Sotalol Hydrochloride Prescribing Information
This summary contains important patient information that has been reviewed and approved by the U.S. Food and Drug Administration. This summary is not meant to take the place of your doctor's instructions. Read this patient information carefully before you start taking Sotalol AF. Each time you get a refill, you will receive patient information. Be sure to read it because it may contain new information that you need to know.
Sotalol AF are indicated for the maintenance of normal sinus rhythm [delay in time to recurrence of atrial fibrillation/atrial flutter (AFIB/AFL)] in patients with symptomatic AFIB/AFL who are currently in sinus rhythm. Because Sotalol AF can cause life-threatening ventricular arrhythmias, it should be reserved for patients in whom AFIB/AFL is highly symptomatic. Patients with paroxysmal AFIB whose AFIB/AFL that is easily reversed (by Valsalva maneuver, for example) should usually not be given Sotalol AF (see
In eight controlled trials of patients with AFIB/AFL and other supraventricular arrhythmias (N=659) there were four cases of Torsade de Pointes reported (0.6%) during the controlled phase of treatment with Sotalol AF. The incidence of Torsade de Pointes was significantly lower in those patients receiving total daily doses of 320 mg or less (0.3%), as summarized in Table 5 below. Both patients who had Torsade de Pointes in the group receiving >320 mg/day were receiving 640 mg/day. In the group receiving ≤320 mg daily, one case of TdP occurred at a daily dose of 320 mg on day 4 of treatment and one case occurred on a daily dose of 160 mg on day 1 of treatment.
| Sotalol AF (Daily Dose) | |||||
Any Dose (N=659) | >320 mg/day (N=62) | ≤320 mg/day (N=597) | ≤240 mg/day (N=340) | Placebo (N=358) | |
| n(%) | n(%) | n(%) | n(%) | n(%) | |
| Torsade de Pointes | 4(0.6%) | 2(3.2%) | 2(0.3%) | 1(0.3%) | 0 |
Prolongation of the QT interval is dose related, increasing from baseline an average of 25, 40, and 50 msec in the 80, 120, and 160 mg groups, respectively, in the clinical dose-response study. In this clinical trial Sotalol AF treatment was not initiated if the QT interval was greater than 450 msec and during therapy the dose was reduced or discontinued if the QT interval was ≥520 msec.
Experience in patients with ventricular arrhythmias is also pertinent to the risk of Torsade de Pointes in patients with AFIB/AFL (see below).
In patients with a history of sustained ventricular tachycardia, the incidence of Torsade de Pointes during sotalol treatment was 4% and worsened VT in about 1%; in patients with other less serious ventricular arrhythmias the incidence of Torsade de Pointes was 1% and new or worsened VT in about 0.7%. Additionally, in approximately 1% of patients, deaths were considered possibly drug related; such cases, although difficult to evaluate, may have been associated with proarrhythmic events.
Torsade de Pointes arrhythmias in patients with VT/VF were dose related, as was the prolongation of QT (QTc) interval, as shown in Table 6 below.
| Daily Dose (mg) | Incidence of Torsade de Pointes | Mean QTchighest on-therapy value(msec) |
| 80 | 0 (69)( ) Number of patients assessed | 463 (17) |
| 160 | 0.5 (832) | 467 (181) |
| 320 | 1.6 (835) | 473 (344) |
| 480 | 4.4 (459) | 483 (234) |
| 640 | 3.7 (324) | 490 (185) |
| >640 | 5.8 (103) | 512 (62) |
Table 7 below relates the incidence of Torsade de Pointes to on-therapy QTcand change in QTcfrom baseline. It should be noted, however, that the highest on therapy QTcwas in many cases the one obtained at the time of the Torsade de Pointes event, so that the table overstates the predictive value of a high QTc.
On-Therapy QTcInterval (msec) | Incidence of Torsade de Pointes | Change in QTc Interval From Baseline (msec) | Incidence of Torsade de Pointes |
| less than 500 | 1.3% (1787)( ) Number of patients assessed | less than 65 | 1.6% (1516) |
| 500 to 525 | 3.4% (236) | 65 to 80 | 3.2% (158) |
| 525 to 550 | 5.6% (125) | 80 to 100 | 4.1% (146) |
| >550 | 10.8% (157) | 100 to 30 | 5.2% (115) |
| >130 | 7.1% (99) |
In addition to dose and presence of sustained VT, other risk factors for Torsade de Pointes were gender (females had a higher incidence), excessive prolongation of the QTcinterval and history of cardiomegaly or congestive heart failure. Patients with sustained ventricular tachycardia and a history of congestive heart failure appear to have the highest risk for serious proarrhythmia (7%). Of the ventricular arrhythmia patients experiencing Torsade de Pointes, approximately two-thirds spontaneously reverted to their baseline rhythm. The others were either converted electrically (D/C cardioversion or overdrive pacing) or treated with other drugs (see OVERDOSAGE). It is not possible to determine whether some sudden deaths represented episodes of Torsade de Pointes, but in some instances sudden death did follow a documented episode of Torsade de Pointes. Although sotalol therapy was discontinued in most patients experiencing Torsade de Pointes, 17% were continued on a lower dose.
The use of Sotalol AF in conjunction with other drugs that prolong the QT interval has not been studied and is not recommended. Such drugs include many antiarrhythmics, some phenothiazines, bepridil, tricyclic antidepressants, and certain oral macrolides. Class I or Class III antiarrhythmic agents should be withheld for at least three half-lives prior to dosing with Sotalol AF. In clinical trials, Sotalol AF was not administered to patients previously treated with oral amiodarone for >1 month in the previous three months. Class Ia antiarrhythmic drugs, such as disopyramide, quinidine and procainamide and other Class III drugs (e.g., amiodarone) are not recommended as concomitant therapy with Sotalol AF because of their potential to prolong refractoriness (see WARNINGS). There is only limited experience with the concomitant use of Class Ib or Ic antiarrhythmics.
Sympathetic stimulation is necessary in supporting circulatory function in congestive heart failure, and beta-blockade carries the potential hazard of further depressing myocardial contractility and precipitating more severe failure. In patients who have heart failure controlled by digitalis and/or diuretics, Sotalol AF should be administered cautiously. Both digitalis and sotalol slow AV conduction. As with all beta-blockers, caution is advised when initiating therapy in patients with any evidence of left ventricular dysfunction. In a pooled data base of four placebo-controlled AFIB/AFL and PSVT studies, new or worsening CHF occurred during therapy with Sotalol AF in 5 (1.2%) of 415 patients. In these studies patients with uncontrolled heart failure were excluded (i.e., NYHA Functional Classes III or IV). In other premarketing sotalol studies, new or worsened congestive heart failure (CHF) occurred in 3.3% (n=3257) of patients and led to discontinuation in approximately 1% of patients receiving sotalol. The incidence was higher in patients presenting with sustained ventricular tachycardia/fibrillation (4.6%, n=1363), or a prior history of heart failure (7.3%, n=696). Based on a life-table analysis, the one-year incidence of new or worsened CHF was 3% in patients without a prior history and 10% in patients with a prior history of CHF. NYHA Classification was also closely associated to the incidence of new or worsened heart failure while receiving sotalol (1.8% in 1395 Class I patients, 4.9% in 1254 Class II patients and 6.1% in 278 Class III or IV patients).
Sotalol AF should not be used in patients with hypokalemia or hypomagnesemia prior to correction of imbalance, as these conditions can exaggerate the degree of QT prolongation, and increase the potential for Torsade de Pointes. Special attention should be given to electrolyte and acid-base balance in patients experiencing severe or prolonged diarrhea or patients receiving concomitant diuretic drugs.
The incidence of bradycardia (as determined by the investigators) in the supraventricular arrhythmia population treated with Sotalol AF (N = 415) was 13%, and led to discontinuation in 2.4% of patients. Bradycardia itself increases the risk of Torsade de Pointes.
Sotalol has been used in a controlled trial following an acute myocardial infarction without evidence of increased mortality (see
Hypersensitivity to catecholamines has been observed in patients withdrawn from beta-blocker therapy. Occasional cases of exacerbation of angina pectoris, arrhythmias and, in some cases, myocardial infarction have been reported after abrupt discontinuation of beta-blocker therapy. Therefore, it is prudent when discontinuing chronically administered Sotalol AF, particularly in patients with ischemic heart disease, to carefully monitor the patient and consider the temporary use of an alternate beta-blocker if appropriate. If possible, the dosage of Sotalol AF should be gradually reduced over a period of one to two weeks. If angina or acute coronary insufficiency develops, appropriate therapy should be instituted promptly. Patients should be warned against interruption or discontinuation of therapy without the physician's advice. Because coronary artery disease is common and may be unrecognized in patients receiving Sotalol AF, abrupt discontinuation in patients with arrhythmias may unmask latent coronary insufficiency.
While taking beta-blockers, patients with a history of anaphylactic reaction to a variety of allergens may have a more severe reaction on repeated challenge, either accidental, diagnostic or therapeutic. Such patients may be unresponsive to the usual doses of epinephrine used to treat the allergic reaction.
Chronically administered beta-blocking therapy should not be routinely withdrawn prior to major surgery, however the impaired ability of the heart to respond to reflex adrenergic stimuli may augment the risks of general anesthesia and surgical procedures.
In patients with diabetes (especially labile diabetes) or with a history of episodes of spontaneous hypoglycemia, Sotalol AF should be given with caution since beta-blockade may mask some important premonitory signs of acute hypoglycemia; e.g., tachycardia.
Sotalol AF should be used only with extreme caution in patients with sick sinus syndrome associated with symptomatic arrhythmias, because it may cause sinus bradycardia, sinus pauses or sinus arrest. In patients with AFIB and sinus node dysfunction, the risk of Torsade de Pointes with Sotalol AF therapy is increased, especially after cardioversion. Bradycardia following cardioversion in these patients is associated with QTcinterval prolongation which is augmented due to the reverse use dependence of the Class III effects of Sotalol AF. Patients with AFIB/AFL associated with the sick sinus syndrome may be treated with Sotalol AF if they have an implanted pacemaker for control of bradycardia symptoms.
Beta-blockade may mask certain clinical signs (e.g., tachycardia) of hyperthyroidism. Patients suspected of developing thyrotoxicosis should be managed carefully to avoid abrupt withdrawal of beta-blockade which might be followed by an exacerbation of symptoms of hyperthyroidism, including thyroid storm. The beta-blocking effects of Sotalol AF may be useful in controlling heart rate in AFIB associated with thyrotoxicosis but no study has been conducted to evaluate this.
In general, antiarrhythmic therapy for AFIB/AFL aims to prolong the time in normal sinus rhythm. Recurrence is expected in some patients (see
Prolongation of Time to Recurrence of Symptomatic Atrial Fibrillation/ Flutter
Sotalol AF has been studied in patients with symptomatic AFIB/AFL in two principal studies, one in patients with primarily paroxysmal AFIB/AFL, the other in patients with primarily chronic AFIB.
In one study, a U.S. multicenter, randomized, placebo-controlled, double-blind, dose-response trial of patients with symptomatic primarily paroxysmal AFIB/AFL, three fixed dose levels of Sotalol AF (80 mg, 120 mg and 160 mg) twice daily and placebo were compared in 253 patients. In patients with reduced creatinine clearance (40 to 60 mL/min) the same doses were given once daily. Patients were not randomized for the following reasons: QT >450 msec; creatinine clearance <40 mL/min; intolerance to beta-blockers; bradycardia-tachycardia syndrome in the absence of an implanted pacemaker; AFIB/AFL was asymptomatic or was associated with syncope, embolic CVA or TIA; acute myocardial infarction within the previous 2 months; congestive heart failure; bronchial asthma or other contraindications to beta-blocker therapy; receiving potassium losing diuretics without potassium replacement or without concurrent use of ACE-inhibitors; uncorrected hypokalemia (serum potassium <3.5 meq/L) or hypomagnesemia (serum magnesium <1.5 meq/L); received chronic oral amiodarone therapy for >1 month within previous 12 weeks; congenital or acquired long QT syndromes; history of Torsade de Pointes with other antiarrhythmic agents which increase the duration of ventricular repolarization; sinus rate <50 bpm during waking hours; unstable angina pectoris; receiving treatment with other drugs that prolong the QT interval; and AFIB/AFL associated with the Wolff-Parkinson-White (WPW) syndrome. If the QT interval increased to ≥520 msec (or JT ≥430 msec if QRS >100 msec) the drug was discontinued. The patient population in this trial was 64% male, and the mean age was 62 years. No structural heart disease was present in 43% of the patients. Doses were administered once daily in 20% of the patients because of reduced creatinine clearance.
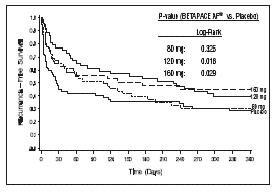
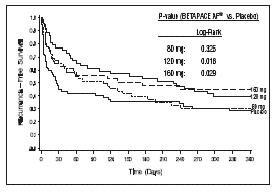
Sotalol AF was shown to prolong the time to the first symptomatic, ECG-documented recurrence of AFIB/AFL, as well as to reduce the risk of such recurrence at both 6 and 12 months. The 120 mg dose was more effective than 80 mg, but 160 mg did not appear to have an added benefit. Note that these doses were given twice or once daily, depending on renal function. The results are shown in Figure 1 and Tables 1 and 2.
| Placebo | Sotalol AF Dose | |||
| 80 mg | 120 mg | 160 mg | ||
| Randomized | 69 | 59 | 63 | 62 |
On treatment in NSR at 12 months without recurrenceSymptomatic AFIB/AFL | 23% | 22% | 29% | 23% |
| RecurrenceEfficacy endpoint of Study 1; study treatment stopped. | 67% | 58% | 49% | 42% |
| D/C for AEs | 6% | 12% | 18% | 29% |
Please note that columns do not add up to 100% due to discontinuations (D/C) for "other" reasons.
| Discontinuation because of adverse events was dose related. | ||||
| Placebo | Sotalol AF Dose | |||
| 80 mg | 120 mg | 160 mg | ||
| p-value vs placebo | p=0.325 | p=0.018 | p=0.029 | |
Relative Risk (RR) to placebo | 0.81 | 0.59 | 0.59 | |
Median time to recurrence (days) | 27 | 106 | 229 | 175 |
In a second multicenter, randomized, placebo-controlled, double-blind study of 6 months duration in 232 patients with chronic AFIB, Sotalol AF was titrated over a dose range from 80 mg/day to 320 mg/day. The patient population of this trial was 70% male with a mean age of 65 years. Structural heart disease was present in 49% of the patients. All patients had chronic AFIB for >2 weeks but <1 year at entry with a mean duration of 4.1 months. Patients were excluded if they had significant electrolyte imbalance, QTc>460 msec, QRS >140 msec, any degree of AV block or functioning pacemaker, uncompensated cardiac failure, asthma, significant renal disease (estimated creatinine clearance <50 mL/min), heart rate <50 bpm, myocardial infarction or open heart surgery in past 2 months, unstable angina, infective endocarditis, active pericarditis or myocarditis, ≥ 3 DC cardioversions in the past, medications that prolonged QT interval, and previous amiodarone treatment. After successful cardioversion patients were randomized to receive placebo (n=114) or Sotalol AF (n=118), at a starting dose of 80 mg twice daily. If the initial dose was not tolerated it was decreased to 80 mg once daily, but if it was tolerated it was increased to 160 mg twice daily. During the maintenance period 67% of treated patients received a dose of 160 mg twice daily, and the remainder received doses of 80 mg once daily (17%) and 80 mg twice daily (16%).
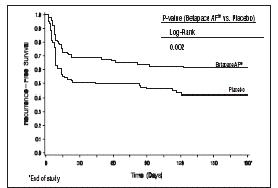
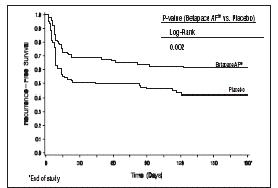
Figure 2 and Tables 3 and 4 show the results of the trial. There was a longer time to ECG-documented recurrence of AFIB and a reduced risk of recurrence at 6 months compared to placebo.
| Sotalol AF | Placebo | |
| Randomized | 118 | 114 |
| On treatment in NSR at 6 months without recurrenceSymptomatic or asymptomatic AFIB/AFL | 45% | 29% |
| RecurrenceEfficacy endpoint of Study 2; study treatment stopped. | 49% | 67% |
| D/C for AEs | 6% | 3% |
| Death | 1% |
| Sotalol AF | Placebo | |
| p-value vs placebo | p=0.002 | |
| Relative Risk (RR) to placebo | 0.55 | |
| Median time to recurrence (days) | >180 | 44 |
Safety in Patients with Structural Heart Disease
In a multicenter double-blind randomized study reported by D. Julian et al, the effect of sotalol 320 mg once daily was compared with that of placebo in 1456 patients (randomized 3:2, sotalol to placebo) surviving an acute myocardial infarction (MI). Treatment was started 5 to 14 days after infarction. Patients were followed for 12 months. The mortality rate was 7.3% in the sotalol group and 8.9% in the placebo group, not a statistically significant difference. Although the results do not show evidence of a benefit of sotalol in this population, they do not show an added risk in post MI patients receiving sotalol.
In healthy subjects, the oral bioavailability of sotalol is 90 to 100%. After oral administration, peak plasma concentrations are reached in 2.5 to 4 hours, and steady-state plasma concentrations are attained within 2 to 3 days (i.e., after 5 to 6 doses when administered twice daily). Over the dosage range 160 to 640 mg/day sotalol displays dose proportionality with respect to plasma concentrations. Distribution occurs to a central (plasma) and to a peripheral compartment, with a mean elimination half-life of 12 hours. Dosing every 12 hours results in trough plasma concentrations which are approximately one-half of those at peak.
Sotalol does not bind to plasma proteins and is not metabolized. Sotalol shows very little intersubject variability in plasma levels. The pharmacokinetics of the d and l enantiomers of sotalol are essentially identical. Sotalol crosses the blood brain barrier poorly. Excretion is predominantly via the kidney in the unchanged form, and therefore lower doses are necessary in conditions of renal impairment (see DOSAGE AND ADMINISTRATION). Age per se does not significantly alter the pharmacokinetics of sotalol, but impaired renal function in geriatric patients can increase the terminal elimination half-life, resulting in increased drug accumulation. The absorption of sotalol was reduced by approximately 20% compared to fasting when it was administered with a standard meal. Since sotalol is not subject to first-pass metabolism, patients with hepatic impairment show no alteration in clearance of sotalol.
The combined analysis of two unblinded, multicenter trials (a single dose and a multiple dose study) with 59 children, aged between 3 days and 12 years, showed the pharmacokinetics of sotalol to be first order. A daily dose of 30 mg/m2of sotalol was administered in the single dose study and daily doses of 30, 90 and 210 mg/m2were administered q8h in the multi-dose study. After rapid absorption with peak levels occurring on average between 2 to 3 hours following administration, sotalol was eliminated with a mean half-life of 9.5 hours. Steady-state was reached after 1 to 2 days. The average peak to trough concentration ratio was 2. BSA was the most important covariate and more relevant than age for the pharmacokinetics of sotalol. The smallest children (BSA <0.33m2) exhibited a greater drug exposure (+59%) than the larger children who showed a uniform drug concentration profile. The intersubject variation for oral clearance was 22%.
Sotalol is also indicated for the treatment of documented life-threatening ventricular arrhythmias and is marketed under the brand name
- Therapy with Sotalol AF must be initiated (and, if necessary, titrated) in a setting that provides continuous electrocardiographic (ECG) monitoring and in the presence of personnel trained in the management of serious ventricular arrhythmias. Patients should continue to be monitored in this way for a minimum of 3 days on the maintenance dose. In addition, patients should not be discharged within 12 hours of electrical or pharmacological conversion to normal sinus rhythm.
- The QT interval is used to determine patient eligibility for Sotalol AF treatment and for monitoring safety during treatment. The baseline QT interval must be ≤450 msec in order for a patient to be started on Sotalol AF therapy. During initiation and titration, the QT interval should be monitored 2 to 4 hours after each dose. If the QT interval prolongs to 500 msec or greater, the dose must be reduced or the drug discontinued.
- The dose of Sotalol AF must be individualized according to calculated creatinine clearance.In patients with a creatinine clearance >60 mL/min Sotalol AF is administered twice daily (BID) while in those with a creatinine clearance between 40 and 60 mL/min, the dose is administered once daily (QD). In patients with a creatinine clearance less than 40 mL/min Sotalol AF is contraindicated. The recommended initial dose of Sotalol AF is 80 mg and is initiated as shown in the dosing algorithm described below. The 80 mg dose can be titrated upward to 120 mg during initial hospitalization or after discharge on 80 mg in the event of recurrence, by rehospitalization and repeating the same steps used during the initiation of therapy (see).
Upward Titration of DoseIf the 80 mg dose level (given BID or QD depending upon the creatinine clearance) does not reduce the frequency of relapses of AFIB/AFL and is tolerated without excessive QT interval prolongation (i.e., ≥520 msec), the dose level may be increased to 120 mg (BID or QD depending upon the creatinine clearance). As proarrhythmic events can occur not only at initiation of therapy, but also with each upward dosage adjustment, Steps 2 through 5 used during initiation of Sotalol AF therapy should be followed when increasing the dose level. In the U.S. multicenter dose-response study, the 120 mg dose (BID or QD) was found to be the most effective in prolonging the time to ECG documented symptomatic recurrence of AFIB/AFL. If the 120 mg dose does not reduce the frequency of early relapse of AFIB/AFL and is tolerated without excessive QT interval prolongation (≥520 msec), an increase to 160 mg (BID or QD depending upon the creatinine clearance), can be considered. Steps 2 through 5 used during the initiation of therapy should be used again to introduce such an increase.
- Patients with atrial fibrillation should be anticoagulated according to usual medical practice. Hypokalemia should be corrected before initiation of Sotalol AF therapy (see ).,
WARNINGSVentricular ArrhythmiaSotalol AF can cause serious ventricular arrhythmias, primarily Torsade de Pointes (TdP) type ventricular tachycardia, a polymorphic ventricular tachycardia associated with QT interval prolongation. QT interval prolongation is directly related to the dose of Sotalol AF. Factors such as reduced creatinine clearance, gender (female) and larger doses increase the risk of TdP. The risk of TdP can be reduced by adjustment of the Sotalol AF dose according to creatinine clearance and by monitoring the ECG for excessive increases in the QT interval.Treatment with Sotalol AF must therefore be started only in patients observed for a minimum of three days on their maintenance dose in a facility that can provide electrocardiographic monitoring and in the presence of personnel trained in the management of serious ventricular arrhythmias. Calculation of the creatinine clearance must precede administration of the first dose of Sotalol AF. For detailed instructions regarding dose selection, see DOSAGE AND ADMINISTRATION.Proarrhythmia in Atrial Fibrillation/Atrial Flutter PatientsIn eight controlled trials of patients with AFIB/AFL and other supraventricular arrhythmias (N=659) there were four cases of Torsade de Pointes reported (0.6%) during the controlled phase of treatment with Sotalol AF. The incidence of Torsade de Pointes was significantly lower in those patients receiving total daily doses of 320 mg or less (0.3%), as summarized in Table 5 below. Both patients who had Torsade de Pointes in the group receiving >320 mg/day were receiving 640 mg/day. In the group receiving ≤320 mg daily, one case of TdP occurred at a daily dose of 320 mg on day 4 of treatment and one case occurred on a daily dose of 160 mg on day 1 of treatment.
Table 5 Incidence of Torsade de Pointes in Controlled Trials of AFIB and Other Supraventricular Arrhythmias Sotalol AF (Daily Dose) Any
Dose
(N=659)>320
mg/day
(N=62)≤320
mg/day
(N=597)≤240
mg/day
(N=340)Placebo
(N=358)n(%) n(%) n(%) n(%) n(%) Torsade de Pointes 4(0.6%) 2(3.2%) 2(0.3%) 1(0.3%) 0 Prolongation of the QT interval is dose related, increasing from baseline an average of 25, 40, and 50 msec in the 80, 120, and 160 mg groups, respectively, in the clinical dose-response study. In this clinical trial Sotalol AF treatment was not initiated if the QT interval was greater than 450 msec and during therapy the dose was reduced or discontinued if the QT interval was ≥520 msec.
Experience in patients with ventricular arrhythmias is also pertinent to the risk of Torsade de Pointes in patients with AFIB/AFL (see below).
Proarrhythmia in Ventricular Arrhythmia Patients: [see Sotalol (sotalol hydrochloride) Package Insert]In patients with a history of sustained ventricular tachycardia, the incidence of Torsade de Pointes during sotalol treatment was 4% and worsened VT in about 1%; in patients with other less serious ventricular arrhythmias the incidence of Torsade de Pointes was 1% and new or worsened VT in about 0.7%. Additionally, in approximately 1% of patients, deaths were considered possibly drug related; such cases, although difficult to evaluate, may have been associated with proarrhythmic events.
Torsade de Pointes arrhythmias in patients with VT/VF were dose related, as was the prolongation of QT (QTc) interval, as shown in Table 6 below.
Table 6 Percent Incidence of Torsade de Pointes and Mean QTcInterval by Dose For Patients With Sustained VT/VF Daily Dose (mg) Incidence of Torsade de Pointes Mean QTchighest on-therapy value(msec) 80 0 (69)( ) Number of patients assessed 463 (17) 160 0.5 (832) 467 (181) 320 1.6 (835) 473 (344) 480 4.4 (459) 483 (234) 640 3.7 (324) 490 (185) >640 5.8 (103) 512 (62) Table 7 below relates the incidence of Torsade de Pointes to on-therapy QTcand change in QTcfrom baseline. It should be noted, however, that the highest on therapy QTcwas in many cases the one obtained at the time of the Torsade de Pointes event, so that the table overstates the predictive value of a high QTc.
Table 7 Relationship Between QTcInterval Prolongation and Torsade de Pointes On-Therapy
QTcInterval
(msec)Incidence of
Torsade de
PointesChange in QTc
Interval From
Baseline (msec)Incidence of
Torsade de
Pointesless than 500 1.3% (1787)( ) Number of patients assessed less than 65 1.6% (1516) 500 to 525 3.4% (236) 65 to 80 3.2% (158) 525 to 550 5.6% (125) 80 to 100 4.1% (146) >550 10.8% (157) 100 to 30 5.2% (115) >130 7.1% (99) In addition to dose and presence of sustained VT, other risk factors for Torsade de Pointes were gender (females had a higher incidence), excessive prolongation of the QTcinterval and history of cardiomegaly or congestive heart failure. Patients with sustained ventricular tachycardia and a history of congestive heart failure appear to have the highest risk for serious proarrhythmia (7%). Of the ventricular arrhythmia patients experiencing Torsade de Pointes, approximately two-thirds spontaneously reverted to their baseline rhythm. The others were either converted electrically (D/C cardioversion or overdrive pacing) or treated with other drugs (see OVERDOSAGE). It is not possible to determine whether some sudden deaths represented episodes of Torsade de Pointes, but in some instances sudden death did follow a documented episode of Torsade de Pointes. Although sotalol therapy was discontinued in most patients experiencing Torsade de Pointes, 17% were continued on a lower dose.
Use with Drugs that Prolong QT Interval and Antiarrhythmic AgentsThe use of Sotalol AF in conjunction with other drugs that prolong the QT interval has not been studied and is not recommended. Such drugs include many antiarrhythmics, some phenothiazines, bepridil, tricyclic antidepressants, and certain oral macrolides. Class I or Class III antiarrhythmic agents should be withheld for at least three half-lives prior to dosing with Sotalol AF. In clinical trials, Sotalol AF was not administered to patients previously treated with oral amiodarone for >1 month in the previous three months. Class Ia antiarrhythmic drugs, such as disopyramide, quinidine and procainamide and other Class III drugs (e.g., amiodarone) are not recommended as concomitant therapy with Sotalol AF because of their potential to prolong refractoriness (see WARNINGS). There is only limited experience with the concomitant use of Class Ib or Ic antiarrhythmics.
Congestive Heart FailureSympathetic stimulation is necessary in supporting circulatory function in congestive heart failure, and beta-blockade carries the potential hazard of further depressing myocardial contractility and precipitating more severe failure. In patients who have heart failure controlled by digitalis and/or diuretics, Sotalol AF should be administered cautiously. Both digitalis and sotalol slow AV conduction. As with all beta-blockers, caution is advised when initiating therapy in patients with any evidence of left ventricular dysfunction. In a pooled data base of four placebo-controlled AFIB/AFL and PSVT studies, new or worsening CHF occurred during therapy with Sotalol AF in 5 (1.2%) of 415 patients. In these studies patients with uncontrolled heart failure were excluded (i.e., NYHA Functional Classes III or IV). In other premarketing sotalol studies, new or worsened congestive heart failure (CHF) occurred in 3.3% (n=3257) of patients and led to discontinuation in approximately 1% of patients receiving sotalol. The incidence was higher in patients presenting with sustained ventricular tachycardia/fibrillation (4.6%, n=1363), or a prior history of heart failure (7.3%, n=696). Based on a life-table analysis, the one-year incidence of new or worsened CHF was 3% in patients without a prior history and 10% in patients with a prior history of CHF. NYHA Classification was also closely associated to the incidence of new or worsened heart failure while receiving sotalol (1.8% in 1395 Class I patients, 4.9% in 1254 Class II patients and 6.1% in 278 Class III or IV patients).
Electrolyte DisturbancesSotalol AF should not be used in patients with hypokalemia or hypomagnesemia prior to correction of imbalance, as these conditions can exaggerate the degree of QT prolongation, and increase the potential for Torsade de Pointes. Special attention should be given to electrolyte and acid-base balance in patients experiencing severe or prolonged diarrhea or patients receiving concomitant diuretic drugs.
Bradycardia/Heart BlockThe incidence of bradycardia (as determined by the investigators) in the supraventricular arrhythmia population treated with Sotalol AF (N = 415) was 13%, and led to discontinuation in 2.4% of patients. Bradycardia itself increases the risk of Torsade de Pointes.
Recent Acute MISotalol has been used in a controlled trial following an acute myocardial infarction without evidence of increased mortality (see
Safety in Patients with Structural Heart Disease). Although specific studies of its use in treating atrial arrhythmias after infarction have not been conducted, the usual precautions regarding heart failure, avoidance of hypokalemia, bradycardia or prolonged QT interval apply.The following warnings are related to the beta-blocking activity of Sotalol AF.Abrupt WithdrawalHypersensitivity to catecholamines has been observed in patients withdrawn from beta-blocker therapy. Occasional cases of exacerbation of angina pectoris, arrhythmias and, in some cases, myocardial infarction have been reported after abrupt discontinuation of beta-blocker therapy. Therefore, it is prudent when discontinuing chronically administered Sotalol AF, particularly in patients with ischemic heart disease, to carefully monitor the patient and consider the temporary use of an alternate beta-blocker if appropriate. If possible, the dosage of Sotalol AF should be gradually reduced over a period of one to two weeks. If angina or acute coronary insufficiency develops, appropriate therapy should be instituted promptly. Patients should be warned against interruption or discontinuation of therapy without the physician's advice. Because coronary artery disease is common and may be unrecognized in patients receiving Sotalol AF, abrupt discontinuation in patients with arrhythmias may unmask latent coronary insufficiency.
Non-Allergic Bronchospasm (e.g., chronic bronchitis and emphysema)PATIENTS WITH BRONCHOSPASTIC DISEASES SHOULD IN GENERAL NOT RECEIVE BETA-BLOCKERS.It is prudent, if Sotalol AF (sotalol hydrochloride) is to be administered, to use the smallest effective dose, so that inhibition of bronchodilation produced by endogenous or exogenous catecholamine stimulation of beta2receptors may be minimized.AnaphylaxisWhile taking beta-blockers, patients with a history of anaphylactic reaction to a variety of allergens may have a more severe reaction on repeated challenge, either accidental, diagnostic or therapeutic. Such patients may be unresponsive to the usual doses of epinephrine used to treat the allergic reaction.
Major SurgeryChronically administered beta-blocking therapy should not be routinely withdrawn prior to major surgery, however the impaired ability of the heart to respond to reflex adrenergic stimuli may augment the risks of general anesthesia and surgical procedures.
DiabetesIn patients with diabetes (especially labile diabetes) or with a history of episodes of spontaneous hypoglycemia, Sotalol AF should be given with caution since beta-blockade may mask some important premonitory signs of acute hypoglycemia; e.g., tachycardia.
Sick Sinus SyndromeSotalol AF should be used only with extreme caution in patients with sick sinus syndrome associated with symptomatic arrhythmias, because it may cause sinus bradycardia, sinus pauses or sinus arrest. In patients with AFIB and sinus node dysfunction, the risk of Torsade de Pointes with Sotalol AF therapy is increased, especially after cardioversion. Bradycardia following cardioversion in these patients is associated with QTcinterval prolongation which is augmented due to the reverse use dependence of the Class III effects of Sotalol AF. Patients with AFIB/AFL associated with the sick sinus syndrome may be treated with Sotalol AF if they have an implanted pacemaker for control of bradycardia symptoms.
ThyrotoxicosisBeta-blockade may mask certain clinical signs (e.g., tachycardia) of hyperthyroidism. Patients suspected of developing thyrotoxicosis should be managed carefully to avoid abrupt withdrawal of beta-blockade which might be followed by an exacerbation of symptoms of hyperthyroidism, including thyroid storm. The beta-blocking effects of Sotalol AF may be useful in controlling heart rate in AFIB associated with thyrotoxicosis but no study has been conducted to evaluate this.
Proarrhythmia in Ventricular Arrhythmia Patients: [see Sotalol (sotalol hydrochloride) Package Insert]In patients with a history of sustained ventricular tachycardia, the incidence of Torsade de Pointes during sotalol treatment was 4% and worsened VT in about 1%; in patients with other less serious ventricular arrhythmias the incidence of Torsade de Pointes was 1% and new or worsened VT in about 0.7%. Additionally, in approximately 1% of patients, deaths were considered possibly drug related; such cases, although difficult to evaluate, may have been associated with proarrhythmic events.
Torsade de Pointes arrhythmias in patients with VT/VF were dose related, as was the prolongation of QT (QTc) interval, as shown in Table 6 below.
Table 6 Percent Incidence of Torsade de Pointes and Mean QTcInterval by Dose For Patients With Sustained VT/VF Daily Dose (mg) Incidence of Torsade de Pointes Mean QTchighest on-therapy value(msec) 80 0 (69)( ) Number of patients assessed 463 (17) 160 0.5 (832) 467 (181) 320 1.6 (835) 473 (344) 480 4.4 (459) 483 (234) 640 3.7 (324) 490 (185) >640 5.8 (103) 512 (62) Table 7 below relates the incidence of Torsade de Pointes to on-therapy QTcand change in QTcfrom baseline. It should be noted, however, that the highest on therapy QTcwas in many cases the one obtained at the time of the Torsade de Pointes event, so that the table overstates the predictive value of a high QTc.
Table 7 Relationship Between QTcInterval Prolongation and Torsade de Pointes On-Therapy
QTcInterval
(msec)Incidence of
Torsade de
PointesChange in QTc
Interval From
Baseline (msec)Incidence of
Torsade de
Pointesless than 500 1.3% (1787)( ) Number of patients assessed less than 65 1.6% (1516) 500 to 525 3.4% (236) 65 to 80 3.2% (158) 525 to 550 5.6% (125) 80 to 100 4.1% (146) >550 10.8% (157) 100 to 30 5.2% (115) >130 7.1% (99) In addition to dose and presence of sustained VT, other risk factors for Torsade de Pointes were gender (females had a higher incidence), excessive prolongation of the QTcinterval and history of cardiomegaly or congestive heart failure. Patients with sustained ventricular tachycardia and a history of congestive heart failure appear to have the highest risk for serious proarrhythmia (7%). Of the ventricular arrhythmia patients experiencing Torsade de Pointes, approximately two-thirds spontaneously reverted to their baseline rhythm. The others were either converted electrically (D/C cardioversion or overdrive pacing) or treated with other drugs (see OVERDOSAGE). It is not possible to determine whether some sudden deaths represented episodes of Torsade de Pointes, but in some instances sudden death did follow a documented episode of Torsade de Pointes. Although sotalol therapy was discontinued in most patients experiencing Torsade de Pointes, 17% were continued on a lower dose.
- Patients to be discharged on Sotalol AF therapy from an in-patient setting should have an adequate supply of Sotalol AF, to allow uninterrupted therapy until the patient can fill a Sotalol AF prescription.
Sotalol AF is contraindicated in patients with sinus bradycardia (<50 bpm during waking hours), sick sinus syndrome or second and third degree AV block (unless a functioning pacemaker is present), congenital or acquired long QT syndromes, baseline QT interval >450 msec, cardiogenic shock, uncontrolled heart failure, hypokalemia (<4 meq/L), creatinine clearance <40 mL/min, bronchial asthma and previous evidence of hypersensitivity to sotalol.
Adverse events that are clearly related to Sotalol AF are those which are typical of its Class II (beta-blocking) and Class III (cardiac action potential duration prolongation) effects. The common documented beta-blocking adverse events (bradycardia, dyspnea, and fatigue) and Class III effects (QT interval prolongation) are dose related.
In a pooled clinical trial population consisting of four placebo-controlled studies with 275 patients with AFIB/AFL treated with 160 to 320 mg doses of Sotalol AF, the following adverse events were reported at a rate of 2% or more in the 160 to 240 mg treated patients and greater than the rate in placebo patients (See Table 8). The data are presented by incidence of events in the Sotalol AF and placebo groups by body system and daily dose. No significant irreversible non-cardiac end-organ toxicity was observed.
Placebo | Sotalol AF Total Daily Dose | ||
Body System/ Adverse Event (Preferred Term) | N=282 | 160 to 240 N=153 | >240 to 320 N=122 |
CARDIOVASCULAR | |||
| Abnormality ECG | 0.4 | 3.3 | 2.5 |
| Angina Pectoris | 1.1 | 2.0 | 1.6 |
| Bradycardia | 2.5 | 13.1 | 12.3 |
| Chest Pain Cardiac/Non-Anginal | 4.6 | 4.6 | 2.5 |
| Disturbance Rhythm Atrial | 2.1 | 2.0 | 1.6 |
| Disturbance Rhythm Subjective | 9.9 | 9.8 | 7.4 |
GASTROINTESTINAL | |||
| Appetite Decreased | 0.4 | 2.0 | 1.6 |
| Diarrhea | 2.1 | 5.2 | 5.7 |
| Distention Abdomen | 0.4 | 0.7 | 2.5 |
| Dyspepsia/Heartburn | 1.8 | 2.0 | 2.5 |
| Nausea/Vomiting | 5.3 | 7.8 | 5.7 |
| Pain Abdomen | 2.5 | 3.9 | 2.5 |
GENERAL | |||
| Fatigue | 8.5 | 19.6 | 18.9 |
| Fever | 0.7 | 0.7 | 3.3 |
| Hyperhidrosis | 3.2 | 5.2 | 4.9 |
| Influenza | 0.4 | 2.0 | 0.8 |
| Sensation Cold | 0.7 | 2.0 | 2.5 |
| Weakness | 3.2 | 5.2 | 4.9 |
MUSCULOSKELETAL/CONNECTIVE TISSUE | |||
| Pain Chest Musculoskeletal | 1.4 | 2.0 | 2.5 |
| Pain Musculoskeletal | 2.8 | 2.6 | 4.1 |
NERVOUS SYSTEM | |||
| Dizziness | 12.4 | 16.3 | 13.1 |
| Headache | 5.3 | 3.3 | 11.5 |
| Insomnia | 1.1 | 2.6 | 4.1 |
RESPIRATORY | |||
| Cough | 2.5 | 3.3 | 2.5 |
| Dyspnea | 7.4 | 9.2 | 9.8 |
| Infection Upper Respiratory | 1.1 | 2.6 | 3.3 |
| Tracheobronchitis | 0.7 | 0.7 | 3.3 |
SPECIAL SENSES | |||
| Disturbance Vision | 0.7 | 2.6 | 0.8 |
Overall, discontinuation because of unacceptable adverse events was necessary in 17% of the patients, and occurred in 10% of patients less than two weeks after starting treatment. The most common adverse events leading to discontinuation of Sotalol AF were: fatigue 4.6%, bradycardia 2.4%, proarrhythmia 2.2%, dyspnea 2%, and QT interval prolongation 1.4%.
In clinical trials involving 1292 patients with sustained VT/VF, the common adverse events (occurring in ≥2% of patients) were similar to those described for the AFIB/AFL population.
Occasional reports of elevated serum liver enzymes have occurred with sotalol therapy but no cause and effect relationship has been established. One case of peripheral neuropathy which resolved on discontinuation of sotalol and recurred when the patient was rechallenged with the drug was reported in an early dose tolerance study. Elevated blood glucose levels and increased insulin requirements can occur in diabetic patients.
In an unblinded multicenter trial of 25 patients with SVT and/or VT receiving daily doses of 30, 90 and 210 mg/m2 with dosing every 8 hours for a total of 9 doses, no Torsades de Pointes or other serious new arrhythmias were observed. One (1) patient, receiving 30 mg/m2 daily, was discontinued because of increased frequency of sinus pauses/bradycardia. Additional cardiovascular AEs were seen at the 90 and 210 mg/m2 daily dose levels. They included QT prolongations (2 patients), sinus pauses/bradycardia (1 patient), increased severity of atrial flutter and reported chest pain (1 patient). Values for QTc ≥525 msec were seen in 2 patients at the 210 mg/m2 daily dose level. Serious adverse events including death, Torsades de Pointes, other proarrhythmias, high-degree A-V blocks and bradycardia have been reported in infants and/or children.
Sotalol is primarily eliminated by renal excretion; therefore, drugs that are metabolized by CYP450 are not expected to alter the pharmacokinetics of sotalol.