Prochlorperazine Maleate - Prochlorperazine Maleate tablet Prescribing Information
Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Prochlorperazine maleate is not approved for the treatment of patients with dementia-related psychosis (see
Both the risk of developing the syndrome and the likelihood that it will become irreversible are believed to increase as the duration of treatment and the total cumulative dose of antipsychotic drugs administered to the patient increase. However, the syndrome can develop, although much less commonly, after relatively brief treatment periods at low doses.
There is no known treatment for established cases of tardive dyskinesia, although the syndrome may remit, partially or completely, if antipsychotic drug treatment is withdrawn. Antipsychotic drug treatment itself, however, may suppress (or partially suppress) the signs and symptoms of the syndrome and thereby may possibly mask the underlying disease process.
The effect that symptomatic suppression has upon the long-term course of the syndrome is unknown.
Given these considerations, antipsychotic drugs should be prescribed in a manner that is most likely to minimize the occurrence of tardive dyskinesia especially in the elderly. Chronic antipsychotic treatment should generally be reserved for patients who suffer from a chronic illness that, 1) is known to respond to antipsychotic drugs, and 2) for whom alternative, equally effective, but potentially less harmful treatments are not available or appropriate. In patients who do require chronic treatment, the smallest dose and the shortest duration of treatment producing a satisfactory clinical response should be sought. The need for continued treatment should be reassessed periodically.
If signs and symptoms of tardive dyskinesia appear in a patient on antipsychotics, drug discontinuation should be considered. However, some patients may require treatment despite the presence of the syndrome.
For further information about the description of tardive dyskinesia and its clinical detection, please refer to the sections on
The diagnostic evaluation of patients with this syndrome is complicated. In arriving at a diagnosis, it is important to identify cases where the clinical presentation includes both serious medical illness (e.g., pneumonia, systemic infection, etc.) and untreated or inadequately treated extrapyramidal signs and symptoms (EPS). Other important considerations in the differential diagnosis include central anticholinergic toxicity, heat stroke, drug fever and primary central nervous systems (CNS) pathology.
The management of NMS should include 1) immediate discontinuation of antipsychotic drugs and other drugs not essential to concurrent therapy, 2) intensive symptomatic treatment and medical monitoring, and 3) treatment of any concomitant serious medical problems for which specific treatments are available. There is no general agreement about specific pharmacological treatment regimens for uncomplicated NMS.
If a patient requires antipsychotic drug treatment after recovery from NMS, the potential reintroduction of drug therapy should be carefully considered. The patient should be carefully monitored, since recurrences of NMS have been reported.
An encephalopathic syndrome (characterized by weakness, lethargy, fever, tremulousness and confusion, extrapyramidal symptoms, leukocytosis, elevated serum enzymes, BUN and FBS) has occurred in a few patients treated with lithium plus an antipsychotic. In some instances, the syndrome was followed by irreversible brain damage. Because of a possible causal relationship between these events and the concomitant administration of lithium and antipsychotics, patients receiving such combined therapy should be monitored closely for early evidence of neurologic toxicity and treatment discontinued promptly if such signs appear. This encephalopathic syndrome may be similar to or the same as neuroleptic malignant syndrome (NMS).
Patients with bone marrow depression or who have previously demonstrated a hypersensitivity reaction (e.g., blood dyscrasias, jaundice) with a phenothiazine should not receive any phenothiazine, including Prochlorperazine, unless in the judgment of the physician the potential benefits of treatment outweigh the possible hazards.
Prochlorperazine may impair mental and/or physical abilities, especially during the first few days of therapy. Therefore, caution patients about activities requiring alertness (e.g., operating vehicles or machinery).
Phenothiazines may intensify or prolong the action of central nervous system depressants (e.g., alcohol, anesthetics, narcotics).
There have been reported instances of prolonged jaundice, extrapyramidal signs, hyperreflexia or hyporeflexia in newborn infants whose mothers received phenothiazines.
Prochlorperazine Maleate should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
For control of severe nausea and vomiting.
For the treatment of schizophrenia.
Prochlorperazine is effective for the short-term treatment of generalized non-psychotic anxiety. However, prochlorperazine is not the first drug to be used in therapy for most patients with non-psychotic anxiety, because certain risks associated with its use are not shared by common alternative treatments (e.g., benzodiazepines).
When used in the treatment of non-psychotic anxiety, prochlorperazine should not be administered at doses of more than 20 mg per day or for longer than 12 weeks, because the use of prochlorperazine at higher doses or for longer intervals may cause persistent tardive dyskinesia that may prove irreversible (see
Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Prochlorperazine maleate is not approved for the treatment of patients with dementia-related psychosis (see
Both the risk of developing the syndrome and the likelihood that it will become irreversible are believed to increase as the duration of treatment and the total cumulative dose of antipsychotic drugs administered to the patient increase. However, the syndrome can develop, although much less commonly, after relatively brief treatment periods at low doses.
There is no known treatment for established cases of tardive dyskinesia, although the syndrome may remit, partially or completely, if antipsychotic drug treatment is withdrawn. Antipsychotic drug treatment itself, however, may suppress (or partially suppress) the signs and symptoms of the syndrome and thereby may possibly mask the underlying disease process.
The effect that symptomatic suppression has upon the long-term course of the syndrome is unknown.
Given these considerations, antipsychotic drugs should be prescribed in a manner that is most likely to minimize the occurrence of tardive dyskinesia especially in the elderly. Chronic antipsychotic treatment should generally be reserved for patients who suffer from a chronic illness that, 1) is known to respond to antipsychotic drugs, and 2) for whom alternative, equally effective, but potentially less harmful treatments are not available or appropriate. In patients who do require chronic treatment, the smallest dose and the shortest duration of treatment producing a satisfactory clinical response should be sought. The need for continued treatment should be reassessed periodically.
If signs and symptoms of tardive dyskinesia appear in a patient on antipsychotics, drug discontinuation should be considered. However, some patients may require treatment despite the presence of the syndrome.
For further information about the description of tardive dyskinesia and its clinical detection, please refer to the sections on
The diagnostic evaluation of patients with this syndrome is complicated. In arriving at a diagnosis, it is important to identify cases where the clinical presentation includes both serious medical illness (e.g., pneumonia, systemic infection, etc.) and untreated or inadequately treated extrapyramidal signs and symptoms (EPS). Other important considerations in the differential diagnosis include central anticholinergic toxicity, heat stroke, drug fever and primary central nervous systems (CNS) pathology.
The management of NMS should include 1) immediate discontinuation of antipsychotic drugs and other drugs not essential to concurrent therapy, 2) intensive symptomatic treatment and medical monitoring, and 3) treatment of any concomitant serious medical problems for which specific treatments are available. There is no general agreement about specific pharmacological treatment regimens for uncomplicated NMS.
If a patient requires antipsychotic drug treatment after recovery from NMS, the potential reintroduction of drug therapy should be carefully considered. The patient should be carefully monitored, since recurrences of NMS have been reported.
An encephalopathic syndrome (characterized by weakness, lethargy, fever, tremulousness and confusion, extrapyramidal symptoms, leukocytosis, elevated serum enzymes, BUN and FBS) has occurred in a few patients treated with lithium plus an antipsychotic. In some instances, the syndrome was followed by irreversible brain damage. Because of a possible causal relationship between these events and the concomitant administration of lithium and antipsychotics, patients receiving such combined therapy should be monitored closely for early evidence of neurologic toxicity and treatment discontinued promptly if such signs appear. This encephalopathic syndrome may be similar to or the same as neuroleptic malignant syndrome (NMS).
Patients with bone marrow depression or who have previously demonstrated a hypersensitivity reaction (e.g., blood dyscrasias, jaundice) with a phenothiazine should not receive any phenothiazine, including Prochlorperazine, unless in the judgment of the physician the potential benefits of treatment outweigh the possible hazards.
Prochlorperazine may impair mental and/or physical abilities, especially during the first few days of therapy. Therefore, caution patients about activities requiring alertness (e.g., operating vehicles or machinery).
Phenothiazines may intensify or prolong the action of central nervous system depressants (e.g., alcohol, anesthetics, narcotics).
There have been reported instances of prolonged jaundice, extrapyramidal signs, hyperreflexia or hyporeflexia in newborn infants whose mothers received phenothiazines.
Prochlorperazine Maleate should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
The effectiveness of prochlorperazine as treatment for non-psychotic anxiety was established in 4-week clinical studies of outpatients with generalized anxiety disorder. This evidence does not predict that prochlorperazine will be useful in patients with other non-psychotic conditions in which anxiety, or signs that mimic anxiety, are found (e.g., physical illness, organic mental conditions, agitated depression, character pathologies, etc.).
Prochlorperazine has not been shown effective in the management of behavioral complications in patients with mental retardation.
(For children’s dosage and administration, see below.) Dosage should be increased more gradually in debilitated or emaciated patients.
Occasionally the patient may react to the drug with signs of restlessness and excitement; if this occurs, do not administer additional doses. Take particular precaution in administering the drug to children with acute illnesses or dehydration (see under Dystonias).
| Weight | Usual Dosage | Not to Exceed |
| under 20 lbs not recommended | | |
| 20 to 29 lbs | 2½ mg 1 or 2 times a day | 7.5 mg per day |
| 30 to 39 lbs | 2½ mg 2 or 3 times a day | 10 mg per day |
| 40 to 85 lbs | 2½ mg 3 times a day or 5 mg 2 times a day | 15 mg per day |
FOR AGES 2 to 5, total daily dosage usually does not exceed 20 mg.
FOR AGES 6 to 12, total daily dosage usually does not exceed 25 mg.
Do not use in patients with known hypersensitivity to phenothiazines.
Do not use in comatose states or in the presence of large amounts of central nervous system depressants (alcohol, barbiturates, narcotics, etc.).
Do not use in pediatric surgery.
Do not use in pediatric patients under 2 years of age or under 20 lbs. Do not use in children for conditions for which dosage has not been established.
Drowsiness, dizziness, amenorrhea, blurred vision, skin reactions and hypotension may occur. Neuroleptic Malignant Syndrome (NMS) has been reported in association with antipsychotic drugs (see
Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Prochlorperazine maleate is not approved for the treatment of patients with dementia-related psychosis (see
Both the risk of developing the syndrome and the likelihood that it will become irreversible are believed to increase as the duration of treatment and the total cumulative dose of antipsychotic drugs administered to the patient increase. However, the syndrome can develop, although much less commonly, after relatively brief treatment periods at low doses.
There is no known treatment for established cases of tardive dyskinesia, although the syndrome may remit, partially or completely, if antipsychotic drug treatment is withdrawn. Antipsychotic drug treatment itself, however, may suppress (or partially suppress) the signs and symptoms of the syndrome and thereby may possibly mask the underlying disease process.
The effect that symptomatic suppression has upon the long-term course of the syndrome is unknown.
Given these considerations, antipsychotic drugs should be prescribed in a manner that is most likely to minimize the occurrence of tardive dyskinesia especially in the elderly. Chronic antipsychotic treatment should generally be reserved for patients who suffer from a chronic illness that, 1) is known to respond to antipsychotic drugs, and 2) for whom alternative, equally effective, but potentially less harmful treatments are not available or appropriate. In patients who do require chronic treatment, the smallest dose and the shortest duration of treatment producing a satisfactory clinical response should be sought. The need for continued treatment should be reassessed periodically.
If signs and symptoms of tardive dyskinesia appear in a patient on antipsychotics, drug discontinuation should be considered. However, some patients may require treatment despite the presence of the syndrome.
For further information about the description of tardive dyskinesia and its clinical detection, please refer to the sections on
The diagnostic evaluation of patients with this syndrome is complicated. In arriving at a diagnosis, it is important to identify cases where the clinical presentation includes both serious medical illness (e.g., pneumonia, systemic infection, etc.) and untreated or inadequately treated extrapyramidal signs and symptoms (EPS). Other important considerations in the differential diagnosis include central anticholinergic toxicity, heat stroke, drug fever and primary central nervous systems (CNS) pathology.
The management of NMS should include 1) immediate discontinuation of antipsychotic drugs and other drugs not essential to concurrent therapy, 2) intensive symptomatic treatment and medical monitoring, and 3) treatment of any concomitant serious medical problems for which specific treatments are available. There is no general agreement about specific pharmacological treatment regimens for uncomplicated NMS.
If a patient requires antipsychotic drug treatment after recovery from NMS, the potential reintroduction of drug therapy should be carefully considered. The patient should be carefully monitored, since recurrences of NMS have been reported.
An encephalopathic syndrome (characterized by weakness, lethargy, fever, tremulousness and confusion, extrapyramidal symptoms, leukocytosis, elevated serum enzymes, BUN and FBS) has occurred in a few patients treated with lithium plus an antipsychotic. In some instances, the syndrome was followed by irreversible brain damage. Because of a possible causal relationship between these events and the concomitant administration of lithium and antipsychotics, patients receiving such combined therapy should be monitored closely for early evidence of neurologic toxicity and treatment discontinued promptly if such signs appear. This encephalopathic syndrome may be similar to or the same as neuroleptic malignant syndrome (NMS).
Patients with bone marrow depression or who have previously demonstrated a hypersensitivity reaction (e.g., blood dyscrasias, jaundice) with a phenothiazine should not receive any phenothiazine, including Prochlorperazine, unless in the judgment of the physician the potential benefits of treatment outweigh the possible hazards.
Prochlorperazine may impair mental and/or physical abilities, especially during the first few days of therapy. Therefore, caution patients about activities requiring alertness (e.g., operating vehicles or machinery).
Phenothiazines may intensify or prolong the action of central nervous system depressants (e.g., alcohol, anesthetics, narcotics).
There have been reported instances of prolonged jaundice, extrapyramidal signs, hyperreflexia or hyporeflexia in newborn infants whose mothers received phenothiazines.
Prochlorperazine Maleate should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Cholestatic jaundice has occurred. If fever with grippe-like symptoms occurs, appropriate liver studies should be conducted. If tests indicate an abnormality, stop treatment. There have been a few observations of fatty changes in the livers of patients who have died while receiving the drug. No causal relationship has been established.
Leukopenia and agranulocytosis have occurred. Warn patients to report the sudden appearance of sore throat or other signs of infection. If white blood cell and differential counts indicate leukocyte depression, stop treatment and start antibiotic and other suitable therapy.
These symptoms are seen in a significant number of hospitalized mental patients. They maybe characterized by motor restlessness, be of the dystonic type, or they may resemble parkinsonism.
Depending on the severity of symptoms, dosage should be reduced or discontinued. If therapy is reinstituted, it should be at a lower dosage. Should these symptoms occur in children or pregnant patients, the drug should be stopped and not reinstituted. In most cases barbiturates by suitable route of administration will suffice. (Or, injectable Benadryl®ll may be useful). In more severe cases, the administration of an anti-parkinsonism agent, except levodopa (See PDR), usually produces rapid reversal of symptoms. Suitable supportive measures such as maintaining a clear airway and adequate hydration should be employed.
Class effect:
These usually subside within a few hours, and almost always within 24 to 48 hours, after the drug has been discontinued.
If these symptoms become too troublesome, they can usually be controlled by a reduction of dosage or change of drug. Treatment with anti-parkinsonian agents, benzodiazepines or propranolol may be helpful.
There is no known effective treatment for tardive dyskinesia; anti-parkinsonism agents do not alleviate the symptoms of this syndrome. It is suggested that all antipsychotic agents be discontinued if these symptoms appear.
Should it be necessary to reinstitute treatment, or increase the dosage of the agent, or switch to a different antipsychotic agent, the syndrome may be masked.
It has been reported that fine vermicular movements of the tongue may be an early sign of the syndrome and if the medication is stopped at that time the syndrome may not develop.
Adverse reactions with different phenothiazines vary in type, frequency and mechanism of occurrence, i.e., some are dose-related, while others involve individual patient sensitivity. Some adverse reactions may be more likely to occur, or occur with greater intensity, in patients with special medical problems, e.g., patients with mitral insufficiency or pheochromocytoma have experienced severe hypotension following recommended doses of certain phenothiazines.
Not all of the following adverse reactions have been observed with every phenothiazine derivative, but they have been reported with 1 or more and should be borne in mind when drugs of this class are administered: extrapyramidal symptoms (opisthotonos, oculogyric crisis, hyperreflexia, dystonia, akathisia, dyskinesia, parkinsonism) some of which have lasted months and even years-particularly in elderly patients with previous brain damage; grand mal and petit mal convulsions, particularly in patients with EEG abnormalities or history of such disorders; altered cerebrospinal fluid proteins; cerebral edema; intensification and prolongation of the action of central nervous system depressants (opiates, analgesics, antihistamines, barbiturates, alcohol), atropine, heat, organophosphorus insecticides; autonomic reactions (dryness of mouth, nasal congestion, headache, nausea, constipation, obstipation, adynamic ileus, ejaculatory disorders/impotence, priapism, atonic colon, urinary retention, miosis and mydriasis); reactivation of psychotic processes, catatonic-like states; hypotension (sometimes fatal); cardiac arrest; blood dyscrasias (pancytopenia, thrombocytopenic purpura, leukopenia, agranulocytosis, eosinophilia, hemolytic anemia, aplastic anemia); liver damage (jaundice, biliary stasis); endocrine disturbances (hyperglycemia, hypoglycemia, glycosuria, lactation, galactorrhea, gynecomastia, menstrual irregularities, false-positive pregnancy tests); skin disorders (photosensitivity, itching, erythema, urticaria, eczema up to exfoliative dermatitis); other allergic reactions (asthma, laryngeal edema, angioneurotic edema, anaphylactoid reactions); peripheral edema; reversed epinephrine effect; hyperpyrexia; mild fever after large I.M. doses; increased appetite; increased weight; a systemic lupus erythematosus-like syndrome; pigmentary retinopathy; with prolonged administration of substantial doses, skin pigmentation, epithelial keratopathy, and lenticular and corneal deposits.
EKG changes- particularly nonspecific, usually reversible Q and T wave distortions-have been observed in some patients receiving phenothiazine.
Although phenothiazines cause neither psychic nor physical dependence, sudden discontinuance in long-term psychiatric patients may cause temporary symptoms, e.g., nausea and vomiting, dizziness, tremulousness.
NOTE: There have been occasional reports of sudden death in patients receiving phenothiazines. In some cases, the cause appeared to be cardiac arrest or asphyxia due to failure of the cough reflex.
Prochlorperazine, USP is a phenothiazine derivative, present in prochlorperazine tablets as the maleate. Prochlorperazine maleate is designated chemically as 2-chloro-10-[3-(4- methyl-1 -piperazinyl)propyl] phenothiazine maleate [molecular weight 606.10] and has the following structure
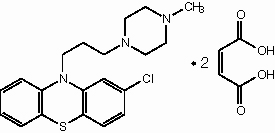
Prochlorperazine Maleate is classified as an anti-emetic and antipsychotic agent. Prochlorperazine maleate is white or pale yellow, practically odorless crystalline powder. It is practically insoluble in water and in alcohol; slightly soluble in warm chloroform.
Each tablet, for oral administration contains prochlorperazine maleate equivalent to 5 mg or 10 mg of prochlorperazine. In addition, each tablet contains the following inactive ingredients: D&C yellow no. 10 aluminum lake, FD&C blue no. 2 aluminum lake, FD&C yellow no. 6 aluminum lake, hydroxypropyl methylcellulose, lactose monohydrate, magnesium stearate, microcrystalline cellulose, polyethylene glycol, polysorbate 80, pregelatinized starch, stearic acid and titanium dioxide.