Valtya 1/35 Prescribing Information
Valtya 1/35 is indicated for the prevention of pregnancy in women who elect to use oral contraceptives as a method of contraception.
Oral contraceptives are highly effective. Table 1 lists the typical accidental pregnancy rates for users of combination oral contraceptives and other methods of contraception. The efficacy of these contraceptive methods, except sterilization and progestogen implants and injections, depends upon the reliability with which they are used. Correct and consistent use of methods can result in lower failure rates.
Emergency Contraceptive Pills : Treatment initiated within 72 hours after unprotected intercourse reduces the risk of pregnancy by at least 75%.The treatment schedule is one dose within 72 hours after unprotected intercourse and a second dose 12 hours after the first dose. The Food and Drug Administration has declared the following brands of oral contraceptives to be safe and effective for emergency contraception: Ovral (1 dose is 2 white pills), Alesse (1 dose is 5 pink pills), Nordette or Levlen (1 dose is 2 light-orange pills), Lo/Ovral (1 dose is 4 white pills), Triphasil or Tri-Levlen (1 dose is 4 yellow pills). | |||
Lactational Amenorrhea Method : LAM is a highly effective, temporary method of contraception.However, to maintain effective protection against pregnancy, another method of contraception must be used as soon as menstruation resumes, the frequency or duration of breastfeeds is reduced, bottle feeds are introduced, or the baby reaches six months of age. | |||
| Source: Trussell J, Contraceptive efficacy. In Hatcher RA, Trussell J, Stewart F, Cates W, Stewart GK, Kowal D, Guest F, Contraceptive Technology: Seventeenth Revised Edition. New York NY: Irvington Publishers, 1998, in press.1 | |||
% of women experiencing an unintended pregnancy within the first year of use | % of women continuing use at one year Among couples attempting to avoid pregnancy, the percentage who continue to use a method for one year. | ||
Method (1) | Typical use Among typical couples who initiate use of a method (not necessarily for the first time), the percentage who experience an accidental pregnancy during the first year if they do not stop use for any other reason.(2) | Perfect use Among couples who initiate use of a method (not necessarily for the first time) and who use it perfectly (both consistently and correctly), the percentage who experience an accidental pregnancy during the first year if they do not stop use for any other reason.(3) | (4) |
Chance The percents becoming pregnant in columns (2) and (3) are based on data from populations where contraception is not used and from women who cease using contraception in order to become pregnant. Among such populations, about 89% become pregnant within one year. This estimate was lowered slightly (to 85%) to represent the percent who would become pregnant within one year among women now relying on reversible methods of contraception if they abandoned contraception altogether. | 85 | 85 | |
Spermicides Foams, creams, gels, vaginal suppositories, and vaginal film. | 26 | 6 | 40 |
Periodic abstinence | 25 | 63 | |
Calendar | 9 | ||
Ovulation method | 3 | ||
Sympto-thermal Cervical mucus (ovulation) method supplemented by calendar in the pre-ovulatory and basal body temperature in the post-ovulatory phases. | 2 | ||
Post-ovulation | 1 | ||
Withdrawal | 19 | 4 | |
Cap With spermicidal cream or jelly. | |||
Parous women | 40 | 26 | 42 |
Nulliparous women | 20 | 9 | 56 |
Sponge | |||
Parous women | 40 | 20 | 42 |
Nulliparous women | 20 | 9 | 56 |
Diaphragm | 20 | 6 | 56 |
Condom Without spermicides. | |||
Female (Reality®) | 21 | 5 | 56 |
Male | 14 | 3 | 61 |
Pill | 5 | 71 | |
Progestin only | 0.5 | ||
Combined | 0.1 | ||
IUD | |||
Progesterone T | 2 | 1.5 | 81 |
Copper T 380A | 0.8 | 0.6 | 78 |
LNg 20 | 0.1 | 0.1 | 81 |
Injection (Depo-Provera) | 0.3 | 0.3 | 70 |
Implant (Norplant and Norplant-2) | 0.05 | 0.05 | 88 |
Female sterilization | 0.5 | 0.5 | 100 |
Male sterilization | 0.15 | 0.1 | 100 |
To achieve maximum contraceptive effectiveness, oral contraceptives must be taken exactly as directed and at intervals of 24 hours.
IMPORTANT: If the Sunday start schedule is selected, the patient should be instructed to use an additional method of protection until after the first week of administration
Each Valtya 1/35 tablet dispenser contains 21 light orange colored active tablets arranged in three numbered rows of 7 tablets each, followed by a fourth row of 7 green placebo tablets.
Days of the week are printed above the tablets, starting with Sunday on the left.
Breakthrough bleeding and spotting are sometimes encountered in patients on oral contraceptives, especially during the first three months of use. Nonhormonal causes should be considered and adequate diagnostic measures taken to rule out malignancy or pregnancy in the event of breakthrough bleeding, as in the case of any abnormal vaginal bleeding. If a pathologic basis has been excluded, time alone or a change to another formulation may solve the problem. In the event of amenorrhea, pregnancy should be ruled out. Some women may encounter post-pill amenorrhea or oligomenorrhea, especially when such a condition was pre-existent.
Extensive epidemiological studies have revealed no increased risk of birth defects in women who have used oral contraceptives prior to pregnancy.126, 129The majority of recent studies also do not suggest a teratogenic effect, particularly insofar as cardiac anomalies and limb reduction defects are concerned,126, 129when the pill is taken inadvertently during early pregnancy.
The administration of oral contraceptives to induce withdrawal bleeding should not be used as a test for pregnancy. Oral contraceptives should not be used during pregnancy to treat threatened or habitual abortion. It is recommended that for any patient who has missed two consecutive periods, pregnancy should be ruled out before continuing oral contraceptive use. If the patient has not adhered to the prescribed schedule, the possibility of pregnancy should be considered at the time of the first missed period and further use of oral contraceptives should be withheld until pregnancy has been ruled out. Oral contraceptive use should be discontinued if pregnancy is confirmed.
If the patient has
If the patient has adhered to the prescribed regimen and misses two consecutive periods, pregnancy should be ruled out before continuing the contraceptive regimen.
The first intermenstrual interval after discontinuing the tablets is usually prolonged; consequently, a patient for whom a 28-day cycle is usual might not begin to menstruate for 35 days or longer. Ovulation in such prolonged cycles will occur correspondingly later in the cycle. Post-treatment cycles after the first one, however, are usually typical for the individual woman prior to taking tablets. (See
Breakthrough bleeding and spotting are sometimes encountered in patients on oral contraceptives, especially during the first three months of use. Nonhormonal causes should be considered and adequate diagnostic measures taken to rule out malignancy or pregnancy in the event of breakthrough bleeding, as in the case of any abnormal vaginal bleeding. If a pathologic basis has been excluded, time alone or a change to another formulation may solve the problem. In the event of amenorrhea, pregnancy should be ruled out. Some women may encounter post-pill amenorrhea or oligomenorrhea, especially when such a condition was pre-existent.
If two consecutive active tablets are missed in week 3 of the dispenser or three consecutive active tablets are missed during any of the first 3 weeks of the dispenser, direct the patient to do one of the following: Day 1 Starters should discard the rest of the dispenser and begin a new dispenser that same day; Sunday Starters should continue to take 1 tablet daily until Sunday, discard the rest of the dispenser and begin a new dispenser that same day. The patient may not have a period this month; however, if she has missed two consecutive periods, pregnancy should be ruled out. An additional method of protection must be used as a backup for the next 7 days after the tablets are missed if she has sex during that time or she may become pregnant.
While there is little likelihood of ovulation if only one active tablet is missed, the possibility of spotting or breakthrough bleeding is increased and should be expected if two or more successive active tablets are missed. However, the possibility of ovulation increases with each successive day that scheduled active tablets are missed.
If one or more placebo tablets of Valtya 1/35 are missed, the Valtya 1/35 schedule should be resumed on the eighth day after the last light orange tablet was taken. Omission of placebo tablets in the 28-tablet courses does not increase the possibility of conception provided that this schedule is followed.
Ethynodiol diacetate and ethinyl estradiol tablets are contraindicated in females who are known to have or develop the following conditions:
• Thrombophlebitis or thromboembolic disorders• A past history of deep vein thrombophlebitis or thromboembolic disorders• Cerebral vascular disease, myocardial infarction, or coronary artery disease, or a past history of these conditions• Current diagnosis of, or history of, breast cancer, which may be hormone-sensitive• Known or suspected carcinoma of the female reproductive organs or suspected estrogen-dependent neoplasia, or a history of these conditions• Undiagnosed abnormal genital bleeding• History of cholestatic jaundice of pregnancy or jaundice with prior oral contraceptive use• Past or present, benign or malignant liver tumors• Known or suspected pregnancy• Are receiving Hepatitis C drug combinations containing ombitasvir/paritaprevir/ritonavir, with or without dasabuvir, due to the potential for ALT elevations (see,WARNINGSCigarette smoking increases the risk of serious cardiovascular side effects from oral contraceptive use. This risk increases with age and with heavy smoking (15 or more cigarettes per day) and is quite marked in women over 35 years of age. Women who use oral contraceptives should be strongly advised not to smoke.The use of oral contraceptives is associated with increased risk of several serious conditions including venous and arterial thromboembolism, thrombotic and hemorrhagic stroke, myocardial infarction, liver tumors or other liver lesions, and gallbladder disease. The risk of morbidity and mortality increases significantly in the presence of other risk factors such as hypertension, hyperlipidemia, obesity, and diabetes mellitus.
Practitioners prescribing oral contraceptives should be familiar with the following information relating to these and other risks.
The information contained herein is principally based on studies carried out in patients who used oral contraceptives with formulations containing higher amounts of estrogens and progestogens than those in common use today. The effect of long-term use of the oral contraceptives with lesser amounts of both estrogens and progestogens remains to be determined.
Throughout this labeling, epidemiological studies reported are of two types: retrospective case-control studies and prospective cohort studies. Case-control studies provide an estimate of the relative risk of a disease, which is defined as the
ratioof the incidence of a disease among oral contraceptive users to that among nonusers. The relative risk (or odds ratio) does not provide information about the actual clinical occurrence of a disease. Cohort studies provide a measure of both the relative risk and the attributable risk. The latter is thedifferencein the incidence of disease between oral contraceptive users and nonusers. The attributable risk does provide information about the actual occurrence or incidence of a disease in the subject population. For further information, the reader is referred to a text on epidemiological methods.1. Thromboembolic disorders and other vascular problemsa. Myocardial infarctionAn increased risk of myocardial infarction has been associated with oral contraceptive use.2-21This increased risk is primarily in smokers or in women with other underlying risk factors for coronary artery disease such as hypertension, obesity, diabetes, and hypercholesterolemia. The relative risk for myocardial infarction in current oral contraceptive users has been estimated to be 2 to 6. The risk is very low under the age of 30. However, there is the possibility of a risk of cardiovascular disease even in very young women who take oral contraceptives.
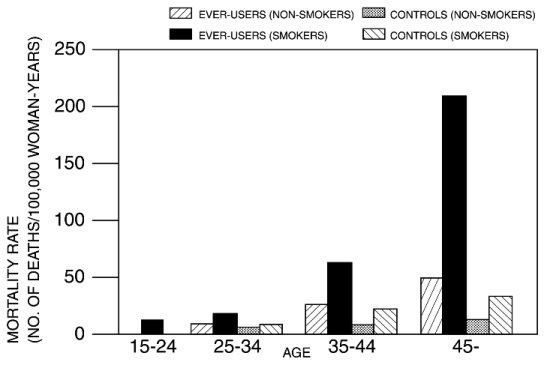
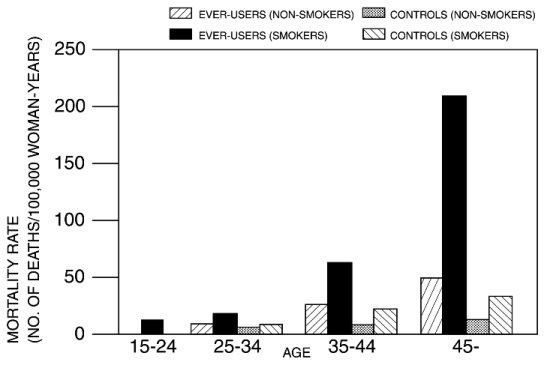
Smoking in combination with oral contraceptive use has been reported to contribute substantially to the risk of myocardial infarction in women in their mid-thirties or older, with smoking accounting for the majority of excess cases.22Mortality rates associated with circulatory disease have been shown to increase substantially in smokers, especially in those 35 years of age and older among women who use oral contraceptives (see Figure 1, Table 2).
Figure 1. Circulatory disease mortality rates per 100,000 woman-years by age, smoking status, and oral contraceptive use.14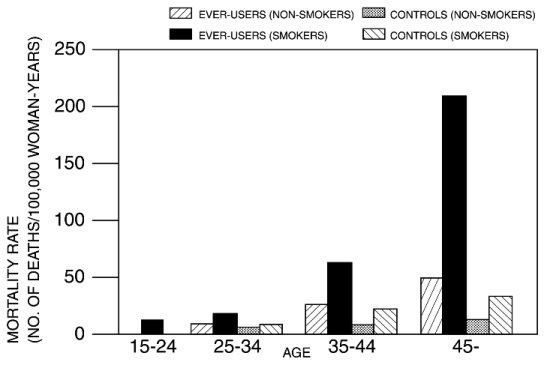
Adapted from Layde and Beral.14
Oral contraceptives may compound the effects of well-known cardiovascular risk factors such as hypertension, diabetes, hyperlipidemias, hypercholesterolemia, age, cigarette smoking, and obesity. In particular, some progestogens decrease HDL cholesterol23-31and cause glucose intolerance, while estrogens may create a state of hyperinsulinism.32Oral contraceptives have been shown to increase blood pressure among some users (see
WARNINGNo. 9). Similar effects on risk factors have been associated with an increased risk of heart disease.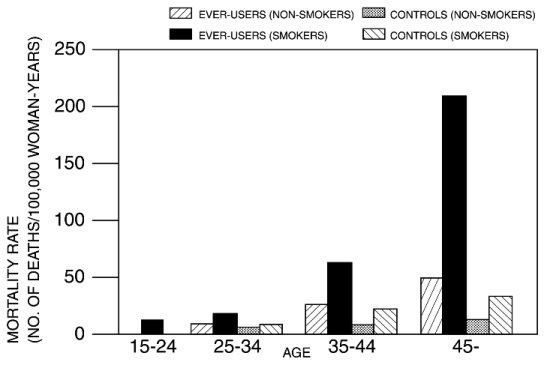
Graph b. ThromboembolismAn increased risk of thromboembolic and thrombotic disease associated with the use of oral contraceptives is well established.17,33-51Case-control studies have estimated the relative risk to be 3 for the first episode of superficial venous thrombosis, 4 to 11 for deep vein thrombosis or pulmonary embolism, and 1.5 to 6 for women with predisposing conditions for venous thromboembolic disease.34-37, 45, 46Cohort studies have shown the relative risk to be somewhat lower, about 3 for new cases (subjects with no past history of venous thrombosis or varicose veins) and about 4.5 for new cases requiring hospitalization.42, 47, 48The risk of venous thromboembolic disease associated with oral contraceptives is not related to duration of use.
A two- to seven-fold increase in relative risk of postoperative thromboembolic complications has been reported with the use of oral contraceptives.38, 39The relative risk of venous thrombosis in women who have predisposing conditions is about twice that of women without such medical conditions.43If feasible, oral contraceptives should be discontinued at least 4 weeks prior to and for 2 weeks after elective surgery of a type associated with an increased risk of thromboembolism, and also during and following prolonged immobilization. Since the immediate postpartum period is also associated with an increased risk of thromboembolism, oral contraceptives should be started no earlier than 4 to 6 weeks after delivery in women who elect not to breast feed.
c. Cerebrovascular diseasesBoth the relative and attributable risks of cerebrovascular events (thrombotic and hemorrhagic strokes) have been reported to be increased with oral contraceptive use,14, 17, 18, 34, 42, 46, 52-59although, in general, the risk was greatest among older (over 35 years), hypertensive women who also smoked. Hypertension was reported to be a risk factor for both users and nonusers, for both types of strokes, while smoking increased the risk for hemorrhagic strokes.
In one large study,52the relative risk for thrombotic stroke was reported as 9.5 times greater in users than in nonusers. It ranged from 3 for normotensive users to 14 for users with severe hypertension.54The relative risk for hemorrhagic stroke was reported to be 1.2 for nonsmokers who used oral contraceptives, 1.9 to 2.6 for smokers who did not use oral contraceptives, 6.1 to 7.6 for smokers who used oral contraceptives, 1.8 for normotensive users, and 25.7 for users with severe hypertension. The risk is also greater in older women and among smokers.
d. Dose-related risk of vascular disease with oral contraceptivesA positive association has been reported between the amount of estrogen and progestogen in oral contraceptives and the risk of vascular disease.41, 43, 53, 59-64A decline in serum high density lipoproteins (HDL) has been reported with many progestogens.23-31A decline in serum high density lipoproteins has been associated with an increased incidence of ischemic heart disease.65Because estrogens increase HDL-cholesterol, the net effect of an oral contraceptive depends on the balance achieved between doses of estrogen and progestogen and the nature and absolute amount of progestogens used in the contraceptives. The amount of both steroids should be considered in the choice of an oral contraceptive.
Minimizing exposure to estrogen and progestogen is in keeping with good principles of therapeutics. For any particular estrogen-progestogen combination, the dosage regimen prescribed should be one that contains the least amount of estrogen and progestogen that is compatible with a low failure rate and the needs of the individual patient. New acceptors of oral contraceptives should be started on preparations containing the lowest estrogen content that produces satisfactory results in the individual.
Products containing 50 mcg estrogen should be used only when medically indicated.
e. Persistence of risk of vascular diseaseThere are three studies that have shown persistence of risk of vascular disease for users of oral contraceptives. In a study in the United States, the risk of developing myocardial infarction after discontinuing oral contraceptives persisted for at least 9 years for women 40 to 49 years old who had used oral contraceptives for 5 or more years, but this increased risk was not demonstrated in other age groups.16Another American study reported former use of oral contraceptives was significantly associated with increased risk of subarachnoid hemorrhage.57In another study, in Great Britain, the risk of developing nonrheumatic heart disease plus hypertension, subarachnoid hemorrhage, cerebral thrombosis, and transient ischemic attacks persisted for at least 6 years after discontinuation of oral contraceptives, although the excess risk was small.14, 18, 66It should be noted that these studies were performed with oral contraceptive formulations containing 50 mcg or more of estrogens.
2. Estimates of mortality from contraceptive useOne study67gathered data from a variety of sources that have estimated the mortality rates associated with different methods of contraception at different ages (Table 2). These estimates include the combined risk of death associated with contraceptive methods plus the risk attributable to pregnancy in the event of method failure. Each method of contraception has its specific benefits and risks. The study concluded that, with the exception of oral contraceptive users 35 and older who smoke and 40 or older who do not smoke, mortality associated with all methods of birth control is low and below that associated with childbirth. The observation of a possible increase in risk of mortality with age for oral contraceptive users is based on data gathered in the 1970's, but not reported until 1983.67However, current clinical practice involves the use of lower estrogen dose formulations combined with careful restriction of oral contraceptive use to women who do not have the various risk factors listed in this labeling.
Because of these changes in practice and, also, because of some limited new data that suggest that the risk of cardiovascular disease with the use of oral contraceptives may now be less than previously observed,48, 152the Fertility and Maternal Health Drugs Advisory Committee was asked to review the topic in 1989. The Committee concluded that, although cardiovascular disease risks may be increased with oral contraceptive use after age 40 in healthy nonsmoking women (even with the newer low-dose formulations), there are greater potential health risks associated with pregnancy in older women and with the alternative surgical and medical procedures that may be necessary if such women do not have access to effective and acceptable means of contraception.
Therefore, the Committee recommended that the benefits of oral contraceptive use by healthy nonsmoking women over 40 may outweigh the possible risks. Of course, older women, as all women who take oral contraceptives, should take the lowest possible dose formulation that is effective.
Table 2. Annual number of birth-related or method-related deaths associated with control of fertility per 100,000 nonsterile women, by fertility control method according to age.67 AgeMethod of control15 to 1920 to 2425 to 2930 to 3435 to 3940 to 44No fertility control methodsDeaths are birth-related
7
7.4
9.1
14.8
25.7
28.2
Oral contraceptives
nonsmokerDeaths are method-related
0.3
0.5
0.9
1.9
13.8
31.6
smoker
2.2
3.4
6.6
13.5
51.1
117.2
IUD
0.8
0.8
1
1
1.4
1.4
Condom
1.1
1.6
0.7
0.2
0.3
0.4
Diaphragm/Spermicide
1.9
1.2
1.2
1.3
2.2
2.8
Periodic abstinence
2.5
1.6
1.6
1.7
2.9
3.6
Adapted from Ory.
673. Malignant NeoplasmsBreast CancerEthynodiol diacetate and ethinyl estradiol tablets are contraindicated in females who currently have or have had breast cancer because breast cancer may be hormonally sensitive (see
Contraindications (4)).Epidemiology studies have not found a consistent association between use of combined oral contraceptives (COCs) and breast cancer risk. Studies do not show an association between ever (current or past) use of COCs and risk of breast cancer. However, some studies report a small increase in the risk of breast cancer among current or recent users (<6 months since last use) and current users with longer duration of COC use (see
Post Marketing Experience).Cervical CancerSome studies suggested that oral contraceptive use was associated with an increase in the risk of cervical intraepithelial neoplasia, dysplasia, erosion, carcinoma, or micro-glandular dysplasia in some populations of women.17, 50, 103-115However, there continues to be controversy about the extent to which such findings may be due to differences in sexual behavior and other factors.
In spite of many studies of the relationship between oral contraceptive use and breast and cervical cancers, a cause and effect relationship has not been established.
4. Hepatic neoplasiaBenign hepatic adenomas and other hepatic lesions have been associated with oral contraceptive use,116-121although the incidence of such benign tumors is rare in the United States. Indirect calculations have estimated the attributable risk to be in the range of 3.3 cases per 100,000 for users, a risk that increases after 4 or more years of use.120Rupture of benign, hepatic adenomas or other lesions may cause death through intraabdominal hemorrhage. Therefore, such lesions should be considered in women presenting with abdominal pain and tenderness, abdominal mass, or shock. About one quarter of the cases presented because of abdominal masses; up to one half had signs and symptoms of acute intraperitoneal hemorrhage.121Diagnosis may prove difficult.
Studies from the U.S.,122, 150Great Britain,123, 124and Italy125have shown an increased risk of hepatocellular carcinoma in long-term (greater than 8 years; relative risk of 7 to 20) oral contraceptive users. However, these cancers are rare in the United States, and the attributable risk (the excess incidence) of liver cancers in oral contraceptive users approaches less than 1 per 1,000,000 users.
RISK OF LIVER ENZYME ELEVATIONS WITH CONCOMITANT HEPATITIS C TREATMENTDuring clinical trials with the Hepatitis C combination drug regimen that contains ombitasvir/paritaprevir/ritonavir, with or without dasabuvir, ALT elevations greater than 5 times the upper limit of normal (ULN), including some cases greater than 20 times the ULN, were significantly more frequent in women using ethinyl estradiol-containing medications such as CHCs. Discontinue ethynodiol diacetate and ethinyl estradiol prior to starting therapy with the combination drug regimen ombitasvir/paritaprevir/ritonavir, with or without dasabuvir
[see Contraindications (4)].Ethynodiol diacetate and ethinyl estradiol can be restarted approximately 2 weeks following completion of treatment with the combination drug regimen.5. Ocular lesionsThere have been reports of retinal thrombosis and other ocular lesions associated with the use of oral contraceptives. Oral contraceptives should be discontinued if there is unexplained, gradual or sudden, partial or complete loss of vision; onset of proptosis or diplopia; papilledema; or any evidence of retinal vascular lesions. Appropriate diagnostic and therapeutic measures should be undertaken immediately.
6. Oral contraceptive use before or during pregnancyExtensive epidemiological studies have revealed no increased risk of birth defects in women who have used oral contraceptives prior to pregnancy.126, 129The majority of recent studies also do not suggest a teratogenic effect, particularly insofar as cardiac anomalies and limb reduction defects are concerned,126, 129when the pill is taken inadvertently during early pregnancy.
The administration of oral contraceptives to induce withdrawal bleeding should not be used as a test for pregnancy. Oral contraceptives should not be used during pregnancy to treat threatened or habitual abortion. It is recommended that for any patient who has missed two consecutive periods, pregnancy should be ruled out before continuing oral contraceptive use. If the patient has not adhered to the prescribed schedule, the possibility of pregnancy should be considered at the time of the first missed period and further use of oral contraceptives should be withheld until pregnancy has been ruled out. Oral contraceptive use should be discontinued if pregnancy is confirmed.
7. Gallbladder diseaseEarlier studies reported an increased lifetime relative risk of gallbladder surgery in users of oral contraceptives and estrogens.40, 42, 53, 70More recent studies, however, have shown that the relative risk of developing gallbladder disease among oral contraceptive users may be minimal.130-132The recent findings of minimal risk may be related to the use of oral contraceptive formulations containing lower doses of estrogens and progestogens.
8. Carbohydrate and lipid metabolic effectsOral contraceptives have been shown to cause a decrease in glucose tolerance in a significant percentage of users.32This effect has been shown to be directly related to estrogen dose.133Progestogens increase insulin secretion and create insulin resistance, the effect varying with different progestational agents.32, 134However, in the nondiabetic woman, oral contraceptives appear to have no effect on fasting blood glucose. Because of these demonstrated effects, prediabetic and diabetic women should be carefully observed while taking oral contraceptives.
Some women may have persistent hypertriglyceridemia while on the pill. As discussed earlier (see
WARNINGS1aand 1d), changes in serum triglycerides and lipoprotein levels have been reported in oral contraceptive users.23-31, 135, 1369. Elevated blood pressureAn increase in blood pressure has been reported in women taking oral contraceptives50, 53, 137-139and this increase is more likely in older oral contraceptive users137and with extended duration of use.53Data from the Royal College of General Practitioners138and subsequent randomized trials have shown that the incidence of hypertension increases with increasing concentrations of progestogens.
Women with a history of hypertension or hypertension-related disease, or renal disease139should be encouraged to use another method of contraception. If such women elect to use oral contraceptives, they should be monitored closely and if significant elevation of blood pressure occurs, oral contraceptives should be discontinued. For most women, elevated blood pressure will return to normal after stopping oral contraceptives,137and there is no difference in the occurrence of hypertension among ever and never-users.140
10. HeadacheThe onset or exacerbation of migraine or the development of headache of a new pattern that is recurrent, persistent, or severe requires discontinuation of oral contraceptives and evaluation of the cause.
11. Bleeding irregularitiesBreakthrough bleeding and spotting are sometimes encountered in patients on oral contraceptives, especially during the first three months of use. Nonhormonal causes should be considered and adequate diagnostic measures taken to rule out malignancy or pregnancy in the event of breakthrough bleeding, as in the case of any abnormal vaginal bleeding. If a pathologic basis has been excluded, time alone or a change to another formulation may solve the problem. In the event of amenorrhea, pregnancy should be ruled out. Some women may encounter post-pill amenorrhea or oligomenorrhea, especially when such a condition was pre-existent.
RISK OF LIVER ENZYME ELEVATIONS WITH CONCOMITANT HEPATITIS C TREATMENT).
An increased risk of the following serious adverse reactions has been associated with the use of oral contraceptives (see
The use of oral contraceptives is associated with increased risk of several serious conditions including venous and arterial thromboembolism, thrombotic and hemorrhagic stroke, myocardial infarction, liver tumors or other liver lesions, and gallbladder disease. The risk of morbidity and mortality increases significantly in the presence of other risk factors such as hypertension, hyperlipidemia, obesity, and diabetes mellitus.
Practitioners prescribing oral contraceptives should be familiar with the following information relating to these and other risks.
The information contained herein is principally based on studies carried out in patients who used oral contraceptives with formulations containing higher amounts of estrogens and progestogens than those in common use today. The effect of long-term use of the oral contraceptives with lesser amounts of both estrogens and progestogens remains to be determined.
Throughout this labeling, epidemiological studies reported are of two types: retrospective case-control studies and prospective cohort studies. Case-control studies provide an estimate of the relative risk of a disease, which is defined as the
An increased risk of myocardial infarction has been associated with oral contraceptive use.2-21This increased risk is primarily in smokers or in women with other underlying risk factors for coronary artery disease such as hypertension, obesity, diabetes, and hypercholesterolemia. The relative risk for myocardial infarction in current oral contraceptive users has been estimated to be 2 to 6. The risk is very low under the age of 30. However, there is the possibility of a risk of cardiovascular disease even in very young women who take oral contraceptives.
Smoking in combination with oral contraceptive use has been reported to contribute substantially to the risk of myocardial infarction in women in their mid-thirties or older, with smoking accounting for the majority of excess cases.22Mortality rates associated with circulatory disease have been shown to increase substantially in smokers, especially in those 35 years of age and older among women who use oral contraceptives (see Figure 1, Table 2).
Adapted from Layde and Beral.14
Oral contraceptives may compound the effects of well-known cardiovascular risk factors such as hypertension, diabetes, hyperlipidemias, hypercholesterolemia, age, cigarette smoking, and obesity. In particular, some progestogens decrease HDL cholesterol23-31and cause glucose intolerance, while estrogens may create a state of hyperinsulinism.32Oral contraceptives have been shown to increase blood pressure among some users (see
An increased risk of thromboembolic and thrombotic disease associated with the use of oral contraceptives is well established.17,33-51Case-control studies have estimated the relative risk to be 3 for the first episode of superficial venous thrombosis, 4 to 11 for deep vein thrombosis or pulmonary embolism, and 1.5 to 6 for women with predisposing conditions for venous thromboembolic disease.34-37, 45, 46Cohort studies have shown the relative risk to be somewhat lower, about 3 for new cases (subjects with no past history of venous thrombosis or varicose veins) and about 4.5 for new cases requiring hospitalization.42, 47, 48The risk of venous thromboembolic disease associated with oral contraceptives is not related to duration of use.
A two- to seven-fold increase in relative risk of postoperative thromboembolic complications has been reported with the use of oral contraceptives.38, 39The relative risk of venous thrombosis in women who have predisposing conditions is about twice that of women without such medical conditions.43If feasible, oral contraceptives should be discontinued at least 4 weeks prior to and for 2 weeks after elective surgery of a type associated with an increased risk of thromboembolism, and also during and following prolonged immobilization. Since the immediate postpartum period is also associated with an increased risk of thromboembolism, oral contraceptives should be started no earlier than 4 to 6 weeks after delivery in women who elect not to breast feed.
Both the relative and attributable risks of cerebrovascular events (thrombotic and hemorrhagic strokes) have been reported to be increased with oral contraceptive use,14, 17, 18, 34, 42, 46, 52-59although, in general, the risk was greatest among older (over 35 years), hypertensive women who also smoked. Hypertension was reported to be a risk factor for both users and nonusers, for both types of strokes, while smoking increased the risk for hemorrhagic strokes.
In one large study,52the relative risk for thrombotic stroke was reported as 9.5 times greater in users than in nonusers. It ranged from 3 for normotensive users to 14 for users with severe hypertension.54The relative risk for hemorrhagic stroke was reported to be 1.2 for nonsmokers who used oral contraceptives, 1.9 to 2.6 for smokers who did not use oral contraceptives, 6.1 to 7.6 for smokers who used oral contraceptives, 1.8 for normotensive users, and 25.7 for users with severe hypertension. The risk is also greater in older women and among smokers.
A positive association has been reported between the amount of estrogen and progestogen in oral contraceptives and the risk of vascular disease.41, 43, 53, 59-64A decline in serum high density lipoproteins (HDL) has been reported with many progestogens.23-31A decline in serum high density lipoproteins has been associated with an increased incidence of ischemic heart disease.65Because estrogens increase HDL-cholesterol, the net effect of an oral contraceptive depends on the balance achieved between doses of estrogen and progestogen and the nature and absolute amount of progestogens used in the contraceptives. The amount of both steroids should be considered in the choice of an oral contraceptive.
Minimizing exposure to estrogen and progestogen is in keeping with good principles of therapeutics. For any particular estrogen-progestogen combination, the dosage regimen prescribed should be one that contains the least amount of estrogen and progestogen that is compatible with a low failure rate and the needs of the individual patient. New acceptors of oral contraceptives should be started on preparations containing the lowest estrogen content that produces satisfactory results in the individual.
Products containing 50 mcg estrogen should be used only when medically indicated.
There are three studies that have shown persistence of risk of vascular disease for users of oral contraceptives. In a study in the United States, the risk of developing myocardial infarction after discontinuing oral contraceptives persisted for at least 9 years for women 40 to 49 years old who had used oral contraceptives for 5 or more years, but this increased risk was not demonstrated in other age groups.16Another American study reported former use of oral contraceptives was significantly associated with increased risk of subarachnoid hemorrhage.57In another study, in Great Britain, the risk of developing nonrheumatic heart disease plus hypertension, subarachnoid hemorrhage, cerebral thrombosis, and transient ischemic attacks persisted for at least 6 years after discontinuation of oral contraceptives, although the excess risk was small.14, 18, 66It should be noted that these studies were performed with oral contraceptive formulations containing 50 mcg or more of estrogens.
One study67gathered data from a variety of sources that have estimated the mortality rates associated with different methods of contraception at different ages (Table 2). These estimates include the combined risk of death associated with contraceptive methods plus the risk attributable to pregnancy in the event of method failure. Each method of contraception has its specific benefits and risks. The study concluded that, with the exception of oral contraceptive users 35 and older who smoke and 40 or older who do not smoke, mortality associated with all methods of birth control is low and below that associated with childbirth. The observation of a possible increase in risk of mortality with age for oral contraceptive users is based on data gathered in the 1970's, but not reported until 1983.67However, current clinical practice involves the use of lower estrogen dose formulations combined with careful restriction of oral contraceptive use to women who do not have the various risk factors listed in this labeling.
Because of these changes in practice and, also, because of some limited new data that suggest that the risk of cardiovascular disease with the use of oral contraceptives may now be less than previously observed,48, 152the Fertility and Maternal Health Drugs Advisory Committee was asked to review the topic in 1989. The Committee concluded that, although cardiovascular disease risks may be increased with oral contraceptive use after age 40 in healthy nonsmoking women (even with the newer low-dose formulations), there are greater potential health risks associated with pregnancy in older women and with the alternative surgical and medical procedures that may be necessary if such women do not have access to effective and acceptable means of contraception.
Therefore, the Committee recommended that the benefits of oral contraceptive use by healthy nonsmoking women over 40 may outweigh the possible risks. Of course, older women, as all women who take oral contraceptives, should take the lowest possible dose formulation that is effective.
Age | ||||||
Method of control | 15 to 19 | 20 to 24 | 25 to 29 | 30 to 34 | 35 to 39 | 40 to 44 |
No fertility control methodsDeaths are birth-related | 7 | 7.4 | 9.1 | 14.8 | 25.7 | 28.2 |
Oral contraceptives | ||||||
nonsmokerDeaths are method-related | 0.3 | 0.5 | 0.9 | 1.9 | 13.8 | 31.6 |
smoker | 2.2 | 3.4 | 6.6 | 13.5 | 51.1 | 117.2 |
IUD | 0.8 | 0.8 | 1 | 1 | 1.4 | 1.4 |
Condom | 1.1 | 1.6 | 0.7 | 0.2 | 0.3 | 0.4 |
Diaphragm/Spermicide | 1.9 | 1.2 | 1.2 | 1.3 | 2.2 | 2.8 |
Periodic abstinence | 2.5 | 1.6 | 1.6 | 1.7 | 2.9 | 3.6 |
Adapted from Ory.
Ethynodiol diacetate and ethinyl estradiol tablets are contraindicated in females who currently have or have had breast cancer because breast cancer may be hormonally sensitive (see
Epidemiology studies have not found a consistent association between use of combined oral contraceptives (COCs) and breast cancer risk. Studies do not show an association between ever (current or past) use of COCs and risk of breast cancer. However, some studies report a small increase in the risk of breast cancer among current or recent users (<6 months since last use) and current users with longer duration of COC use (see
Some studies suggested that oral contraceptive use was associated with an increase in the risk of cervical intraepithelial neoplasia, dysplasia, erosion, carcinoma, or micro-glandular dysplasia in some populations of women.17, 50, 103-115However, there continues to be controversy about the extent to which such findings may be due to differences in sexual behavior and other factors.
In spite of many studies of the relationship between oral contraceptive use and breast and cervical cancers, a cause and effect relationship has not been established.
Benign hepatic adenomas and other hepatic lesions have been associated with oral contraceptive use,116-121although the incidence of such benign tumors is rare in the United States. Indirect calculations have estimated the attributable risk to be in the range of 3.3 cases per 100,000 for users, a risk that increases after 4 or more years of use.120Rupture of benign, hepatic adenomas or other lesions may cause death through intraabdominal hemorrhage. Therefore, such lesions should be considered in women presenting with abdominal pain and tenderness, abdominal mass, or shock. About one quarter of the cases presented because of abdominal masses; up to one half had signs and symptoms of acute intraperitoneal hemorrhage.121Diagnosis may prove difficult.
Studies from the U.S.,122, 150Great Britain,123, 124and Italy125have shown an increased risk of hepatocellular carcinoma in long-term (greater than 8 years; relative risk of 7 to 20) oral contraceptive users. However, these cancers are rare in the United States, and the attributable risk (the excess incidence) of liver cancers in oral contraceptive users approaches less than 1 per 1,000,000 users.
During clinical trials with the Hepatitis C combination drug regimen that contains ombitasvir/paritaprevir/ritonavir, with or without dasabuvir, ALT elevations greater than 5 times the upper limit of normal (ULN), including some cases greater than 20 times the ULN, were significantly more frequent in women using ethinyl estradiol-containing medications such as CHCs. Discontinue ethynodiol diacetate and ethinyl estradiol prior to starting therapy with the combination drug regimen ombitasvir/paritaprevir/ritonavir, with or without dasabuvir
There have been reports of retinal thrombosis and other ocular lesions associated with the use of oral contraceptives. Oral contraceptives should be discontinued if there is unexplained, gradual or sudden, partial or complete loss of vision; onset of proptosis or diplopia; papilledema; or any evidence of retinal vascular lesions. Appropriate diagnostic and therapeutic measures should be undertaken immediately.
Extensive epidemiological studies have revealed no increased risk of birth defects in women who have used oral contraceptives prior to pregnancy.126, 129The majority of recent studies also do not suggest a teratogenic effect, particularly insofar as cardiac anomalies and limb reduction defects are concerned,126, 129when the pill is taken inadvertently during early pregnancy.
The administration of oral contraceptives to induce withdrawal bleeding should not be used as a test for pregnancy. Oral contraceptives should not be used during pregnancy to treat threatened or habitual abortion. It is recommended that for any patient who has missed two consecutive periods, pregnancy should be ruled out before continuing oral contraceptive use. If the patient has not adhered to the prescribed schedule, the possibility of pregnancy should be considered at the time of the first missed period and further use of oral contraceptives should be withheld until pregnancy has been ruled out. Oral contraceptive use should be discontinued if pregnancy is confirmed.
Earlier studies reported an increased lifetime relative risk of gallbladder surgery in users of oral contraceptives and estrogens.40, 42, 53, 70More recent studies, however, have shown that the relative risk of developing gallbladder disease among oral contraceptive users may be minimal.130-132The recent findings of minimal risk may be related to the use of oral contraceptive formulations containing lower doses of estrogens and progestogens.
Oral contraceptives have been shown to cause a decrease in glucose tolerance in a significant percentage of users.32This effect has been shown to be directly related to estrogen dose.133Progestogens increase insulin secretion and create insulin resistance, the effect varying with different progestational agents.32, 134However, in the nondiabetic woman, oral contraceptives appear to have no effect on fasting blood glucose. Because of these demonstrated effects, prediabetic and diabetic women should be carefully observed while taking oral contraceptives.
Some women may have persistent hypertriglyceridemia while on the pill. As discussed earlier (see
An increase in blood pressure has been reported in women taking oral contraceptives50, 53, 137-139and this increase is more likely in older oral contraceptive users137and with extended duration of use.53Data from the Royal College of General Practitioners138and subsequent randomized trials have shown that the incidence of hypertension increases with increasing concentrations of progestogens.
Women with a history of hypertension or hypertension-related disease, or renal disease139should be encouraged to use another method of contraception. If such women elect to use oral contraceptives, they should be monitored closely and if significant elevation of blood pressure occurs, oral contraceptives should be discontinued. For most women, elevated blood pressure will return to normal after stopping oral contraceptives,137and there is no difference in the occurrence of hypertension among ever and never-users.140
The onset or exacerbation of migraine or the development of headache of a new pattern that is recurrent, persistent, or severe requires discontinuation of oral contraceptives and evaluation of the cause.
Breakthrough bleeding and spotting are sometimes encountered in patients on oral contraceptives, especially during the first three months of use. Nonhormonal causes should be considered and adequate diagnostic measures taken to rule out malignancy or pregnancy in the event of breakthrough bleeding, as in the case of any abnormal vaginal bleeding. If a pathologic basis has been excluded, time alone or a change to another formulation may solve the problem. In the event of amenorrhea, pregnancy should be ruled out. Some women may encounter post-pill amenorrhea or oligomenorrhea, especially when such a condition was pre-existent.
• Thrombophlebitis and thrombosis• Arterial thromboembolism• Pulmonary embolism• Myocardial infarction and coronary thrombosis• Cerebral hemorrhage• Cerebral thrombosis• Hypertension• Gallbladder disease• Benign and malignant liver tumors, and other hepatic lesions
There is evidence of an association between the following conditions and the use of oral contraceptives, although additional confirmatory studies are needed:
• Mesenteric thrombosis• Neuro-ocular lesions (e.g., retinal thrombosis and optic neuritis)
The following adverse reactions have been reported in patients receiving oral contraceptives and are believed to be drug-related:
• Nausea• Vomiting• Gastrointestinal symptoms (such as abdominal cramps and bloating)• Breakthrough bleeding• Spotting• Change in menstrual flow• Amenorrhea during or after use• Temporary infertility after discontinuation of use• Edema• Chloasma or melasma, which may persist• Breast changes: tenderness, enlargement, secretion• Change in weight (increase or decrease)• Change in cervical erosion or secretion• Diminution in lactation when given immediately postpartum• Cholestatic jaundice• Migraine• Rash (allergic)• Mental depression• Reduced tolerance to carbohydrates• Vaginal candidiasis• Change in corneal curvature (steepening)• Intolerance to contact lenses
The following adverse reactions or conditions have been reported in users of oral contraceptives and the association has been neither confirmed nor refuted:
• Premenstrual syndrome• Cataracts• Changes in appetite• Cystitis-like syndrome• Headache• Nervousness• Dizziness• Hirsutism• Loss of scalp hair• Erythema multiforme• Erythema nodosum• Hemorrhagic eruption• Vaginitis• Porphyria• Impaired renal function• Hemolytic uremic syndrome• Acne• Changes in libido• Colitis• Budd-Chiari syndrome• Endocervical hyperplasia or ectropion
Five studies that compared breast cancer risk between ever-users (current or past use) of COCs and never-users of COCs reported no association between ever use of COCs and breast cancer risk, with effect estimates ranging from 0.90 - 1.12 (Figure 2).
Three studies compared breast cancer risk between current or recent COC users (<6 months since last use) and never users of COCs (Figure 2). One of these studies reported no association between breast cancer risk and COC use. The other two studies found an increased relative risk of 1.19 - 1.33 with current or recent use. Both of these studies found an increased risk of breast cancer with current use of longer duration, with relative risks ranging from 1.03 with less than one year of COC use to approximately 1.4 with more than 8-10 years of COC use.
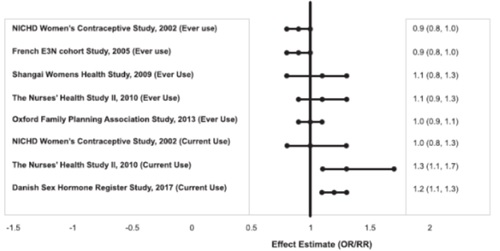
RR = relative risk; OR = odds ratio; HR = hazard ratio. “ever COC” are females with current or past COC use; “never COC use” are females that never used COCs.
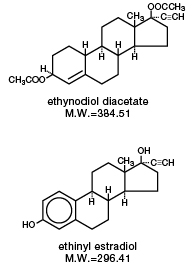
The chemical name for ethynodiol diacetate is 19-Nor-17α-pregn-4-en-20-yne-3β, 17-diol diacetate, and for ethinyl estradiol it is 19-Nor- 17α-pregna-1,3,5(10)-trien-20-yne-3, 17-diol.
The structural formulas are as follows:
Therapeutic class: Oral contraceptive.