Nalmefene Hydrochloride
(Nalmefene Hydrochloride Injection)Nalmefene Hydrochloride Prescribing Information
Nalmefene Hydrochloride Injection is indicated for the complete or partial reversal of opioid drug effects, including respiratory depression, induced by either natural or synthetic opioids.
Nalmefene Hydrochloride Injection is indicated in the management of known or suspected opioid overdose.
Nalmefene Hydrochloride Injection is supplied in two concentrations that can be identified by their color coded container labels: a concentration suitable for postoperative use (100 µg/mL) in a blue labeled vial containing ONE (1) mL and a concentration suitable for the management of overdose (1 mg/mL, 10 times as concentrated, 20 times as much drug) in a green labeled vial containing TWO (2) mL. Proper steps should be taken to prevent use of the incorrect concentration.
Nalmefene hydrochloride injection should be titrated to reverse the undesired effects of opioids. Once adequate reversal has been established, additional administration is not required and may actually be harmful due to unwanted reversal of analgesia or precipitated withdrawal.
The duration of action of nalmefene hydrochloride injection is as long as most opioid analgesics. The apparent duration of action of nalmefene hydrochloride injection will vary, however, depending on the half-life and plasma concentration of the narcotic being reversed, the presence or absence of other drugs affecting the brain or muscles of respiration, and the dose of nalmefene hydrochloride injection administered.
Partially reversing doses of nalmefene hydrochloride injection (1 µg/kg) lose their effect as the drug is redistributed through the body, and the effects of these low doses may not last more than 30-60 minutes in the presence of persistent opioid effects. Fully reversing doses (1 mg/70 kg) have been shown to last many hours in both experimental and clinical studies, but may complicate the management of patients who are in pain, at high cardiovascular risk, or who are physically dependent on opioids.
The recommended doses represent a compromise between a desirable controlled reversal and the need for prompt response and adequate duration of action. Using higher dosages or shorter intervals between incremental doses is likely to increase the incidence and severity of symptoms related to acute withdrawal such as nausea, vomiting, elevated blood pressure, and anxiety.
Nalmefene hydrochloride injection may cause acute withdrawal symptoms in individuals who have some degree of tolerance to and dependence on opioids. These patients should be closely observed for symptoms of withdrawal following administration of the initial and subsequent injections of nalmefene hydrochloride injection. Subsequent doses should be administered with intervals of at least 2-5 minutes between doses to allow the full effect of each incremental dose of nalmefene hydrochloride injection to be reached.
Use 100 µg/mL dosage strength (blue label) and see Table 2 for initial doses.
The goal of treatment with nalmefene hydrochloride injection in the postoperative setting is to achieve reversal of excessive opioid effects without inducing a complete reversal and acute pain. This is best accomplished with an initial dose of 0.25 µg/kg followed by 0.25 µg/kg incremental doses at 2-5 minute intervals, stopping as soon as the desired degree of opioid reversal is obtained. A cumulative total dose above 1.0 µg/kg does not provide additional therapeutic effect.
Body Weight | mL of Nalmefene 100 µg/mL Solution |
50 kg | 0.125 |
60 kg | 0.150 |
70 kg | 0.175 |
80 kg | 0.200 |
90 kg | 0.225 |
100 kg | 0.250 |
In cases where the patient is known to be at increased cardiovascular risk, it may be desirable to dilute Nalmefene Hydrochloride Injection 1:1 with saline or sterile water and use smaller initial and incremental doses of 0.1 µg/kg.
Use 1.0 mg/mL dosage strength (green label).
The recommended initial dose of nalmefene hydrochloride injection for non-opioid dependent patients is 0.5 mg/70 kg. If needed, this may be followed by a second dose of 1.0 mg/70 kg, 2-5 minutes later. If a total dose of 1.5 mg /70 kg has been administered without clinical response, additional Nalmefene Hydrochloride Injection is unlikely to have an effect.
Patients should not be given more nalmefene hydrochloride injection than is required to restore the respiratory rate to normal, thus minimizing the likelihood of cardiovascular stress and precipitated withdrawal syndrome.
If there is a reasonable suspicion of opioid dependency, a challenge dose of nalmefene hydrochloride injection 0.1 mg/70 kg should be administered initially. If there is no evidence of withdrawal in 2 minutes, the recommended dosing should be followed.
Nalmefene hydrochloride injection had no effect in cases where opioids were not responsible for sedation and hypoventilation. Therefore, patients should only be treated with Nalmefene Hydrochloride Injection when the likelihood of an opioid overdose is high, based on a history of opioid overdose or the clinical presentation of respiratory depression with concurrent pupillary constriction.
Nalmefene hydrochloride injection is the longest acting of the currently available parenteral opioid antagonists. If recurrence of respiratory depression does occur, the dose should again be titrated to clinical effect using incremental doses to avoid over-reversal.
Hepatic disease and renal failure substantially reduce the clearance of nalmefene (see
Should intravenous access be lost or not readily obtainable, a pharmacokinetic study has shown that a single dose of nalmefene hydrochloride injection should be effective within 5-15 minutes after intramuscular or subcutaneous doses of 1.0 mg. (see
ELDERLY
Dose proportionality was observed in nalmefene AUC0-inf following 0.5 to 2 mg intravenous administration to elderly male subjects. Following a 1 mg intravenous nalmefene dose, there were no significant differences between young (19-32 years) and elderly (62-80 years) adult male subjects with respect to plasma clearance, steady-state volume of distribution, or half-life. There was an apparent age-related decrease in the central volume of distribution (young: 3.9 ± 1.1 L/kg, elderly: 2.8 ± 1.1 L/kg) that resulted in a greater initial nalmefene concentration in the elderly group. While initial nalmefene plasma concentrations were transiently higher in the elderly, it would not be anticipated that this population would require dosing adjustment. No clinical adverse events were noted in the elderly following the 1 mg intravenous nalmefene dose.
PATIENTS WITH HEPATIC IMPAIRMENT
Subjects with hepatic disease, when compared to matched normal controls, had a 28.3% decrease in plasma clearance of nalmefene (0.56 ± 0.21 L/hr/kg versus 0.78 ± 0.24 L/hr/kg, respectively). Elimination halflife increased from 10.2 ± 2.2 hours to 11.9 ± 2.0 hours in the hepatically impaired. No dosage adjustment is recommended since nalmefene will be administered as an acute course of therapy.
PATIENTS WITH RENAL IMPAIRMENT
There was a statistically significant 27% decrease in plasma clearance of nalmefene in the end-stage renal disease (ESRD) population during interdialysis (0.57 ± 0.20 L/hr/kg) and a 25% decreased plasma clearance in the ESRD population during intradialysis (0.59
GENDER DIFFERENCES
There has not been sufficient pharmacokinetic study to make a definitive statement as to whether the pharmacokinetics of nalmefene differs between the genders.
Nalmefene Hydrochloride Injection is contraindicated in patients with a known hypersensitivity to the product.
Adverse event information was obtained following administration of nalmefene hydrochloride injection to 152 normal volunteers and in controlled clinical trials to 1127 patients for the treatment of opioid overdose or for postoperative opioid reversal.
Nalmefene was well tolerated and showed no serious toxicity during experimental administration to healthy individuals, even when given at 15 times the highest recommended dose. In a small number of subjects, at doses exceeding the recommended nalmefene hydrochloride injection dose, nalmefene produced symptoms suggestive of reversal of endogenous opioids, such as have been reported for other narcotic antagonist drugs. These symptoms (nausea, chills, myalgia, dysphoria, abdominal cramps, and joint pain) were usually transient and occurred at very low frequency.
Such symptoms of precipitated opioid withdrawal at the recommended clinical doses were seen in both postoperative and overdose patients who were later found to have had histories of covert opioid use. Symptoms of precipitated withdrawal were similar to those seen with other opioid antagonists, were transient following the lower doses used in the postoperative setting, and more prolonged following the administration of the larger doses used in the treatment of overdose.
Tachycardia and nausea following the use of nalmefene in the postoperative setting were reported at the same frequencies as for naloxone at equivalent doses. The risk of both these adverse events was low at doses giving partial opioid reversal and increased with increases in dose. Thus, total doses larger than 1.0 µg/kg in the postoperative setting and 1.5 mg/70 kg in the treatment of overdose are not recommended.
(all patients, all clinical settings)
Adverse Event | Nalmefene | Naloxone | Placebo |
N=1127 | N=369 | N=77 | |
Nausea | 18% | 18% | 6% |
Vomiting | 9% | 7% | 4% |
Tachycardia | 5% | 8% | - |
Hypertension | 5% | 7% | - |
Postoperative pain | 4% | 4% | N/A |
Fever | 3% | 4% | - |
Dizziness | 3% | 4% | 1% |
Headache | 1% | 1% | 4% |
Chills | 1% | 1% | - |
Hypotension | 1% | 1% | - |
Vasodilatation | 1% | 1% | - |
CARDIOVASCULAR: Bradycardia, arrhythmia
DIGESTIVE: Diarrhea, dry mouth
NERVOUS SYSTEM: Somnolence, depression, agitation, nervousness, tremor, confusion, withdrawal syndrome, myoclonus
RESPIRATORY: Pharyngitis
SKIN: Pruritus
UROGENITAL: Urinary retention
The incidence of adverse events was highest in patients who received more than the recommended dose of nalmefene hydrochloride injection.
Laboratory findings: Transient increases in CPK were reported as adverse events in 0.5% of the postoperative patients studied. These increases were believed to be related to surgery and not believed to be related to the administration of nalmefene hydrochloride injection. Increases in AST were reported as adverse events in 0.3% of the patients receiving either nalmefene or naloxone. The clinical significance of this finding is unknown. No cases of hepatitis or hepatic injury due to either nalmefene or naloxone were observed in the clinical trials.
Nalmefene Hydrochloride Injection, an opioid antagonist, is a 6-methylene analogue of naltrexone. The chemical structure is shown below:
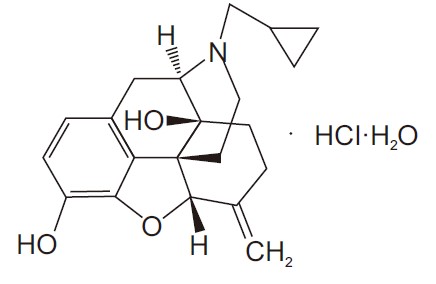
Molecular Formula: C21H25NO3•HCl•H2O
Molecular Weight: 393.91, CAS # 1228646-72-7
Chemical Name: 17-(Cyclopropylmethyl)-4,5α-epoxy-6-methylenemorphinan-3,14-diol, hydrochloride salt, monohydrate
Nalmefene hydrochloride is a white to almost white crystalline powder which is freely soluble in water up to 130 mg/mL and slightly soluble in chloroform up to 0.13 mg/mL, with a pKa of 7.6.
Nalmefene Hydrochloride Injection is available as a sterile solution for intravenous, intramuscular, and subcutaneous administration in two concentrations, containing 100 µg or 1.0 mg of nalmefene free base per mL. The 100 µg/mL concentration contains 110.8 µg of nalmefene hydrochloride and the 1.0 mg/mL concentration contains 1.108 mg of nalmefene hydrochloride per mL. Both concentrations contain 9.0 mg of sodium chloride per mL and the pH is adjusted in the range of 3.3-3.5 with hydrochloric acid.
Concentrations and dosages of Nalmefene Hydrochloride Injection are expressed as the free base equivalent of nalmefene.