Nimodipine Prescribing Information
DO NOT ADMINISTER NIMODIPINE INTRAVENOUSLY OR BY OTHER PARENTERAL ROUTES. DEATHS AND SERIOUS, LIFE THREATENING ADVERSE EVENTS HAVE OCCURRED WHEN THE CONTENTS OF NIMODIPINE CAPSULES HAVE BEEN INJECTED PARENTERALLY (See
Moderate and weak inducers of CYP3A4 may also reduce the efficacy of nimodipine to a lesser extent. Patients on these should be closely monitored for lack of effectiveness, and a nimodipine dosage increase may be required. Moderate and weak CYP3A4 inhibitors include, for example: amprenavir, aprepitant, armodafinil, bosentan, efavirenz, etravirine, echinacea, modafinil, nafcillin, pioglitazone, prednisone and rufinamide.
Nimodipine is given orally in the form of soft gelatin 30 mg capsules for subarachnoid hemorrhage.
The recommended oral dose is 60 mg (two 30 mg capsules) every 4 hours for 21 consecutive days. In general, the capsules should be swallowed whole with a little liquid, preferably not less than one hour before or two hours after meals. Grapefruit juice is to be avoided (see
If the capsule cannot be swallowed, e.g., at the time of surgery, or if the patient is unconscious, a hole should be made in both ends of the capsule with an 18 gauge needle, and the contents of the capsule extracted into a syringe. A parenteral syringe can be used to extract the liquid inside the capsule, but the liquid should always be transferred to a syringe that cannot accept a needle and that is designed for administration orally or via a naso-gastric tube or PEG. To help minimize administration errors, it is recommended that the syringe used for administration be labeled "Not for IV Use". The contents should then be emptied into the patient's
Severely disturbed liver function, particularly liver cirrhosis, may result in an increased bioavailability of nimodipine due to a decreased first pass capacity and a reduced metabolic clearance. The reduction in blood pressure and other adverse effects may be more pronounced in these patients. Dosage should be reduced to one 30 mg capsule every 4 hours with close monitoring of blood pressure and heart rate; if necessary, discontinuation of the treatment should be considered.
Strong inhibitors of CYP3A4 should not be administered concomitantly with nimodipine (see
Nimodipine is indicated for the improvement of neurological outcome by reducing the incidence and severity of ischemic deficits in patients with subarachnoid hemorrhage from ruptured intracranial berry aneurysms regardless of their post-ictus neurological condition (i.e., Hunt and Hess Grades I to V).
Moderate and weak inducers of CYP3A4 may also reduce the efficacy of nimodipine to a lesser extent. Patients on these should be closely monitored for lack of effectiveness, and a nimodipine dosage increase may be required. Moderate and weak CYP3A4 inhibitors include, for example: amprenavir, aprepitant, armodafinil, bosentan, efavirenz, etravirine, echinacea, modafinil, nafcillin, pioglitazone, prednisone and rufinamide.
Nimodipine is given orally in the form of soft gelatin 30 mg capsules for subarachnoid hemorrhage.
The recommended oral dose is 60 mg (two 30 mg capsules) every 4 hours for 21 consecutive days. In general, the capsules should be swallowed whole with a little liquid, preferably not less than one hour before or two hours after meals. Grapefruit juice is to be avoided (see
Intestinal pseudo-obstruction and ileus have been reported rarely in patients treated with nimodipine. A causal relationship has not been established. The condition has responded to conservative management.
None known.
Nimodipine is metabolized via the cytochrome P450 3A4 system located both in the intestinal mucosa and in the liver. Drugs that are known to either inhibit or to induce this enzyme system may therefore alter the first pass or the clearance of nimodipine.
In addition, the blood pressure lowering effects of antihypertensives could be enhanced when taken concomitantly with nimodipine.
Other moderate and weak inducers of CYP3A4 may also reduce the efficacy of nimodipine, although the magnitude of decrease in nimodipine plasma concentrations is not known. Patients on these should be closely monitored for lack of effectiveness, and a nimodipine dosage increase may be required. Moderate and weak CYP3A4 inducers include: amprenavir, aprepitant, armodafinil, bosentan, efavirenz, etravirine, Echinacea, modafinil, nafcillin, pioglitazone, prednisone and rufinamide.
- macrolide antibiotics (e.g., clarithromycin, telithromycin),
-HIV protease inhibitors (e.g., delavirdine, indinavir, nelfinavir, ritonavir, saquinavir),
- azole antimycotics (e.g., ketoconazole, itraconazole, voriconazole),
- antidepressants (e.g. nefazodone)
- grapefruit juice: after intake of grapefruit juice and nimodipine, the blood pressure lowering effect may last for at least 4 days after the last ingestion of grapefruit juice. Ingestion of grapefruit/grapefruit juice is therefore not recommended while taking nimodipine (see
Nimodipine plasma concentration can also be increased in the presence of moderate and weak inhibitors of CYP3A4. If nimodipine is concomitantly administered with these drugs, blood pressure should be monitored, and a reduction of the nimodipine dose may be necessary. Moderate and weak CYP3A4 inhibitors include amprenavir, aprepitant, atazanavir, amiodarone, alprozalam, cyclosporine, cimetidine, erythromycin, fluconazole, fluoxetine, isoniazid, oral contraceptives, quinuprestin/dalforpristin, and valproic acid.
– diuretics,
– β-blockers,
– ACE inhibitors,
– A1-antagonists,
– other calcium antagonists,
– α-adrenergic blocking agents,
– PDE5 inhibitors,
– α-methyldopa.
Blood pressure should be carefully monitored, and dose adjustment of the blood pressure lowering drug(s) may be necessary.
In a two-year study, higher incidences of adenocarcinoma of the uterus and Leydig-cell adenoma of the testes were observed in rats given a diet containing 1800 ppm nimodipine (equivalent to 91 to 121 mg/kg/day nimodipine) than in placebo controls. The differences were not statistically significant, however, and the higher rates were well within historical control range for these tumors in the Wistar strain. Nimodipine was found not to be carcinogenic in a 91-week mouse study but the high dose of 1800 ppm nimodipine-in-feed (546 to 774 mg/kg/day) shortened the life expectancy of the animals. Mutagenicity studies, including the Ames, micronucleus and dominant lethal tests were negative.
Nimodipine did not impair the fertility and general reproductive performance of male and female Wistar rats following oral doses of up to 30 mg/kg/day when administered daily for more than 10 weeks in the males and 3 weeks in the females prior to mating and continued to day 7 of pregnancy. This dose in a rat is about 4 times the equivalent clinical dose of 60 mg q4h in a 50 kg patient.
Nimodipine has been shown to have a teratogenic effect in Himalayan rabbits. Incidences of malformations and stunted fetuses were increased at oral doses of 1 and 10 mg/kg/day administered (by gavage) from day 6 through day 18 of pregnancy but not at 3 mg/kg/day in one of two identical rabbit studies. In the second study an increased incidence of stunted fetuses was seen at 1 mg/kg/day but not at higher doses. Nimodipine was embryotoxic, causing resorption and stunted growth of fetuses, in Long Evans rats at 100 mg/kg/day administered by gavage from day 6 through day 15 of pregnancy. In two other rat studies, doses of 30 mg/kg/day nimodipine administered by gavage from day 16 of gestation and continued until sacrifice (day 20 of pregnancy or day 21 post partum) were associated with higher incidences of skeletal variation, stunted fetuses and stillbirths but no malformations. There are no adequate and well controlled studies in pregnant women to directly assess the effect on human fetuses. Nimodipine should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Nimodipine and/or its metabolites have been shown to appear in rat milk at concentrations much higher than in maternal plasma. It is not known whether the drug is excreted in human milk. Because many drugs are excreted in human milk, nursing mothers are advised not to breast feed their babies when taking the drug.
Safety and effectiveness in children have not been established.
Clinical studies of nimodipine did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dosing in elderly patients should be cautious, reflecting the greater frequency of decreased hepatic, renal or cardiac function, and of concomitant disease or other drug therapy.
If the capsule cannot be swallowed, e.g., at the time of surgery, or if the patient is unconscious, a hole should be made in both ends of the capsule with an 18 gauge needle, and the contents of the capsule extracted into a syringe. A parenteral syringe can be used to extract the liquid inside the capsule, but the liquid should always be transferred to a syringe that cannot accept a needle and that is designed for administration orally or via a naso-gastric tube or PEG. To help minimize administration errors, it is recommended that the syringe used for administration be labeled "Not for IV Use". The contents should then be emptied into the patient's
Severely disturbed liver function, particularly liver cirrhosis, may result in an increased bioavailability of nimodipine due to a decreased first pass capacity and a reduced metabolic clearance. The reduction in blood pressure and other adverse effects may be more pronounced in these patients. Dosage should be reduced to one 30 mg capsule every 4 hours with close monitoring of blood pressure and heart rate; if necessary, discontinuation of the treatment should be considered.
Strong inhibitors of CYP3A4 should not be administered concomitantly with nimodipine (see
The concomitant use of nimodipine with strong inhibitors of CYP3A4 such as some macrolide antibiotics (e.g., clarithromycin, telithromycin), some anti-HIV protease inhibitors (e.g., delaviridine, indinavir, nelfinavir, ritonavir, saquinavir), some azole antimycotics (e.g., ketoconazole, itraconazole, voriconazole) and some antidepressants (e.g., nefazadone) is contraindicated because of a risk of significant hypotension (see
Moderate and weak inducers of CYP3A4 may also reduce the efficacy of nimodipine to a lesser extent. Patients on these should be closely monitored for lack of effectiveness, and a nimodipine dosage increase may be required. Moderate and weak CYP3A4 inhibitors include, for example: amprenavir, aprepitant, armodafinil, bosentan, efavirenz, etravirine, echinacea, modafinil, nafcillin, pioglitazone, prednisone and rufinamide.
Intestinal pseudo-obstruction and ileus have been reported rarely in patients treated with nimodipine. A causal relationship has not been established. The condition has responded to conservative management.
None known.
Nimodipine is metabolized via the cytochrome P450 3A4 system located both in the intestinal mucosa and in the liver. Drugs that are known to either inhibit or to induce this enzyme system may therefore alter the first pass or the clearance of nimodipine.
In addition, the blood pressure lowering effects of antihypertensives could be enhanced when taken concomitantly with nimodipine.
Other moderate and weak inducers of CYP3A4 may also reduce the efficacy of nimodipine, although the magnitude of decrease in nimodipine plasma concentrations is not known. Patients on these should be closely monitored for lack of effectiveness, and a nimodipine dosage increase may be required. Moderate and weak CYP3A4 inducers include: amprenavir, aprepitant, armodafinil, bosentan, efavirenz, etravirine, Echinacea, modafinil, nafcillin, pioglitazone, prednisone and rufinamide.
- macrolide antibiotics (e.g., clarithromycin, telithromycin),
-HIV protease inhibitors (e.g., delavirdine, indinavir, nelfinavir, ritonavir, saquinavir),
- azole antimycotics (e.g., ketoconazole, itraconazole, voriconazole),
- antidepressants (e.g. nefazodone)
- grapefruit juice: after intake of grapefruit juice and nimodipine, the blood pressure lowering effect may last for at least 4 days after the last ingestion of grapefruit juice. Ingestion of grapefruit/grapefruit juice is therefore not recommended while taking nimodipine (see
Nimodipine plasma concentration can also be increased in the presence of moderate and weak inhibitors of CYP3A4. If nimodipine is concomitantly administered with these drugs, blood pressure should be monitored, and a reduction of the nimodipine dose may be necessary. Moderate and weak CYP3A4 inhibitors include amprenavir, aprepitant, atazanavir, amiodarone, alprozalam, cyclosporine, cimetidine, erythromycin, fluconazole, fluoxetine, isoniazid, oral contraceptives, quinuprestin/dalforpristin, and valproic acid.
– diuretics,
– β-blockers,
– ACE inhibitors,
– A1-antagonists,
– other calcium antagonists,
– α-adrenergic blocking agents,
– PDE5 inhibitors,
– α-methyldopa.
Blood pressure should be carefully monitored, and dose adjustment of the blood pressure lowering drug(s) may be necessary.
In a two-year study, higher incidences of adenocarcinoma of the uterus and Leydig-cell adenoma of the testes were observed in rats given a diet containing 1800 ppm nimodipine (equivalent to 91 to 121 mg/kg/day nimodipine) than in placebo controls. The differences were not statistically significant, however, and the higher rates were well within historical control range for these tumors in the Wistar strain. Nimodipine was found not to be carcinogenic in a 91-week mouse study but the high dose of 1800 ppm nimodipine-in-feed (546 to 774 mg/kg/day) shortened the life expectancy of the animals. Mutagenicity studies, including the Ames, micronucleus and dominant lethal tests were negative.
Nimodipine did not impair the fertility and general reproductive performance of male and female Wistar rats following oral doses of up to 30 mg/kg/day when administered daily for more than 10 weeks in the males and 3 weeks in the females prior to mating and continued to day 7 of pregnancy. This dose in a rat is about 4 times the equivalent clinical dose of 60 mg q4h in a 50 kg patient.
Nimodipine has been shown to have a teratogenic effect in Himalayan rabbits. Incidences of malformations and stunted fetuses were increased at oral doses of 1 and 10 mg/kg/day administered (by gavage) from day 6 through day 18 of pregnancy but not at 3 mg/kg/day in one of two identical rabbit studies. In the second study an increased incidence of stunted fetuses was seen at 1 mg/kg/day but not at higher doses. Nimodipine was embryotoxic, causing resorption and stunted growth of fetuses, in Long Evans rats at 100 mg/kg/day administered by gavage from day 6 through day 15 of pregnancy. In two other rat studies, doses of 30 mg/kg/day nimodipine administered by gavage from day 16 of gestation and continued until sacrifice (day 20 of pregnancy or day 21 post partum) were associated with higher incidences of skeletal variation, stunted fetuses and stillbirths but no malformations. There are no adequate and well controlled studies in pregnant women to directly assess the effect on human fetuses. Nimodipine should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Nimodipine and/or its metabolites have been shown to appear in rat milk at concentrations much higher than in maternal plasma. It is not known whether the drug is excreted in human milk. Because many drugs are excreted in human milk, nursing mothers are advised not to breast feed their babies when taking the drug.
Safety and effectiveness in children have not been established.
Clinical studies of nimodipine did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dosing in elderly patients should be cautious, reflecting the greater frequency of decreased hepatic, renal or cardiac function, and of concomitant disease or other drug therapy.
The concomitant use of nimodipine with strong inhibitors of CYP3A4 such as some macrolide antibiotics (e.g., clarithromycin, telithromycin), some anti-HIV protease inhibitors (e.g., delaviridine, indinavir, nelfinavir, ritonavir, saquinavir), some azole antimycotics (e.g., ketoconazole, itraconazole, voriconazole) and some antidepressants (e.g., nefazadone) is contraindicated because of a risk of significant hypotension (see
Intestinal pseudo-obstruction and ileus have been reported rarely in patients treated with nimodipine. A causal relationship has not been established. The condition has responded to conservative management.
None known.
Nimodipine is metabolized via the cytochrome P450 3A4 system located both in the intestinal mucosa and in the liver. Drugs that are known to either inhibit or to induce this enzyme system may therefore alter the first pass or the clearance of nimodipine.
In addition, the blood pressure lowering effects of antihypertensives could be enhanced when taken concomitantly with nimodipine.
Other moderate and weak inducers of CYP3A4 may also reduce the efficacy of nimodipine, although the magnitude of decrease in nimodipine plasma concentrations is not known. Patients on these should be closely monitored for lack of effectiveness, and a nimodipine dosage increase may be required. Moderate and weak CYP3A4 inducers include: amprenavir, aprepitant, armodafinil, bosentan, efavirenz, etravirine, Echinacea, modafinil, nafcillin, pioglitazone, prednisone and rufinamide.
- macrolide antibiotics (e.g., clarithromycin, telithromycin),
-HIV protease inhibitors (e.g., delavirdine, indinavir, nelfinavir, ritonavir, saquinavir),
- azole antimycotics (e.g., ketoconazole, itraconazole, voriconazole),
- antidepressants (e.g. nefazodone)
- grapefruit juice: after intake of grapefruit juice and nimodipine, the blood pressure lowering effect may last for at least 4 days after the last ingestion of grapefruit juice. Ingestion of grapefruit/grapefruit juice is therefore not recommended while taking nimodipine (see
Nimodipine plasma concentration can also be increased in the presence of moderate and weak inhibitors of CYP3A4. If nimodipine is concomitantly administered with these drugs, blood pressure should be monitored, and a reduction of the nimodipine dose may be necessary. Moderate and weak CYP3A4 inhibitors include amprenavir, aprepitant, atazanavir, amiodarone, alprozalam, cyclosporine, cimetidine, erythromycin, fluconazole, fluoxetine, isoniazid, oral contraceptives, quinuprestin/dalforpristin, and valproic acid.
– diuretics,
– β-blockers,
– ACE inhibitors,
– A1-antagonists,
– other calcium antagonists,
– α-adrenergic blocking agents,
– PDE5 inhibitors,
– α-methyldopa.
Blood pressure should be carefully monitored, and dose adjustment of the blood pressure lowering drug(s) may be necessary.
In a two-year study, higher incidences of adenocarcinoma of the uterus and Leydig-cell adenoma of the testes were observed in rats given a diet containing 1800 ppm nimodipine (equivalent to 91 to 121 mg/kg/day nimodipine) than in placebo controls. The differences were not statistically significant, however, and the higher rates were well within historical control range for these tumors in the Wistar strain. Nimodipine was found not to be carcinogenic in a 91-week mouse study but the high dose of 1800 ppm nimodipine-in-feed (546 to 774 mg/kg/day) shortened the life expectancy of the animals. Mutagenicity studies, including the Ames, micronucleus and dominant lethal tests were negative.
Nimodipine did not impair the fertility and general reproductive performance of male and female Wistar rats following oral doses of up to 30 mg/kg/day when administered daily for more than 10 weeks in the males and 3 weeks in the females prior to mating and continued to day 7 of pregnancy. This dose in a rat is about 4 times the equivalent clinical dose of 60 mg q4h in a 50 kg patient.
Nimodipine has been shown to have a teratogenic effect in Himalayan rabbits. Incidences of malformations and stunted fetuses were increased at oral doses of 1 and 10 mg/kg/day administered (by gavage) from day 6 through day 18 of pregnancy but not at 3 mg/kg/day in one of two identical rabbit studies. In the second study an increased incidence of stunted fetuses was seen at 1 mg/kg/day but not at higher doses. Nimodipine was embryotoxic, causing resorption and stunted growth of fetuses, in Long Evans rats at 100 mg/kg/day administered by gavage from day 6 through day 15 of pregnancy. In two other rat studies, doses of 30 mg/kg/day nimodipine administered by gavage from day 16 of gestation and continued until sacrifice (day 20 of pregnancy or day 21 post partum) were associated with higher incidences of skeletal variation, stunted fetuses and stillbirths but no malformations. There are no adequate and well controlled studies in pregnant women to directly assess the effect on human fetuses. Nimodipine should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Nimodipine and/or its metabolites have been shown to appear in rat milk at concentrations much higher than in maternal plasma. It is not known whether the drug is excreted in human milk. Because many drugs are excreted in human milk, nursing mothers are advised not to breast feed their babies when taking the drug.
Safety and effectiveness in children have not been established.
Clinical studies of nimodipine did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dosing in elderly patients should be cautious, reflecting the greater frequency of decreased hepatic, renal or cardiac function, and of concomitant disease or other drug therapy.
Adverse experiences were reported by 92 of 823 patients with subarachnoid hemorrhage (11.2%) who were given nimodipine. The most frequently reported adverse experience was decreased blood pressure in 4.4% of these patients. Twenty-nine of 479 (6.1%) placebo treated patients also reported adverse experiences. The events reported with a frequency greater than 1% are displayed below by dose.
Sign/Symptom | 0.35 mg/kg (n=82) | 30 mg (n=71) | 60 mg (n=494) | 90 mg (n=172) | 120 mg (n=4) | Placebo (n=479) |
| Decreased | ||||||
| Blood Pressure | 1 (1.2) | 0 | 19 (3.8) | 14 (8.1) | 2 (50.0) | 6 (1.2) |
| Abnormal Liver | ||||||
| Function Test | 1 (1.2) | 0 | 2 (0.4) | 1 (0.6) | 0 | 7 (1.5) |
| Edema | 0 | 0 | 2 (0.4) | 2 (1.2) | 0 | 3 (0.6) |
| Diarrhea | 0 | 3 (4.2) | 0 | 3 (1.7) | 0 | 3 (0.6) |
| Rash | 2 (2.4) | 0 | 3 (0.6) | 2 (1.2) | 0 | 3 (0.6) |
| Headache | 0 | 1 (1.4) | 6 (1.2) | 0 | 0 | 1 (0.2) |
| Gastrointestinal | ||||||
| Symptoms | 2 (2.4) | 0 | 0 | 2 (1.2) | 0 | 0 |
| Nausea | 1 (1.2) | 1 (1.4) | 6 (1.2) | 1 (0.6) | 0 | 0 |
| Dyspnea | 1 (1.2) | 0 | 0 | 0 | 0 | 0 |
| EKG Abnormalities | 0 | 1 (1.4) | 0 | 1 (0.6) | 0 | 0 |
| Tachycardia | 0 | 1 (1.4) | 0 | 0 | 0 | 0 |
| Bradycardia | 0 | 0 | 5 (1.0) | 1 (0.6) | 0 | 0 |
| Muscle Pain/Cramp | 0 | 1 (1.4) | 1 (0.2) | 1 (0.6) | 0 | 0 |
| Acne | 0 | 1 (1.4) | 0 | 0 | 0 | 0 |
| Depression | 0 | 1 (1.4) | 0 | 0 | 0 | 0 |
There were no other adverse experiences reported by the patients who were given 0.35 mg/kg q4h, 30 mg q4h or 120 mg q4h. Adverse experiences with an incidence rate of less than 1% in the 60 mg q4h dose group were: hepatitis; itching; gastrointestinal hemorrhage; thrombocytopenia; anemia; palpitations; vomiting; flushing; diaphoresis; wheezing; phenytoin toxicity; lightheadedness; dizziness; rebound vasospasm; jaundice; hypertension; hematoma.
Adverse experiences with an incidence rate less than 1% in the 90 mg q4h dose group were: itching, gastrointestinal hemorrhage; thrombocytopenia; neurological deterioration; vomiting; diaphoresis; congestive heart failure; hyponatremia; decreasing platelet count; disseminated intravascular coagulation; deep vein thrombosis.
As can be seen from the table, side effects that appear related to nimodipine use based on increased incidence with higher dose or a higher rate compared to placebo control, included decreased blood pressure, edema and headaches which are known pharmacologic actions of calcium channel blockers. It must be noted, however, that SAH is frequently accompanied by alterations in consciousness which lead to an under reporting of adverse experiences. Patients who received nimodipine in clinical trials for other indications reported flushing (2.1%), headache (4.1%) and fluid retention (0.3%), typical responses to calcium channel blockers. As a calcium channel blocker, nimodipine may have the potential to exacerbate heart failure in susceptible patients or to interfere with A-V conduction, but these events were not observed.
No clinically significant effects on hematologic factors, renal or hepatic function or carbohydrate metabolism have been causally associated with oral nimodipine. Isolated cases of non-fasting elevated serum glucose levels (0.8%), elevated LDH levels (0.4%), decreased platelet counts (0.3%), elevated alkaline phosphatase levels (0.2%) and elevated SGPT levels (0.2%) have been reported rarely.
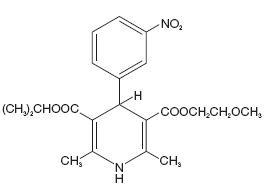
Nimodipine belongs to the class of pharmacological agents known as calcium channel blockers. Nimodipine is isopropyl 2-methoxyethyl 1,4-dihydro-2,6-dimethyl-4-(
Nimodipine capsules are formulated as soft gelatin capsules for oral administration. Each liquid filled capsule contains 30 mg of nimodipine in a vehicle of glycerin, peppermint oil and polyethylene glycol. The gelatin shell contains FD&C Yellow No. 6 Aluminum Lake, gelatin, glycerin, iron oxide black, lecithin, medium-chain triglycerides, shellac, sorbitol and titanium dioxide.