Ticagrelor Prescribing Information
- Ticagrelor, like other antiplatelet agents, can cause significant, sometimes fatal bleeding (,
5.1 Risk of BleedingDrugs that inhibit platelet function including ticagrelor increase the risk of bleeding
[see Warnings and Precautions (5.2)and Adverse Reactions (6.1)].
Patients treated for acute ischemic stroke or TIA
Patients at NIHSS >5 and patients receiving thrombolysis were excluded from THALES and use of ticagrelor in such patients is not recommended.).6.1 Clinical Trials ExperienceBecause clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Ticagrelor has been evaluated for safety in more than 58,000 patients.Bleeding in PLATO (Reduction in risk of thrombotic events in ACS)
Figure 1 is a plot of time to the first non-CABG major bleeding event.Figure 1 - Kaplan-Meier estimate of time to first non-CABG PLATO-defined major bleeding event (PLATO)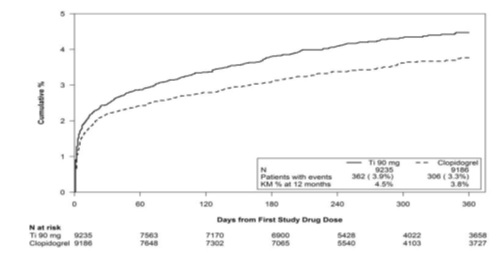
Frequency of bleeding in PLATO is summarized in Tables 1 and 2. About half of the non-CABG major bleeding events were in the first 30 days.
Table 1 - Non-CABG related bleeds (PLATO)Ticagrelor*N=9,235ClopidogrelN=9,186n (%) patients with eventn (%) patients with eventPLATO Major + Minor 713 (7.7) 567 (6.2) Major 362 (3.9) 306 (3.3) Fatal/Life-threatening 171 (1.9) 151 (1.6) Fatal 15 (0.2) 16 (0.2) Intracranial hemorrhage
(Fatal/Life-threatening)26 (0.3) 15 (0.2) PLATO Minor bleed:requires medical intervention to stop or treat bleeding.PLATO Major bleed:any one of the following: fatal; intracranial; intrapericardial with cardiac tamponade; hypovolemic shock or severe hypotension requiring intervention; significantly disabling (e.g., intraocular with permanent vision loss); associated with a decrease in Hb of at least 3 g/dL (or a fall in hematocrit (Hct) of at least 9%); transfusion of 2 or more units.PLATO Major bleed, fatal/life-threatening:any major bleed as described above and associated with a decrease in Hb of more than 5 g/dL (or a fall in hematocrit (Hct) of at least 15%); transfusion of 4 or more units.Fatal:A bleeding event that directly led to death within 7 days.*90 mg BID
No baseline demographic factor altered the relative risk of bleeding with ticagrelor compared to clopidogrel.
In PLATO, 1,584 patients underwent CABG surgery. The percentages of those patients who bled are shown in Figure 2 and Table 2.
Figure 2 – ‘Major fatal/life-threatening’ CABG-related bleeding by days from last dose of study drug to CABG procedure (PLATO)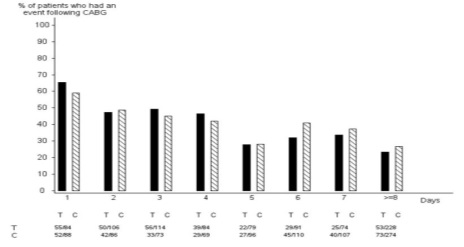
X-axis is days from last dose of study drug prior to CABG.
The PLATO protocol recommended a procedure for withholding study drug prior to CABG or other major surgery without unblinding. If surgery was elective or non-urgent, study drug was interrupted temporarily, as follows: If local practice was to allow antiplatelet effects to dissipate before surgery, capsules (blinded clopidogrel) were withheld 5 days before surgery and tablets (blinded ticagrelor) were withheld for a minimum of 24 hours and a maximum of 72 hours before surgery. If local practice was to perform surgery without waiting for dissipation of antiplatelet effects capsules and tablets were withheld 24 hours prior to surgery and use of aprotinin or other hemostatic agents was allowed. If local practice was to use IPA monitoring to determine when surgery could be performed both the capsules and tablets were withheld at the same time and the usual monitoring procedures followed.
T Ticagrelor; C Clopidogrel.Table 2 - CABG-related bleeding (PLATO)Ticagrelor*N=770ClopidogrelN=814n (%) patients with eventn (%) patients with eventPLATO Total Major 626 (81.3) 666 (81.8) Fatal/Life-threatening 337 (43.8) 350 (43) Fatal 6 (0.8) 7 (0.9) PLATO Major bleed:any one of the following: fatal; intracranial; intrapericardial with cardiac tamponade; hypovolemic shock or severe hypotension requiring intervention; significantly disabling (e.g., intraocular with permanent vision loss); associated with a decrease in Hb of at least 3 g/dL (or a fall in hematocrit (Hct) of at least 9%); transfusion of 2 or more units.PLATO Major bleed, fatal/life-threatening:any major bleed as described above and associated with a decrease in Hb of more than 5 g/dL (or a fall in hematocrit (Hct) of at least 15%); transfusion of 4 or more units.*90 mg BID
When antiplatelet therapy was stopped 5 days before CABG, major bleeding occurred in 75% of ticagrelor treated patients and 79% on clopidogrel.Other Adverse Reactions in PLATO
Adverse reactions that occurred at a rate of 4% or more in PLATO are shown in Table 3.Table 3 - Percentage of patients reporting non-hemorrhagic adverse reactions at least 4% or more in either group and more frequently on ticagrelor (PLATO)Ticagrelor*N=9,235ClopidogrelN=9,186Dyspnea 13.8 7.8 Dizziness 4.5 3.9 Nausea 4.3 3.8 *90 mg BID
Bleeding in PEGASUS(Secondary Prevention in Patients with a History of Myocardial Infarction)
Overall outcome of bleeding events in the PEGASUS study are shown in Table 4.Table 4 – Bleeding events (PEGASUS)Ticagrelor*N=6,958PlaceboN=6,996Events / 1,000 patient yearsEvents / 1,000 patient yearsTIMI Major 8 3 Fatal 1 1 Intracranial hemorrhage 2 1 TIMI Major or Minor 11 5 TIMI Major:Fatal bleeding, OR any intracranial bleeding, OR clinically overt signs of hemorrhage associated with a drop in hemoglobin (Hgb) of ≥5 g/dL, or a fall in hematocrit (Hct) of ≥15%.Fatal:A bleeding event that directly led to death within 7 days.TIMI Minor:Clinically apparent with 3 to 5 g/dL decrease in hemoglobin.*60 mg BID
The bleeding profile of ticagrelor 60 mg compared to aspirin alone was consistent across multiple pre-defined subgroups (e.g., by age, gender, weight, race, geographic region, concurrent conditions, concomitant therapy, stent, and medical history) for TIMI Major and TIMI Major or Minor bleeding events.Other Adverse Reactions in PEGASUS
Adverse reactions that occurred in PEGASUS at rates of 3% or more are shown in Table 5.Table 5 – Non-hemorrhagic adverse reactions reported in >3% of patients in the ticagrelor 60 mg treatment group (PEGASUS)Ticagrelor*N=6,958PlaceboN=6,996Dyspnea 14.2% 5.5% Dizziness 4.5% 4.1% Diarrhea 3.3% 2.5% *60 mg BID
Bleeding in THEMIS (Prevention of major CV events in patients with CAD and Type 2 Diabetes Mellitus)
The Kaplan-Meier curve of time to first TIMI Major bleeding event is presented in Figure 3.Figure 3 -Time to first TIMI Major bleeding event (THEMIS)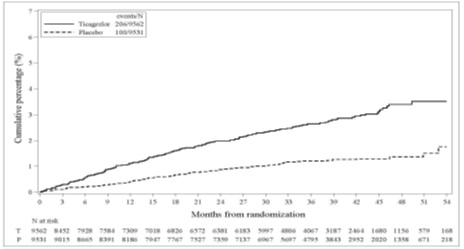
.
T = Ticagrelor; P = Placebo; N = Number of patients
The bleeding events in THEMIS are shown below in Table 6.Table 6 – Bleeding events (THEMIS)TicagrelorN=9,562PlaceboN=9,531Events / 1,000 patient yearsEvents / 1,000 patient yearsTIMI Major 9 4 TIMI Major or Minor 12 5 TIMI Major or Minor or Requiring medical attention 46 18 Fatal bleeding 1 0 Intracranial hemorrhage 3 2 Bleeding in THALES (Reduction in risk of stroke in patients with acute ischemic stroke or TIA)
The Kaplan-Meier curve of time course of GUSTO severe bleeding events is presented in Figure 4.
Figure 4 -Time course of GUSTO severe bleeding events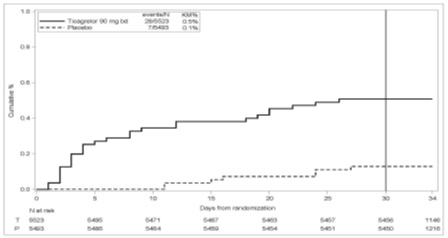
KM%: Kaplan-Meier percentage evaluated at Day 30; T = Ticagrelor; P = placebo; N = Number of patients
GUSTO Severe:Any one of the following: fatal bleeding, intracranial bleeding (excluding asymptomatic hemorrhagic transformations of ischemic brain infarctions and excluding microhemorrhages < 10 mm evident only on gradient-echo magnetic resonance imaging), bleeding that caused hemodynamic compromise requiring intervention (e.g., systolic blood pressure <90 mmg Hg that required blood or fluid replacement, or vasopressor/inotropic support, or surgical intervention).Intracranial bleeding and fatal bleeding in THALES:In total, there were 21 intracranial hemorrhages (ICHs) for ticagrelor and 6 ICHs for placebo. Fatal bleedings, almost all ICH, occurred in 11 for ticagrelor and in 2 for placebo.Bradycardia
In a Holter substudy of about 3,000 patients in PLATO, more patients had ventricular pauses with ticagrelor (6%) than with clopidogrel (3.5%) in the acute phase; rates were 2.2% and 1.6%, respectively, after 1 month. PLATO, PEGASUS, THEMIS and THALES, excluded patients at increased risk of bradycardic events (e.g., patients who have sick sinus syndrome, 2nd or 3rd degree AV block, or bradycardic-related syncope and not protected with a pacemaker).Lab abnormalities
Serum Uric Acid:
In PLATO, serum uric acid levels increased approximately 0.6 mg/dL from baseline on ticagrelor 90 mg and approximately 0.2 mg/dL on clopidogrel. The difference disappeared within 30 days of discontinuing treatment. Reports of gout did not differ between treatment groups in PLATO (0.6% in each group).
In PEGASUS, serum uric acid levels increased approximately 0.2 mg/dL from baseline on ticagrelor 60 mg and no elevation was observed on aspirin alone. Gout occurred more commonly in patients on ticagrelor than in patients on aspirin alone (1.5%, 1.1%). Mean serum uric acid concentrations decreased after treatment was stopped.
Serum Creatinine:
In PLATO, a >50% increase in serum creatinine levels was observed in 7.4% of patients receiving ticagrelor 90 mg compared to 5.9% of patients receiving clopidogrel. The increases typically did not progress with ongoing treatment and often decreased with continued therapy. Evidence of reversibility upon discontinuation was observed even in those with the greatest on treatment increases. Treatment groups in PLATO did not differ for renal-related serious adverse events such as acute renal failure, chronic renal failure, toxic nephropathy, or oliguria.
In PEGASUS, serum creatinine concentration increased by >50% in approximately 4% of patients receiving ticagrelor 60 mg, similar to aspirin alone. The frequency of renal related adverse events was similar for ticagrelor and aspirin alone regardless of age and baseline renal function.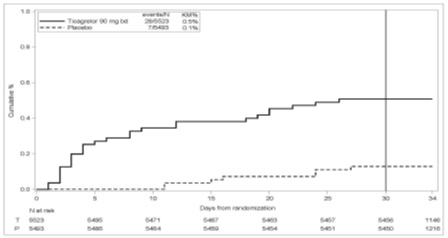
tica-tabs-fig-04 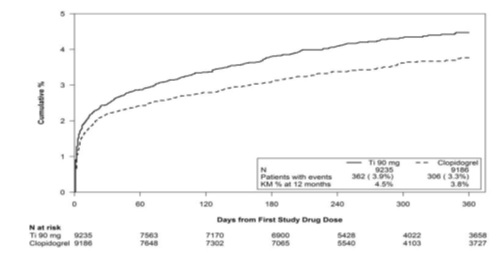
tica-tabs-fig-01 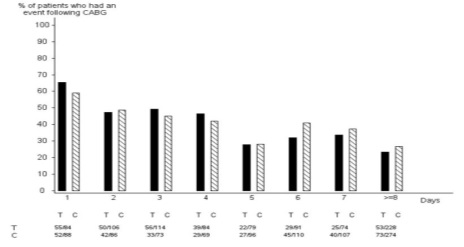
tica-tabs-fig-02 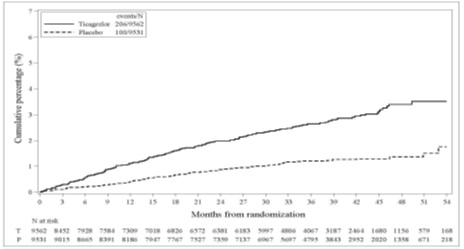
tica-tabs-fig-03 - Do not use ticagrelor in patients with active pathological bleeding or a history of intracranial hemorrhage (,
4.1 History of Intracranial HemorrhageTicagrelor is contraindicated in patients with a history of intracranial hemorrhage (ICH) because of a high risk of recurrent ICH in this population
[see Clinical Studies (14.1, 14.2)].).4.2 Active BleedingTicagrelor is contraindicated in patients with active pathological bleeding such as peptic ulcer or intracranial hemorrhage
[see Warnings and Precautions (5.1)and Adverse Reactions (6.1)]. - Do not start ticagrelor in patients undergoing urgent coronary artery bypass graft surgery (CABG) (,
5.1 Risk of BleedingDrugs that inhibit platelet function including ticagrelor increase the risk of bleeding
[see Warnings and Precautions (5.2)and Adverse Reactions (6.1)].
Patients treated for acute ischemic stroke or TIA
Patients at NIHSS >5 and patients receiving thrombolysis were excluded from THALES and use of ticagrelor in such patients is not recommended.).6.1 Clinical Trials ExperienceBecause clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Ticagrelor has been evaluated for safety in more than 58,000 patients.Bleeding in PLATO (Reduction in risk of thrombotic events in ACS)
Figure 1 is a plot of time to the first non-CABG major bleeding event.Figure 1 - Kaplan-Meier estimate of time to first non-CABG PLATO-defined major bleeding event (PLATO)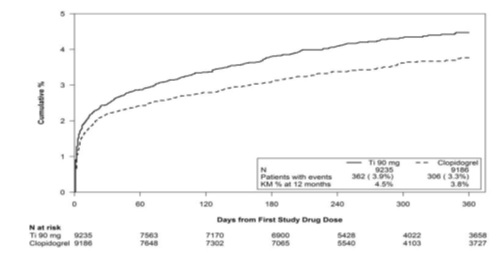
Frequency of bleeding in PLATO is summarized in Tables 1 and 2. About half of the non-CABG major bleeding events were in the first 30 days.
Table 1 - Non-CABG related bleeds (PLATO)Ticagrelor*N=9,235ClopidogrelN=9,186n (%) patients with eventn (%) patients with eventPLATO Major + Minor 713 (7.7) 567 (6.2) Major 362 (3.9) 306 (3.3) Fatal/Life-threatening 171 (1.9) 151 (1.6) Fatal 15 (0.2) 16 (0.2) Intracranial hemorrhage
(Fatal/Life-threatening)26 (0.3) 15 (0.2) PLATO Minor bleed:requires medical intervention to stop or treat bleeding.PLATO Major bleed:any one of the following: fatal; intracranial; intrapericardial with cardiac tamponade; hypovolemic shock or severe hypotension requiring intervention; significantly disabling (e.g., intraocular with permanent vision loss); associated with a decrease in Hb of at least 3 g/dL (or a fall in hematocrit (Hct) of at least 9%); transfusion of 2 or more units.PLATO Major bleed, fatal/life-threatening:any major bleed as described above and associated with a decrease in Hb of more than 5 g/dL (or a fall in hematocrit (Hct) of at least 15%); transfusion of 4 or more units.Fatal:A bleeding event that directly led to death within 7 days.*90 mg BID
No baseline demographic factor altered the relative risk of bleeding with ticagrelor compared to clopidogrel.
In PLATO, 1,584 patients underwent CABG surgery. The percentages of those patients who bled are shown in Figure 2 and Table 2.
Figure 2 – ‘Major fatal/life-threatening’ CABG-related bleeding by days from last dose of study drug to CABG procedure (PLATO)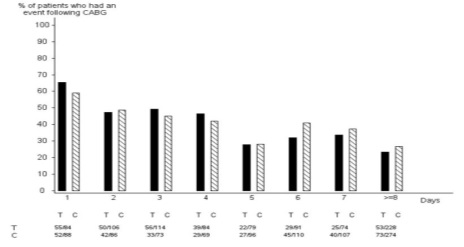
X-axis is days from last dose of study drug prior to CABG.
The PLATO protocol recommended a procedure for withholding study drug prior to CABG or other major surgery without unblinding. If surgery was elective or non-urgent, study drug was interrupted temporarily, as follows: If local practice was to allow antiplatelet effects to dissipate before surgery, capsules (blinded clopidogrel) were withheld 5 days before surgery and tablets (blinded ticagrelor) were withheld for a minimum of 24 hours and a maximum of 72 hours before surgery. If local practice was to perform surgery without waiting for dissipation of antiplatelet effects capsules and tablets were withheld 24 hours prior to surgery and use of aprotinin or other hemostatic agents was allowed. If local practice was to use IPA monitoring to determine when surgery could be performed both the capsules and tablets were withheld at the same time and the usual monitoring procedures followed.
T Ticagrelor; C Clopidogrel.Table 2 - CABG-related bleeding (PLATO)Ticagrelor*N=770ClopidogrelN=814n (%) patients with eventn (%) patients with eventPLATO Total Major 626 (81.3) 666 (81.8) Fatal/Life-threatening 337 (43.8) 350 (43) Fatal 6 (0.8) 7 (0.9) PLATO Major bleed:any one of the following: fatal; intracranial; intrapericardial with cardiac tamponade; hypovolemic shock or severe hypotension requiring intervention; significantly disabling (e.g., intraocular with permanent vision loss); associated with a decrease in Hb of at least 3 g/dL (or a fall in hematocrit (Hct) of at least 9%); transfusion of 2 or more units.PLATO Major bleed, fatal/life-threatening:any major bleed as described above and associated with a decrease in Hb of more than 5 g/dL (or a fall in hematocrit (Hct) of at least 15%); transfusion of 4 or more units.*90 mg BID
When antiplatelet therapy was stopped 5 days before CABG, major bleeding occurred in 75% of ticagrelor treated patients and 79% on clopidogrel.Other Adverse Reactions in PLATO
Adverse reactions that occurred at a rate of 4% or more in PLATO are shown in Table 3.Table 3 - Percentage of patients reporting non-hemorrhagic adverse reactions at least 4% or more in either group and more frequently on ticagrelor (PLATO)Ticagrelor*N=9,235ClopidogrelN=9,186Dyspnea 13.8 7.8 Dizziness 4.5 3.9 Nausea 4.3 3.8 *90 mg BID
Bleeding in PEGASUS(Secondary Prevention in Patients with a History of Myocardial Infarction)
Overall outcome of bleeding events in the PEGASUS study are shown in Table 4.Table 4 – Bleeding events (PEGASUS)Ticagrelor*N=6,958PlaceboN=6,996Events / 1,000 patient yearsEvents / 1,000 patient yearsTIMI Major 8 3 Fatal 1 1 Intracranial hemorrhage 2 1 TIMI Major or Minor 11 5 TIMI Major:Fatal bleeding, OR any intracranial bleeding, OR clinically overt signs of hemorrhage associated with a drop in hemoglobin (Hgb) of ≥5 g/dL, or a fall in hematocrit (Hct) of ≥15%.Fatal:A bleeding event that directly led to death within 7 days.TIMI Minor:Clinically apparent with 3 to 5 g/dL decrease in hemoglobin.*60 mg BID
The bleeding profile of ticagrelor 60 mg compared to aspirin alone was consistent across multiple pre-defined subgroups (e.g., by age, gender, weight, race, geographic region, concurrent conditions, concomitant therapy, stent, and medical history) for TIMI Major and TIMI Major or Minor bleeding events.Other Adverse Reactions in PEGASUS
Adverse reactions that occurred in PEGASUS at rates of 3% or more are shown in Table 5.Table 5 – Non-hemorrhagic adverse reactions reported in >3% of patients in the ticagrelor 60 mg treatment group (PEGASUS)Ticagrelor*N=6,958PlaceboN=6,996Dyspnea 14.2% 5.5% Dizziness 4.5% 4.1% Diarrhea 3.3% 2.5% *60 mg BID
Bleeding in THEMIS (Prevention of major CV events in patients with CAD and Type 2 Diabetes Mellitus)
The Kaplan-Meier curve of time to first TIMI Major bleeding event is presented in Figure 3.Figure 3 -Time to first TIMI Major bleeding event (THEMIS)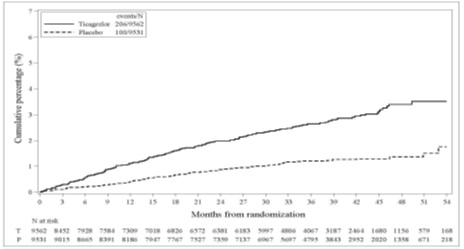
.
T = Ticagrelor; P = Placebo; N = Number of patients
The bleeding events in THEMIS are shown below in Table 6.Table 6 – Bleeding events (THEMIS)TicagrelorN=9,562PlaceboN=9,531Events / 1,000 patient yearsEvents / 1,000 patient yearsTIMI Major 9 4 TIMI Major or Minor 12 5 TIMI Major or Minor or Requiring medical attention 46 18 Fatal bleeding 1 0 Intracranial hemorrhage 3 2 Bleeding in THALES (Reduction in risk of stroke in patients with acute ischemic stroke or TIA)
The Kaplan-Meier curve of time course of GUSTO severe bleeding events is presented in Figure 4.
Figure 4 -Time course of GUSTO severe bleeding events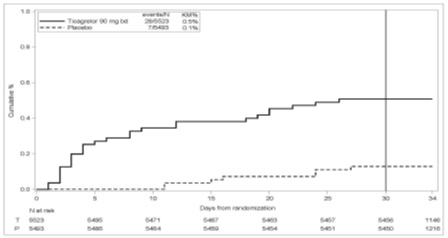
KM%: Kaplan-Meier percentage evaluated at Day 30; T = Ticagrelor; P = placebo; N = Number of patients
GUSTO Severe:Any one of the following: fatal bleeding, intracranial bleeding (excluding asymptomatic hemorrhagic transformations of ischemic brain infarctions and excluding microhemorrhages < 10 mm evident only on gradient-echo magnetic resonance imaging), bleeding that caused hemodynamic compromise requiring intervention (e.g., systolic blood pressure <90 mmg Hg that required blood or fluid replacement, or vasopressor/inotropic support, or surgical intervention).Intracranial bleeding and fatal bleeding in THALES:In total, there were 21 intracranial hemorrhages (ICHs) for ticagrelor and 6 ICHs for placebo. Fatal bleedings, almost all ICH, occurred in 11 for ticagrelor and in 2 for placebo.Bradycardia
In a Holter substudy of about 3,000 patients in PLATO, more patients had ventricular pauses with ticagrelor (6%) than with clopidogrel (3.5%) in the acute phase; rates were 2.2% and 1.6%, respectively, after 1 month. PLATO, PEGASUS, THEMIS and THALES, excluded patients at increased risk of bradycardic events (e.g., patients who have sick sinus syndrome, 2nd or 3rd degree AV block, or bradycardic-related syncope and not protected with a pacemaker).Lab abnormalities
Serum Uric Acid:
In PLATO, serum uric acid levels increased approximately 0.6 mg/dL from baseline on ticagrelor 90 mg and approximately 0.2 mg/dL on clopidogrel. The difference disappeared within 30 days of discontinuing treatment. Reports of gout did not differ between treatment groups in PLATO (0.6% in each group).
In PEGASUS, serum uric acid levels increased approximately 0.2 mg/dL from baseline on ticagrelor 60 mg and no elevation was observed on aspirin alone. Gout occurred more commonly in patients on ticagrelor than in patients on aspirin alone (1.5%, 1.1%). Mean serum uric acid concentrations decreased after treatment was stopped.
Serum Creatinine:
In PLATO, a >50% increase in serum creatinine levels was observed in 7.4% of patients receiving ticagrelor 90 mg compared to 5.9% of patients receiving clopidogrel. The increases typically did not progress with ongoing treatment and often decreased with continued therapy. Evidence of reversibility upon discontinuation was observed even in those with the greatest on treatment increases. Treatment groups in PLATO did not differ for renal-related serious adverse events such as acute renal failure, chronic renal failure, toxic nephropathy, or oliguria.
In PEGASUS, serum creatinine concentration increased by >50% in approximately 4% of patients receiving ticagrelor 60 mg, similar to aspirin alone. The frequency of renal related adverse events was similar for ticagrelor and aspirin alone regardless of age and baseline renal function.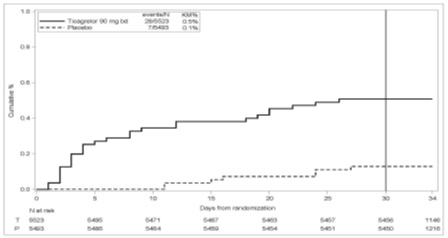
tica-tabs-fig-04 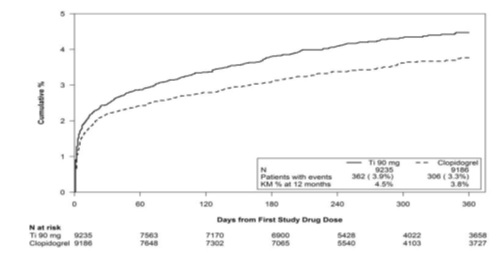
tica-tabs-fig-01 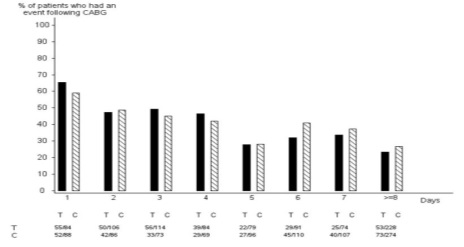
tica-tabs-fig-02 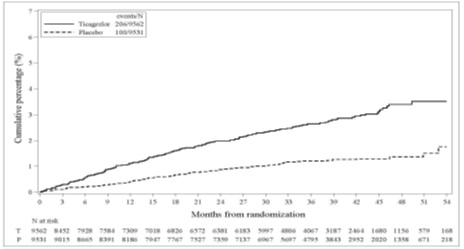
tica-tabs-fig-03 - If possible, manage bleeding without discontinuing ticagrelor. Stopping ticagrelor increases the risk of subsequent cardiovascular events ().
5.2 Discontinuation of Ticagrelor in Patients Treated for Coronary Artery DiseaseDiscontinuation of ticagrelor will increase the risk of myocardial infarction, stroke, and death in patients being treated for coronary artery disease. If ticagrelor must be temporarily discontinued (e.g., to treat bleeding or for significant surgery), restart it as soon as possible. When possible, interrupt therapy with ticagrelor for five days prior to surgery that has a major risk of bleeding. Resume ticagrelor as soon as hemostasis is achieved.
Dosage and Administration (
Initiate treatment with a 180 mg loading dose of ticagrelor tablets. Administer
Initiate ticagrelor tablets with a daily maintenance dose of aspirin of 75 mg to 100 mg. However, in patients who have undergone percutaneous coronary intervention (PCI), consider single antiplatelet therapy with ticagrelor tablets based on the evolving risk for thrombotic versus bleeding events
Initiate treatment with a 180 mg loading dose of ticagrelor tablets and then continue
Use ticagrelor tablets with a loading dose of aspirin (300 mg to 325 mg) and a daily maintenance dose of aspirin of 75 mg to 100 mg
Ticagrelor tablets are a P2Y12 platelet inhibitor indicated
- to reduce the risk of cardiovascular (CV) death, myocardial infarction (MI), and stroke in patients with acute coronary syndrome (ACS) or a history of MI. For at least the first 12 months following ACS, it is superior to clopidogrel.
Ticagrelor tablets also reduces the risk of stent thrombosis in patients who have been stented for treatment of ACS. ()1.1 Acute Coronary Syndrome or a History of Myocardial InfarctionTicagrelor tablets are indicated to reduce the risk of cardiovascular (CV) death, myocardial infarction (MI), and stroke in patients with acute coronary syndrome (ACS) or a history of MI. For at least the first 12 months following ACS, it is superior to clopidogrel.
Ticagrelor tablets also reduces the risk of stent thrombosis in patients who have been stented for treatment of ACS[see Clinical Studies (14.1)]. - to reduce the risk of a first MI or stroke in patients with coronary artery disease (CAD) at high risk for such events. While use is not limited to this setting, the efficacy of ticagrelor tablets was established in a population with type 2 diabetes mellitus (T2DM). ()
1.2 Coronary Artery Disease but No Prior Stroke or Myocardial InfarctionTicagrelor tablets are indicated to reduce the risk of a first MI or stroke in patients with coronary artery disease (CAD) at high risk for such events
[see Clinical Studies (14.2)]. While use is not limited to this setting, the efficacy of ticagrelor tablets was established in a population with type 2 diabetes mellitus (T2DM). - to reduce the risk of stroke in patients with acute ischemic stroke (NIH Stroke Scale score ≤5) or high-risk transient ischemic attack (TIA). ()
1.3 Acute Ischemic Stroke or Transient Ischemic Attack (TIA)Ticagrelor tablets are indicated to reduce the risk of stroke in patients with acute ischemic stroke (NIH Stroke Scale score ≤5) or high-risk transient ischemic attack (TIA)
[see Clinical Studies (14.3)].
- ACS or History of MI
- Initiate treatment with 180 mg oral loading dose of ticagrelor tablets. Then administer 90 mg twice daily during the first year. After one year, administer 60 mg twice daily. ()
2.2 Acute Coronary Syndrome or a History of Myocardial InfarctionInitiate treatment with a 180 mg loading dose of ticagrelor tablets. Administer
thefirst 90 mg maintenance dose of ticagrelor tablets, 6 to 12 hours after the loading dose. Administer 90 mg of ticagrelor tablets twice daily during the first year after an ACS event. After one year, administer 60 mg of ticagrelor tablets twice daily.
Initiate ticagrelor tablets with a daily maintenance dose of aspirin of 75 mg to 100 mg. However, in patients who have undergone percutaneous coronary intervention (PCI), consider single antiplatelet therapy with ticagrelor tablets based on the evolving risk for thrombotic versus bleeding events[see Warnings and Precautions (5.1)and Clinical Studies (14)]. - Patients with CAD and No Prior Stroke or MI
- Administer 60 mg ticagrelor tablets twice daily. ()
2.3 Coronary Artery Disease but No Prior Stroke or Myocardial InfarctionAdminister 60 mg of ticagrelor tablets twice daily.
Generally, use ticagrelor tablets with a daily maintenance dose of aspirin of 75 mg to 100 mg[see Clinical Studies (14)]. - Acute Ischemic Stroke
- Initiate treatment with a 180 mg loading dose of ticagrelor tablets then continue with 90 mg twice daily for up to 30 days. ()
2.4 Acute Ischemic Stroke or Transient Ischemic Attack (TIA)Initiate treatment with a 180 mg loading dose of ticagrelor tablets and then continue
with90 mg twice daily for up to 30 days. Administer the first maintenance dose 6 to 12 hours after the loading dose.
Use ticagrelor tablets with a loading dose of aspirin (300 mg to 325 mg) and a daily maintenance dose of aspirin of 75 mg to 100 mg[see Clinical Studies (14)].
Use ticagrelor tablets with a daily maintenance dose of aspirin of 75 to 100 mg. (
- ACS or History of MI
- Initiate treatment with 180 mg oral loading dose of ticagrelor tablets. Then administer 90 mg twice daily during the first year. After one year, administer 60 mg twice daily.
- Patients with CAD and No Prior Stroke or MI
- Administer 60 mg ticagrelor tablets twice daily.
- Acute Ischemic Stroke
- Initiate treatment with a 180 mg loading dose of ticagrelor tablets then continue with 90 mg twice daily for up to 30 days.
Use ticagrelor tablets with a daily maintenance dose of aspirin of 75 to 100 mg. However, in patients who have undergone PCI, consider single antiplatelet therapy with ticagrelor tablets based on the evolving risk for thrombotic versus bleeding events.
Advise patients who miss a dose of ticagrelor tablets to take their next dose at its scheduled time.
For patients who are unable to swallow tablets whole, ticagrelor tablets can be crushed, mixed with water, and drunk. The mixture can also be administered via a nasogastric tube (CH8 or greater)
Do not administer ticagrelor tablets with another oral P2Y12platelet inhibitor.
Avoid aspirin at doses higher than recommended
Initiate treatment with a 180 mg loading dose of ticagrelor tablets. Administer
Initiate ticagrelor tablets with a daily maintenance dose of aspirin of 75 mg to 100 mg. However, in patients who have undergone percutaneous coronary intervention (PCI), consider single antiplatelet therapy with ticagrelor tablets based on the evolving risk for thrombotic versus bleeding events
Administer 60 mg of ticagrelor tablets twice daily.
Generally, use ticagrelor tablets with a daily maintenance dose of aspirin of 75 mg to 100 mg
Initiate treatment with a 180 mg loading dose of ticagrelor tablets and then continue
Use ticagrelor tablets with a loading dose of aspirin (300 mg to 325 mg) and a daily maintenance dose of aspirin of 75 mg to 100 mg
Initiate treatment with a 180 mg loading dose of ticagrelor tablets. Administer
Initiate ticagrelor tablets with a daily maintenance dose of aspirin of 75 mg to 100 mg. However, in patients who have undergone percutaneous coronary intervention (PCI), consider single antiplatelet therapy with ticagrelor tablets based on the evolving risk for thrombotic versus bleeding events
Ticagrelor tablets, 90 mg is supplied as a round, biconvex, yellow, film-coated tablets debossed with “M” on one side and “90” on other side.
- Lactation: Breastfeeding not recommended ()
8.2 LactationRisk Summary
There are no data on the presence of ticagrelor or its metabolites in human milk, the effects on the breastfed infant, or the effects on milk production. Ticagrelor and its metabolites were present in rat milk at higher concentrations than in maternal plasma. When a drug is present in animal milk, it is likely that the drug will be present in human milk. Breastfeeding is not recommended during treatment with ticagrelor.