Sodium Nitroprusside - Sodium Nitroprusside injection, Solution, Concentrate Prescribing Information
Because sodium nitroprusside’s hypotensive effect is very rapid in onset and in dissipation, small variations in infusion rate can lead to wide, undesirable variations in blood pressure. Since there is inherent variation in blood pressure measurement, confirm the drug effect at any infusion rate after an additional 5 minutes before titrating to a higher dose to achieve the desired blood pressure.
Because sodium nitroprusside can induce essentially unlimited blood-pressure reduction,
When sodium nitroprusside is used in the treatment of acute congestive heart failure, titration of the infusion rate must be guided by the results of invasive hemodynamic monitoring with simultaneous monitoring of urine output. Sodium nitroprusside can be titrated by increasing the infusion rate until:
• measured cardiac output is no longer increasing,
• systemic blood pressure cannot be further reduced without compromising the perfusion of vital organs, or
• the maximum recommended infusion rate has been reached, whichever comes earliest. Specific hemodynamic goals must be tailored to the clinical situation, but improvements in cardiac output and left ventricular filling pressure must not be purchased at the price of undue hypotension and consequent hypoperfusion.
Table 2 below shows the infusion rates corresponding to the recommended initial and maximal doses (0.3 mcg/kg/min and 10 mcg/kg/min, respectively) for both adult and pediatric patients of various weights. This infusion rate may be lower than indicated in the table for patients less than 10 kg. Note that when the concentration used in a given patient is changed, the tubing is still filled with a solution at the previous concentration.
Volume Sodium Nitroprusside Injection concentration | 250 mL 50 mg 200 mcg/mL | 500 mL 50 mg 100 mcg/mL | 1000 mL 50 mg 50 mcg/mL | ||||
pt | weight | ||||||
kg | lbs | init | max | init | max | init | max |
10 | 22 | 1 | 30 | 2 | 60 | 4 | 120 |
20 | 44 | 2 | 60 | 4 | 120 | 7 | 240 |
30 | 66 | 3 | 90 | 5 | 180 | 11 | 360 |
40 | 88 | 4 | 120 | 7 | 240 | 14 | 480 |
50 | 110 | 5 | 150 | 9 | 300 | 18 | 600 |
60 | 132 | 5 | 180 | 11 | 360 | 22 | 720 |
70 | 154 | 6 | 210 | 13 | 420 | 25 | 840 |
80 | 176 | 7 | 240 | 14 | 480 | 29 | 960 |
90 | 198 | 8 | 270 | 16 | 540 | 32 | 1080 |
100 | 220 | 9 | 300 | 18 | 600 | 36 | 1200 |
Co-infusions of sodium thiosulfate have been administered at rates of 5 to 10 times that of sodium nitroprusside. Care must be taken to avoid the indiscriminate use of prolonged or high doses of sodium nitroprusside with sodium thiosulfate as this may result in thiocyanate toxicity and hypovolemia. Incautious administration of sodium nitroprusside must still be avoided, and all of the precautions concerning sodium nitroprusside administration must still be observed.
In accordance with the descriptions in
(See also the boxed warning at the beginning of this insert.)
The principal hazards of Sodium Nitroprusside Injection administration are excessive hypotension and excessive accumulation of cyanide (see also
The true rates of clinically important cyanide toxicity cannot be assessed from spontaneous reports or published data. Most patients reported to have experienced such toxicity have received relatively prolonged infusions, and the only patients whose deaths have been unequivocally attributed to nitroprusside-induced cyanide toxicity have been patients who had received nitroprusside infusions at rates (30 to 120 mcg/kg/min) much greater than those now recommended. Elevated cyanide levels, metabolic acidosis, and marked clinical deterioration, however, have occasionally been reported in patients who received infusions at recommended rates for only a few hours and even, in one case, for only 35 minutes. In some of these cases, infusion of sodium thiosulfate caused dramatic clinical improvement, supporting the diagnosis of cyanide toxicity.
Cyanide toxicity may manifest itself as venous hyperoxemia with bright red venous blood, as cells become unable to extract the oxygen delivered to them; metabolic (lactic) acidosis; air hunger; confusion; and death. Cyanide toxicity due to causes other than nitroprusside has been associated with angina pectoris and myocardial infarction; ataxia, seizures, and stroke; and other diffuse ischemic damage.
Hypertensive patients, and patients concomitantly receiving other antihypertensive medications, may be more sensitive to the effects of sodium nitroprusside than normal subjects.
Sodium nitroprusside is indicated for the immediate reduction of blood pressure of adult and pediatric patients in hypertensive crises. Concomitant longer-acting antihypertensive medication should be administered so that the duration of treatment with sodium nitroprusside can be minimized.
Sodium nitroprusside is also indicated for producing controlled hypotension in order to reduce bleeding during surgery.
Sodium nitroprusside is also indicated for the treatment of acute congestive heart failure.
Because sodium nitroprusside’s hypotensive effect is very rapid in onset and in dissipation, small variations in infusion rate can lead to wide, undesirable variations in blood pressure. Since there is inherent variation in blood pressure measurement, confirm the drug effect at any infusion rate after an additional 5 minutes before titrating to a higher dose to achieve the desired blood pressure.
Because sodium nitroprusside can induce essentially unlimited blood-pressure reduction,
When sodium nitroprusside is used in the treatment of acute congestive heart failure, titration of the infusion rate must be guided by the results of invasive hemodynamic monitoring with simultaneous monitoring of urine output. Sodium nitroprusside can be titrated by increasing the infusion rate until:
• measured cardiac output is no longer increasing,
• systemic blood pressure cannot be further reduced without compromising the perfusion of vital organs, or
• the maximum recommended infusion rate has been reached, whichever comes earliest. Specific hemodynamic goals must be tailored to the clinical situation, but improvements in cardiac output and left ventricular filling pressure must not be purchased at the price of undue hypotension and consequent hypoperfusion.
Table 2 below shows the infusion rates corresponding to the recommended initial and maximal doses (0.3 mcg/kg/min and 10 mcg/kg/min, respectively) for both adult and pediatric patients of various weights. This infusion rate may be lower than indicated in the table for patients less than 10 kg. Note that when the concentration used in a given patient is changed, the tubing is still filled with a solution at the previous concentration.
Volume Sodium Nitroprusside Injection concentration | 250 mL 50 mg 200 mcg/mL | 500 mL 50 mg 100 mcg/mL | 1000 mL 50 mg 50 mcg/mL | ||||
pt | weight | ||||||
kg | lbs | init | max | init | max | init | max |
10 | 22 | 1 | 30 | 2 | 60 | 4 | 120 |
20 | 44 | 2 | 60 | 4 | 120 | 7 | 240 |
30 | 66 | 3 | 90 | 5 | 180 | 11 | 360 |
40 | 88 | 4 | 120 | 7 | 240 | 14 | 480 |
50 | 110 | 5 | 150 | 9 | 300 | 18 | 600 |
60 | 132 | 5 | 180 | 11 | 360 | 22 | 720 |
70 | 154 | 6 | 210 | 13 | 420 | 25 | 840 |
80 | 176 | 7 | 240 | 14 | 480 | 29 | 960 |
90 | 198 | 8 | 270 | 16 | 540 | 32 | 1080 |
100 | 220 | 9 | 300 | 18 | 600 | 36 | 1200 |
The principal pharmacological action of sodium nitroprusside is relaxation of vascular smooth muscle and consequent dilatation of peripheral arteries and veins. Other smooth muscle (e.g., uterus, duodenum) is not affected. Sodium nitroprusside is more active on veins than on arteries, but this selectivity is much less marked than that of nitroglycerin. Dilatation of the veins promotes peripheral pooling of blood and decreases venous return to the heart, thereby reducing left ventricular end diastolic pressure and pulmonary capillary wedge pressure (preload). Arteriolar relaxation reduces systemic vascular resistance, systolic arterial pressure, and mean arterial pressure (afterload). Dilatation of the coronary arteries also occurs.
In association with the decrease in blood pressure, sodium nitroprusside administered intravenously to hypertensive and normotensive patients produces slight increases in heart rate and a variable effect on cardiac output. In hypertensive patients, moderate doses induce renal vasodilatation roughly proportional to the decrease in systemic blood pressure, so there is no appreciable change in renal blood flow or glomerular filtration rate.
In normotensive subjects, acute reduction of mean arterial pressure to 60 to 75 mm Hg by infusion of sodium nitroprusside caused a significant increase in renin activity. In the same study, ten renovascular-hypertensive patients given sodium nitroprusside had significant increases in renin release from the involved kidney at mean arterial pressures of 90 to 137 mm Hg.
The hypotensive effect of sodium nitroprusside is seen within a minute or two after the start of an adequate infusion, and it dissipates almost as rapidly after an infusion is discontinued. The effect is augmented by ganglionic blocking agents and inhaled anesthetics.
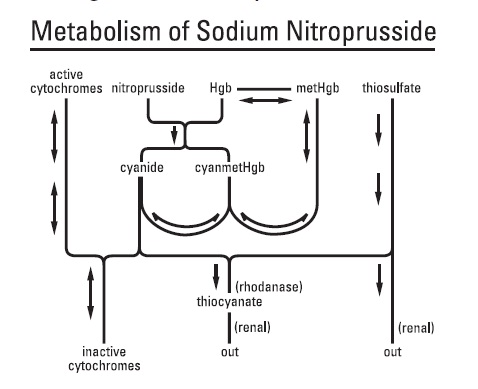
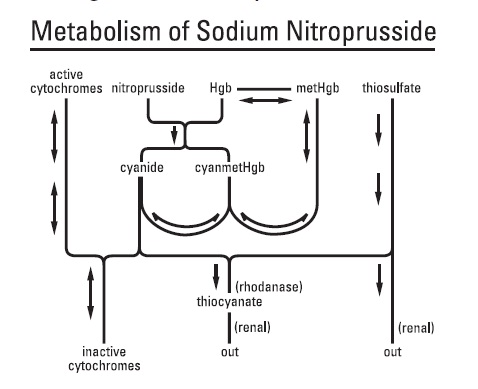
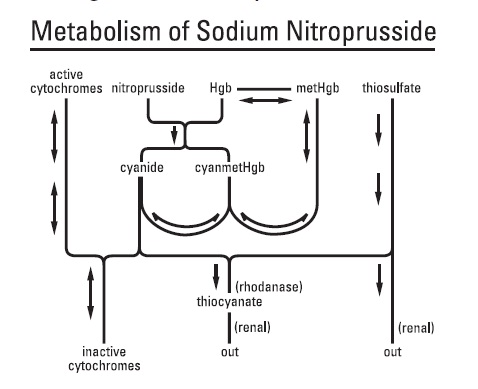
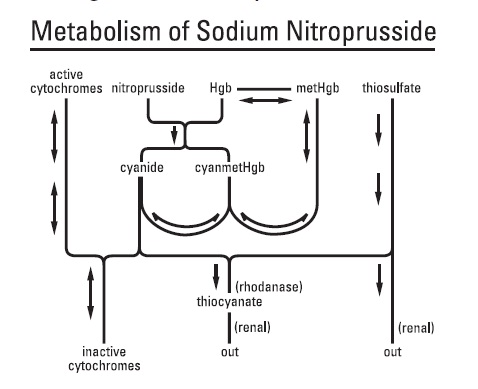
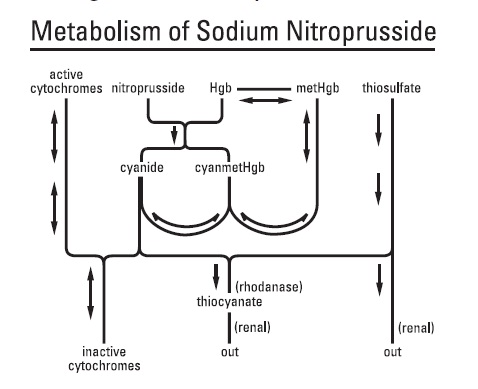
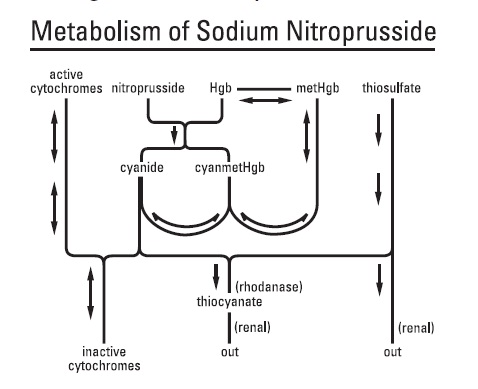
The products of the nitroprusside/hemoglobin reaction are cyanmethemoglobin (cyanmetHgb) and cyanide ion (CN-). Safe use of sodium nitroprusside injection must be guided by knowledge of the further metabolism of these products.
As shown in the diagram below, the essential features of nitroprusside metabolism are
- one molecule of sodium nitroprusside is metabolized by combination with hemoglobin to produce one molecule of cyanmethemoglobin and four CN-ions;
- methemoglobin, obtained from hemoglobin, can sequester cyanide as cyanmethemoglobin;
- thiosulfate reacts with cyanide to produce thiocyanate;
- thiocyanate is eliminated in the urine;
- cyanide not otherwise removed binds to cytochromes; and
- cyanide is much more toxic than methemoglobin or thiocyanate.
Cyanide ion is normally found in serum; it is derived from dietary substrates and from tobacco smoke.
Cyanide binds avidly (but reversibly) to ferric ion (Fe+++), most body stores of which are found in erythrocyte methemoglobin (metHgb) and in mitochondrial cytochromes. When CN–is infused or generated within the bloodstream, essentially all of it is bound to methemoglobin until intraerythrocytic methemoglobin has been saturated.
When the Fe+++of cytochromes is bound to cyanide, the cytochromes are unable to participate in oxidative metabolism. In this situation, cells may be able to provide for their energy needs by utilizing anaerobic pathways, but they thereby generate an increasing body burden of lactic acid. Other cells may be unable to utilize these alternative pathways, and they may die hypoxic deaths.
CN–levels in packed erythrocytes are typically less than 1 mcmol/L (less than 25 mcg/L); levels are roughly doubled in heavy smokers.
At healthy steady state, most people have less than 1% of their hemoglobin in the form of methemoglobin. Nitroprusside metabolism can lead to methemoglobin formation (a) through dissociation of cyanmethemoglobin formed in the original reaction of sodium nitroprusside with Hgb and (b) by direct oxidation of Hgb by the released nitroso group. Relatively large quantities of sodium nitroprusside, however, are required to produce significant methemoglobinemia.
At physiologic methemoglobin levels, the CN–binding capacity of packed red cells is a little less than 200 mcmol/L (5 mg/L). Cytochrome toxicity is seen at levels only slightly higher, and death has been reported at levels from 300 to 3000 mcmol/L (8 to 80 mg/L). Put another way, a patient with a normal red-cell mass (35 mL/kg) and normal methemoglobin levels can buffer about 175 mcg/kg of CN–, corresponding to a little less than 500 mcg/kg of infused sodium nitroprusside.
Some cyanide is eliminated from the body as expired hydrogen cyanide, but most is enzymatically converted to thiocyanate (SCN–) by thiosulfate-cyanide sulfur transferase (rhodanase, EC 2.8.1.1), a mitochondrial enzyme. The enzyme is normally present in great excess, so the reaction is rate-limited by the availability of sulfur donors, especially thiosulfate, cystine, and cysteine.
Thiosulfate is a normal constituent of serum, produced from cysteine by way of β-mercaptopyruvate. Physiological levels of thiosulfate are typically about 0.1 mmol/L (11 mg/L), but they are approximately twice this level in pediatric and adult patients who are not eating. Infused thiosulfate is cleared from the body (primarily by the kidneys) with a half-life of about 20 minutes.
When thiosulfate is being supplied only by normal physiologic mechanisms, conversion of CN–to SCN–generally proceeds at about 1 mcg/kg/min. This rate of CN–clearance corresponds to steady-state processing of a sodium nitroprusside infusion of slightly more than 2 mcg/kg/min. CN–begins to accumulate when sodium nitroprusside infusions exceed this rate.
Thiocyanate (SCN–) is also a normal physiological constituent of serum, with normal levels typically in the range of 50 to 250 mcmol/L (3 to 15 mg/L). Clearance of SCN–is primarily renal, with a half-life of about 3 days. In renal failure, the half-life can be doubled or tripled.
Clinical trials have also shown that the hypotensive effect of sodium nitroprusside is associated with reduced blood loss in a variety of major surgical procedures.
In patients with acute congestive heart failure and increased peripheral vascular resistance, administration of sodium nitroprusside causes reductions in peripheral resistance, increases in cardiac output, and reductions in left ventricular filling pressure.
Many trials have verified the clinical significance of the metabolic pathways described above. In patients receiving unopposed infusions of sodium nitroprusside, cyanide and thiocyanate levels have increased with increasing rates of sodium nitroprusside infusion. Mild to moderate metabolic acidosis has usually accompanied higher cyanide levels, but peak base deficits have lagged behind the peak cyanide levels by an hour or more.
Progressive tachyphylaxis to the hypotensive effects of sodium nitroprusside has been reported in several trials and numerous case reports. This tachyphylaxis has frequently been attributed to concomitant cyanide toxicity, but the only evidence adduced for this assertion has been the observation that in patients treated with sodium nitroprusside and found to be resistant to its hypotensive effects, cyanide levels are often found to be elevated. In the only reported
There were 203 pediatric patients in a parallel, dose-ranging study (Study 1). During the 30 minute blinded phase, patients were randomized 1:1:1:1 to receive sodium nitroprusside 0.3, 1, 2, or 3 mcg/kg/min. The infusion rate was increased step-wise to the target dose rate (i.e., 1/3 of the full rate for the first 5 minutes, 2/3 of the full rate for the next 5 minutes, and the full dose rate for the last 20 minutes). If the investigator believed that an increase to the next higher dose rate would be unsafe, the infusion remained at the current rate for the remainder of the blinded infusion. Since there was no placebo group, the change from baseline likely overestimates the true magnitude of blood pressure effect. Nevertheless, MAP decreased 11 to 20 mmHg from baseline across the four doses (Table 1).
There were 63 pediatric patients in a long-term infusion trial (Study 2). During an open-label phase (12 to 24 hours), sodium nitroprusside was started at ≤0.3 mcg/kg/min and titrated according to the BP response. Patients were then randomized to placebo or to continuing the same dose of sodium nitroprusside. The average MAP was greater in the control group than in the sodium nitroprusside group for every time point during the blinded withdrawal phase, demonstrating that sodium nitroprusside is effective for at least 12 hours. In both studies, similar effects on MAP were seen in all age groups.
Treatment | ||||
Endpoint | 0.3 mcg/kg/min (N=50) | 1 mcg/kg/min (N=49) | 2 mcg/kg/min (N=53) | 3 mcg/kg/min (N=51) |
Baseline | 76 ± 11 | 77 ± 15 | 74 ± 12 | 76 ± 12 |
30 Min | 65 ± 13 | 60 ± 15 | 54 ± 12 | 60 ± 18 |
Change from Baseline | -11 ± 16 (-15, -6.5) | -17 ± 13 (-21, -13) | -20 ± 16 (-24, -16) | -17 ± 19 (-22, -11) |
Mean ± SD (95% Cl) | ||||
Co-infusions of sodium thiosulfate have been administered at rates of 5 to 10 times that of sodium nitroprusside. Care must be taken to avoid the indiscriminate use of prolonged or high doses of sodium nitroprusside with sodium thiosulfate as this may result in thiocyanate toxicity and hypovolemia. Incautious administration of sodium nitroprusside must still be avoided, and all of the precautions concerning sodium nitroprusside administration must still be observed.
In accordance with the descriptions in
The most important adverse reactions to sodium nitroprusside are the avoidable ones of excessive hypotension and cyanide toxicity, described above under
Methemoglobin levels can be measured by most clinical laboratories. The diagnosis should be suspected in patients who have received >10 mg/kg of sodium nitroprusside and who exhibit signs of impaired oxygen delivery despite adequate cardiac output and adequate arterial pO2. Classically, methemoglobinemic blood is described as chocolate brown, without color change on exposure to air.
When methemoglobinemia is diagnosed, the treatment of choice is 1 to 2 mg/kg of methylene blue, administered intravenously over several minutes. In patients likely to have substantial amounts of cyanide bound to methemoglobin as cyanmethemoglobin, treatment of methemoglobinemia with methylene blue must be undertaken with extreme caution.
Thiocyanate is mildly neurotoxic (tinnitus, miosis, hyperreflexia) at serum levels of 1 mmol/L (60 mg/L). Thiocyanate toxicity is life-threatening when levels are 3 or 4 times higher (200 mg/L).
The steady-state thiocyanate level after prolonged infusions of sodium nitroprusside is increased with increased infusion rate, and the half-time of accumulation is 3 to 4 days. To keep the steady-state thiocyanate level below 1 mmol/L, a prolonged infusion of sodium nitroprusside should not be more rapid than 3 mcg/kg/min; in anuric patients, the corresponding limit is just 1 mcg/kg/min. When prolonged infusions are more rapid than these, thiocyanate levels should be measured daily.
Physiologic maneuvers (e.g., those that alter the pH of the urine) are not known to increase the elimination of thiocyanate. Thiocyanate clearance rates during dialysis, on the other hand, can approach the blood flow rate of the dialyzer.
Thiocyanate interferes with iodine uptake by the thyroid.
Abdominal pain, apprehension, diaphoresis, “dizziness,” headache, muscle twitching, nausea, palpitations, restlessness, retching, and retrosternal discomfort have been noted when the blood pressure was too rapidly reduced. These symptoms quickly disappeared when the infusion was slowed or discontinued, and they did not reappear with a continued (or resumed) slower infusion.
Other adverse reactions reported are:
To report SUSPECTED ADVERSE REACTIONS, contact Hainan Poly Pharm. Co., Ltd. at 1-800-571-8369 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Sodium nitroprusside should not be used in the treatment of compensatory hypertension, where the primary hemodynamic lesion is aortic coarctation or arteriovenous shunting.
Sodium nitroprusside should not be used to produce hypotension during surgery in patients with known inadequate cerebral circulation, or in moribund patients (A.S.A. Class 5E) coming to emergency surgery.
Patients with congenital (Leber’s) optic atrophy or with tobacco amblyopia have unusually high cyanide/thiocyanate ratios. These rare conditions are probably associated with defective or absent rhodanase, and sodium nitroprusside should be avoided in these patients.
Sodium nitroprusside should not be used for the treatment of acute congestive heart failure associated with reduced peripheral vascular resistance such as high-output heart failure that may be seen in endotoxic sepsis.
The most important adverse reactions to sodium nitroprusside are the avoidable ones of excessive hypotension and cyanide toxicity, described above under
(See also the boxed warning at the beginning of this insert.)
The principal hazards of Sodium Nitroprusside Injection administration are excessive hypotension and excessive accumulation of cyanide (see also
The true rates of clinically important cyanide toxicity cannot be assessed from spontaneous reports or published data. Most patients reported to have experienced such toxicity have received relatively prolonged infusions, and the only patients whose deaths have been unequivocally attributed to nitroprusside-induced cyanide toxicity have been patients who had received nitroprusside infusions at rates (30 to 120 mcg/kg/min) much greater than those now recommended. Elevated cyanide levels, metabolic acidosis, and marked clinical deterioration, however, have occasionally been reported in patients who received infusions at recommended rates for only a few hours and even, in one case, for only 35 minutes. In some of these cases, infusion of sodium thiosulfate caused dramatic clinical improvement, supporting the diagnosis of cyanide toxicity.
Cyanide toxicity may manifest itself as venous hyperoxemia with bright red venous blood, as cells become unable to extract the oxygen delivered to them; metabolic (lactic) acidosis; air hunger; confusion; and death. Cyanide toxicity due to causes other than nitroprusside has been associated with angina pectoris and myocardial infarction; ataxia, seizures, and stroke; and other diffuse ischemic damage.
Hypertensive patients, and patients concomitantly receiving other antihypertensive medications, may be more sensitive to the effects of sodium nitroprusside than normal subjects.
The principal pharmacological action of sodium nitroprusside is relaxation of vascular smooth muscle and consequent dilatation of peripheral arteries and veins. Other smooth muscle (e.g., uterus, duodenum) is not affected. Sodium nitroprusside is more active on veins than on arteries, but this selectivity is much less marked than that of nitroglycerin. Dilatation of the veins promotes peripheral pooling of blood and decreases venous return to the heart, thereby reducing left ventricular end diastolic pressure and pulmonary capillary wedge pressure (preload). Arteriolar relaxation reduces systemic vascular resistance, systolic arterial pressure, and mean arterial pressure (afterload). Dilatation of the coronary arteries also occurs.
In association with the decrease in blood pressure, sodium nitroprusside administered intravenously to hypertensive and normotensive patients produces slight increases in heart rate and a variable effect on cardiac output. In hypertensive patients, moderate doses induce renal vasodilatation roughly proportional to the decrease in systemic blood pressure, so there is no appreciable change in renal blood flow or glomerular filtration rate.
In normotensive subjects, acute reduction of mean arterial pressure to 60 to 75 mm Hg by infusion of sodium nitroprusside caused a significant increase in renin activity. In the same study, ten renovascular-hypertensive patients given sodium nitroprusside had significant increases in renin release from the involved kidney at mean arterial pressures of 90 to 137 mm Hg.
The hypotensive effect of sodium nitroprusside is seen within a minute or two after the start of an adequate infusion, and it dissipates almost as rapidly after an infusion is discontinued. The effect is augmented by ganglionic blocking agents and inhaled anesthetics.
The products of the nitroprusside/hemoglobin reaction are cyanmethemoglobin (cyanmetHgb) and cyanide ion (CN-). Safe use of sodium nitroprusside injection must be guided by knowledge of the further metabolism of these products.
As shown in the diagram below, the essential features of nitroprusside metabolism are
- one molecule of sodium nitroprusside is metabolized by combination with hemoglobin to produce one molecule of cyanmethemoglobin and four CN-ions;
- methemoglobin, obtained from hemoglobin, can sequester cyanide as cyanmethemoglobin;
- thiosulfate reacts with cyanide to produce thiocyanate;
- thiocyanate is eliminated in the urine;
- cyanide not otherwise removed binds to cytochromes; and
- cyanide is much more toxic than methemoglobin or thiocyanate.
Cyanide ion is normally found in serum; it is derived from dietary substrates and from tobacco smoke.
Cyanide binds avidly (but reversibly) to ferric ion (Fe+++), most body stores of which are found in erythrocyte methemoglobin (metHgb) and in mitochondrial cytochromes. When CN–is infused or generated within the bloodstream, essentially all of it is bound to methemoglobin until intraerythrocytic methemoglobin has been saturated.
When the Fe+++of cytochromes is bound to cyanide, the cytochromes are unable to participate in oxidative metabolism. In this situation, cells may be able to provide for their energy needs by utilizing anaerobic pathways, but they thereby generate an increasing body burden of lactic acid. Other cells may be unable to utilize these alternative pathways, and they may die hypoxic deaths.
CN–levels in packed erythrocytes are typically less than 1 mcmol/L (less than 25 mcg/L); levels are roughly doubled in heavy smokers.
At healthy steady state, most people have less than 1% of their hemoglobin in the form of methemoglobin. Nitroprusside metabolism can lead to methemoglobin formation (a) through dissociation of cyanmethemoglobin formed in the original reaction of sodium nitroprusside with Hgb and (b) by direct oxidation of Hgb by the released nitroso group. Relatively large quantities of sodium nitroprusside, however, are required to produce significant methemoglobinemia.
At physiologic methemoglobin levels, the CN–binding capacity of packed red cells is a little less than 200 mcmol/L (5 mg/L). Cytochrome toxicity is seen at levels only slightly higher, and death has been reported at levels from 300 to 3000 mcmol/L (8 to 80 mg/L). Put another way, a patient with a normal red-cell mass (35 mL/kg) and normal methemoglobin levels can buffer about 175 mcg/kg of CN–, corresponding to a little less than 500 mcg/kg of infused sodium nitroprusside.
Some cyanide is eliminated from the body as expired hydrogen cyanide, but most is enzymatically converted to thiocyanate (SCN–) by thiosulfate-cyanide sulfur transferase (rhodanase, EC 2.8.1.1), a mitochondrial enzyme. The enzyme is normally present in great excess, so the reaction is rate-limited by the availability of sulfur donors, especially thiosulfate, cystine, and cysteine.
Thiosulfate is a normal constituent of serum, produced from cysteine by way of β-mercaptopyruvate. Physiological levels of thiosulfate are typically about 0.1 mmol/L (11 mg/L), but they are approximately twice this level in pediatric and adult patients who are not eating. Infused thiosulfate is cleared from the body (primarily by the kidneys) with a half-life of about 20 minutes.
When thiosulfate is being supplied only by normal physiologic mechanisms, conversion of CN–to SCN–generally proceeds at about 1 mcg/kg/min. This rate of CN–clearance corresponds to steady-state processing of a sodium nitroprusside infusion of slightly more than 2 mcg/kg/min. CN–begins to accumulate when sodium nitroprusside infusions exceed this rate.
Thiocyanate (SCN–) is also a normal physiological constituent of serum, with normal levels typically in the range of 50 to 250 mcmol/L (3 to 15 mg/L). Clearance of SCN–is primarily renal, with a half-life of about 3 days. In renal failure, the half-life can be doubled or tripled.
Clinical trials have also shown that the hypotensive effect of sodium nitroprusside is associated with reduced blood loss in a variety of major surgical procedures.
In patients with acute congestive heart failure and increased peripheral vascular resistance, administration of sodium nitroprusside causes reductions in peripheral resistance, increases in cardiac output, and reductions in left ventricular filling pressure.
Many trials have verified the clinical significance of the metabolic pathways described above. In patients receiving unopposed infusions of sodium nitroprusside, cyanide and thiocyanate levels have increased with increasing rates of sodium nitroprusside infusion. Mild to moderate metabolic acidosis has usually accompanied higher cyanide levels, but peak base deficits have lagged behind the peak cyanide levels by an hour or more.
Progressive tachyphylaxis to the hypotensive effects of sodium nitroprusside has been reported in several trials and numerous case reports. This tachyphylaxis has frequently been attributed to concomitant cyanide toxicity, but the only evidence adduced for this assertion has been the observation that in patients treated with sodium nitroprusside and found to be resistant to its hypotensive effects, cyanide levels are often found to be elevated. In the only reported
There were 203 pediatric patients in a parallel, dose-ranging study (Study 1). During the 30 minute blinded phase, patients were randomized 1:1:1:1 to receive sodium nitroprusside 0.3, 1, 2, or 3 mcg/kg/min. The infusion rate was increased step-wise to the target dose rate (i.e., 1/3 of the full rate for the first 5 minutes, 2/3 of the full rate for the next 5 minutes, and the full dose rate for the last 20 minutes). If the investigator believed that an increase to the next higher dose rate would be unsafe, the infusion remained at the current rate for the remainder of the blinded infusion. Since there was no placebo group, the change from baseline likely overestimates the true magnitude of blood pressure effect. Nevertheless, MAP decreased 11 to 20 mmHg from baseline across the four doses (Table 1).
There were 63 pediatric patients in a long-term infusion trial (Study 2). During an open-label phase (12 to 24 hours), sodium nitroprusside was started at ≤0.3 mcg/kg/min and titrated according to the BP response. Patients were then randomized to placebo or to continuing the same dose of sodium nitroprusside. The average MAP was greater in the control group than in the sodium nitroprusside group for every time point during the blinded withdrawal phase, demonstrating that sodium nitroprusside is effective for at least 12 hours. In both studies, similar effects on MAP were seen in all age groups.
Treatment | ||||
Endpoint | 0.3 mcg/kg/min (N=50) | 1 mcg/kg/min (N=49) | 2 mcg/kg/min (N=53) | 3 mcg/kg/min (N=51) |
Baseline | 76 ± 11 | 77 ± 15 | 74 ± 12 | 76 ± 12 |
30 Min | 65 ± 13 | 60 ± 15 | 54 ± 12 | 60 ± 18 |
Change from Baseline | -11 ± 16 (-15, -6.5) | -17 ± 13 (-21, -13) | -20 ± 16 (-24, -16) | -17 ± 19 (-22, -11) |
Mean ± SD (95% Cl) | ||||
Methemoglobin levels can be measured by most clinical laboratories. The diagnosis should be suspected in patients who have received >10 mg/kg of sodium nitroprusside and who exhibit signs of impaired oxygen delivery despite adequate cardiac output and adequate arterial pO2. Classically, methemoglobinemic blood is described as chocolate brown, without color change on exposure to air.
When methemoglobinemia is diagnosed, the treatment of choice is 1 to 2 mg/kg of methylene blue, administered intravenously over several minutes. In patients likely to have substantial amounts of cyanide bound to methemoglobin as cyanmethemoglobin, treatment of methemoglobinemia with methylene blue must be undertaken with extreme caution.
The principal pharmacological action of sodium nitroprusside is relaxation of vascular smooth muscle and consequent dilatation of peripheral arteries and veins. Other smooth muscle (e.g., uterus, duodenum) is not affected. Sodium nitroprusside is more active on veins than on arteries, but this selectivity is much less marked than that of nitroglycerin. Dilatation of the veins promotes peripheral pooling of blood and decreases venous return to the heart, thereby reducing left ventricular end diastolic pressure and pulmonary capillary wedge pressure (preload). Arteriolar relaxation reduces systemic vascular resistance, systolic arterial pressure, and mean arterial pressure (afterload). Dilatation of the coronary arteries also occurs.
In association with the decrease in blood pressure, sodium nitroprusside administered intravenously to hypertensive and normotensive patients produces slight increases in heart rate and a variable effect on cardiac output. In hypertensive patients, moderate doses induce renal vasodilatation roughly proportional to the decrease in systemic blood pressure, so there is no appreciable change in renal blood flow or glomerular filtration rate.
In normotensive subjects, acute reduction of mean arterial pressure to 60 to 75 mm Hg by infusion of sodium nitroprusside caused a significant increase in renin activity. In the same study, ten renovascular-hypertensive patients given sodium nitroprusside had significant increases in renin release from the involved kidney at mean arterial pressures of 90 to 137 mm Hg.
The hypotensive effect of sodium nitroprusside is seen within a minute or two after the start of an adequate infusion, and it dissipates almost as rapidly after an infusion is discontinued. The effect is augmented by ganglionic blocking agents and inhaled anesthetics.
The products of the nitroprusside/hemoglobin reaction are cyanmethemoglobin (cyanmetHgb) and cyanide ion (CN-). Safe use of sodium nitroprusside injection must be guided by knowledge of the further metabolism of these products.
As shown in the diagram below, the essential features of nitroprusside metabolism are
- one molecule of sodium nitroprusside is metabolized by combination with hemoglobin to produce one molecule of cyanmethemoglobin and four CN-ions;
- methemoglobin, obtained from hemoglobin, can sequester cyanide as cyanmethemoglobin;
- thiosulfate reacts with cyanide to produce thiocyanate;
- thiocyanate is eliminated in the urine;
- cyanide not otherwise removed binds to cytochromes; and
- cyanide is much more toxic than methemoglobin or thiocyanate.
Cyanide ion is normally found in serum; it is derived from dietary substrates and from tobacco smoke.
Cyanide binds avidly (but reversibly) to ferric ion (Fe+++), most body stores of which are found in erythrocyte methemoglobin (metHgb) and in mitochondrial cytochromes. When CN–is infused or generated within the bloodstream, essentially all of it is bound to methemoglobin until intraerythrocytic methemoglobin has been saturated.
When the Fe+++of cytochromes is bound to cyanide, the cytochromes are unable to participate in oxidative metabolism. In this situation, cells may be able to provide for their energy needs by utilizing anaerobic pathways, but they thereby generate an increasing body burden of lactic acid. Other cells may be unable to utilize these alternative pathways, and they may die hypoxic deaths.
CN–levels in packed erythrocytes are typically less than 1 mcmol/L (less than 25 mcg/L); levels are roughly doubled in heavy smokers.
At healthy steady state, most people have less than 1% of their hemoglobin in the form of methemoglobin. Nitroprusside metabolism can lead to methemoglobin formation (a) through dissociation of cyanmethemoglobin formed in the original reaction of sodium nitroprusside with Hgb and (b) by direct oxidation of Hgb by the released nitroso group. Relatively large quantities of sodium nitroprusside, however, are required to produce significant methemoglobinemia.
At physiologic methemoglobin levels, the CN–binding capacity of packed red cells is a little less than 200 mcmol/L (5 mg/L). Cytochrome toxicity is seen at levels only slightly higher, and death has been reported at levels from 300 to 3000 mcmol/L (8 to 80 mg/L). Put another way, a patient with a normal red-cell mass (35 mL/kg) and normal methemoglobin levels can buffer about 175 mcg/kg of CN–, corresponding to a little less than 500 mcg/kg of infused sodium nitroprusside.
Some cyanide is eliminated from the body as expired hydrogen cyanide, but most is enzymatically converted to thiocyanate (SCN–) by thiosulfate-cyanide sulfur transferase (rhodanase, EC 2.8.1.1), a mitochondrial enzyme. The enzyme is normally present in great excess, so the reaction is rate-limited by the availability of sulfur donors, especially thiosulfate, cystine, and cysteine.
Thiosulfate is a normal constituent of serum, produced from cysteine by way of β-mercaptopyruvate. Physiological levels of thiosulfate are typically about 0.1 mmol/L (11 mg/L), but they are approximately twice this level in pediatric and adult patients who are not eating. Infused thiosulfate is cleared from the body (primarily by the kidneys) with a half-life of about 20 minutes.
When thiosulfate is being supplied only by normal physiologic mechanisms, conversion of CN–to SCN–generally proceeds at about 1 mcg/kg/min. This rate of CN–clearance corresponds to steady-state processing of a sodium nitroprusside infusion of slightly more than 2 mcg/kg/min. CN–begins to accumulate when sodium nitroprusside infusions exceed this rate.
Thiocyanate (SCN–) is also a normal physiological constituent of serum, with normal levels typically in the range of 50 to 250 mcmol/L (3 to 15 mg/L). Clearance of SCN–is primarily renal, with a half-life of about 3 days. In renal failure, the half-life can be doubled or tripled.
Clinical trials have also shown that the hypotensive effect of sodium nitroprusside is associated with reduced blood loss in a variety of major surgical procedures.
In patients with acute congestive heart failure and increased peripheral vascular resistance, administration of sodium nitroprusside causes reductions in peripheral resistance, increases in cardiac output, and reductions in left ventricular filling pressure.
Many trials have verified the clinical significance of the metabolic pathways described above. In patients receiving unopposed infusions of sodium nitroprusside, cyanide and thiocyanate levels have increased with increasing rates of sodium nitroprusside infusion. Mild to moderate metabolic acidosis has usually accompanied higher cyanide levels, but peak base deficits have lagged behind the peak cyanide levels by an hour or more.
Progressive tachyphylaxis to the hypotensive effects of sodium nitroprusside has been reported in several trials and numerous case reports. This tachyphylaxis has frequently been attributed to concomitant cyanide toxicity, but the only evidence adduced for this assertion has been the observation that in patients treated with sodium nitroprusside and found to be resistant to its hypotensive effects, cyanide levels are often found to be elevated. In the only reported
There were 203 pediatric patients in a parallel, dose-ranging study (Study 1). During the 30 minute blinded phase, patients were randomized 1:1:1:1 to receive sodium nitroprusside 0.3, 1, 2, or 3 mcg/kg/min. The infusion rate was increased step-wise to the target dose rate (i.e., 1/3 of the full rate for the first 5 minutes, 2/3 of the full rate for the next 5 minutes, and the full dose rate for the last 20 minutes). If the investigator believed that an increase to the next higher dose rate would be unsafe, the infusion remained at the current rate for the remainder of the blinded infusion. Since there was no placebo group, the change from baseline likely overestimates the true magnitude of blood pressure effect. Nevertheless, MAP decreased 11 to 20 mmHg from baseline across the four doses (Table 1).
There were 63 pediatric patients in a long-term infusion trial (Study 2). During an open-label phase (12 to 24 hours), sodium nitroprusside was started at ≤0.3 mcg/kg/min and titrated according to the BP response. Patients were then randomized to placebo or to continuing the same dose of sodium nitroprusside. The average MAP was greater in the control group than in the sodium nitroprusside group for every time point during the blinded withdrawal phase, demonstrating that sodium nitroprusside is effective for at least 12 hours. In both studies, similar effects on MAP were seen in all age groups.
Treatment | ||||
Endpoint | 0.3 mcg/kg/min (N=50) | 1 mcg/kg/min (N=49) | 2 mcg/kg/min (N=53) | 3 mcg/kg/min (N=51) |
Baseline | 76 ± 11 | 77 ± 15 | 74 ± 12 | 76 ± 12 |
30 Min | 65 ± 13 | 60 ± 15 | 54 ± 12 | 60 ± 18 |
Change from Baseline | -11 ± 16 (-15, -6.5) | -17 ± 13 (-21, -13) | -20 ± 16 (-24, -16) | -17 ± 19 (-22, -11) |
Mean ± SD (95% Cl) | ||||
Thiocyanate is mildly neurotoxic (tinnitus, miosis, hyperreflexia) at serum levels of 1 mmol/L (60 mg/L). Thiocyanate toxicity is life-threatening when levels are 3 or 4 times higher (200 mg/L).
The steady-state thiocyanate level after prolonged infusions of sodium nitroprusside is increased with increased infusion rate, and the half-time of accumulation is 3 to 4 days. To keep the steady-state thiocyanate level below 1 mmol/L, a prolonged infusion of sodium nitroprusside should not be more rapid than 3 mcg/kg/min; in anuric patients, the corresponding limit is just 1 mcg/kg/min. When prolonged infusions are more rapid than these, thiocyanate levels should be measured daily.
Physiologic maneuvers (e.g., those that alter the pH of the urine) are not known to increase the elimination of thiocyanate. Thiocyanate clearance rates during dialysis, on the other hand, can approach the blood flow rate of the dialyzer.
Thiocyanate interferes with iodine uptake by the thyroid.
Abdominal pain, apprehension, diaphoresis, “dizziness,” headache, muscle twitching, nausea, palpitations, restlessness, retching, and retrosternal discomfort have been noted when the blood pressure was too rapidly reduced. These symptoms quickly disappeared when the infusion was slowed or discontinued, and they did not reappear with a continued (or resumed) slower infusion.
Other adverse reactions reported are:
To report SUSPECTED ADVERSE REACTIONS, contact Hainan Poly Pharm. Co., Ltd. at 1-800-571-8369 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.