Vivacaine - Bupivacaine Hydrochloride And Epinephrine Bitartrate injection, Solution
(Bupivacaine Hydrochloride And Epinephrine Bitartrate)Vivacaine - Bupivacaine Hydrochloride And Epinephrine Bitartrate injection, Solution Prescribing Information
Vivacaine® (bupivacaine hydrochloride and epinephrine injection, USP) is indicated for the production of local anesthesia for dental procedures by infiltration injection or nerve block in adults.
Vivacaine® is not recommended for children.
As with all local anesthetics, the dosage varies and depends upon the area to be anesthetized, the vascularity of the tissues, the number of neuronal segments to be blocked, individual tolerance, and the technique of anesthesia. The lowest dosage needed to provide effective anesthesia should be administered. For specific techniques and procedures, refer to standard textbooks.
The 0.5% concentration with epinephrine is recommended for infiltration and block injection in the maxillary and mandibular area when a longer duration of local anesthetic action is desired, such as for oral surgical procedures generally associated with significant postoperative pain. The average dose of 1.8 mL (9 mg) per injection site will usually suffice; an occasional second dose of 1.8 mL (9 mg) may be used if necessary to produce adequate anesthesia after making allowance for 2 to 10 minutes onset time (see
Bupivacaine stabilizes the neuronal membrane and prevents the initiation and transmission of nerve impulses, thereby effecting local anesthesia.
The onset of action following dental injections is usually 2 to 10 minutes and anesthesia may last two or three times longer than lidocaine and mepivacaine for dental use, in many patients up to 7 hours. The duration of anesthetic effect is prolonged by the addition of epinephrine 1:200,000.
It has also been noted that there is a period of analgesia that persists after the return of sensation, during which time the need for strong analgesic is reduced.
After injection of bupivacaine for caudal, epidural or peripheral nerve block in man, peak levels of bupivacaine in the blood are reached in 30 to 45 minutes, followed by a decline to insignificant levels during the next three to six hours. Because of its amide structure, bupivacaine is not detoxified by plasma esterases but is detoxified, via conjugation with glucuronic acid, in the liver. When administered in recommended doses and concentrations, bupivacaine does not ordinarily produce irritation or tissue damage.
Systemic absorption of local anesthetics produces effects on the cardiovascular and central nervous systems (CNS). At blood concentrations achieved with normal therapeutic doses, changes in cardiac conduction, excitability, refractoriness, contractility, and peripheral vascular resistance are minimal. However, toxic blood concentrations depress cardiac conduction and excitability, which may lead to atrioventricular block, ventricular arrhythmias, and cardiac arrest, sometimes resulting in fatalities. In addition, myocardial contractility is depressed and peripheral vasodilation occurs, leading to decreased cardiac output and arterial blood pressure. Recent clinical reports and animal research suggest that these cardiovascular changes are more likely to occur after unintended intravascular injection of bupivacaine. Therefore, incremental dosing is necessary.
Following systemic absorption, local anesthetics can produce central nervous system stimulation, depression, or both. Apparent central stimulation is manifested as restlessness, tremors and shivering progressing to convulsions, followed by depression and coma progressing ultimately to respiratory arrest. However, the local anesthetics have a primary depressant effect on the medulla and on higher centers. The depressed stage may occur without a prior excited state.
Parental drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. Discard unused portion.
Vivacaine® (bupivacaine hydrochloride and epinephrine injection, USP) is contraindicated in patients with a known hypersensitivity to it or to any local anesthetic agent of the amide type or to other components of bupivacaine solutions.
Reactions to Vivacaine® (bupivacaine hydrochloride and epinephrine injection, USP) are characteristic of those associated with other amide-type local anesthetics. A major cause of adverse reactions to this group of drugs is excessive plasma levels, which may be due to overdosage, inadvertent intravascular injection or slow metabolic degradation.
Excessive plasma levels of the amide-type local anesthetics cause systemic reactions involving the central nervous system and the cardiovascular system. The
See
LOCAL ANESTHETICS SHOULD BE EMPLOYED ONLY BY CLINICIANS WHO ARE WELL VERSED IN DIAGNOSIS AND MANAGEMENT OF DOSE-RELATED TOXICITY AND OTHER ACUTE EMERGENCIES WHICH MIGHT ARISE FROM THE BLOCK TO BE EMPLOYED, AND THEN ONLY AFTER ENSURING THE
Small doses of local anesthetics injected into the head and neck area, as small as nine to eighteen milligrams, may produce adverse reactions similar to systemic toxicity seen with unintentional intravascular injections of larger doses. Confusion, convulsions, respiratory depression, and/or respiratory arrest, cardiovascular stimulation or depression and cardiac arrest have been reported. Reactions resulting in fatalities have occurred on rare occasions. In a few cases, resuscitation has been difficult or impossible despite apparently adequate preparation and appropriate management. These reactions may be due to intra-arterial injection of the local anesthetic with retrograde flow to the cerebral circulation. Patients receiving these blocks should have their circulation and respiration monitored and be constantly observed. Resuscitative equipment and personnel for treating adverse reactions should be immediately available. Dosage recommendations should not be exceeded (see
It is essential that aspiration for blood or cerebrospinal fluid (where applicable) be done prior to injecting any local anesthetic, both the original dose and all subsequent doses, to avoid intravascular injection. However, a negative aspiration does
Reactions resulting in fatality have occurred on rare occasions with the use of local anesthetics, even in the absence of a history of hypersensitivity.
This solution, which contains a vasoconstrictor, should be used with extreme caution for patients whose medical history and physical evaluation suggest the existence of hypertension, arteriosclerotic heart disease, cerebral vascular insufficiency, heart block, thyrotoxicosis and diabetes, etc., as well as patients receiving drugs likely to produce alterations in blood pressure.
Signs of methemoglobinemia may occur immediately or may be delayed some hours after exposure, and are characterized by a cyanotic skin discoloration and/or abnormal coloration of the blood. Methemoglobin levels may continue to rise; therefore, immediate treatment is required to avert more serious central nervous system and cardiovascular adverse effects, including seizures, coma, arrhythmias, and death. Discontinue Vivacaine® and any other oxidizing agents. Depending on the severity of the signs and symptoms, patients may respond to supportive care, i.e., oxygen therapy, hydration. A more severe clinical presentation may require treatment with methylene blue, exchange transfusion, or hyperbaric oxygen.
Bupivacaine with epinephrine 1:200,000 or other vasopressors should not be used concomitantly with ergot-type oxytocic drugs, because a severe persistent hypertension may occur. Likewise, solutions of bupivacaine containing a vasoconstrictor, such as epinephrine, should be used with extreme caution in patients receiving monoamine oxidase inhibitors (MAOI) or antidepressants of the triptyline or imipramine types, because severe prolonged hypertension may result.
Until further experience is gained in children younger than 12 years, administration of bupivacaine in this age group is not recommended.
Contains sodium metabisulfite, a sulfite that may cause allergic-type reactions including anaphylactic symptoms and life-threatening or less severe asthmatic episodes in certain susceptible people. The overall prevalence of sulfite sensitivity in the general population is unknown and probably low. Sulfite sensitivity is seen more frequently in asthmatic than in nonasthmatic people.
If sedatives are employed to reduce patient apprehension, use reduced doses, since local anesthetic agents, like sedatives, are central nervous system depressants which in combination may have an additive effect.
Vivacaine® (bupivacaine hydrochloride and epinephrine injection, USP) should be used cautiously in persons with known drug allergies or sensitivities, particularly to the amide-type local anesthetics.
Serious dose-related cardiac arrhythmias may occur if preparations containing a vasoconstrictor such as epinephrine are employed in patients during or following the administration of chloroform, halothane, cyclopropane, trichloroethylene, or other related agents. In deciding whether to use these products concurrently in the same patient, the combined action of both agents upon the myocardium, the concentration and volume of vasoconstrictor used, and the time since injection, when applicable, should be taken into account.
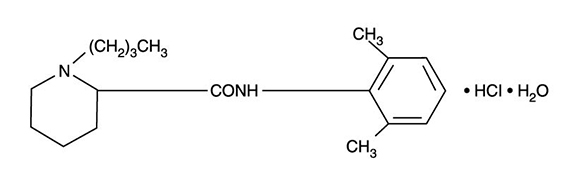
Bupivacaine hydrochloride is (±) -1-Butyl-2´, 6´-pipecoloxylidide monohydrochloride, monohydrate, a white crystalline powder that is freely soluble in 95 percent ethanol, soluble in water, and slightly soluble in chloroform or acetone. It has the following structural formula:
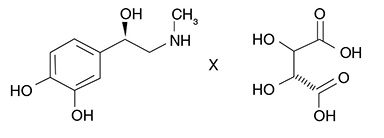
Epinephrine bitartrate is (-)-1-(3,4-Dihydroxyphenyl)-2-methylamino-ethanol (+) tartrate (1:1) salt. It has the following structural formula:
Bupivacaine is available in a sterile isotonic solution with epinephrine 1:200,000 (as bitartrate). Solutions of bupivacaine containing epinephrine may not be autoclaved.
Bupivacaine is related chemically and pharmacologically to the aminoacyl local anesthetics. It is a homologue of mepivacaine and is chemically related to lidocaine. All three of these anesthetics contain an amide linkage between the aromatic nucleus and the amino or piperidine group. They differ in this respect from the procaine-type local anesthetics, which have an ester linkage.