below 30,000/mcL Interrupt lenalidomide treatment Return to at least 30,000/mcL Resume lenalidomide at next lower dose. Do not dose below 2.5 mg daily Absolute Neutrophil counts (ANC)Neutropenia in MMWhen NeutrophilsRecommended Course Days 1 to 21 of repeated 28-day cycleFall below 1,000/mcL Interrupt lenalidomide treatment, follow CBC weekly Return to at least 1,000/mcL and neutropenia is the only toxicity Resume lenalidomide at 25 mg daily or initial starting dose Return to at least 1,000/mcL and if other toxicity Resume lenalidomide at next lower dose. Do not dose below 2.5 mg daily For each subsequent drop below 1,000/mcL Interrupt lenalidomide treatment Return to at least 1,000/mcL Resume lenalidomide at next lower dose. Do not dose below 2.5 mg daily Lenalidomide Maintenance Therapy Following Auto-HSCTFollowing auto-HSCT, initiate lenalidomide maintenance therapy after adequate hematologic recovery (ANC at least 1,000/mcL and/or platelet counts at least 75,000/mcL). The recommended starting dose of lenalidomide is 10 mg once daily continuously (Days 1 to 28 of repeated 28-day cycles) until disease progression or unacceptable toxicity. After 3 cycles of maintenance therapy, the dose can be increased to 15 mg once daily if tolerated.
Dose Adjustments for Hematologic Toxicities During MM TreatmentDose modification guidelines, as summarized in Table 2 below, are recommended to manage Grade 3 or 4 neutropenia or thrombocytopenia or other Grade 3 or 4 toxicity judged to be related to lenalidomide.
Table 2: Dose Adjustments for Hematologic Toxicities for MMPlatelet countsThrombocytopenia in MMWhen PlateletsRecommended CourseFall below 30,000/mcL
Return to at least 30,000/mcL
Interrupt lenalidomide treatment, follow CBC weekly
Resume lenalidomide at next lower dose, continuously for Days 1 to 28 of repeated 28-day cycle
If at the 5 mg daily dose,
For a subsequent drop below 30,000/mcL
Return to at least 30,000/mcL
Interrupt lenalidomide treatment. Do not dose below 5 mg daily for Day 1 to 21 of 28 day cycle
Resume lenalidomide at 5 mg daily for Days 1 to 21 of 28-day cycle. Do not dose below 5 mg daily for Day 1 to 21 of 28 day cycle
Absolute Neutrophil counts (ANC)Neutropenia in MMWhen NeutrophilsRecommended CourseFall below 500/mcL
Return to at least 500/mcL
Interrupt lenalidomide treatment, follow CBC weekly
Resume lenalidomide at next lower dose, continuously for Days 1 to 28 of repeated 28-day cycle
If at 5 mg daily dose,
For a subsequent drop below 500/mcL
Return to at least 500/mcL
Interrupt lenalidomide treatment. Do not dose below 5 mg daily for Day 1 to 21 of 28-day cycle
Resume lenalidomide at 5 mg daily for Days 1 to 21 of 28-day cycle. Do not dose below 5 mg daily for Day 1 to 21 of 28-day cycle
MDS: 10 mg once daily (
).2.2 Recommended Dosage for Myelodysplastic SyndromesThe recommended starting dose of lenalidomide is 10 mg daily. Treatment is continued or modified based upon clinical and laboratory findings. Continue treatment until disease progression or unacceptable toxicity.
Dose Adjustments for Hematologic Toxicities During MDS TreatmentPatients who are dosed initially at 10 mg and who experience thrombocytopenia should have their dosage adjusted as follows:
Platelet countsIf thrombocytopenia develops WITHIN 4 weeks of starting treatment at 10 mg daily in MDS
If baseline is at least 100,000/mcLWhen PlateletsRecommended CourseFall below 50,000/mcL Interrupt lenalidomide treatment Return to at least 50,000/mcL Resume lenalidomide at 5 mg daily If baseline is below 100,000/mcLWhen PlateletsRecommended CourseFall to 50% of the baseline value
If baseline is at least 60,000/mcL and returns to at least 50,000/mcL
If baseline is below 60,000/mcL and returns to at least 30,000/mcL
Interrupt lenalidomide treatment
Resume lenalidomide at 5 mg daily
Resume lenalidomide at 5 mg daily
If thrombocytopenia develops AFTER 4 weeks of starting treatment at 10 mg daily in MDS
When PlateletsRecommended CourseFall below 30,000/mcL or below 50,000/mcL with platelet transfusions Interrupt lenalidomide treatment Return to at least 30,000/mcL (without hemostatic failure) Resume lenalidomide at 5 mg daily Patients who experience thrombocytopenia at 5 mg daily should have their dosage adjusted as follows:
If thrombocytopenia develops during treatment at 5 mg daily in MDS
When PlateletsRecommended CourseFall below 30,000/mcL or below 50,000/mcL with platelet transfusions Interrupt lenalidomide treatment Return to at least 30,000/mcL (without hemostatic failure) Resume lenalidomide at 2.5 mg daily Patients who are dosed initially at 10 mg and experience neutropenia should have their dosage adjusted as follows:
Absolute Neutrophil counts (ANC)If neutropenia develops WITHIN 4 weeks of starting treatment at 10 mg daily in MDS
If baseline ANC is at least 1,000/mcLWhen NeutrophilsRecommended CourseFall below 750/mcL Interrupt lenalidomide treatment Return to at least 1,000/mcL Resume lenalidomide at 5 mg daily If baseline ANC is below 1,000/mcLWhen NeutrophilsRecommended CourseFall below 500/mcL Interrupt lenalidomide treatment Return to at least 500/mcL Resume lenalidomide at 5 mg daily If neutropenia develops AFTER 4 weeks of starting treatment at 10 mg daily in MDS
When PlateletsRecommended CourseFall below 500/mcL for at least 7 days or below 500/mcL associated with fever (at least 38.5°C) Interrupt lenalidomide treatment Return to at least 500/mcL Resume lenalidomide at 5 mg daily Patients who experience neutropenia at 5 mg daily should have their dosage adjusted as follows:
If neutropenia develops during treatment at 5 mg daily in MDS
When PlateletsRecommended CourseFall below 500/mcL for at least 7 days or below 500/mcL associated with fever (at least 38.5°C) Interrupt lenalidomide treatment Return to at least 500/mcL Resume lenalidomide at 2.5 mg daily MCL: 25 mg once daily orally on Days 1 to 21 of repeated 28-day cycles (
).2.3 Recommended Dosage for Mantle Cell LymphomaThe recommended starting dose of lenalidomide is 25 mg/day orally on Days 1 to 21 of repeated 28-day cycles for relapsed or refractory mantle cell lymphoma.
Treatment should be continued until disease progression or unacceptable toxicity.
Treatment is continued, modified or discontinued based upon clinical and laboratory findings.
Dose Adjustments for Hematologic Toxicities During MCL TreatmentDose modification guidelines as summarized below are recommended to manage Grade 3 or 4 neutropenia or thrombocytopenia or other Grade 3 or 4 toxicities considered to be related to lenalidomide.
Platelet countsThrombocytopenia during treatment in MCL
When PlateletsRecommended CourseFall below 50,000/mcL Interrupt lenalidomide treatment and follow CBC weekly Return to at least 50,000/mcL Resume lenalidomide at 5 mg less than the previous dose. Do not dose below 5 mg daily Absolute Neutrophil counts (ANC)Neutropenia during treatment in MCL
When PlateletsRecommended CourseFall below 1,000/mcL for at least 7 days
OR
Falls below 1,000/mcL with an associated temperature at least 38.5°C
OR
Falls below 500/mcL
Interrupt lenalidomide treatment and follow CBC weekly Return to at least 1,000/mcL Resume lenalidomide at 5 mg less than the previous dose. Do not dose below 5 mg daily FL or MZL: 20 mg once daily orally on Days 1 to 21 of repeated 28-day cycles for up to 12 cycles (
).2.4 Recommended Dosage for Follicular Lymphoma or Marginal Zone LymphomaThe recommended starting dose of lenalidomide is 20 mg orally once daily on Days 1 to 21 of repeated 28-day cycles for up to 12 cycles of treatment in combination with a rituximab-product. Refer to Section 14.4 for specific rituximab dosing from the AUGMENT trial. For dose adjustments due to toxicity with rituximab, refer to the product prescribing information.
Dose Adjustments for Hematologic Toxicities during FL or MZL TreatmentDose modification guidelines, as summarized below, are recommended to manage Grade 3 or 4 neutropenia or thrombocytopenia or other Grade 3 or 4 toxicity judged to be related to lenalidomide.
Platelet countsThrombocytopenia during treatment in FL or MZL
When PlateletsRecommended CourseFall below 50,000/mcL Interrupt lenalidomide treatment and follow CBC weekly. Return to at least 50,000/mcL If patient starting dose was 20 mg daily, resume lenalidomide at 5 mg less than the previous dose. Do not dose below 5 mg daily.
If patient starting dose was 10 mg daily, resume at 5 mg less than previous dose. Do not dose below 2.5 mg daily.
Absolute Neutrophil counts (ANC)Neutropenia during treatment in FL or MZL
When PlateletsRecommended CourseFall below 1,000/mcL for at least 7 days
OR
Falls below 1,000/mcL with an associated temperature at least 38.5°C
OR
Falls below 500/mcL
Interrupt lenalidomide treatment and follow CBC weekly Return to at least 1,000/mcL If patient starting dose was 20 mg daily, resume lenalidomide at 5 mg less than the previous dose. Do not dose below 5 mg daily.
If patient starting dose was 10 mg daily, resume at 5 mg less than previous dose. Do not dose below 2.5 mg daily.
Renal impairment: Adjust starting dose based on the creatinine clearance value (
).2.6 Recommended Dosage for Patients with Renal ImpairmentThe recommendations for dosing patients with renal impairment are shown in the following table
[see Clinical Pharmacology (12.3)].Table 3: Dose Adjustments for Patients with Renal Impairment Renal Function(Cockcroft-Gault)Dose in Lenalidomide Combination Therapy for MM and MCLDose in Lenalidomide Combination Therapy for FL and MZLDose in Lenalidomide Maintenance Therapy Following Auto-HSCT for MM and for MDSCLcr 30 to 60 mL/min
10 mg once daily
10 mg once daily
5 mg once daily
CLcr below 30 mL/min (not requiring dialysis)
15 mg every other day
5 mg once daily
2.5 mg once daily
CLcr below 30 mL/min (requiring dialysis)
5 mg once daily. On dialysis days, administer the dose following dialysis.
5 mg once daily. On dialysis days, administer the dose following dialysis.
2.5 mg once daily. On dialysis days, administer the dose following dialysis.
Lenalidomide Combination Therapy for MM: For CLcr of 30 to 60 mL/min, consider escalating the dose to 15 mg after 2 cycles if the patient tolerates the 10 mg dose of lenalidomide without dose-limiting toxicity.Lenalidomide Maintenance Therapy Following Auto-HSCT for MM and for MCL and MDS: Base subsequent lenalidomide dose increase or decrease on individual patient treatment tolerance[see Dosage and Administration ].Lenalidomide Combination Therapy for FL or for MZL:For patients with CLcr of 30 to 60 mL/min, after 2 cycles, the lenalidomide dose may be increased to 15 mg orally if the patient has tolerated therapy.For concomitant therapy doses, see Full Prescribing Information (
,2.1 Recommended Dosage for Multiple MyelomaLenalidomide Combination TherapyThe recommended starting dose of lenalidomide is 25 mg orally once daily on Days 1 to 21 of repeated 28-day cycles in combination with dexamethasone. Refer to Section 14.1 for specific dexamethasone dosing. For patients greater than 75 years old, the starting dose of dexamethasone may be reduced
[see Clinical Studies (14.1)]. Treatment should be continued until disease progression or unacceptable toxicity.In patients who are not eligible for auto-HSCT, treatment should continue until disease progression or unacceptable toxicity. For patients who are auto-HSCT-eligible, hematopoietic stem cell mobilization should occur within 4 cycles of a lenalidomide-containing therapy
[see Warnings and Precautions (5.12)].Dose Adjustments for Hematologic Toxicities During MM TreatmentDose modification guidelines, as summarized in Table 1 below, are recommended to manage Grade 3 or 4 neutropenia or thrombocytopenia or other Grade 3 or 4 toxicity judged to be related to lenalidomide.
Table 1: Dose Adjustments for Hematologic Toxicities for MMPlatelet countsThrombocytopenia in MMWhen PlateletsRecommended Course Days 1 to 21 of repeated 28-day cycleFall below 30,000/mcL Interrupt lenalidomide treatment, follow CBC weekly Return to at least 30,000/mcL Resume lenalidomide at next lower dose. Do not dose below 2.5 mg daily For each subsequent drop below 30,000/mcL Interrupt lenalidomide treatment Return to at least 30,000/mcL Resume lenalidomide at next lower dose. Do not dose below 2.5 mg daily Absolute Neutrophil counts (ANC)Neutropenia in MMWhen NeutrophilsRecommended Course Days 1 to 21 of repeated 28-day cycleFall below 1,000/mcL Interrupt lenalidomide treatment, follow CBC weekly Return to at least 1,000/mcL and neutropenia is the only toxicity Resume lenalidomide at 25 mg daily or initial starting dose Return to at least 1,000/mcL and if other toxicity Resume lenalidomide at next lower dose. Do not dose below 2.5 mg daily For each subsequent drop below 1,000/mcL Interrupt lenalidomide treatment Return to at least 1,000/mcL Resume lenalidomide at next lower dose. Do not dose below 2.5 mg daily Lenalidomide Maintenance Therapy Following Auto-HSCTFollowing auto-HSCT, initiate lenalidomide maintenance therapy after adequate hematologic recovery (ANC at least 1,000/mcL and/or platelet counts at least 75,000/mcL). The recommended starting dose of lenalidomide is 10 mg once daily continuously (Days 1 to 28 of repeated 28-day cycles) until disease progression or unacceptable toxicity. After 3 cycles of maintenance therapy, the dose can be increased to 15 mg once daily if tolerated.
Dose Adjustments for Hematologic Toxicities During MM TreatmentDose modification guidelines, as summarized in Table 2 below, are recommended to manage Grade 3 or 4 neutropenia or thrombocytopenia or other Grade 3 or 4 toxicity judged to be related to lenalidomide.
Table 2: Dose Adjustments for Hematologic Toxicities for MMPlatelet countsThrombocytopenia in MMWhen PlateletsRecommended CourseFall below 30,000/mcL
Return to at least 30,000/mcL
Interrupt lenalidomide treatment, follow CBC weekly
Resume lenalidomide at next lower dose, continuously for Days 1 to 28 of repeated 28-day cycle
If at the 5 mg daily dose,
For a subsequent drop below 30,000/mcL
Return to at least 30,000/mcL
Interrupt lenalidomide treatment. Do not dose below 5 mg daily for Day 1 to 21 of 28 day cycle
Resume lenalidomide at 5 mg daily for Days 1 to 21 of 28-day cycle. Do not dose below 5 mg daily for Day 1 to 21 of 28 day cycle
Absolute Neutrophil counts (ANC)Neutropenia in MMWhen NeutrophilsRecommended CourseFall below 500/mcL
Return to at least 500/mcL
Interrupt lenalidomide treatment, follow CBC weekly
Resume lenalidomide at next lower dose, continuously for Days 1 to 28 of repeated 28-day cycle
If at 5 mg daily dose,
For a subsequent drop below 500/mcL
Return to at least 500/mcL
Interrupt lenalidomide treatment. Do not dose below 5 mg daily for Day 1 to 21 of 28-day cycle
Resume lenalidomide at 5 mg daily for Days 1 to 21 of 28-day cycle. Do not dose below 5 mg daily for Day 1 to 21 of 28-day cycle
,2.4 Recommended Dosage for Follicular Lymphoma or Marginal Zone LymphomaThe recommended starting dose of lenalidomide is 20 mg orally once daily on Days 1 to 21 of repeated 28-day cycles for up to 12 cycles of treatment in combination with a rituximab-product. Refer to Section 14.4 for specific rituximab dosing from the AUGMENT trial. For dose adjustments due to toxicity with rituximab, refer to the product prescribing information.
Dose Adjustments for Hematologic Toxicities during FL or MZL TreatmentDose modification guidelines, as summarized below, are recommended to manage Grade 3 or 4 neutropenia or thrombocytopenia or other Grade 3 or 4 toxicity judged to be related to lenalidomide.
Platelet countsThrombocytopenia during treatment in FL or MZL
When PlateletsRecommended CourseFall below 50,000/mcL Interrupt lenalidomide treatment and follow CBC weekly. Return to at least 50,000/mcL If patient starting dose was 20 mg daily, resume lenalidomide at 5 mg less than the previous dose. Do not dose below 5 mg daily.
If patient starting dose was 10 mg daily, resume at 5 mg less than previous dose. Do not dose below 2.5 mg daily.
Absolute Neutrophil counts (ANC)Neutropenia during treatment in FL or MZL
When PlateletsRecommended CourseFall below 1,000/mcL for at least 7 days
OR
Falls below 1,000/mcL with an associated temperature at least 38.5°C
OR
Falls below 500/mcL
Interrupt lenalidomide treatment and follow CBC weekly Return to at least 1,000/mcL If patient starting dose was 20 mg daily, resume lenalidomide at 5 mg less than the previous dose. Do not dose below 5 mg daily.
If patient starting dose was 10 mg daily, resume at 5 mg less than previous dose. Do not dose below 2.5 mg daily.
,14.1 Multiple MyelomaRandomized, Open-Label Clinical Trial in Patients with Newly Diagnosed MM:A randomized multicenter, open-label, 3-arm trial of 1,623 patients, was conducted to compare the efficacy and safety of lenalidomide and low-dose dexamethasone (Rd) given for 2 different durations of time to that of melphalan, prednisone and thalidomide (MPT) in newly diagnosed MM patients who were not a candidate for stem cell transplant. In the first arm of the study, Rd was given continuously until progressive disease [Arm Rd Continuous]. In the second arm, Rd was given for up to eighteen 28-day cycles [72 weeks, Arm Rd18]). In the third arm, melphalan, prednisone and thalidomide (MPT) was given for a maximum of twelve 42-day cycles (72 weeks). For the purposes of this study, a patient who was < 65 years of age was not a candidate for SCT if the patient refused to undergo SCT therapy or the patient did not have access to SCT due to cost or other reasons. Patients were stratified at randomization by age (≤75 versus >75 years), stage (ISS Stages I and II versus Stage III), and country.
Patients in the Rd Continuous and Rd18 arms received lenalidomide 25 mg once daily on Days 1 to 21 of 28-day cycles. Dexamethasone was dosed 40 mg once daily on Days 1, 8, 15, and 22 of each 28-day cycle. For patients over > 75 years old, the starting dose of dexamethasone was 20 mg orally once daily on days 1,8,15, and 22 of repeated 28-day cycles. Initial dose and regimens for Rd Continuous and Rd18 were adjusted according to age and renal function. All patients received prophylactic anticoagulation with the most commonly used being aspirin.
The demographics and disease-related baseline characteristics of the patients were balanced among the 3 arms. In general, study subjects had advanced-stage disease. Of the total study population, the median age was 73 in the 3 arms with 35% of total patients > 75 years of age; 59% had ISS Stage I/II; 41% had ISS stage III; 9% had severe renal impairment (creatinine clearance [CLcr] < 30 mL/min); 23% had moderate renal impairment (CLcr > 30 to 50 mL/min; 44% had mild renal impairment (CLcr > 50 to 80 mL/min). For ECOG Performance Status, 29% were Grade 0, 49% Grade 1, 21% Grade 2, 0.4% ≥ Grade 3.
The primary efficacy endpoint, progression-free survival (PFS), was defined as the time from randomization to the first documentation of disease progression as determined by Independent Response Adjudication Committee (IRAC), based on International Myeloma Working Group [IMWG] criteria or death due to any cause, whichever occurred first during the study until the end of the PFS follow-up phase. For the efficacy analysis of all endpoints, the primary comparison was between Rd Continuous and MPT arms. The efficacy results are summarized in the table below. PFS was significantly longer with Rd Continuous than MPT: HR 0.72 (95% CI: 0.61-0.85 p <0.0001). A lower percentage of subjects in the Rd Continuous arm compared with the MPT arm had PFS events (52% versus 61%, respectively). The improvement in median PFS time in the Rd Continuous arm compared with the MPT arm was 4.3 months. The myeloma response rate was higher with Rd Continuous compared with MPT (75.1% versus 62.3%); with a complete response in 15.1% of Rd Continuous arm patients versus 9.3% in the MPT arm. The median time to first response was 1.8 months in the Rd Continuous arm versus 2.8 months in the MPT arm.
For the interim OS analysis with 03 March 2014 data cutoff, the median follow-up time for all surviving patients is 45.5 months, with 697 death events, representing 78% of prespecified events required for the planned final OS analysis (697/896 of the final OS events). The observed OS HR was 0.75 for Rd Continuous versus MPT (95% CI = 0.62, 0.90).
Table 13: Overview of Efficacy Results – Study MM-020 (Intent-to-treat Population)Rd Continuous (N = 535)Rd18 (N = 541)MPT (N = 547)PFS – IRAC (months)gNumber of PFS events 278 (52) 348 (64.3) 334 (61.1) MedianaPFS time, months (95% CI)b 25.5 (20.7, 29.4) 20.7 (19.4, 22) 21.2 (19.3, 23.2) HR [95% CI]c; p-valued Rd Continuous vs MPT 0.72 (0.61, 0.85); <0.0001 Rd Continuous vs Rd18 0.70 (0.60, 0.82) Rd18 vs MPT 1.03 (0.89, 1.20) Overall Survival (months)hNumber of Death events 208 (38.9) 228 (42.1) 261 (47.7) MedianaOS time, months (95% CI)b 58.9 (56, NE)f 56.7 (50.1, NE) 48.5 (44.2, 52) HR [95% CI]c Rd Continuous vs MPT 0.75 (0.62, 0.90) Rd Continuous vs Rd18 0.91 (0.75, 1.09) Rd18 vs MPT 0.83 (0.69, 0.99) Response Ratee– IRAC, n (%)gCR 81 (15.1) 77 (14.2) 51 (9.3) VGPR 152 (28.4) 154 (28.5) 103 (18.8) PR 169 (31.6) 166 (30.7) 187 (34.2) Overall response: CR, VGPR, or PR 402 (75.1) 397 (73.4) 341 (62.3) CR = complete response; d = low-dose dexamethasone; HR = hazard ratio; IRAC = Independent Response Adjudication Committee; M = melphalan; NE = not estimable; OS = overall survival; P = prednisone; PFS = progression-free survival; PR = partial response; R = lenalidomide; Rd Continuous = Rd given until documentation of progressive disease; Rd18 = Rd given for ≤ 18 cycles; T = thalidomide; VGPR = very good partial response; vs = versus.
a The median is based on the Kaplan-Meier estimate.
b The 95% Confidence Interval (CI) about the median.
c Based on Cox proportional hazards model comparing the hazard functions associated with the indicated treatment arms.
d The p-value is based on the unstratified log-rank test of Kaplan-Meier curve differences between the indicated treatment arms.
e Best assessment of response during the treatment phase of the study.
f Including patients with no response assessment data or whose only assessment was “response not evaluable.”
g Data cutoff date = 24 May 2013.
h Data cutoff date = 3 March 2014.
Kaplan-Meier Curves of Progression-free Survival Based on IRAC Assessment (ITT MM Population) Between Arms Rd Continuous, Rd18 and MPT Cutoff date: 24 May 2013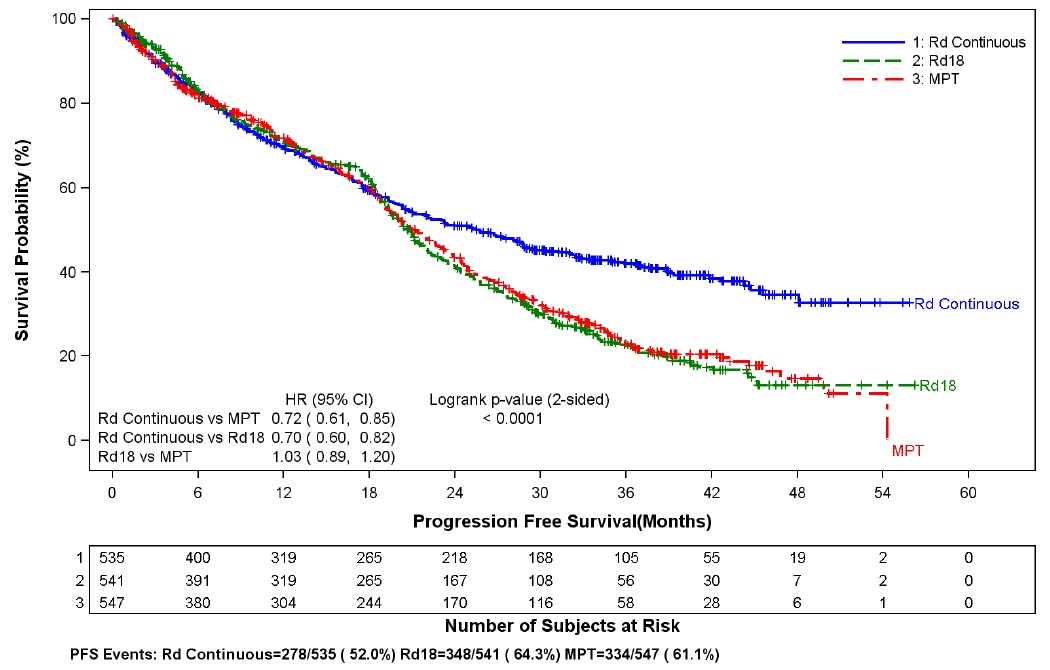
CI = confidence interval; d = low-dose dexamethasone; HR = hazard ratio; IRAC = Independent Response Adjudication Committee; M = melphalan; P = prednisone; R = lenalidomide; Rd Continuous = Rd given until documentation of progressive disease; Rd18 = Rd given for ≤ 18 cycles; T = thalidomide.
Kaplan-Meier Curves of Overall Survival (ITT MM Population) Between Arms Rd Continuous, Rd18 and MPT Cutoff date: 03 Mar 2014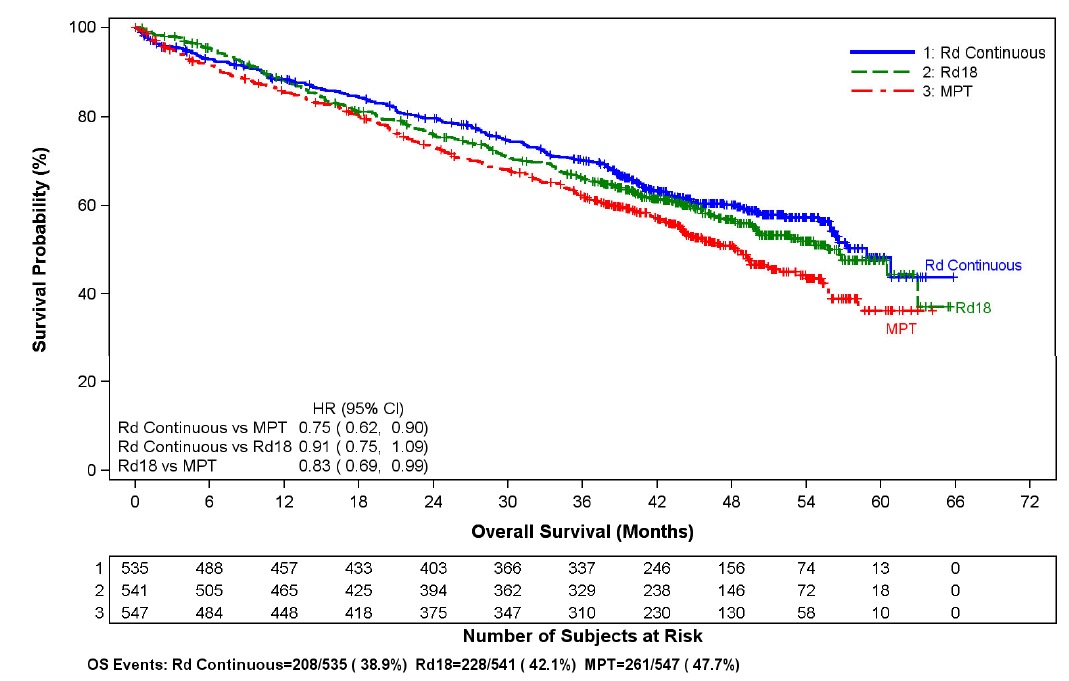
CI = confidence interval; d = low-dose dexamethasone; HR = hazard ratio; M = melphalan; P = prednisone; R = lenalidomide; Rd Continuous = Rd given until documentation of progressive disease; Rd18 = Rd given for ≤18 cycles; T = thalidomide.
Randomized, Placebo-Controlled Clinical Trials - Maintenance Following Auto-HSCT:Two multicenter, randomized, double-blind, parallel group, placebo-controlled studies were conducted to evaluate the efficacy and safety of lenalidomide maintenance therapy in the treatment of MM patients after auto-HSCT. In Maintenance Study 1, patients between 18 and 70 years of age who had undergone induction therapy followed by auto-HSCT were eligible. Induction therapy must have occurred within 12 months. Within 90 to 100 days after auto-HSCT, patients with at least a stable disease response were randomized 1:1 to receive either lenalidomide or placebo maintenance. In Maintenance Study 2, patients aged < 65 years at diagnosis who had undergone induction therapy followed by auto-HSCT and had achieved at least a stable disease response at the time of hematologic recovery were eligible. Within 6 months after auto-HSCT, patients were randomized 1:1 to receive either lenalidomide or placebo maintenance. Patients eligible for both trials had to have CLcr ≥30 mL/minute.
In both studies, the lenalidomide maintenance dose was 10 mg once daily on days 1 to 28 of repeated 28-day cycles, could be increased to 15 mg once daily after 3 months in the absence of dose-limiting toxicity, and treatment was to be continued until disease progression or patient withdrawal for another reason. The dose was reduced, or treatment was temporarily interrupted or stopped, as needed to manage toxicity. A dose increase to 15 mg once daily occurred in 135 patients (58%) in Maintenance Study 1, and in 185 patients (60%) in Maintenance Study 2.
The demographics and disease-related baseline characteristics of the patients were similar across the two studies and reflected a typical MM population after auto- HSCT (see Table 14).
Table 14: Baseline Demographic and Disease-Related Characteristics – MM Maintenance Studies 1 and 2Maintenance Study 1Maintenance Study 2LenalidomideN = 231
PlaceboN = 229LenalidomideN = 307
PlaceboN = 307Age (years)Median 58 58 57.5 58.1 (Min, max) (29, 71) (39, 71) (22.7, 68.3) (32.3, 67) Sex, n (%)Male 121 (52) 129 (56) 169 (55) 181 (59) Female 110 (48) 100 (44) 138 (45) 126 (41) ISS Stage at Diagnosis, n (%)Stage I or II 120 (52) 131 (57) 232 (76) 250 (81) Stage I62 (27) 85 (37) 128 (42) 143 (47) Stage II58 (25) 46 (20) 104 (34) 107 (35) Stage III 39 (17) 35 (15) 66 (21) 46 (15) Missing 72 (31) 63 (28) 9 (3) 11 (4) CrCl at Post-auto-HSCT, n (%)< 50 mL/min 23 (10) 16 (7) 10 (3) 9 (3) ≥ 50 mL/min 201 (87) 204 (89) 178 (58) 200 (65) Missing 7 (3) 9 (4) 119 (39) 98 (32) Data cutoff date = 1 March 2015.
The major efficacy endpoint of both studies was PFS defined from randomization to the date of progression or death, whichever occurred first; the individual studies were not powered for an overall survival endpoint. Both studies were unblinded upon the recommendations of their respective data monitoring committees and after surpassing the respective thresholds for preplanned interim analyses of PFS. After unblinding, patients continued to be followed as before. Patients in the placebo arm of Maintenance Study 1 were allowed to cross over to receive lenalidomide before disease progression (76 patients [33%] crossed over to lenalidomide); patients in Maintenance Study 2 were not recommended to cross over. The efficacy results are summarized in the following table. In both studies, the primary analysis of PFS at unblinding was significantly longer with lenalidomide compared to placebo: Maintenance Study 1 HR 0.38 (95% CI: 0.27 to 0.54 p <0.001) and Maintenance Study 2 HR 0.50 (95% CI: 0.39 to 0.64 p <0.001). For both studies, PFS was updated with a cutoff date of 1 March 2015 as shown in the table and the following Kaplan Meier graphs. With longer follow-up (median 72.4 and 86.0 months, respectively), the updated PFS analyses for both studies continue to show a PFS advantage for lenalidomide compared to placebo: Maintenance Study 1 HR 0.38 (95% CI: 0.28 to 0.50) with median PFS of 68.6 months and Maintenance Study 2 HR 0.53 (95% CI: 0.44 to 0.64) with median PFS of 46.3 months.
Descriptive analysis of OS data with a cutoff date of 1 February 2016 are provided in Table 15. Median follow-up time was 81.6 and 96.7 months for Maintenance Study 1 and Maintenance Study 2, respectively. Median OS was 111.0 and 84.2 months for lenalidomide and placebo, respectively, for Maintenance Study 1, and 105.9 and 88.1 months, for lenalidomide and placebo, respectively, for Maintenance Study 2.
Table 15: Progression-free Survival and Overall Survival from Randomization in MM Maintenance Studies 1 and 2 (ITT Post-Auto-HSCT Population)Maintenance Study 1Maintenance Study 2LenalidomideN = 231Placebo N = 229LenalidomideN = 307Placebo N = 307PFS at UnblindingPFS Events n (%)
46 (20) 98 (43) 103 (34) 160 (52) Median in months [95% CI] 33.9
[NE, NE]
19
[16.2, 25.6]
41.2
[38.3, NE]
23.0
[21.2, 28.0]
Hazard Ratio [95% CI] 0.38
[0.27, 0.54]
0.50
[0.39, 0.64]
Log-rank Test p-value <0.001 <0.001 PFS at Updated Analysis1 March 2015 (Studies 1 and 2)PFS Events n (%) 97 (42) 116 (51) 191 (62) 248 (81) Median in months [95% CI] 68.6
[52.8, NE]
22.5
[18.8, 30.0]
46.3
[40.1, 56.6]
23.8
[21.0, 27.3]
Hazard Ratio [95% CI] 0.38
[0.28, 0.50]
0.53
[0.44, 0.64]
OS at Updated Analysis1 Feb 2016 (Studies 1 and 2)OS Events n (%) 82 (35) 114 (50) 143 (47) 160 (52) Median in months [95% CI] 111
[101.8, NE]
84.2
[71.0, 102.7]
105.9
[88.8, NE]
88.1
[80.7, 108.4]
Hazard Ratio [95% CI] 0.59
[0.44, 0.78]
0.90
[0.72, 1.13]
Date of Unblinding in Maintenance Study 1 and 2 = 17 December 2009 and 7 July 2010, respectively.
Auto-HSCT = autologous hematopoietic stem cell transplantation; CI = confidence interval; ITT = intent to treat; NE = not estimable;
PFS = progression-free survival.
PFS at time of unblinding for Maintenance Study 2 was based on assessment by an Independent Review Committee. All other PFS
analyses were based on assessment by investigator.
Note: The median is based on Kaplan-Meier estimate, with 95% CIs about the median overall PFS time. Hazard ratio is based on a proportional hazards model stratified by stratification factors comparing the hazard functions associated with treatment arms (lenalidomide: placebo).
Kaplan-Meier Curves of Progression-free Survival from Randomization (ITT Post-Auto-HSCT Population) in MM Maintenance Study 1 between lenalidomide and Placebo Arms (Updated Cutoff Date 1 March 2015)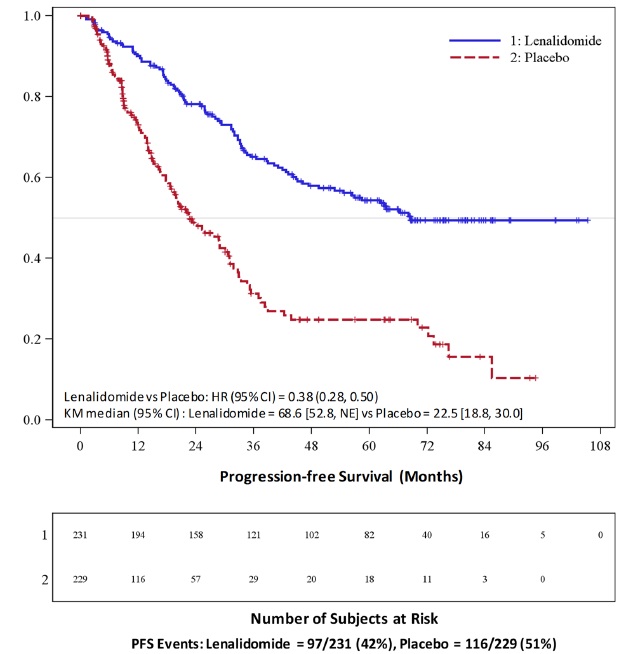
Auto-HSCT = autologous hematopoietic stem cell transplantation; CI = confidence interval; HR = hazard ratio; ITT = intent to treat; KM = Kaplan-Meier; PFS = progression-free survival; vs = versus.
Kaplan-Meier Curves of Progression-free Survival from Randomization (ITT Post-Auto-HSCT Population) in MM Maintenance Study 2 between lenalidomide and Placebo Arms (Updated Cutoff Date 1 March 2015)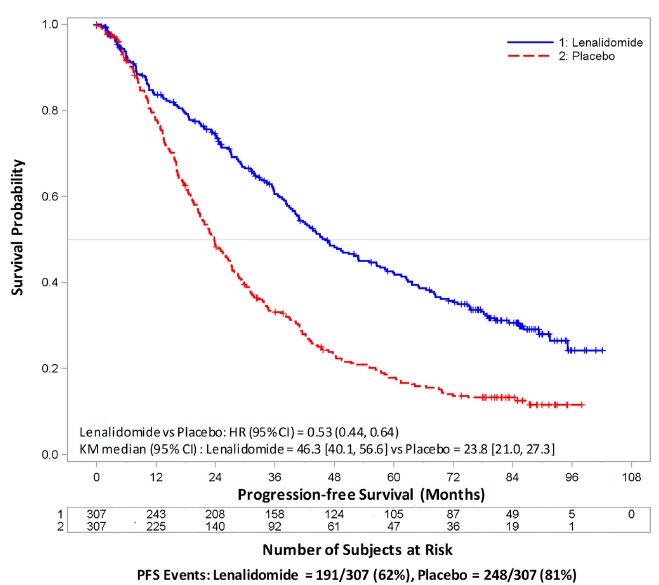
Auto-HSCT = autologous hematopoietic stem cell transplantation; CI = confidence interval; HR = hazard ratio; ITT = intent to treat; KM = Kaplan-Meier; NE = not estimable; PFS = progression-free survival; vs = versus.
Randomized, Open-Label Clinical Studies in Patients with MM After At Least One Prior TherapyTwo randomized studies (Studies 1 and 2) were conducted to evaluate the efficacy and safety of lenalidomide. These multicenter, multinational, double-blind, placebo-controlled studies compared lenalidomide plus oral pulse high-dose dexamethasone therapy to dexamethasone therapy alone in patients with MM who had received at least one prior treatment. These studies enrolled patients with absolute neutrophil counts (ANC) ≥ 1, 000/mm3, platelet counts ≥ 75,000/mm3, serum creatinine ≤ 2.5 mg/dL, serum SGOT/AST or SGPT/ALT ≤ 3 × upper limit of normal (ULN), and serum direct bilirubin ≤ 2 mg/dL.
In both studies, patients in the lenalidomide/dexamethasone group took 25 mg of lenalidomide orally once daily on Days 1 to 21 and a matching placebo capsule once daily on Days 22 to 28 of each 28-day cycle. Patients in the placebo/dexamethasone group took 1 placebo capsule on Days 1 to 28 of each 28-day cycle.
Patients in both treatment groups took 40 mg of dexamethasone orally once daily on Days 1 to 4, 9 to 12, and 17 to 20 of each 28-day cycle for the first 4 cycles of therapy.
The dose of dexamethasone was reduced to 40 mg orally once daily on Days 1 to 4 of each 28-day cycle after the first 4 cycles of therapy. In both studies, treatment was to continue until disease progression.
In both studies, dose adjustments were allowed based on clinical and laboratory findings. Sequential dose reductions to 15 mg daily, 10 mg daily and 5 mg daily were allowed for toxicity
[see Dosage and Administration (2.1)].Table 16 summarizes the baseline patient and disease characteristics in the two studies. In both studies, baseline demographic and disease-related characteristics were comparable between the lenalidomide/dexamethasone and placebo/dexamethasone groups.
Table 16: Baseline Demographic and Disease-Related Characteristics – MM Studies 1 and 2Study 1Study 2Lenalidomide/DexN=177Placebo/DexN=176Lenalidomide/DexN=176Placebo/DexN=175Patient CharacteristicsAge (years) Median 64 62 63 64 Min, Max 36, 86 37, 85 33, 84 40, 82 Sex Male 106 (60%) 104 (59%) 104 (59%) 103 (59%) Female 71 (40%) 72 (41%) 72 (41%) 72 (41%) Race/Ethnicity White 141(80%) 148 (84%) 172 (98%) 175 (100%) Other 36 (20%) 28 (16%) 4 (2%) 0 (0%) ECOG Performance Status 0 to 1 157 (89%) 168 (95%) 150 (85%) 144 (82%) Disease CharacteristicsMultiple Myeloma Stage (Durie-Salmon) I 3% 3% 6% 5% II 32% 31% 28% 33% III 64% 66% 65% 63% β2-microglobulin (mg/L) ≤ 2.5 mg/L 52 (29%) 51 (29%) 51 (29%) 48 (27%) > 2.5 mg/L 125 (71%) 125 (71%) 125 (71%) 127 (73%) Number of Prior Therapies1 38% 38% 32% 33% ≥ 2 62% 62% 68% 67% Types of Prior TherapiesStem Cell Transplantation 62% 61% 55% 54% Thalidomide 42% 46% 30% 38% Dexamethasone 81% 71% 66% 69% Bortezomib 11% 11% 5% 4% Melphalan 33% 31% 56% 52% Doxorubicin 55% 51% 56% 57% The primary efficacy endpoint in both studies was time to progression (TTP). TTP was defined as the time from randomization to the first occurrence of progressive disease.
Preplanned interim analyses of both studies showed that the combination of lenalidomide/dexamethasone was significantly superior to dexamethasone alone for TTP. The studies were unblinded to allow patients in the placebo/dexamethasone group to receive treatment with the lenalidomide/dexamethasone combination. For both studies, the extended follow-up survival data with crossovers were analyzed. In study 1, the median survival time was 39.4 months (95% CI: 32.9, 47.4) in lenalidomide/dexamethasone group and 31.6 months (95% CI: 24.1, 40.9) in placebo/dexamethasone group, with a hazard ratio of 0.79 (95% CI: 0.61 to 1.03). In study 2, the median survival time was 37.5 months (95%CI: 29.9, 46.6) in lenalidomide/dexamethasone group and 30.8 months (95% CI: 23.5, 40.3) in placebo/dexamethasone group, with a hazard ratio of 0.86 (95% CI: 0.65 to 1.14).
Table 17: TTP Results in MM Study 1 and Study 2Study 1Study 2Lenalidomide/Dex N=177Placebo/Dex N=176Lenalidomide/Dex N=176Placebo/Dex N=175TTPEvents n (%) 73 (41) 120 (68) 68 (39) 130 (74) Median TTP in months [95% CI] 13.9 [9.5, 18.5] 4.7 [3.7, 4.9] 12.1 [9.5, NE] 4.7 [3.8, 4.8] Hazard Ratio [95% CI] 0.285 [0.210, 0.386] 0.324 [0.240, 0.438] Log-rank Test p-value 3 <0.001 <0.001 ResponseComplete Response (CR) n (%) 23 (13) 1 (1) 27 (15) 7 (4) Partial Response (RR/PR) n (%) 84 (48) 33 (19) 77 (44) 34 (19) Overall Response n (%) 107 (61) 34 (19) 104 (59) 41 (23) p-value <0.001 <0.001 Odds Ratio [95% CI] 6.38 [3.95, 10.32] 4.72 [2.98, 7.49] Kaplan-Meier Estimate of Time to Progression — MM Study 1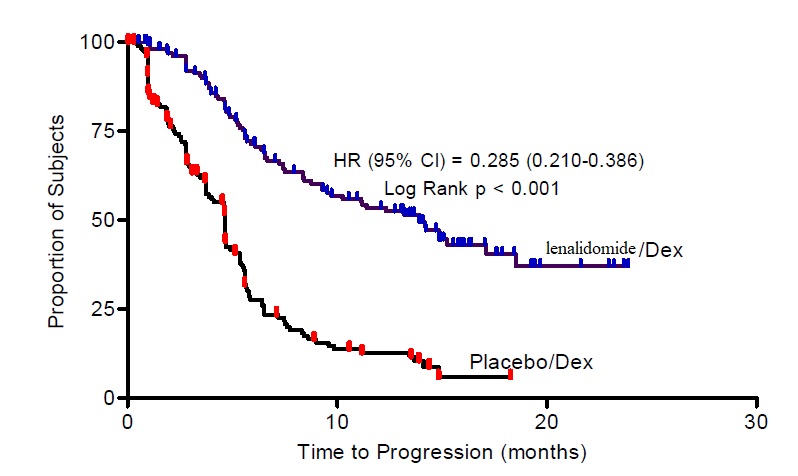 Kaplan-Meier Estimate of Time to Progression — MM Study 2
Kaplan-Meier Estimate of Time to Progression — MM Study 2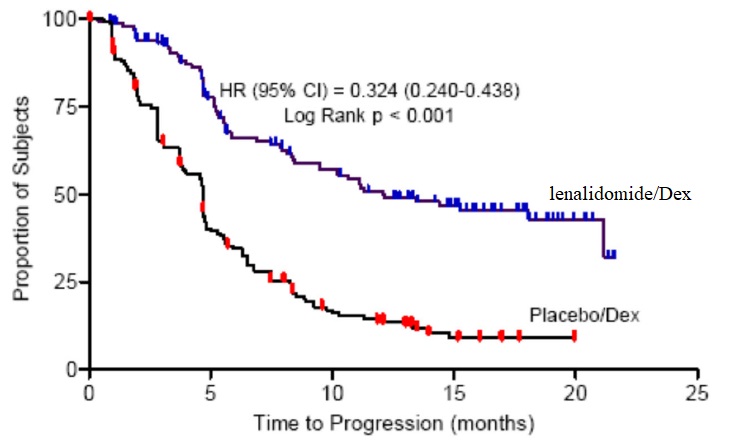 ).
).14.4 Follicular and Marginal Zone LymphomaThe efficacy of lenalidomide with rituximab in patients with relapsed or refractory follicular and marginal zone lymphoma was evaluated in the AUGMENT (NCT01938001) and MAGNIFY (NCT01996865) trials.
AUGMENT is a randomized, double-blind, multicenter trial (n=358) in which patients with relapsed or refractory follicular or marginal zone lymphoma were randomized 1:1 to receive lenalidomide and rituximab or rituximab and placebo. AUGMENT included patients diagnosed with Grade 1, 2, or 3a follicular lymphoma, who received at least 1 prior systemic therapy, were refractory or relapsed, not rituximab-refractory, had at least one measurable nodal or extranodal lesion by CT or MRI scan, and had adequate bone marrow, liver, and renal function. Randomization was stratified by follicular versus marginal zone lymphoma, previous rituximab therapy, and time since other anti-lymphoma therapy. In AUGMENT, lenalidomide was administered orally 20 mg once daily for Days 1 to 21 of repeating 28-day cycles for a maximum of 12 cycles or until unacceptable toxicity. The dose of rituximab was 375 mg/m2every week in Cycle 1 (Days 1, 8, 15, and 22) and on Day 1 of every 28-day cycle from Cycles 2 through 5. All dosage calculations for rituximab were based on the patient’s body surface area (BSA), using actual patient weight. Dose adjustments for lenalidomide were allowed based on clinical and laboratory findings. A patient with moderate renal insufficiency (≥30 to <60 mL/minute) received a lower lenalidomide starting dose of 10 mg daily on the same schedule. After 2 cycles, the lenalidomide dose could be increased to 15 mg once daily on Days 1 to 21 of each 28-day cycle if the patient tolerated the medication.
MAGNIFY is an open-label, multicenter trial (n=232) in which patients with relapsed or refractory follicular, marginal zone, or mantle cell lymphoma received 12 induction cycles of lenalidomide and rituximab. MAGNIFY included patients diagnosed with Grade 1, 2,3a, 3b follicular (including transformed), marginal zone, or mantle cell lymphoma Stage I to IV who were previously treated for their lymphoma, had been refractory or had a relapse after their last treatment, had at least one measurable nodal or extranodal lesion by CT or MRI scan, and had adequate bone marrow, liver, and renal function. Patients refractory to rituximab were also included. The information from the subjects who received at least 1 dose of initial therapy in the first 12 induction cycles (n=222) in the MAGNIFY trial was included in the evaluation of the efficacy of lenalidomide /rituximab in patients with relapsed or refractory follicular and marginal zone lymphoma. In MAGNIFY, lenalidomide 20 mg was given on Days 1 to 21 of repeated 28-day cycles for up to 12 cycles or until unacceptable toxicity, progression, or withdrawal of consent. The dose of rituximab was 375 mg/m2every week in Cycle 1 (Days 1, 8, 15, and 22) and on Day 1 of every other 28-day cycle (Cycles 3,5,7,9, and 11) up to 12 cycles therapy. All dosage calculations for rituximab were based on the patient BSA and actual weight. Dose adjustments were allowed based on clinical and laboratory findings.
The demographic and disease-related baseline characteristics in the AUGMENT and MAGNIFY trials are shown in the following table.
Table 21: Baseline Demographics and Disease-Related Characteristics of Patients with FL and MZL in AUGMENT and MAGNIFY TrialsParameterAUGMENT TrialMAGNIFY TrialLenalidomide + Rituximab (N=178)Rituximab + Placebo(Control Arm)(N=180)Lenalidomide + Rituximab (N=222)Age (years) Median (Max, Min) 64 (26, 86) 62 (35, 88) 65 (35, 91) Age distribution, n (%) <65 years 96 (54) 107 (59) 103 (46) ≥65 years 82 (46) 73 (41) 119 (54) Sex, n (%) Male 75 (42) 97 (54) 122 (55) Female 103 (58) 83 (46) 100 (45) Race White 118 (66) 115 (64) 206 (93) Other races 54 (30) 64 (36) 14 (6) Not collected or reported 6 (3) 1 (0.6) 2 (1) Body Surface Area (BSA, m2) Median (Max, Min) 1.8 (1.4, 3.1) 1.8 (1.3, 2.7) 2 (1.3, 2.6) Disease Type FL or MZL Follicular lymphoma 147 (83) 148 (82) 177 (80) Marginal zone lymphoma 31 (17) 32 (18) 45 (20) MZL subtype at diagnosis (investigator), n (%) MALT 14 (45) 16 (50) 10 (22) Nodal 8 (26) 10 (31) 25 (56) Splenic 9 (29) 6 (19) 10 (22) FL stage at diagnosis (investigator), n (%) FL Grade 1-2 125 (85) 123 (83) 149 (84) FL Grade 3a 22 (15) 25 (17) 28 (16) FLIPI score at baseline (calculated), n (%) Not Collected ParameterAUGMENT TrialMAGNIFY TrialLenalidomide + Rituximab (N=178)Rituximab + Placebo(Control Arm)(N=180)Lenalidomide + Rituximab (N=222)Low risk (0,1) 52 (29) 67 (37) Intermediate risk (2) 55 (31) 58 (32) High risk (≥3) 69 (39) 54 (30) Missing 2 (1) 1 (0.6) ECOG score at baseline, n (%) 0 116 (65) 128 (71) 102 (46) 1 60 (34) 50 (28) 113 (51) 2 2 (1) 2 (1) 7 (3) High tumor burdenaat baseline, n (%) Yes 97 (54) 86 (48) 148 (67) No 81 (46) 94 (52) 74 (33) Number of prior systemic antilymphoma therapies 1 102 (57) 97 (54) 94 (42)b >1 76 (43) 83 (46) 128 (58) Data Cutoff: 22 June 2018 (AUGMENT) and 1 May 2017 (MAGNIFY).
a Defined by GELF criteria.
b Patient had either 0 (n=2) or 1 prior systemic therapy.
ECOG = Eastern Cooperative Oncology Group; FLIPI = follicular lymphoma international prognostic index
In AUGMENT, efficacy was established in the intent-to-treat (ITT) population based on progression-free survival by Independent Review Committee using modified 2007 International Working Group response criteria. Efficacy results are summarized in Table 22.
Table 22: Efficacy Results for Patients in the AUGMENT Trial (ITT FL and MZL Population)ParameterLenalidomide + Rituximab (N=178)Rituximab + Placebo (N=180)PFSPatients with event, n (%) 68 (38.2) 115 (63.9) Death 6 (8.8) 2 (1.7) Progression of disease 62 (91.2) 113 (98.3) PFS, mediana[95% CI] (months) 39.4 [ 22.9, NE] 14.1 [11.4, 16.7] HR b[95% CI]0.46 [ 0.34, 0.62] p-valuec <0.0001 Objective response (CR+PR) , n(%)[95% CI]d138 (77.5) [70.7, 83.4] 96 (53.3) [45.8, 60.8] aMedian estimate is from Kaplan-Meier analysis.
b hazard ratio and its CI were estimated from Cox proportional hazard model adjusting for the stratification 3: previous rituximab treatment (yes, no), time since last antilymphoma therapy (≤ 2, > 2 years), and disease histology (FL, MZL).
cp-value from log-rank test stratified by 3 factors noted above: previous rituximab treatment (yes, no), time since last antilymphoma therapy (≤ 2, > 2 years), and disease histology (FL, MZL).
dExact confidence interval for binomial distribution.
Kaplan-Meier Curves of Progression-free Survival by IRC Assessment Between Arms in AUGMENT Trial (ITT FL and MZL Population)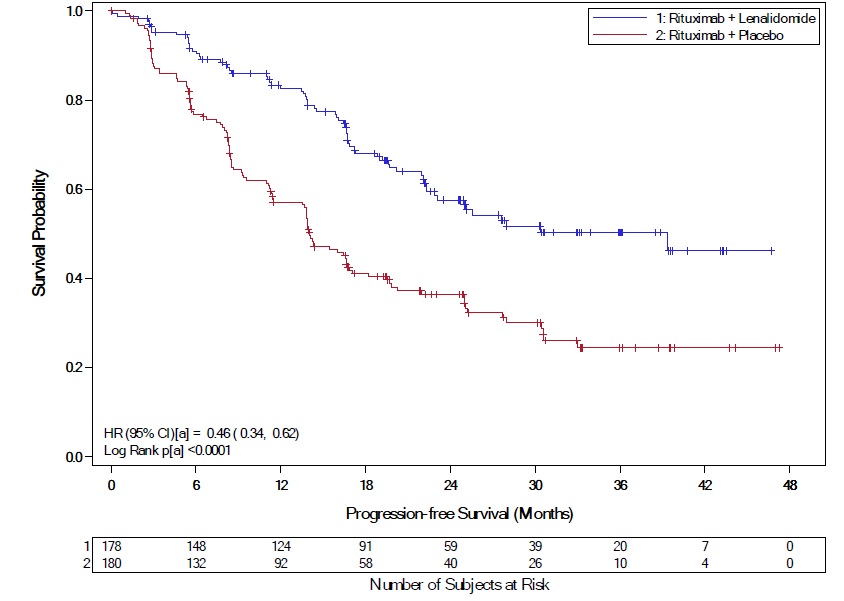
a = Stratification factors included: previous rituximab treatment (y/n), time since last anti-lymphoma therapy (≤2 years, >2years), and disease histology (FL or MZL).
CI = confidence interval; HR = hazard ratio; KM = Kaplan-Meier; PFS = progression-free survival
Follicular LymphomaIn AUGMENT, the objective response by IRC assessment for patients with follicular lymphoma was 80% (118/147) [95% CI: 73%, 86%]) in lenalidomide with rituximab arm compared to 55% (82/148) [95% CI: 47, 64] in control arm.
In MAGNIFY, the overall response by investigator assessment was 59% (104/177) [95% CI: 51, 66] for patients with follicular lymphoma. Median duration of response was not reached with a median follow-up time of 7.9 months [95% CI: 4.6, 9.2].
Marginal Zone LymphomaIn AUGMENT, the objective response by IRC assessment for patients with marginal zone lymphoma was 65% (20/31) [95% CI: 45%, 81%] in lenalidomide with rituximab arm compared to 44% (14/32) [95% CI: 26%, 62%] in control arm.
In MAGNIFY, the overall response by investigator assessment was 51% (23/45) [95% CI: 36, 66] for patients with marginal zone lymphoma. Median duration of response was not reached with a median follow-up time of 11.5 months [95% CI: 8.0, 18.9].
Capsules:
2.5 mg: Hard gelatin capsule with blue-green opaque cap and white opaque body; imprinted with “Biocon Logo” on the cap and “2.5 mg” on the body with black ink.
5 mg: Hard gelatin capsule with white opaque cap and white opaque body; imprinted with “Biocon Logo” on the cap and “5 mg” on the body with black ink.
10 mg: Hard gelatin capsule with blue-green opaque cap and pale yellow opaque body; imprinted with “Biocon Logo” on the cap and “10 mg” on the body with black ink.
15 mg: Hard gelatin capsule with powder blue opaque cap and white opaque body; imprinted with “Biocon Logo” on the cap and “15 mg” on the body with black ink.
20 mg: Hard gelatin capsule with blue-green opaque cap and powder blue opaque body; imprinted with “Biocon Logo” on the cap and “20 mg” on the body with black ink.
25 mg: Hard gelatin capsule with white opaque body and white opaque cap imprinted with “Biocon Logo” on the cap and “25 mg” on the body with black ink.
Lactation: Advise not to breastfeed (
).8.2 LactationRisk SummaryThere is no information regarding the presence of lenalidomide in human milk, the effects of lenalidomide on the breastfed child, or the effects of lenalidomide on milk production. Because many drugs are excreted in human milk and because of the potential for adverse reactions in breastfed children from lenalidomide, advise women not to breastfeed during treatment with lenalidomide.