Lutera - Levonorgestrel And Ethinyl Estradiol
(Levonorgestrel And Ethinyl Estradiol)Lutera - Levonorgestrel And Ethinyl Estradiol Prescribing Information
Lutera is indicated for the prevention of pregnancy in women who elect to use oral contraceptives as a method of contraception.
Oral contraceptives are highly effective. Table II lists the typical accidental pregnancy rates for users of combination oral contraceptives and other methods of contraception. The efficacy of these contraceptive methods, except sterilization, the IUD, and Norplant® System, depends upon the reliability with which they are used. Correct and consistent use of methods can result in lower failure rates.
| % of Women Experiencing an Unintended Pregnancy within the First Year of Use | % of Women Continuing Use at One YearAmong couples attempting to avoid pregnancy, the percentage who continue to use a method for one year. | ||
|---|---|---|---|
| Method | Typical UseAmong typical couples who initiate use of a method (not necessarily for the first time), the percentage who experience an accidental pregnancy during the first year if they do not stop use for any other reason. | Perfect UseAmong couples who initiate use of a method (not necessarily for the first time) and who use it perfectly (both consistently and correctly), the percentage who experience and accidental pregnancy during the first year if they do not stop use for any other reason. | |
| (1) | (2) | (3) | (4) |
| Emergency Contraceptive Pills: The FDA has concluded that certain combined oral contraceptives containing ethinyl estradiol and norgestrel or levonorgestrel are safe and effective for use as postcoital emergency contraception. Treatment initiated within 72 hours after unprotected intercourse reduces the risk of pregnancy by at least 75%.The treatment schedule is one dose within 72 hours after unprotected intercourse, and a second dose 12 hours after the first dose. The FDA has declared the following dosage regimens of oral contraceptives to be safe and effective for emergency contraception: for tablets containing 50 mcg of ethinyl estradiol and 500 mcg norgestrel 1 dose is 2 tablets; for tablets containing 20 mcg of ethinyl estradiol and 100 mcg of levonorgestrel 1 dose is 5 tablets; for tablets containing 30 mcg of ethinyl estradiol and 150 mcg of levonorgestrel 1 dose is 4 tablets. | |||
| Lactation Amenorrhea Method: LAM is a highly effective, temporary method of contraception.However, to maintain effective protection against pregnancy, another method of contraception must be used as soon as menstruation resumes, the frequency or duration of breastfeeds is reduced, bottle feeds are introduced, or the baby reaches 6 months of age. | |||
| Source: Trussell J. Contraceptive efficacy. In: Hatcher RA, Trussell J, Stewart F, Cates W, Stewart GK, Kowel D, Gust F. Contraceptive Technology: Seventeenth Revised Edition. New York NY: Irvington Publishers; 1998. | |||
| ChanceThe percents becoming pregnant in columns (2) and (3) are based on data from populations where contraception is not used and from women who cease using contraception in order to become pregnant. Among such populations, about 89% become pregnant within one year. This estimate was lowered slightly (to 85%) to represent the percent who would become pregnant within one year among women now relying on reversible methods of contraception if they abandoned contraception altogether. | 85 | 85 | |
| SpermicidesFoams, creams, gels, vaginal suppositories, and vaginal film. | 26 | 6 | 40 |
| Periodic abstinence | 25 | 63 | |
| Calendar | 9 | ||
| Ovulation Method | 3 | ||
| Sympto-ThermalCervical mucus (ovulation) method supplemented by calendar in the pre-ovulatory and basal body temperature in the post-ovulatory phases. | 2 | ||
| Post-Ovulation | 1 | ||
| CapWith spermicidal cream or jelly. | |||
| Parous Women | 40 | 26 | 42 |
| Nulliparous Women | 20 | 9 | 56 |
| Sponge | |||
| Parous Women | 40 | 20 | 42 |
| Nulliparous Women | 20 | 9 | 56 |
| Diaphragm | 20 | 6 | 56 |
| Withdrawal | 19 | 4 | |
| CondomWithout spermicides. | |||
| Female (Reality) | 21 | 5 | 56 |
| Male | 14 | 3 | 61 |
| Pill | 5 | 71 | |
| Progestin only | 0.5 | ||
| Combined | 0.1 | ||
| IUD | |||
| Progesterone T | 2.0 | 1.5 | 81 |
| Copper T380A | 0.8 | 0.6 | 78 |
| LNg 20 | 0.1 | 0.1 | 81 |
| Depo-Provera® | 0.3 | 0.3 | 70 |
| Levonorgestrel Implants (Norplant®) | 0.05 | 0.05 | 88 |
| Female Sterilization | 0.5 | 0.5 | 100 |
| Male Sterilization | 0.15 | 0.10 | 100 |
In a clinical trial with levonorgestrel and ethinyl estradiol tablets, 1,477 subjects had 7,720 cycles of use and a total of 5 pregnancies were reported. This represents an overall pregnancy rate of 0.84 per 100 woman-years. This rate includes patients who did not take the drug correctly. One or more pills were missed during 1,479 (18.8%) of the 7,870 cycles; thus all tablets were taken during 6,391 (81.2%) of the 7,870 cycles. Of the total 7,870 cycles, a total of 150 cycles were excluded from the calculation of the Pearl index due to the use of backup contraception and/or missing 3 or more consecutive pills.
To achieve maximum contraceptive effectiveness, Lutera® (levonorgestrel and ethinyl estradiol tablets) must be taken exactly as directed and at intervals not exceeding 24 hours. The dosage of Lutera is one white tablet daily for 21 consecutive days, followed by one peach inert tablet daily for 7 consecutive days, according to the prescribed schedule. It is recommended that Lutera tablets be taken at the same time each day.
The dispenser should be kept in the wallet supplied to avoid possible fading of the pills. If the pills fade, patients should continue to take them as directed.
Lutera is contraindicated in females who are known to have or develop the following conditions:
- Thrombophlebitis or thromboembolic disorders
- A history of deep-vein thrombophlebitis or thromboembolic disorders
- Cerebrovascular or coronary artery disease (current or past history)
- Valvular heart disease with thrombogenic complications
- Thrombogenic rhythm disorders
- Hereditary or acquired thrombophilias
- Major surgery with prolonged immobilization
- Diabetes with vascular involvement
- Headaches with focal neurological symptoms
- Uncontrolled hypertension
- Current diagnosis of, or history of, breast cancer, which may be hormone-sensitive
- Carcinoma of the endometrium or other known or suspected estrogen-dependent neoplasia
- Undiagnosed abnormal genital bleeding
- Cholestatic jaundice of pregnancy or jaundice with prior pill use
- Hepatic adenomas or carcinomas, or active liver disease
- Known or suspected pregnancy
- Hypersensitivity to any of the components of Lutera
- Are receiving Hepatitis C drug combinations containing ombitasvir/paritaprevir/ritonavir, with or without dasabuvir, due to the potential for ALT elevations (see ).
5. RISK OF LIVER ENZYME ELEVATIONS WITH CONCOMITANT HEPATITIS C TREATMENTDuring clinical trials with the Hepatitis C combination drug regimen that contains ombitasvir/paritaprevir/ritonavir, with or without dasabuvir, ALT elevations greater than 5 times the upper limit of normal (ULN), including some cases greater than 20 times the ULN, were significantly more frequent in women using ethinyl estradiol-containing medications such as COCs. Discontinue Lutera prior to starting therapy with the combination drug regimen ombitasvir/paritaprevir/ritonavir, with or without dasabuvir [see
CONTRAINDICATIONS(4)]. Lutera can be restarted approximately 2 weeks following completion of treatment with the combination drug regimen.
Five studies that compared breast cancer risk between ever-users (current or past use) of COCs and never-users of COCs reported no association between ever use of COCs and breast cancer risk, with effect estimates ranging from 0.90 – 1.12 (Figure III).
Three studies compared breast cancer risk between current or recent COC users (<6 months since last use) and never users of COCs (Figure III). One of these studies reported no association between breast cancer risk and COC use. The other two studies found an increased relative risk of 1.19 – 1.33 with current or recent use. Both of these studies found an increased risk of breast cancer with current use of longer duration, with relative risks ranging from 1.03 with less than one year of COC use to approximate 1.4 with more than 8-10 years of COC use.
Figure III: Risk of Breast Cancer with Combined Oral Contraceptive Use
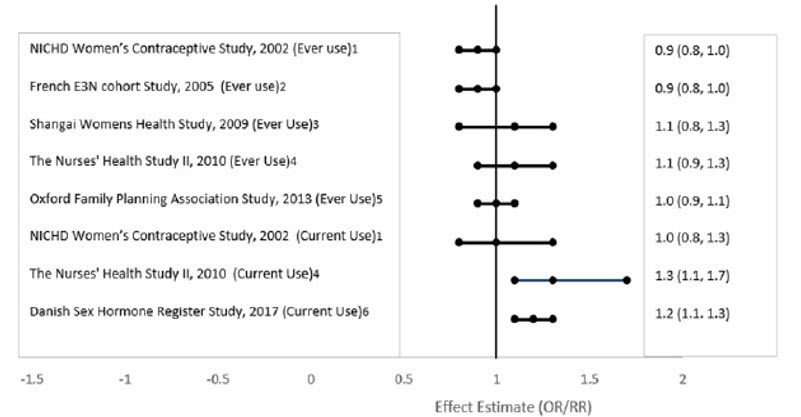
RR = relative risk; OR = odds ratio; HR = hazard ratio. "ever COC" are females with current or past COC use; "never COC use" are females that never used COCs.
An increased risk of the following serious adverse reactions (see
Cigarette smoking increases the risk of serious cardiovascular side effects from oral-contraceptive use. This risk increases with age and with the extent of smoking (in epidemiologic studies, 15 or more cigarettes per day was associated with a significantly increase risk) and is quite marked in women over 35 years of age. Women who use oral contraceptives should be strongly advised not to smoke. |
The use of oral contraceptives is associated with increased risks of several serious conditions including venous and arterial thrombotic and thromboembolic events (such as myocardial infarction, thromboembolism, and stroke), hepatic neoplasia, gallbladder disease, and hypertension, although the risk of serious morbidity or mortality is very small in healthy women without underlying risk factors. The risk of morbidity and mortality increases significantly in the presence of other underlying risk factors such as certain inherited or acquired thrombophilias, hypertension, hyperlipidemias, obesity, diabetes, and surgery or trauma with increased risk of thrombosis (see
Practitioners prescribing oral contraceptives should be familiar with the following information relating to these risks.
The information contained in this package insert is principally based on studies carried out in patients who used oral contraceptives with higher doses of estrogens and progestogens than those in common use today. The effect of long-term use of the oral contraceptives with lower doses of both estrogens and progestogens remains to be determined.
Throughout this labeling, epidemiological studies reported are of two types: retrospective or case control studies and prospective or cohort studies. Case control studies provide a measure of the relative risk of disease, namely, a ratio of the incidence of a disease among oral-contraceptive users to that among nonusers. The relative risk does not provide information on the actual clinical occurrence of a disease. Cohorts studies provide a measure of attributable risk, which is the difference in the incidence of disease between oral-contraceptive users and nonusers. The attributable risk does provide information about the actual occurrence of a disease in the population. For further information, the reader is referred to a text on epidemiological methods.
An increased risk of myocardial infarction has been attributed to oral-contraceptive use. This risk is primarily in smokers or women with other underlying risk factors for coronary-artery disease such as hypertension, hypercholesterolemia, morbid obesity, and diabetes. The relative risk of heart attack for current oral-contraceptive users has been estimated to be two to six. The risk is very low under the age of 30.
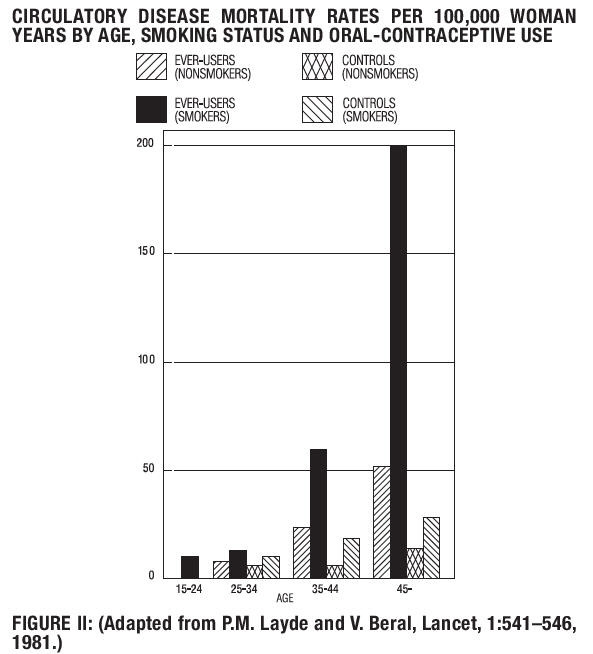
Smoking in combination with oral-contraceptive use has been shown to contribute substantially to the incidence of myocardial infarction in women in their mid-thirties or older with smoking accounting for the majority of excess cases. Mortality rates associated with circulatory disease have been shown to increase substantially in smokers over the age of 35 and nonsmokers over the age of 40 (FIGURE II) among women who use oral contraceptives.
Oral contraceptives may compound the effects of well-known risk factors, such as hypertension, diabetes, hyperlipidemias, age and obesity. In particular, some progestogens are known to decrease HDL cholesterol and cause glucose intolerance, while estrogens may create a state of hyperinsulinism. Oral contraceptives have been shown to increase blood pressure among users (see
An increased risk of venous thromboembolic and thrombotic disease associated with the use of oral contraceptives is well established. Case control studies have found the relative risk of users compared to non-users to be 3 for the first episode of superficial venous thrombosis, 4 to 11 for deep vein thrombosis or pulmonary embolism, and 1.5 to 6 for women with predisposing conditions for venous thromboembolic disease. Cohort studies have shown the relative risk to be somewhat lower, about 3 for new cases and about 4.5 for new cases requiring hospitalization. The approximate incidence of deep-vein thrombosis and pulmonary embolism in users of low dose (<50 mcg ethinyl estradiol) combination oral contraceptives is up to 4 per 10,000 women-years compared to 0.5-3 per 10,000 woman-years for non-users. However, the incidence is less than that associated with pregnancy (6 per 10,000 woman-years). The excess risk is highest during the first year a woman ever uses a combined oral contraceptive. Venous thromboembolism may be fatal. The risk of thromboembolic disease due to oral contraceptives is not related to length of use and disappears after pill use is stopped.
A two- to four-fold increase in relative risk of postoperative thromboembolic complications has been reported with the use of oral contraceptives. The relative risk of venous thrombosis in women who have predisposing conditions is twice that of women without such medical conditions. If feasible, oral contraceptives should be discontinued at least four weeks prior to and for two weeks after elective surgery of a type associated with an increase in risk of thromboembolism and during and following prolonged immobilization. Since the immediate post-partum period is also associated with an increased risk of thromboembolism, oral contraceptives should be started no earlier than four to six weeks after delivery in women who elect not to breast-feed, or a midtrimester pregnancy termination.
Oral contraceptives have been shown to increase both the relative and attributable risks of cerebrovascular events (thrombotic and hemorrhagic strokes), although, in general, the risk is greatest among older (>35 years), hypertensive women who also smoke. Hypertension was found to be a risk factor for both users and non-users, for both types of strokes, while smoking interacted to increase the risk for hemorrhagic strokes.
In a large study, the relative risk of thrombotic strokes has been shown to range from 3 for normotensive users to 14 for users with severe hypertension. The relative risk of hemorrhagic stroke is reported to be 1.2 for nonsmokers who used oral contraceptives, 2.6 for smokers who did not use oral contraceptives, 7.6 for smokers who used oral contraceptives, 1.8 for normotensive users and 25.7 for users with severe hypertension. The attributable risk is also greater in older women. Oral contraceptives also increase the risk for stroke in women with other underlying risk factors such as certain inherited or acquired thrombophilias. Women with migraine (particularly migraine/headaches with focal neurological symptoms, see
A positive association has been observed between the amount of estrogen and progestogen in oral contraceptives and the risk of vascular disease. A decline in serum high-density lipoproteins (HDL) has been reported with many progestational agents. A decline in serum high density lipoproteins has been associated with an increased incidence of ischemic heart disease. Because estrogens increase HDL cholesterol, the net effect of an oral contraceptive depends on a balance achieved between doses of estrogen and progestogen and the nature and absolute amount of progestogen used in the contraceptive. The amount of both hormones should be considered in the choice of an oral contraceptive.
Minimizing exposure to estrogen and progestogen is in keeping with good principles of therapeutics. For any particular estrogen/progestogen combination, the dosage regimen prescribed should be one which contains the least amount of estrogen and progestogen that is compatible with a low failure rate and the needs of the individual patient. New acceptors of oral contraceptive agents should be started on preparations containing less than 50 mcg of estrogen.
There are two studies which have shown persistence of risk of vascular disease for ever-users of oral contraceptives. In a study in the United States, the risk of developing myocardial infarction after discontinuing oral contraceptives persists for at least 9 years for women 40-49 years who had used oral contraceptives for five or more years, but this increased risk was not demonstrated in other age groups.
In another study in Great Britain, the risk of developing cerebrovascular disease persisted for at least 6 years after discontinuation of oral contraceptives, although excess risk was very small. However, both studies were performed with oral contraceptive formulations containing 50 mcg or higher of estrogens.
One study gathered data from a variety of sources which have estimated the mortality rate associated with different methods of contraception at different ages (TABLE III). These estimates include the combined risk of death associated with contraceptive methods plus the risk attributable to pregnancy in the event of method failure. Each method of contraception has its specific benefits and risks. The study concluded that with the exception of oral-contraceptive users 35 and older who smoke and 40 and older who do not smoke, mortality associated with all methods of birth control is less than that associated with childbirth. The observation of a possible increase in risk of mortality with age for oral-contraceptive users is based on data gathered in the 1970's—but not reported until 1983. However, current clinical practice involves the use of lower estrogen dose formulations combined with careful restriction of oral contraceptive use to women who do not have the various risk factors listed in this labeling.
Because of these changes in practice and, also, because of some limited new data which suggest that the risk of cardiovascular disease with the use of oral contraceptives may now be less than previously observed, the Fertility and Maternal Health Drugs Advisory Committee was asked to review the topic in 1989. The Committee concluded that although cardiovascular disease risks may be increased with oral- contraceptive use after age 40 in healthy non-smoking women (even with the newer low-dose formulations), there are greater potential health risks associated with pregnancy in older women and with the alternative surgical and medical procedures which may be necessary if such women do not have access to effective and acceptable means of contraception.
Therefore, the Committee recommended that the benefits of oral contraceptive use by healthy non- smoking women over 40 may outweigh the possible risks. Of course, older women, as all women who take oral contraceptives, should take the lowest possible dose formulation that is effective.
| Method of control and outcome | 15-19 | 20-24 | 25-29 | 30-34 | 35-39 | 40-44 |
|---|---|---|---|---|---|---|
| Adapted from H.W. Ory, Family Planning Perspectives, 15 :57-63, 1983. | ||||||
| No fertility-control methodsDeaths are birth related | 7.0 | 7.4 | 9.1 | 14.8 | 25.7 | 28.2 |
| Oral contraceptives nonsmokerDeaths are method related | 0.3 | 0.5 | 0.9 | 1.9 | 13.8 | 31.6 |
| Oral contraceptives smoker | 2.2 | 3.4 | 6.6 | 13.5 | 51.1 | 117.2 |
| IUD | 0.8 | 0.8 | 1.0 | 1.0 | 1.4 | 1.4 |
| Condom | 1.1 | 1.6 | 0.7 | 0.2 | 0.3 | 0.4 |
| Diaphragm/spermicide | 1.9 | 1.2 | 1.2 | 1.3 | 2.2 | 2.8 |
| Periodic abstinence | 2.5 | 1.6 | 1.6 | 1.7 | 2.9 | 3.6 |
Lutera is contraindicated in females who currently have or have had breast cancer because breast cancer may be hormonally sensitive [see
Epidemiology studies have not found a consistent association between use of combined oral contraceptives (COCs) and breast cancer risk. Studies do not show an association between ever (current or past) use of COCs and risk of breast cancer. However, some studies report a small increase in the risk of breast cancer among current or recent users (<6 months since last use) and current users with longer duration of COC use [see
Some studies suggest that oral contraceptive use has been associated with an increase in the risk of cervical intraepithelial neoplasia in some populations of women. However, there continues to be controversy about the extent to which such findings may be due to differences in sexual behavior and other factors.
In spite of many studies of the relationship between oral contraceptive use and breast and cervical cancers, a cause-and-effect relationship has not been established.
Benign hepatic adenomas are associated with oral-contraceptive use, although the incidence of these benign tumors is rare in the United States. Indirect calculations have estimated the attributable risk to be in the range of 3.3 cases/100,000 for users, a risk that increases after four or more years of use. Rupture of rare, benign, hepatic adenomas may cause death through intra-abdominal hemorrhage.
Studies from Britain have shown an increased risk of developing hepatocellular carcinoma in long-term (>8 years) oral-contraceptive users. However, these cancers are extremely rare in the U.S. and the attributable risk (the excess incidence) of liver cancers in oral-contraceptive users approaches less than one per million users.
During clinical trials with the Hepatitis C combination drug regimen that contains ombitasvir/paritaprevir/ritonavir, with or without dasabuvir, ALT elevations greater than 5 times the upper limit of normal (ULN), including some cases greater than 20 times the ULN, were significantly more frequent in women using ethinyl estradiol-containing medications such as COCs. Discontinue Lutera prior to starting therapy with the combination drug regimen ombitasvir/paritaprevir/ritonavir, with or without dasabuvir [see
There have been clinical case reports of retinal thrombosis associated with the use of oral contraceptives that may lead to partial or complete loss of vision. Oral contraceptives should be discontinued if there is unexplained partial or complete loss of vision; onset of proptosis or diplopia; papilledema; or retinal vascular lesions. Appropriate diagnostic and therapeutic measures should be undertaken immediately.
Extensive epidemiological studies have revealed no increased risk of birth defects in women who have used oral contraceptives prior to pregnancy. Studies also do not suggest a teratogenic effect particularly insofar as cardiac anomalies and limb-reduction defects are concerned, when taken inadvertently during early pregnancy (see
The administration of oral contraceptives to induce withdrawal bleeding should not be used as a test for pregnancy. Oral contraceptives should not be used during pregnancy to treat threatened or habitual abortion. It is recommended that for any patient who has missed two consecutive periods, pregnancy should be ruled out. If the patient has not adhered to the prescribed schedule, the possibility of pregnancy should be considered at the time of the first missed period. Oral contraceptive use should be discontinued if pregnancy is confirmed.
Combination oral contraceptives may worsen existing gallbladder disease and may accelerate the development of this disease in previously asymptomatic women. Earlier studies have reported an increased lifetime relative risk of gallbladder surgery in users of oral contraceptives and estrogens. More recent studies, however, have shown that the relative risk of developing gallbladder disease among oral contraceptive users may be minimal. The recent findings of minimal risk may be related to the use of oral-contraceptive formulations containing lower hormonal doses of estrogens and progestogens.
Oral contraceptives have been shown to cause glucose intolerance in a significant percentage of users. Oral contraceptives containing greater than 75 mcg of estrogens cause hyperinsulinism, while lower doses of estrogen cause less glucose intolerance. Progestogens increase insulin secretion and create insulin resistance, this effect varying with different progestational agents. However, in the nondiabetic woman, oral contraceptives appear to have no effect on fasting blood glucose. Because of these demonstrated effects, prediabetic and diabetic women should be carefully observed while taking oral contraceptives.
A small proportion of women will have persistent hypertriglyceridemia while on the pill. As discussed earlier (see
An increase in blood pressure has been reported in women taking oral contraceptives and this increase is more likely in older oral-contraceptive users and with continued use. Data from the Royal College of General Practitioners and subsequent randomized trials have shown that the incidence of hypertension increases with increasing quantities of progestogens.
Women with a history of hypertension or hypertension-related diseases, or renal disease should be encouraged to use another method of contraception. If women with hypertension elect to use oral contraceptives, they should be monitored closely and if significant elevation of blood pressure occurs, oral contraceptives should be discontinued (see
The onset or exacerbation of migraine or development of headache with a new pattern that is recurrent, persistent or severe requires discontinuation of oral contraceptives and evaluation of the cause. (See
Breakthrough bleeding and spotting are sometimes encountered in patients on oral contraceptives, especially during the first three months of use. The type and dose of progestogen may be important. If bleeding persists or recurs, nonhormonal causes should be considered and adequate diagnostic measures taken to rule out malignancy or pregnancy in the event of breakthrough bleeding, as in the case of any abnormal vaginal bleeding. If pathology has been excluded, time or a change to another formulation may solve the problem. In the event of amenorrhea, pregnancy should be ruled out.
Some women may encounter post-pill amenorrhea or oligomenorrhea, especially when such a condition was pre-existent.
Ectopic as well as intrauterine pregnancy may occur in contraceptive failures.
Thromboembolic and thrombotic disorders and other vascular problems (including thrombophlebitis and venous thrombosis with or without pulmonary embolism, mesenteric thrombosis, arterial thromboembolism, myocardial infarction, cerebral hemorrhage, cerebral thrombosis), carcinoma of the reproductive organs and breasts, hepatic neoplasia (including hepatic adenomas or benign liver tumors), ocular lesions (including retinal vascular thrombosis), gallbladder disease, carbohydrate and lipid effects, elevated blood pressure, and headache including migraine.
The following adverse reactions have been reported in patients receiving oral contraceptives and are believed to be drug related (alphabetically listed):
The following adverse reactions have been reported in users of oral contraceptives:
Contraceptive effectiveness may be reduced when hormonal contraceptives are coadministered with antibiotics, anticonvulsants, and other drugs that increase the metabolism of contraceptive steroids. This could result in unintended pregnancy or breakthrough bleeding. Examples include rifampin, rifabutin, barbiturates, primidone, phenylbutazone, phenytoin, dexamethasone, carbamazepine, felbamate, oxcarbazepine, topiramate, griseofulvin, and modafinil. In such cases a back-up nonhormonal method of birth control should be considered.
Several cases of contraceptive failure and breakthrough bleeding have been reported in the literature with concomitant administration of antibiotics such as ampicillin and other penicillins, and tetracyclines. However, clinical pharmacology studies investigating drug interactions between combined oral contraceptives and these antibiotics have reported inconsistent results.
Several of the anti-HIV protease inhibitors have been studied with co-administration of oral combination hormonal contraceptives; significant changes (increase and decrease) in the plasma levels of the estrogen and progestin have been noted in some cases. The safety and efficacy of oral contraceptive products may be affected with coadministration of anti-HIV protease inhibitors. Healthcare providers should refer to the label of the individual anti-HIV protease inhibitors for further drug-drug interaction information.
Herbal products containing St. John's Wort (Hypericum perforatum) may induce hepatic enzymes (cytochrome P 450) and p-glycoprotein transporter and may reduce the effectiveness of contraceptive steroids. This may also result in breakthrough bleeding.
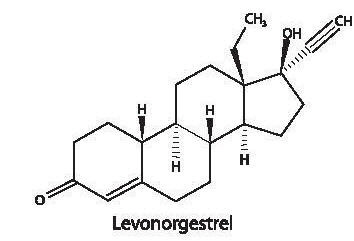
Each active, white tablet (21) contains 0.1 mg of levonorgestrel, d (-)-13β-ethyl-17α-ethinyl-17β- hydroxygon-4-en-3-one, a totally synthetic progestogen, and 0.02 mg of ethinyl estradiol, 17α-ethinyl- 1,3,5(10)-estratriene-3,17β-diol. The inactive ingredients present are croscarmellose sodium, lactose monohydrate, magnesium stearate, microcrystalline cellulose, and povidone.
Each inactive, peach tablet (7) contains the following inactive ingredients: FD&C Yellow #6, lactose anhydrous, lactose monohydrate, magnesium stearate, and microcrystalline cellulose.
 | 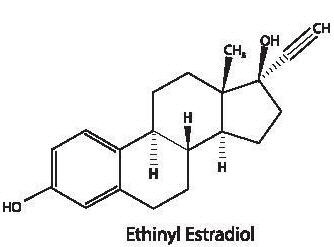 |
| C21H28O2 M.W. 312.45 | C20H24O2 M.W. 296.4 |