Vancomycin Hydrochloride
Vancomycin Hydrochloride Prescribing Information
Vancomycin hydrochloride for injection is indicated for the treatment of serious or severe infections caused by susceptible strains of methicillin-resistant (β-lactam-resistant) staphylococci. It is indicated for penicillin-allergic patients, for patients who cannot receive or who have failed to respond to other drugs, including the penicillins or cephalosporins, and for infections caused by vancomycin-susceptible organisms that are resistant to other antimicrobial drugs. Vancomycin hydrochloride for injection is indicated for initial therapy when methicillin-resistant staphylococci are suspected, but after susceptibility data are available, therapy should be adjusted accordingly.
Vancomycin hydrochloride for injection is effective in the treatment of staphylococcal endocarditis. Its effectiveness has been documented in other infections due to staphylococci, including septicemia, bone infections, lower respiratory tract infections, skin and skin structure infections. When staphylococcal infections are localized and purulent, antibiotics are used as adjuncts to appropriate surgical measures.
Vancomycin hydrochloride for injection has been reported to be effective alone or in combination with an aminoglycoside for endocarditis caused by
Vancomycin hydrochloride for injection has been reported to be effective for the treatment of diphtheroid endocarditis. Vancomycin hydrochloride for injection has been used successfully in combination with either rifampin, an aminoglycoside, or both in early-onset prosthetic valve endocarditis caused by
Specimens for bacteriologic cultures should be obtained in order to isolate and identify causative organisms and to determine their susceptibilities to vancomycin.
To reduce the development of drug-resistant bacteria and maintain the effectiveness of vancomycin hydrochloride for injection and other antibacterial drugs, vancomycin hydrochloride for injection should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
The parenteral form of vancomycin hydrochloride may be administered orally for treatment of antibiotic-associated pseudomembranous colitis produced by
Infusion-related events are related to both the concentration and the rate of administration of vancomycin. Concentrations of no more than 5 mg/mL and rates of no more than 10 mg/min are recommended in adults (see also age-specific recommendations). In selected patients in need of fluid restriction, a concentration up to 10 mg/mL may be used; use of such higher concentrations may increase the risk of infusion-related events. An infusion rate of 10 mg/min or less is associated with fewer infusion-related events (see
During or soon after rapid infusion of vancomycin hydrochloride for injection, patients may develop anaphylactoid reactions, including hypotension (see
Systemic vancomycin exposure may result in acute kidney injury (AKI). The risk of AKI increases as systemic exposure/serum levels increase. Additional risk factors for AKI in patients receiving vancomycin include receipt of concomitant drugs known to be nephrotoxic, in patients with pre-existing renal impairment, or with co-morbidities that predispose to renal impairment. Interstitial nephritis has also been reported in patients receiving vancomycin.
Onset of pseudomembranous colitis symptoms may occur during or after antibiotic treatment (see
A few dozen cases of hearing loss associated with vancomycin have been reported. Most of these patients had kidney dysfunction or a preexisting hearing loss or were receiving concomitant treatment with an ototoxic drug. Vertigo, dizziness, and tinnitus have been reported rarely.
Reversible neutropenia, usually starting 1 week or more after onset of therapy with vancomycin or after a total dosage of more than 25 g, has been reported for several dozen patients.
Neutropenia appears to be promptly reversible when vancomycin is discontinued. Thrombocytopenia has rarely been reported. Although a causal relationship has not been established, reversible agranulocytosis (granulocytes <500/mm3) has been reported rarely.
Inflammation at the injection site has been reported.
Patients have been reported to have had anaphylaxis, drug fever, nausea, chills, eosinophilia, rashes including exfoliative dermatitis, Stevens-Johnson syndrome (see
Chemical peritonitis has been reported following intraperitoneal administration (see
The following adverse reactions have been identified during post-approval use of vancomycin. Because these reactions are reported voluntarily from a population of uncertain size, it is not possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Severe dermatologic reactions such as toxic epidermal necrolysis (TEN), drug reaction with eosinophilia and systemic symptoms (DRESS), acute generalized exanthematous pustulosis (AGEP), and linear IgA bullous dermatosis (LABD) (see
To report SUSPECTED ADVERSE EVENTS, contact FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
The use of ADD-Vantage vials of vancomycin hydrochloride is indicated only when doses of 500 mg, 750 mg or 1 g are appropriate. Patient factors, such as renal function and age, are critical in calculating correct dosage regimens (see below). If doses of 500 mg, 750 mg or 1 g are determined to be inappropriate, conventional vials of vancomycin hydrochloride should be used. ADD-VANTAGE VIALS OF VANCOMYCIN HYDROCHLORIDE SHOULD NOT BE USED IN NEONATES, INFANTS, OR PEDIATRIC PATIENTS WHO REQUIRE DOSES OF LESS THAN 500 MG.
Vancomycin hydrochloride for injection is contraindicated in patients with known hypersensitivity to this antibiotic.
During or soon after rapid infusion of vancomycin hydrochloride for injection, patients may develop anaphylactoid reactions, including hypotension (see
In animal studies, hypotension and bradycardia occurred in dogs receiving an intravenous infusion of vancomycin hydrochloride 25 mg/kg, at a concentration of 25 mg/mL and an infusion rate of 13.3 mL/min.
Concomitant administration of vancomycin and anesthetic agents has been associated with erythema and histamine-like flushing (see
In pediatric patients, it may be appropriate to confirm desired vancomycin serum concentrations. Concomitant administration of vancomycin and anesthetic agents has been associated with erythema and histamine-like flushing in pediatric patients (see
During or soon after rapid infusion of vancomycin hydrochloride for injection, patients may develop anaphylactoid reactions, including hypotension (see
Systemic vancomycin exposure may result in acute kidney injury (AKI). The risk of AKI increases as systemic exposure/serum levels increase. Additional risk factors for AKI in patients receiving vancomycin include receipt of concomitant drugs known to be nephrotoxic, in patients with pre-existing renal impairment, or with co-morbidities that predispose to renal impairment. Interstitial nephritis has also been reported in patients receiving vancomycin.
Onset of pseudomembranous colitis symptoms may occur during or after antibiotic treatment (see
A few dozen cases of hearing loss associated with vancomycin have been reported. Most of these patients had kidney dysfunction or a preexisting hearing loss or were receiving concomitant treatment with an ototoxic drug. Vertigo, dizziness, and tinnitus have been reported rarely.
Reversible neutropenia, usually starting 1 week or more after onset of therapy with vancomycin or after a total dosage of more than 25 g, has been reported for several dozen patients.
Neutropenia appears to be promptly reversible when vancomycin is discontinued. Thrombocytopenia has rarely been reported. Although a causal relationship has not been established, reversible agranulocytosis (granulocytes <500/mm3) has been reported rarely.
Inflammation at the injection site has been reported.
Patients have been reported to have had anaphylaxis, drug fever, nausea, chills, eosinophilia, rashes including exfoliative dermatitis, Stevens-Johnson syndrome (see
Chemical peritonitis has been reported following intraperitoneal administration (see
The following adverse reactions have been identified during post-approval use of vancomycin. Because these reactions are reported voluntarily from a population of uncertain size, it is not possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Severe dermatologic reactions such as toxic epidermal necrolysis (TEN), drug reaction with eosinophilia and systemic symptoms (DRESS), acute generalized exanthematous pustulosis (AGEP), and linear IgA bullous dermatosis (LABD) (see
To report SUSPECTED ADVERSE EVENTS, contact FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Monitor renal function in patients receiving vancomycin and concurrent and/or sequential systemic or topical use of other potentially neurotoxic and/or nephrotoxic drugs, such as amphotericin B, aminoglycosides, bacitracin, polymixin B, colistin, viomycin, or cisplatin.
Vancomycin hydrochloride for injection, USP is a lyophilized powder, for preparing intravenous (IV) infusions, in ADD-Vantage® vials each containing the equivalent of 500 mg, 750 mg or 1 g vancomycin base. 500 mg of the base are equivalent to 0.34 mmol, 750 mg of the base are equivalent to 0.51 mmol, and 1 g of the base are equivalent to 0.67 mmol. When reconstituted with Sterile Water for Injection to a concentration of 50 mg/mL, the pH of the solution is between 2.5 and 4.5. This product is oxygen sensitive. Vancomycin Hydrochloride for Injection, USP should be administered intravenously in diluted solution (see
Infusion-related events are related to both the concentration and the rate of administration of vancomycin. Concentrations of no more than 5 mg/mL and rates of no more than 10 mg/min are recommended in adults (see also age-specific recommendations). In selected patients in need of fluid restriction, a concentration up to 10 mg/mL may be used; use of such higher concentrations may increase the risk of infusion-related events. An infusion rate of 10 mg/min or less is associated with fewer infusion-related events (see
The use of ADD-Vantage vials of vancomycin hydrochloride is indicated only when doses of 500 mg, 750 mg or 1 g are appropriate. Patient factors, such as renal function and age, are critical in calculating correct dosage regimens (see below). If doses of 500 mg, 750 mg or 1 g are determined to be inappropriate, conventional vials of vancomycin hydrochloride should be used. ADD-VANTAGE VIALS OF VANCOMYCIN HYDROCHLORIDE SHOULD NOT BE USED IN NEONATES, INFANTS, OR PEDIATRIC PATIENTS WHO REQUIRE DOSES OF LESS THAN 500 MG.
The usual daily intravenous dose is 2 g divided either as 500 mg every 6 hours or 1 g every 12 hours. Each dose should be administered at no more than 10 mg/min or over a period of at least 60 minutes, whichever is longer. Other patient factors, such as age or obesity, may call for modification of the usual intravenous daily dose.
The usual intravenous dosage of vancomycin is 10 mg/kg per dose given every 6 hours. Each dose should be administered over a period of at least 60 minutes. Close monitoring of serum concentrations of vancomycin may be warranted in these patients.
In pediatric patients up to the age of 1 month, the total daily intravenous dosage may be lower. In neonates, an initial dose of 15 mg/kg is suggested, followed by 10 mg/kg every 12 hours for neonates in the 1st week of life and every 8 hours thereafter up to the age of 1 month. Each dose should be administered over 60 minutes. In premature infants, vancomycin clearance decreases as postconceptional age decreases. Therefore, longer dosing intervals may be necessary in premature infants. Close monitoring of serum concentrations of vancomycin is recommended in these patients.
Dosage adjustment must be made in patients with impaired renal function. In premature infants and the elderly, greater dosage reductions than expected may be necessary because of decreased renal function. Measurement of vancomycin serum concentrations can be helpful in optimizing therapy, especially in seriously ill patients with changing renal function. Vancomycin serum concentrations can be determined by use of microbiologic assay, radioimmunoassay, fluorescence polarization immunoassay, fluorescence immunoassay, or high-pressure liquid chromatography. If creatinine clearance can be measured or estimated accurately, the dosage for most patients with renal impairment can be calculated using the following table. The dosage of vancomycin hydrochloride for injection per day in mg is about 15 times the glomerular filtration rate in mL/min (see following table).
Creatinine Clearance mL/min | Vancomycin Dose mg/24 h |
|---|---|
100 | 1,545 |
90 | 1,390 |
80 | 1,235 |
70 | 1,080 |
60 | 925 |
50 | 770 |
40 | 620 |
30 | 465 |
20 | 310 |
10 | 155 |
The initial dose should be no less than 15 mg/kg, even in patients with mild to moderate renal insufficiency. The table is not valid for functionally anephric patients. For such patients, an initial dose of 15 mg/kg of body weight should be given to achieve prompt therapeutic serum concentrations. The dose required to maintain stable concentrations is 1.9 mg/kg/24 h. In patients with marked renal impairment, it may be more convenient to give maintenance doses of 250 to 1,000 mg once every several days rather than administering the drug on a daily basis. In anuria, a dose of 1,000 mg every 7 to 10 days has been recommended. When only serum creatinine is known, the following formula (based on sex, weight, and age of the patient) may be used to calculate creatinine clearance. Calculated creatinine clearances (mL/min) are only estimates. The creatinine clearance should be measured promptly.
Men: | [Weight (kg) × (140 – age in years)] | ||
72 × serum creatinine concentration (mg/dL) | |||
Women: | 0.85 × above value |
The serum creatinine must represent a steady state of renal function. Otherwise, the estimated value for creatinine clearance is not valid. Such a calculated clearance is an overestimate of actual clearance in patients with conditions: (1) characterized by decreasing renal function, such as shock, severe heart failure, or oliguria; (2) in which a normal relationship between muscle mass and total body weight is not present, such as in obese patients or those with liver disease, edema, or ascites; and (3) accompanied by debilitation, malnutrition, or inactivity. The safety and efficacy of vancomycin administration by the intrathecal (intralumbar or intraventricular) routes have not been established. Intermittent infusion is the recommended method of administration.
Vancomycin Hydrochloride ADD-Vantage vials should be used only with approved diluents (5% dextrose injection or 0.9% sodium chloride injection) (see
It has been shown that after reconstitution, the admixture solution prepared in either dextrose injection or sodium chloride injection may be stored for 24 hours at room temperature or in a refrigerator for 14 days without significant loss of potency. However, this information is not intended to suggest that it is acceptable practice to administer such an admixture well after the time of preparation. Admixtures should be prepared as close to the time of administration as is reasonable.
Intermittent infusion is the recommended method of administration.
The 500 mg ADD-Vantage vial should be joined with at least a 100 mL ADD-Vantage flexible diluent container, the 750 mg and the 1 g ADD-Vantage vial should be joined
Solutions that are diluted with 5% Dextrose Injection or 0.9% Sodium Chloride Injection may be stored in a refrigerator for 14 days without significant loss of potency.
Vancomycin solution has a low pH and may cause physical instability when it is mixed with other compounds.
Mixtures of solutions of vancomycin and beta-lactam antibiotics have been shown to be physically incompatible. The likelihood of precipitation increases with higher concentrations of vancomycin. It is recommended to adequately flush the intravenous lines between the administration of these antibiotics. It is also recommended to dilute solutions of vancomycin to 5 mg/mL or less.
Although intravitreal injection is not an approved route of administration for vancomycin, precipitation has been reported after intravitreal injection of vancomycin and ceftazidime for endophthalmitis using different syringes and needles. The precipitates dissolved gradually, with complete clearing of the vitreous cavity over two months and with improvement of visual acuity.
Parenteral drug products should be visually inspected for particulate matter and discoloration prior to administration, whenever solution or container permits.
Oral vancomycin is used in treating antibiotic-associated pseudomembranous colitis caused by
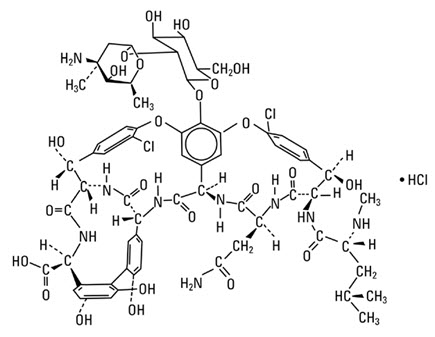
Vancomycin is a tricyclic glycopeptide antibiotic derived from
The solutions contain no bacteriostat, antimicrobial agent (except vancomycin) or buffer and are intended for use only as a single-dose injection only with the ADD-Vantage Flexible Diluent Container.