Solu-medrol
(Methylprednisolone Sodium Succinate)Solu-Medrol Prescribing Information
When oral therapy is not feasible, and the strength, dosage form, and route of administration of the drug reasonably lend the preparation to the treatment of the condition, the
SOLU-MEDROL Sterile Powder is an anti-inflammatory glucocorticoid, which contains methylprednisolone sodium succinate as the active ingredient. Methylprednisolone sodium succinate, USP, is the sodium succinate ester of methylprednisolone, and it occurs as a white, or nearly white, odorless hygroscopic, amorphous solid. It is very soluble in water and in alcohol; it is insoluble in chloroform and is very slightly soluble in acetone.
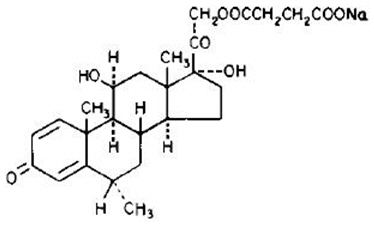
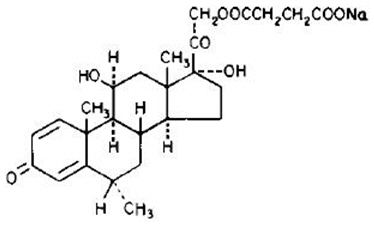
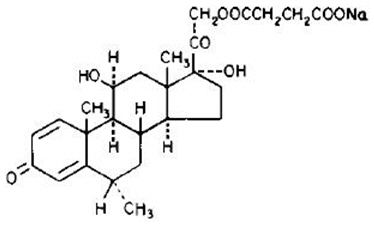
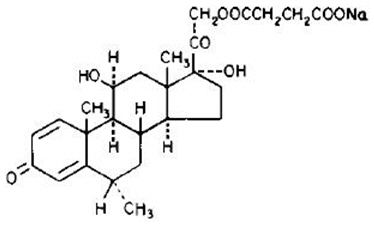
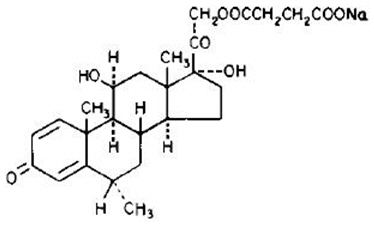
The chemical name for methylprednisolone sodium succinate is pregna-1,4-diene-3,20-dione,21-(3-carboxy-1-oxopropoxy)-11,17-dihydroxy-6-methyl-monosodium salt, (6α, 11β), and the molecular weight is 496.53. The structural formula is represented below:
Methylprednisolone sodium succinate is soluble in water; it may be administered in a small volume of diluent and is well suited for intravenous use in situations where high blood levels of methylprednisolone are required rapidly.
SOLU-MEDROL is available in preservative and preservative-free formulations:
Preservative-free Formulations |
40 mg Act-O-Vial System (Single-Dose Vial) —Each mL (when mixed) contains methylprednisolone sodium succinate equivalent to 40 mg methylprednisolone; also 1.6 mg monobasic sodium phosphate anhydrous; 17.46 mg dibasic sodium phosphate dried; and 25 mg lactose hydrous. |
125 mg Act-O-Vial System (Single-Dose Vial) —Each 2 mL (when mixed) contains methylprednisolone sodium succinate equivalent to 125 mg methylprednisolone; also 1.6 mg monobasic sodium phosphate anhydrous; and 17.4 mg dibasic sodium phosphate dried. |
Formulations preserved with Benzyl Alcohol |
1 gram Vial —Each 16 mL (when mixed as directed) contains methylprednisolone sodium succinate equivalent to 1 gram methylprednisolone; also 12.8 mg monobasic sodium phosphate anhydrous; 139.2 mg dibasic sodium phosphate dried. |
This package does not contain diluent. Recommended diluent (Bacteriostatic water) contains benzyl alcohol as a preservative. |
IMPORTANT — Use only the accompanying diluent or Bacteriostatic Water For Injection with Benzyl Alcohol when reconstituting SOLU-MEDROL. |
Use within 48 hours after mixing. |
When necessary, the pH of each formula was adjusted with sodium hydroxide so that the pH of the reconstituted solution is within the USP specified range of 7 to 8.
Serious neurologic events, some resulting in death, have been reported with epidural injection of corticosteroids. Specific events reported include, but are not limited to, spinal cord infarction, paraplegia, quadriplegia, cortical blindness, and stroke. These serious neurologic events have been reported with and without use of fluoroscopy. The safety and effectiveness of epidural administration of corticosteroids have not been established, and corticosteroids are not approved for this use.
Injection of SOLU-MEDROL may result in dermal and/or subdermal changes forming depressions in the skin at the injection site. In order to minimize the incidence of dermal and subdermal atrophy, care must be exercised not to exceed recommended doses in injections. Injection into the deltoid muscle should be avoided because of a high incidence of subcutaneous atrophy.
Rare instances of anaphylactoid reactions have occurred in patients receiving corticosteroid therapy (see
In patients receiving the 40 mg presentation of SOLU-MEDROL during the treatment for acute allergic conditions and where these symptoms worsen or any new allergic symptoms occur, consideration should be given to the potential for hypersensitivity reactions to cow's milk ingredients (see
Increased dosage of rapidly acting corticosteroids is indicated in patients on corticosteroid therapy who are subjected to any unusual stress before, during, and after the stressful situation.
Results from one multicenter, randomized, placebo-controlled study with methylprednisolone hemisuccinate, an intravenous corticosteroid, showed an increase in early (at 2 weeks) and late (at 6 months) mortality in patients with cranial trauma who were determined not to have other clear indications for corticosteroid treatment. High doses of systemic corticosteroids, including SOLU-MEDROL, should not be used for the treatment of traumatic brain injury.
Average and large doses of corticosteroids can cause elevation of blood pressure, salt and water retention, and increased excretion of potassium. These effects are less likely to occur with the synthetic derivatives except when used in large doses. Dietary salt restriction and potassium supplementation may be necessary. All corticosteroids increase calcium excretion.
Literature reports suggest an apparent association between the use of corticosteroids and left ventricular free wall rupture after a recent myocardial infarction; therefore, therapy with corticosteroids should be used with great caution in these patients.
There have been cases reported in which concomitant use of amphotericin B and hydrocortisone was followed by cardiac enlargement and congestive heart failure (see
Hypothalamic-pituitary adrenal (HPA) axis suppression, Cushing's syndrome, and hyperglycemia. Monitor patients for these conditions with chronic use.
Corticosteroids can produce reversible HPA axis suppression with the potential for glucocorticosteroid insufficiency after withdrawal of treatment. Drug induced secondary adrenocortical insufficiency may be minimized by gradual reduction of dosage. This type of relative insufficiency may persist for months after discontinuation of therapy; therefore, in any situation of stress occurring during that period, hormone therapy should be reinstituted.
Corticosteroids, including SOLU-MEDROL, suppress the immune system and increase the risk of infection with any pathogen, including viral, bacterial, fungal, protozoan, or helminthic pathogens. Corticosteroids can:
• Reduce resistance to new infections• Exacerbate existing infections• Increase the risk of disseminated infections• Increase the risk of reactivation or exacerbation of latent infections• Mask some signs of infection
Corticosteroid‑associated infections can be mild but can be severe and at times fatal. The rate of infectious complications increases with increasing corticosteroid dosages.
A study has failed to establish the efficacy of methylprednisolone sodium succinate in the treatment of sepsis syndrome and septic shock. The study also suggests that treatment of these conditions with methylprednisolone sodium succinate may increase the risk of mortality in certain patients (i.e., patients with elevated serum creatinine levels or patients who develop secondary infections after methylprednisolone sodium succinate).
Monitor for the development of infection and consider SOLU-MEDROL withdrawal or dosage reduction as needed.
If SOLU-MEDROL is used to treat a condition in patients with latent tuberculosis or tuberculin reactivity, reactivation of the disease may occur. Closely monitor such patients for reactivation. During prolonged SOLU-MEDROL therapy, patients with latent tuberculosis or tuberculin reactivity should receive chemoprophylaxis.
Varicella and measles can have a serious or even fatal course in non-immune patients taking corticosteroids, including SOLU-MEDROL. In corticosteroid-treated patients who have not had these diseases or are non-immune, particular care should be taken to avoid exposure to varicella and measles:
• If a SOLU‑MEDROL‑treated patient is exposed to varicella, prophylaxis with varicella zoster immune globulin (VZIG) may be indicated. If varicella develops, treatment with antiviral agents may be considered.• If a SOLU‑MEDROL‑treated patient is exposed to measles, prophylaxis with immunoglobulin (IG) may be indicated.
Hepatitis B virus reactivation can occur in patients who are hepatitis B carriers treated with immunosuppressive dosages of corticosteroids, including SOLU-MEDROL. Reactivation can also occur infrequently in corticosteroid-treated patients who appear to have resolved hepatitis B infection.
Screen patients for hepatitis B infection before initiating immunosuppressive (e.g., prolonged) treatment with SOLU-MEDROL. For patients who show evidence of hepatitis B infection, recommend consultation with physicians with expertise in managing hepatitis B regarding monitoring and consideration for hepatitis B antiviral therapy.
Corticosteroids, including SOLU-MEDROL, may exacerbate systemic fungal infections; therefore, avoid SOLU-MEDROL use in the presence of such infections unless SOLU‑MEDROL is needed to control drug reactions. For patients on chronic SOLU‑MEDROL therapy who develop systemic fungal infections, SOLU-MEDROL withdrawal or dosage reduction is recommended.
Corticosteroids, including SOLU-MEDROL, may activate latent amebiasis. Therefore, it is recommended that latent amebiasis or active amebiasis be ruled out before initiating SOLU-MEDROL in patients who have spent time in the tropics or patients with unexplained diarrhea.
Corticosteroids, including SOLU-MEDROL, should be used with great care in patients with known or suspected Strongyloides (threadworm) infestation. In such patients, corticosteroid-induced immunosuppression may lead to Strongyloides hyperinfection and dissemination with widespread larval migration, often accompanied by severe enterocolitis and potentially fatal gram-negative septicemia.
Avoid corticosteroids, including SOLU-MEDROL, in patients with cerebral malaria.
Rarely, high doses of cyclically pulsed intravenous methylprednisolone (usually for the treatment of exacerbations of multiple sclerosis at doses of 1 gram/day) can induce a toxic form of acute hepatitis. The time to onset of this form of steroid-induced liver injury can be several weeks or longer. Resolution has been observed after discontinuation of treatment. However, serious liver injury can occur, sometimes resulting in acute liver failure and death. Discontinue intravenous methylprednisolone if toxic hepatitis occurs. Since recurrence has occurred after re-challenge, avoid use of high dose intravenous methylprednisolone in patients with a history of toxic hepatitis caused by methylprednisolone.
Reports of severe medical events have been associated with the intrathecal route of administration (see
Use of corticosteroids may produce posterior subcapsular cataracts, glaucoma with possible damage to the optic nerves, and may enhance the establishment of secondary ocular infections due to bacteria, fungi, or viruses. The use of oral corticosteroids is not recommended in the treatment of optic neuritis and may lead to an increase in the risk of new episodes. Corticosteroids should be used cautiously in patients with ocular herpes simplex because of corneal perforation. Corticosteroids should not be used in active ocular herpes simplex.
Kaposi’s sarcoma has been reported to occur in patients receiving corticosteroid therapy, most often for chronic conditions. Discontinuation of corticosteroids may result in clinical improvement of Kaposi’s sarcoma.
Some formulations of this product contain benzyl alcohol as a preservative (see
Benzyl alcohol, a component of this product, has been associated with serious adverse events and death, particularly in pediatric patients. The "gasping syndrome" (characterized by central nervous system depression, metabolic acidosis, gasping respirations, and high levels of benzyl alcohol and its metabolites found in the blood and urine) has been associated with benzyl alcohol dosages >99 mg/kg/day in neonates and low-birth-weight neonates. Additional symptoms may include gradual neurological deterioration, seizures, intracranial hemorrhage, hematologic abnormalities, skin breakdown, hepatic and renal failure, hypotension, bradycardia, and cardiovascular collapse. Although normal therapeutic doses of this product ordinarily delivers amounts of benzyl alcohol that are substantially lower than those reported in association with the "gasping syndrome", the minimum amount of benzyl alcohol at which toxicity may occur is not known. The risk of benzyl alcohol toxicity depends on the quantity administered and the hepatic capacity to detoxify the chemical. Premature and low-birth-weight infants, as well as patients receiving high dosages, may be more likely to develop toxicity. Practitioners administering this and other medications containing benzyl alcohol should consider the combined daily metabolic load of benzyl alcohol from all sources.
The efficacy and safety of corticosteroids in the pediatric population are based on the well-established course of effect of corticosteroids which is similar in pediatric and adult populations. Published studies provide evidence of efficacy and safety in pediatric patients for the treatment of nephrotic syndrome (>2 years of age), and aggressive lymphomas and leukemias (>1 month of age). Other indications for pediatric use of corticosteroids, e.g., severe asthma and wheezing, are based on adequate and well-controlled trials conducted in adults, on the premises that the course of the diseases and their pathophysiology are considered to be substantially similar in both populations.
The adverse effects of corticosteroids in pediatric patients are similar to those in adults (see
Hypertrophic cardiomyopathy may develop after administration of methylprednisolone to prematurely born infants, therefore appropriate diagnostic evaluation and monitoring of cardiac function and structure should be performed.
Use only the accompanying diluent or Bacteriostatic Water For Injection with Benzyl Alcohol when reconstituting SOLU-MEDROL (see
SOLU-MEDROL Sterile Powder is an anti-inflammatory glucocorticoid, which contains methylprednisolone sodium succinate as the active ingredient. Methylprednisolone sodium succinate, USP, is the sodium succinate ester of methylprednisolone, and it occurs as a white, or nearly white, odorless hygroscopic, amorphous solid. It is very soluble in water and in alcohol; it is insoluble in chloroform and is very slightly soluble in acetone.
The chemical name for methylprednisolone sodium succinate is pregna-1,4-diene-3,20-dione,21-(3-carboxy-1-oxopropoxy)-11,17-dihydroxy-6-methyl-monosodium salt, (6α, 11β), and the molecular weight is 496.53. The structural formula is represented below:
Methylprednisolone sodium succinate is soluble in water; it may be administered in a small volume of diluent and is well suited for intravenous use in situations where high blood levels of methylprednisolone are required rapidly.
SOLU-MEDROL is available in preservative and preservative-free formulations:
Preservative-free Formulations |
40 mg Act-O-Vial System (Single-Dose Vial) —Each mL (when mixed) contains methylprednisolone sodium succinate equivalent to 40 mg methylprednisolone; also 1.6 mg monobasic sodium phosphate anhydrous; 17.46 mg dibasic sodium phosphate dried; and 25 mg lactose hydrous. |
125 mg Act-O-Vial System (Single-Dose Vial) —Each 2 mL (when mixed) contains methylprednisolone sodium succinate equivalent to 125 mg methylprednisolone; also 1.6 mg monobasic sodium phosphate anhydrous; and 17.4 mg dibasic sodium phosphate dried. |
Formulations preserved with Benzyl Alcohol |
1 gram Vial —Each 16 mL (when mixed as directed) contains methylprednisolone sodium succinate equivalent to 1 gram methylprednisolone; also 12.8 mg monobasic sodium phosphate anhydrous; 139.2 mg dibasic sodium phosphate dried. |
This package does not contain diluent. Recommended diluent (Bacteriostatic water) contains benzyl alcohol as a preservative. |
IMPORTANT — Use only the accompanying diluent or Bacteriostatic Water For Injection with Benzyl Alcohol when reconstituting SOLU-MEDROL. |
Use within 48 hours after mixing. |
When necessary, the pH of each formula was adjusted with sodium hydroxide so that the pH of the reconstituted solution is within the USP specified range of 7 to 8.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
This preparation may be administered by intravenous injection, by intravenous infusion, or by intramuscular injection, the preferred method for initial emergency use being intravenous injection. Following the initial emergency period, consideration should be given to employing a longer acting injectable preparation or an oral preparation.
There are reports of cardiac arrhythmias and/or cardiac arrest following the rapid administration of large intravenous doses of SOLU-MEDROL (
In general, high dose corticosteroid therapy should be continued only until the patient's condition has stabilized; usually not beyond 48 to 72 hours.
In other indications, initial dosage will vary from 10 to 40 mg of methylprednisolone depending on the specific disease entity being treated. However, in certain overwhelming, acute, life-threatening situations, administrations in dosages exceeding the usual dosages may be justified and may be in multiples of the oral dosages.
SOLU-MEDROL may be administered by intravenous or intramuscular injection or by intravenous infusion, the preferred method for initial emergency use being intravenous injection. To administer by intravenous (or intramuscular) injection, prepare solution as directed. The desired dose may be administered intravenously over a period of several minutes. If desired, the medication may be administered in diluted solutions by adding Water for Injection or other suitable diluent (see below) to the
To prepare solutions for intravenous infusion, first prepare the solution for injection as directed. This solution may then be added to indicated amounts of 5% dextrose in water, isotonic saline solution, or 5% dextrose in isotonic saline solution. From a microbiological point of view, unless the method of opening/reconstitution/dilution precludes the risk of microbial contamination, the product should be used immediately. If not used immediately, in-use storage times and conditions are the responsibility of the user. Chemical and physical stability of the further diluted product has been demonstrated within 4 hours of preparation if stored below 25°C or within 24 hours of preparation if stored at 2°C to 8°C.
In pediatric patients, the initial dose of methylprednisolone may vary depending on the specific disease entity being treated. The range of initial doses is 0.11 to 1.6 mg/kg/day in three or four divided doses (3.2 to 48 mg/m2bsa/day).
The National Heart, Lung, and Blood Institute (NHLBI) recommended dosing for systemic
Dosage may be reduced for infants and children but should be governed more by the severity of the condition and response of the patient than by age or size. It should not be less than 0.5 mg per kg every 24 hours.
Dosage must be decreased or discontinued gradually when the drug has been administered for more than a few days. If a period of spontaneous remission occurs in a chronic condition, treatment should be discontinued. Routine laboratory studies, such as urinalysis, two-hour postprandial blood sugar, determination of blood pressure and body weight, and a chest X-ray should be made at regular intervals during prolonged therapy. Upper GI X-rays are desirable in patients with an ulcer history or significant dyspepsia.
In treatment of acute exacerbations of multiple sclerosis, daily doses of 160 mg of methylprednisolone for a week followed by 64 mg every other day for 1 month have been shown to be effective (see
Although controlled clinical trials have shown corticosteroids to be effective in speeding the resolution of acute exacerbations of multiple sclerosis, they do not show that corticosteroids affect the ultimate outcome or natural history of the disease. The studies do show that relatively high doses of corticosteroids are necessary to demonstrate a significant effect (see
An acute myopathy has been observed with the use of high doses of corticosteroids, most often occurring in patients with disorders of neuromuscular transmission (e.g., myasthenia gravis), or in patients receiving concomitant therapy with neuromuscular blocking drugs (e.g., pancuronium). This acute myopathy is generalized, may involve ocular and respiratory muscles, and may result in quadriparesis. Elevations of creatine kinase may occur. Clinical improvement or recovery after stopping corticosteroids may require weeks to years.
Psychic derangements may appear when corticosteroids are used, ranging from euphoria, insomnia, mood swings, personality changes, and severe depression, to frank psychotic manifestations. Also, existing emotional instability or psychotic tendencies may be aggravated by corticosteroids.
Cortisone, 25 | Triamcinolone, 4 |
Hydrocortisone, 20 | Paramethasone, 2 |
Prednisolone, 5 | Betamethasone, 0.75 |
Prednisone, 5 | Dexamethasone, 0.75 |
Methylprednisolone, 4 |
SOLU-MEDROL Sterile Powder is contraindicated:
• in systemic fungal infections and patients with known hypersensitivity to the product and its constituents. The SOLU-MEDROL 40 mg presentation includes lactose monohydrate produced from cow's milk. This presentation is therefore contraindicated in patients with a known or suspected hypersensitivity to cow's milk or its components or other dairy products because it may contain trace amounts of milk ingredients.• for intrathecal administration. Reports of severe medical events have been associated with this route of administration.
Intramuscular corticosteroid preparations are contraindicated for idiopathic thrombocytopenic purpura.
Additional contraindication for the use of SOLU-MEDROL Sterile Powder preserved with benzyl alcohol:
Formulations preserved with benzyl alcohol are contraindicated for use in premature infants (see
Serious neurologic events, some resulting in death, have been reported with epidural injection of corticosteroids. Specific events reported include, but are not limited to, spinal cord infarction, paraplegia, quadriplegia, cortical blindness, and stroke. These serious neurologic events have been reported with and without use of fluoroscopy. The safety and effectiveness of epidural administration of corticosteroids have not been established, and corticosteroids are not approved for this use.
Injection of SOLU-MEDROL may result in dermal and/or subdermal changes forming depressions in the skin at the injection site. In order to minimize the incidence of dermal and subdermal atrophy, care must be exercised not to exceed recommended doses in injections. Injection into the deltoid muscle should be avoided because of a high incidence of subcutaneous atrophy.
Rare instances of anaphylactoid reactions have occurred in patients receiving corticosteroid therapy (see
In patients receiving the 40 mg presentation of SOLU-MEDROL during the treatment for acute allergic conditions and where these symptoms worsen or any new allergic symptoms occur, consideration should be given to the potential for hypersensitivity reactions to cow's milk ingredients (see
Increased dosage of rapidly acting corticosteroids is indicated in patients on corticosteroid therapy who are subjected to any unusual stress before, during, and after the stressful situation.
Results from one multicenter, randomized, placebo-controlled study with methylprednisolone hemisuccinate, an intravenous corticosteroid, showed an increase in early (at 2 weeks) and late (at 6 months) mortality in patients with cranial trauma who were determined not to have other clear indications for corticosteroid treatment. High doses of systemic corticosteroids, including SOLU-MEDROL, should not be used for the treatment of traumatic brain injury.
Average and large doses of corticosteroids can cause elevation of blood pressure, salt and water retention, and increased excretion of potassium. These effects are less likely to occur with the synthetic derivatives except when used in large doses. Dietary salt restriction and potassium supplementation may be necessary. All corticosteroids increase calcium excretion.
Literature reports suggest an apparent association between the use of corticosteroids and left ventricular free wall rupture after a recent myocardial infarction; therefore, therapy with corticosteroids should be used with great caution in these patients.
There have been cases reported in which concomitant use of amphotericin B and hydrocortisone was followed by cardiac enlargement and congestive heart failure (see
Hypothalamic-pituitary adrenal (HPA) axis suppression, Cushing's syndrome, and hyperglycemia. Monitor patients for these conditions with chronic use.
Corticosteroids can produce reversible HPA axis suppression with the potential for glucocorticosteroid insufficiency after withdrawal of treatment. Drug induced secondary adrenocortical insufficiency may be minimized by gradual reduction of dosage. This type of relative insufficiency may persist for months after discontinuation of therapy; therefore, in any situation of stress occurring during that period, hormone therapy should be reinstituted.
Corticosteroids, including SOLU-MEDROL, suppress the immune system and increase the risk of infection with any pathogen, including viral, bacterial, fungal, protozoan, or helminthic pathogens. Corticosteroids can:
• Reduce resistance to new infections• Exacerbate existing infections• Increase the risk of disseminated infections• Increase the risk of reactivation or exacerbation of latent infections• Mask some signs of infection
Corticosteroid‑associated infections can be mild but can be severe and at times fatal. The rate of infectious complications increases with increasing corticosteroid dosages.
A study has failed to establish the efficacy of methylprednisolone sodium succinate in the treatment of sepsis syndrome and septic shock. The study also suggests that treatment of these conditions with methylprednisolone sodium succinate may increase the risk of mortality in certain patients (i.e., patients with elevated serum creatinine levels or patients who develop secondary infections after methylprednisolone sodium succinate).
Monitor for the development of infection and consider SOLU-MEDROL withdrawal or dosage reduction as needed.
If SOLU-MEDROL is used to treat a condition in patients with latent tuberculosis or tuberculin reactivity, reactivation of the disease may occur. Closely monitor such patients for reactivation. During prolonged SOLU-MEDROL therapy, patients with latent tuberculosis or tuberculin reactivity should receive chemoprophylaxis.
Varicella and measles can have a serious or even fatal course in non-immune patients taking corticosteroids, including SOLU-MEDROL. In corticosteroid-treated patients who have not had these diseases or are non-immune, particular care should be taken to avoid exposure to varicella and measles:
• If a SOLU‑MEDROL‑treated patient is exposed to varicella, prophylaxis with varicella zoster immune globulin (VZIG) may be indicated. If varicella develops, treatment with antiviral agents may be considered.• If a SOLU‑MEDROL‑treated patient is exposed to measles, prophylaxis with immunoglobulin (IG) may be indicated.
Hepatitis B virus reactivation can occur in patients who are hepatitis B carriers treated with immunosuppressive dosages of corticosteroids, including SOLU-MEDROL. Reactivation can also occur infrequently in corticosteroid-treated patients who appear to have resolved hepatitis B infection.
Screen patients for hepatitis B infection before initiating immunosuppressive (e.g., prolonged) treatment with SOLU-MEDROL. For patients who show evidence of hepatitis B infection, recommend consultation with physicians with expertise in managing hepatitis B regarding monitoring and consideration for hepatitis B antiviral therapy.
Corticosteroids, including SOLU-MEDROL, may exacerbate systemic fungal infections; therefore, avoid SOLU-MEDROL use in the presence of such infections unless SOLU‑MEDROL is needed to control drug reactions. For patients on chronic SOLU‑MEDROL therapy who develop systemic fungal infections, SOLU-MEDROL withdrawal or dosage reduction is recommended.
Corticosteroids, including SOLU-MEDROL, may activate latent amebiasis. Therefore, it is recommended that latent amebiasis or active amebiasis be ruled out before initiating SOLU-MEDROL in patients who have spent time in the tropics or patients with unexplained diarrhea.
Corticosteroids, including SOLU-MEDROL, should be used with great care in patients with known or suspected Strongyloides (threadworm) infestation. In such patients, corticosteroid-induced immunosuppression may lead to Strongyloides hyperinfection and dissemination with widespread larval migration, often accompanied by severe enterocolitis and potentially fatal gram-negative septicemia.
Avoid corticosteroids, including SOLU-MEDROL, in patients with cerebral malaria.
Rarely, high doses of cyclically pulsed intravenous methylprednisolone (usually for the treatment of exacerbations of multiple sclerosis at doses of 1 gram/day) can induce a toxic form of acute hepatitis. The time to onset of this form of steroid-induced liver injury can be several weeks or longer. Resolution has been observed after discontinuation of treatment. However, serious liver injury can occur, sometimes resulting in acute liver failure and death. Discontinue intravenous methylprednisolone if toxic hepatitis occurs. Since recurrence has occurred after re-challenge, avoid use of high dose intravenous methylprednisolone in patients with a history of toxic hepatitis caused by methylprednisolone.
Reports of severe medical events have been associated with the intrathecal route of administration (see
Use of corticosteroids may produce posterior subcapsular cataracts, glaucoma with possible damage to the optic nerves, and may enhance the establishment of secondary ocular infections due to bacteria, fungi, or viruses. The use of oral corticosteroids is not recommended in the treatment of optic neuritis and may lead to an increase in the risk of new episodes. Corticosteroids should be used cautiously in patients with ocular herpes simplex because of corneal perforation. Corticosteroids should not be used in active ocular herpes simplex.
Kaposi’s sarcoma has been reported to occur in patients receiving corticosteroid therapy, most often for chronic conditions. Discontinuation of corticosteroids may result in clinical improvement of Kaposi’s sarcoma.
Some formulations of this product contain benzyl alcohol as a preservative (see
Benzyl alcohol, a component of this product, has been associated with serious adverse events and death, particularly in pediatric patients. The "gasping syndrome" (characterized by central nervous system depression, metabolic acidosis, gasping respirations, and high levels of benzyl alcohol and its metabolites found in the blood and urine) has been associated with benzyl alcohol dosages >99 mg/kg/day in neonates and low-birth-weight neonates. Additional symptoms may include gradual neurological deterioration, seizures, intracranial hemorrhage, hematologic abnormalities, skin breakdown, hepatic and renal failure, hypotension, bradycardia, and cardiovascular collapse. Although normal therapeutic doses of this product ordinarily delivers amounts of benzyl alcohol that are substantially lower than those reported in association with the "gasping syndrome", the minimum amount of benzyl alcohol at which toxicity may occur is not known. The risk of benzyl alcohol toxicity depends on the quantity administered and the hepatic capacity to detoxify the chemical. Premature and low-birth-weight infants, as well as patients receiving high dosages, may be more likely to develop toxicity. Practitioners administering this and other medications containing benzyl alcohol should consider the combined daily metabolic load of benzyl alcohol from all sources.
The efficacy and safety of corticosteroids in the pediatric population are based on the well-established course of effect of corticosteroids which is similar in pediatric and adult populations. Published studies provide evidence of efficacy and safety in pediatric patients for the treatment of nephrotic syndrome (>2 years of age), and aggressive lymphomas and leukemias (>1 month of age). Other indications for pediatric use of corticosteroids, e.g., severe asthma and wheezing, are based on adequate and well-controlled trials conducted in adults, on the premises that the course of the diseases and their pathophysiology are considered to be substantially similar in both populations.
The adverse effects of corticosteroids in pediatric patients are similar to those in adults (see
Hypertrophic cardiomyopathy may develop after administration of methylprednisolone to prematurely born infants, therefore appropriate diagnostic evaluation and monitoring of cardiac function and structure should be performed.
The following adverse reactions have been reported with SOLU-MEDROL or other corticosteroids:
Serious neurologic events, some resulting in death, have been reported with epidural injection of corticosteroids. Specific events reported include, but are not limited to, spinal cord infarction, paraplegia, quadriplegia, cortical blindness, and stroke. These serious neurologic events have been reported with and without use of fluoroscopy. The safety and effectiveness of epidural administration of corticosteroids have not been established, and corticosteroids are not approved for this use.
Injection of SOLU-MEDROL may result in dermal and/or subdermal changes forming depressions in the skin at the injection site. In order to minimize the incidence of dermal and subdermal atrophy, care must be exercised not to exceed recommended doses in injections. Injection into the deltoid muscle should be avoided because of a high incidence of subcutaneous atrophy.
Rare instances of anaphylactoid reactions have occurred in patients receiving corticosteroid therapy (see
In patients receiving the 40 mg presentation of SOLU-MEDROL during the treatment for acute allergic conditions and where these symptoms worsen or any new allergic symptoms occur, consideration should be given to the potential for hypersensitivity reactions to cow's milk ingredients (see
Increased dosage of rapidly acting corticosteroids is indicated in patients on corticosteroid therapy who are subjected to any unusual stress before, during, and after the stressful situation.
Results from one multicenter, randomized, placebo-controlled study with methylprednisolone hemisuccinate, an intravenous corticosteroid, showed an increase in early (at 2 weeks) and late (at 6 months) mortality in patients with cranial trauma who were determined not to have other clear indications for corticosteroid treatment. High doses of systemic corticosteroids, including SOLU-MEDROL, should not be used for the treatment of traumatic brain injury.
Average and large doses of corticosteroids can cause elevation of blood pressure, salt and water retention, and increased excretion of potassium. These effects are less likely to occur with the synthetic derivatives except when used in large doses. Dietary salt restriction and potassium supplementation may be necessary. All corticosteroids increase calcium excretion.
Literature reports suggest an apparent association between the use of corticosteroids and left ventricular free wall rupture after a recent myocardial infarction; therefore, therapy with corticosteroids should be used with great caution in these patients.
There have been cases reported in which concomitant use of amphotericin B and hydrocortisone was followed by cardiac enlargement and congestive heart failure (see
Hypothalamic-pituitary adrenal (HPA) axis suppression, Cushing's syndrome, and hyperglycemia. Monitor patients for these conditions with chronic use.
Corticosteroids can produce reversible HPA axis suppression with the potential for glucocorticosteroid insufficiency after withdrawal of treatment. Drug induced secondary adrenocortical insufficiency may be minimized by gradual reduction of dosage. This type of relative insufficiency may persist for months after discontinuation of therapy; therefore, in any situation of stress occurring during that period, hormone therapy should be reinstituted.
Corticosteroids, including SOLU-MEDROL, suppress the immune system and increase the risk of infection with any pathogen, including viral, bacterial, fungal, protozoan, or helminthic pathogens. Corticosteroids can:
• Reduce resistance to new infections• Exacerbate existing infections• Increase the risk of disseminated infections• Increase the risk of reactivation or exacerbation of latent infections• Mask some signs of infection
Corticosteroid‑associated infections can be mild but can be severe and at times fatal. The rate of infectious complications increases with increasing corticosteroid dosages.
A study has failed to establish the efficacy of methylprednisolone sodium succinate in the treatment of sepsis syndrome and septic shock. The study also suggests that treatment of these conditions with methylprednisolone sodium succinate may increase the risk of mortality in certain patients (i.e., patients with elevated serum creatinine levels or patients who develop secondary infections after methylprednisolone sodium succinate).
Monitor for the development of infection and consider SOLU-MEDROL withdrawal or dosage reduction as needed.
If SOLU-MEDROL is used to treat a condition in patients with latent tuberculosis or tuberculin reactivity, reactivation of the disease may occur. Closely monitor such patients for reactivation. During prolonged SOLU-MEDROL therapy, patients with latent tuberculosis or tuberculin reactivity should receive chemoprophylaxis.
Varicella and measles can have a serious or even fatal course in non-immune patients taking corticosteroids, including SOLU-MEDROL. In corticosteroid-treated patients who have not had these diseases or are non-immune, particular care should be taken to avoid exposure to varicella and measles:
• If a SOLU‑MEDROL‑treated patient is exposed to varicella, prophylaxis with varicella zoster immune globulin (VZIG) may be indicated. If varicella develops, treatment with antiviral agents may be considered.• If a SOLU‑MEDROL‑treated patient is exposed to measles, prophylaxis with immunoglobulin (IG) may be indicated.
Hepatitis B virus reactivation can occur in patients who are hepatitis B carriers treated with immunosuppressive dosages of corticosteroids, including SOLU-MEDROL. Reactivation can also occur infrequently in corticosteroid-treated patients who appear to have resolved hepatitis B infection.
Screen patients for hepatitis B infection before initiating immunosuppressive (e.g., prolonged) treatment with SOLU-MEDROL. For patients who show evidence of hepatitis B infection, recommend consultation with physicians with expertise in managing hepatitis B regarding monitoring and consideration for hepatitis B antiviral therapy.
Corticosteroids, including SOLU-MEDROL, may exacerbate systemic fungal infections; therefore, avoid SOLU-MEDROL use in the presence of such infections unless SOLU‑MEDROL is needed to control drug reactions. For patients on chronic SOLU‑MEDROL therapy who develop systemic fungal infections, SOLU-MEDROL withdrawal or dosage reduction is recommended.
Corticosteroids, including SOLU-MEDROL, may activate latent amebiasis. Therefore, it is recommended that latent amebiasis or active amebiasis be ruled out before initiating SOLU-MEDROL in patients who have spent time in the tropics or patients with unexplained diarrhea.
Corticosteroids, including SOLU-MEDROL, should be used with great care in patients with known or suspected Strongyloides (threadworm) infestation. In such patients, corticosteroid-induced immunosuppression may lead to Strongyloides hyperinfection and dissemination with widespread larval migration, often accompanied by severe enterocolitis and potentially fatal gram-negative septicemia.
Avoid corticosteroids, including SOLU-MEDROL, in patients with cerebral malaria.
Rarely, high doses of cyclically pulsed intravenous methylprednisolone (usually for the treatment of exacerbations of multiple sclerosis at doses of 1 gram/day) can induce a toxic form of acute hepatitis. The time to onset of this form of steroid-induced liver injury can be several weeks or longer. Resolution has been observed after discontinuation of treatment. However, serious liver injury can occur, sometimes resulting in acute liver failure and death. Discontinue intravenous methylprednisolone if toxic hepatitis occurs. Since recurrence has occurred after re-challenge, avoid use of high dose intravenous methylprednisolone in patients with a history of toxic hepatitis caused by methylprednisolone.
Reports of severe medical events have been associated with the intrathecal route of administration (see
Use of corticosteroids may produce posterior subcapsular cataracts, glaucoma with possible damage to the optic nerves, and may enhance the establishment of secondary ocular infections due to bacteria, fungi, or viruses. The use of oral corticosteroids is not recommended in the treatment of optic neuritis and may lead to an increase in the risk of new episodes. Corticosteroids should be used cautiously in patients with ocular herpes simplex because of corneal perforation. Corticosteroids should not be used in active ocular herpes simplex.
Kaposi’s sarcoma has been reported to occur in patients receiving corticosteroid therapy, most often for chronic conditions. Discontinuation of corticosteroids may result in clinical improvement of Kaposi’s sarcoma.
Rarely, high doses of cyclically pulsed intravenous methylprednisolone (usually for the treatment of exacerbations of multiple sclerosis at doses of 1 gram/day) can induce a toxic form of acute hepatitis. The time to onset of this form of steroid-induced liver injury can be several weeks or longer. Resolution has been observed after discontinuation of treatment. However, serious liver injury can occur, sometimes resulting in acute liver failure and death. Discontinue intravenous methylprednisolone if toxic hepatitis occurs. Since recurrence has occurred after re-challenge, avoid use of high dose intravenous methylprednisolone in patients with a history of toxic hepatitis caused by methylprednisolone.
Reports of severe medical events have been associated with the intrathecal route of administration (see
Serious neurologic events, some resulting in death, have been reported with epidural injection of corticosteroids. Specific events reported include, but are not limited to, spinal cord infarction, paraplegia, quadriplegia, cortical blindness, and stroke. These serious neurologic events have been reported with and without use of fluoroscopy. The safety and effectiveness of epidural administration of corticosteroids have not been established, and corticosteroids are not approved for this use.
Injection of SOLU-MEDROL may result in dermal and/or subdermal changes forming depressions in the skin at the injection site. In order to minimize the incidence of dermal and subdermal atrophy, care must be exercised not to exceed recommended doses in injections. Injection into the deltoid muscle should be avoided because of a high incidence of subcutaneous atrophy.
Rare instances of anaphylactoid reactions have occurred in patients receiving corticosteroid therapy (see
In patients receiving the 40 mg presentation of SOLU-MEDROL during the treatment for acute allergic conditions and where these symptoms worsen or any new allergic symptoms occur, consideration should be given to the potential for hypersensitivity reactions to cow's milk ingredients (see
Increased dosage of rapidly acting corticosteroids is indicated in patients on corticosteroid therapy who are subjected to any unusual stress before, during, and after the stressful situation.
Results from one multicenter, randomized, placebo-controlled study with methylprednisolone hemisuccinate, an intravenous corticosteroid, showed an increase in early (at 2 weeks) and late (at 6 months) mortality in patients with cranial trauma who were determined not to have other clear indications for corticosteroid treatment. High doses of systemic corticosteroids, including SOLU-MEDROL, should not be used for the treatment of traumatic brain injury.
Average and large doses of corticosteroids can cause elevation of blood pressure, salt and water retention, and increased excretion of potassium. These effects are less likely to occur with the synthetic derivatives except when used in large doses. Dietary salt restriction and potassium supplementation may be necessary. All corticosteroids increase calcium excretion.
Literature reports suggest an apparent association between the use of corticosteroids and left ventricular free wall rupture after a recent myocardial infarction; therefore, therapy with corticosteroids should be used with great caution in these patients.
There have been cases reported in which concomitant use of amphotericin B and hydrocortisone was followed by cardiac enlargement and congestive heart failure (see
Hypothalamic-pituitary adrenal (HPA) axis suppression, Cushing's syndrome, and hyperglycemia. Monitor patients for these conditions with chronic use.
Corticosteroids can produce reversible HPA axis suppression with the potential for glucocorticosteroid insufficiency after withdrawal of treatment. Drug induced secondary adrenocortical insufficiency may be minimized by gradual reduction of dosage. This type of relative insufficiency may persist for months after discontinuation of therapy; therefore, in any situation of stress occurring during that period, hormone therapy should be reinstituted.
Corticosteroids, including SOLU-MEDROL, suppress the immune system and increase the risk of infection with any pathogen, including viral, bacterial, fungal, protozoan, or helminthic pathogens. Corticosteroids can:
• Reduce resistance to new infections• Exacerbate existing infections• Increase the risk of disseminated infections• Increase the risk of reactivation or exacerbation of latent infections• Mask some signs of infection
Corticosteroid‑associated infections can be mild but can be severe and at times fatal. The rate of infectious complications increases with increasing corticosteroid dosages.
A study has failed to establish the efficacy of methylprednisolone sodium succinate in the treatment of sepsis syndrome and septic shock. The study also suggests that treatment of these conditions with methylprednisolone sodium succinate may increase the risk of mortality in certain patients (i.e., patients with elevated serum creatinine levels or patients who develop secondary infections after methylprednisolone sodium succinate).
Monitor for the development of infection and consider SOLU-MEDROL withdrawal or dosage reduction as needed.
If SOLU-MEDROL is used to treat a condition in patients with latent tuberculosis or tuberculin reactivity, reactivation of the disease may occur. Closely monitor such patients for reactivation. During prolonged SOLU-MEDROL therapy, patients with latent tuberculosis or tuberculin reactivity should receive chemoprophylaxis.
Varicella and measles can have a serious or even fatal course in non-immune patients taking corticosteroids, including SOLU-MEDROL. In corticosteroid-treated patients who have not had these diseases or are non-immune, particular care should be taken to avoid exposure to varicella and measles:
• If a SOLU‑MEDROL‑treated patient is exposed to varicella, prophylaxis with varicella zoster immune globulin (VZIG) may be indicated. If varicella develops, treatment with antiviral agents may be considered.• If a SOLU‑MEDROL‑treated patient is exposed to measles, prophylaxis with immunoglobulin (IG) may be indicated.
Hepatitis B virus reactivation can occur in patients who are hepatitis B carriers treated with immunosuppressive dosages of corticosteroids, including SOLU-MEDROL. Reactivation can also occur infrequently in corticosteroid-treated patients who appear to have resolved hepatitis B infection.
Screen patients for hepatitis B infection before initiating immunosuppressive (e.g., prolonged) treatment with SOLU-MEDROL. For patients who show evidence of hepatitis B infection, recommend consultation with physicians with expertise in managing hepatitis B regarding monitoring and consideration for hepatitis B antiviral therapy.
Corticosteroids, including SOLU-MEDROL, may exacerbate systemic fungal infections; therefore, avoid SOLU-MEDROL use in the presence of such infections unless SOLU‑MEDROL is needed to control drug reactions. For patients on chronic SOLU‑MEDROL therapy who develop systemic fungal infections, SOLU-MEDROL withdrawal or dosage reduction is recommended.
Corticosteroids, including SOLU-MEDROL, may activate latent amebiasis. Therefore, it is recommended that latent amebiasis or active amebiasis be ruled out before initiating SOLU-MEDROL in patients who have spent time in the tropics or patients with unexplained diarrhea.
Corticosteroids, including SOLU-MEDROL, should be used with great care in patients with known or suspected Strongyloides (threadworm) infestation. In such patients, corticosteroid-induced immunosuppression may lead to Strongyloides hyperinfection and dissemination with widespread larval migration, often accompanied by severe enterocolitis and potentially fatal gram-negative septicemia.
Avoid corticosteroids, including SOLU-MEDROL, in patients with cerebral malaria.
Rarely, high doses of cyclically pulsed intravenous methylprednisolone (usually for the treatment of exacerbations of multiple sclerosis at doses of 1 gram/day) can induce a toxic form of acute hepatitis. The time to onset of this form of steroid-induced liver injury can be several weeks or longer. Resolution has been observed after discontinuation of treatment. However, serious liver injury can occur, sometimes resulting in acute liver failure and death. Discontinue intravenous methylprednisolone if toxic hepatitis occurs. Since recurrence has occurred after re-challenge, avoid use of high dose intravenous methylprednisolone in patients with a history of toxic hepatitis caused by methylprednisolone.
Reports of severe medical events have been associated with the intrathecal route of administration (see
Use of corticosteroids may produce posterior subcapsular cataracts, glaucoma with possible damage to the optic nerves, and may enhance the establishment of secondary ocular infections due to bacteria, fungi, or viruses. The use of oral corticosteroids is not recommended in the treatment of optic neuritis and may lead to an increase in the risk of new episodes. Corticosteroids should be used cautiously in patients with ocular herpes simplex because of corneal perforation. Corticosteroids should not be used in active ocular herpes simplex.
Kaposi’s sarcoma has been reported to occur in patients receiving corticosteroid therapy, most often for chronic conditions. Discontinuation of corticosteroids may result in clinical improvement of Kaposi’s sarcoma.
Corticosteroids, including SOLU-MEDROL, suppress the immune system and increase the risk of infection with any pathogen, including viral, bacterial, fungal, protozoan, or helminthic pathogens. Corticosteroids can:
• Reduce resistance to new infections• Exacerbate existing infections• Increase the risk of disseminated infections• Increase the risk of reactivation or exacerbation of latent infections• Mask some signs of infection
Corticosteroid‑associated infections can be mild but can be severe and at times fatal. The rate of infectious complications increases with increasing corticosteroid dosages.
A study has failed to establish the efficacy of methylprednisolone sodium succinate in the treatment of sepsis syndrome and septic shock. The study also suggests that treatment of these conditions with methylprednisolone sodium succinate may increase the risk of mortality in certain patients (i.e., patients with elevated serum creatinine levels or patients who develop secondary infections after methylprednisolone sodium succinate).
Monitor for the development of infection and consider SOLU-MEDROL withdrawal or dosage reduction as needed.
If SOLU-MEDROL is used to treat a condition in patients with latent tuberculosis or tuberculin reactivity, reactivation of the disease may occur. Closely monitor such patients for reactivation. During prolonged SOLU-MEDROL therapy, patients with latent tuberculosis or tuberculin reactivity should receive chemoprophylaxis.
Varicella and measles can have a serious or even fatal course in non-immune patients taking corticosteroids, including SOLU-MEDROL. In corticosteroid-treated patients who have not had these diseases or are non-immune, particular care should be taken to avoid exposure to varicella and measles:
• If a SOLU‑MEDROL‑treated patient is exposed to varicella, prophylaxis with varicella zoster immune globulin (VZIG) may be indicated. If varicella develops, treatment with antiviral agents may be considered.• If a SOLU‑MEDROL‑treated patient is exposed to measles, prophylaxis with immunoglobulin (IG) may be indicated.
Hepatitis B virus reactivation can occur in patients who are hepatitis B carriers treated with immunosuppressive dosages of corticosteroids, including SOLU-MEDROL. Reactivation can also occur infrequently in corticosteroid-treated patients who appear to have resolved hepatitis B infection.
Screen patients for hepatitis B infection before initiating immunosuppressive (e.g., prolonged) treatment with SOLU-MEDROL. For patients who show evidence of hepatitis B infection, recommend consultation with physicians with expertise in managing hepatitis B regarding monitoring and consideration for hepatitis B antiviral therapy.
Corticosteroids, including SOLU-MEDROL, may exacerbate systemic fungal infections; therefore, avoid SOLU-MEDROL use in the presence of such infections unless SOLU‑MEDROL is needed to control drug reactions. For patients on chronic SOLU‑MEDROL therapy who develop systemic fungal infections, SOLU-MEDROL withdrawal or dosage reduction is recommended.
Corticosteroids, including SOLU-MEDROL, may activate latent amebiasis. Therefore, it is recommended that latent amebiasis or active amebiasis be ruled out before initiating SOLU-MEDROL in patients who have spent time in the tropics or patients with unexplained diarrhea.
Corticosteroids, including SOLU-MEDROL, should be used with great care in patients with known or suspected Strongyloides (threadworm) infestation. In such patients, corticosteroid-induced immunosuppression may lead to Strongyloides hyperinfection and dissemination with widespread larval migration, often accompanied by severe enterocolitis and potentially fatal gram-negative septicemia.
Avoid corticosteroids, including SOLU-MEDROL, in patients with cerebral malaria.
SOLU-MEDROL Sterile Powder is an anti-inflammatory glucocorticoid, which contains methylprednisolone sodium succinate as the active ingredient. Methylprednisolone sodium succinate, USP, is the sodium succinate ester of methylprednisolone, and it occurs as a white, or nearly white, odorless hygroscopic, amorphous solid. It is very soluble in water and in alcohol; it is insoluble in chloroform and is very slightly soluble in acetone.
The chemical name for methylprednisolone sodium succinate is pregna-1,4-diene-3,20-dione,21-(3-carboxy-1-oxopropoxy)-11,17-dihydroxy-6-methyl-monosodium salt, (6α, 11β), and the molecular weight is 496.53. The structural formula is represented below:
Methylprednisolone sodium succinate is soluble in water; it may be administered in a small volume of diluent and is well suited for intravenous use in situations where high blood levels of methylprednisolone are required rapidly.
SOLU-MEDROL is available in preservative and preservative-free formulations:
Preservative-free Formulations |
40 mg Act-O-Vial System (Single-Dose Vial) —Each mL (when mixed) contains methylprednisolone sodium succinate equivalent to 40 mg methylprednisolone; also 1.6 mg monobasic sodium phosphate anhydrous; 17.46 mg dibasic sodium phosphate dried; and 25 mg lactose hydrous. |
125 mg Act-O-Vial System (Single-Dose Vial) —Each 2 mL (when mixed) contains methylprednisolone sodium succinate equivalent to 125 mg methylprednisolone; also 1.6 mg monobasic sodium phosphate anhydrous; and 17.4 mg dibasic sodium phosphate dried. |
Formulations preserved with Benzyl Alcohol |
1 gram Vial —Each 16 mL (when mixed as directed) contains methylprednisolone sodium succinate equivalent to 1 gram methylprednisolone; also 12.8 mg monobasic sodium phosphate anhydrous; 139.2 mg dibasic sodium phosphate dried. |
This package does not contain diluent. Recommended diluent (Bacteriostatic water) contains benzyl alcohol as a preservative. |
IMPORTANT — Use only the accompanying diluent or Bacteriostatic Water For Injection with Benzyl Alcohol when reconstituting SOLU-MEDROL. |
Use within 48 hours after mixing. |
When necessary, the pH of each formula was adjusted with sodium hydroxide so that the pH of the reconstituted solution is within the USP specified range of 7 to 8.