Gadoterate Meglumine - Gadoterate Meglumine injection prescribing information
WARNING: RISK ASSOCIATED WITH INTRATHECAL USE and NEPHROGENIC SYSTEMIC FIBROSIS
Risk Associated with Intrathecal Use
Intrathecal administration of gadolinium-based contrast agents (GBCAs) can cause serious adverse
reactions including death, coma, encephalopathy, and seizures. Gadoterate Meglumine Injection is not approved for intrathecal use [see Warnings and Precautions (5.1 )].
Nephrogenic Systemic Fibrosis
GBCAs increase the risk for nephrogenic systemic fibrosis (NSF) among patients with impaired elimination of the drugs. Avoid use of Gadoterate Meglumine Injection in these patients unless the diagnostic information is essential and not available with non-contrasted MRI or other modalities. NSF may result in fatal or debilitating fibrosis affecting the skin, muscle and internal organs.
The risk for NSF appears highest among patients with:
- Chronic, severe kidney disease (GFR < 30 mL/min/1.73 m 2 ), or
- Acute kidney injury.
Screen patients for acute kidney injury and other conditions that may reduce renal function. For patients at risk for chronically reduced renal function (e.g. age > 60 years, hypertension, diabetes), estimate the glomerular filtration rate (GFR) through laboratory testing (5.1 ).
For patients at highest risk for NSF, do not exceed the recommended Gadoterate Meglumine Injection dose and allow a sufficient period of time for elimination of the drug from the body prior to any re-administration [see Warnings and Precautions (5.2 )] .
INDICATIONS AND USAGE
Gadoterate Meglumine Injection is a gadolinium-based contrast agent indicated for intravenous use with magnetic resonance imaging (MRI) in brain (intracranial), spine and associated tissues in adult and pediatric patients (including term neonates) to detect and visualize areas with disruption of the blood brain barrier (BBB) and/or abnormal vascularity.
DOSAGE AND ADMINISTRATION
Adult and pediatric patients: The recommended dose of Gadoterate Meglumine Injection is 0.2 mL/kg (0.1 mmol/kg) body weight administered as an intravenous bolus injection at a flow rate of approximately 2 mL/second for adults and 1-2 mL/second for pediatric patients (including term neonates). The dose is delivered by manual or power injection. (2 )
Dosing Guidelines
For adult and pediatric patients (including term neonates), the recommended dose of Gadoterate Meglumine Injection is 0.2 mL/kg (0.1 mmol/kg) body weight administered as an intravenous bolus injection, manually or by power injector, at a flow rate of approximately 2 mL/second for adults and 1-2 mL/second for pediatric patients. Table 1 provides weight-adjusted dose volumes.
Body Weight | Volume | |
Pounds (lb) | Kilograms (kg) | Milliliters (mL) |
5.5 | 2.5 | 0.5 |
11 | 5 | 1 |
22 | 10 | 2 |
44 | 20 | 4 |
66 | 30 | 6 |
88 | 40 | 8 |
110 | 50 | 10 |
132 | 60 | 12 |
154 | 70 | 14 |
176 | 80 | 16 |
198 | 90 | 18 |
220 | 100 | 20 |
242 | 110 | 22 |
264 | 120 | 24 |
286 | 130 | 26 |
308 | 140 | 28 |
330 | 150 | 30 |
To ensure complete injection of Gadoterate Meglumine the injection may be followed by normal saline flush. Contrast MRI can begin immediately following Gadoterate Meglumine Injection.
Drug Handling
- Visually inspect Gadoterate Meglumine Injection for particulate matter prior to administration. Do not use the solution if particulate matter is present or if the container appears damaged. Gadoterate Meglumine Injection should be a clear, colorless to yellow solution.
- Do not mix with other drugs or parenteral nutrition.
- Discard any unused portions of the drug.
Directions for Use of the Gadoterate Meglumine Injection
Glass vial:
Aseptically draw up the contrast medium into a disposable syringe and use immediately.
DOSAGE FORMS AND STRENGTHS
Gadoterate Meglumine Injection, USP 0.5 mmol/mL is a sterile, clear, colorless to yellow, aqueous solution for intravenous injection containing 376.9 mg/mL gadoterate meglumine and is available in vials.
USE IN SPECIFIC POPULATIONS
- Pregnancy: Use only if imaging is essential during pregnancy and cannot be delayed. (8.1 )
Pregnancy
Risk Summary
GBCAs cross the human placenta and result in fetal exposure and gadolinium retention. The human data on the association between GBCAs and adverse fetal outcomes are limited and inconclusive (see Data ) . In animal reproduction studies, there were no adverse developmental effects observed in rats or rabbits with intravenous administration of gadoterate meglumine during organogenesis at doses up to 16 and 10 times, respectively, the recommended human dose (see Data ) . Because of the potential risks of gadolinium to the fetus, use Gadoterate Meglumine Injection only if imaging is essential during pregnancy and cannot be delayed.
The estimated background risk of major birth defects and miscarriage for the indicated population(s) are unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2-4% and 15-20% respectively.
Data
Human Data
Contrast enhancement is visualized in the placenta and fetal tissues after maternal GBCA administration.
Cohort studies and case reports on exposure to GBCAs during pregnancy have not reported a clear association between GBCAs and adverse effects in the exposed neonates. However, a retrospective cohort study, comparing pregnant women who had a GBCA MRI to pregnant women who did not have an MRI, reported a higher occurrence of stillbirths and neonatal deaths in the group receiving GBCA MRI. Limitations of this study include a lack of comparison with non-contrast MRI and lack of information about the material indication for MRI. Overall, these data preclude a reliable evaluation of the potential risk of adverse fetal outcomes with the use of GBCAs in pregnancy.
Animal Data
Gadolinium Retention
GBCAs administered to pregnant non-human primates (0.1 mmol/kg on gestational days 85 and 135) result in measurable gadolinium concentration in the offspring in bone, brain, skin, liver, kidney, and spleen for at least 7 months. GBCAs administered to pregnant mice (2 mmol/kg daily on gestational days 16 through 19) result in measurable gadolinium concentrations in the pups in bone, brain, kidney, liver, blood, muscle, and spleen at one month postnatal age.
Reproductive Toxicology
Gadoterate meglumine was administered in intravenous doses of 0, 2, 4 and 10 mmol/kg/day [3, 7 and 16 times the recommended human dose (RHD) based on body surface area (BSA)] to female rats for 14 days before mating, throughout the mating period and until gestation day (GD) 17. Pregnant rabbits were administered gadoterate meglumine in intravenous doses of 0, 1, 3 and 7 mmol/kg/day (3, 10 and 23 times the RHD based on BSA) from GD6 to GD19. No effects on embryo-fetal development were observed at doses up to 10 mmol/kg/day in rats and 3 mmol/kg/day in rabbits. Maternal toxicity was observed in rats at 10 mmol/kg/day and in rabbits at 7 mmol/kg/day. This maternal toxicity was characterized in rats by a slightly lower litter size and gravid uterus weight compared to the control group, and in rabbits by a reduction in body weight and food consumption.
Lactation
Risk Summary
There are no data on the presence of gadoterate in human milk, the effects on the breastfed infant, or the effects on milk production. However, published lactation data on other GBCAs indicate that 0.01 to 0.04% of the maternal gadolinium dose is excreted in breast milk. Additionally, there is limited GBCA gastrointestinal absorption in the breast-fed infant. Gadoterate is present in goat milk (see Data ) . The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for Gadoterate Meglumine Injection and any potential adverse effects on the breastfed infant from Gadoterate Meglumine Injection or from the underlying maternal condition.
Data
Nonclinical data demonstrate that gadoterate is detected in goat milk in amounts < 0.1% of the dose intravenously administered. Furthermore, in rats, absorption of gadoterate via the gastrointestinal tract is poor (1.2% of the administered dose was absorbed and eliminated in urine).
Pediatric Use
The safety and efficacy of Gadoterate Meglumine Injection at a single dose of 0.1 mmol/kg have been established in pediatric patients from birth (term neonates ≥ 37 weeks gestational age) to 17 years of age based on clinical data in 133 pediatric patients 2 years of age and older, and clinical data in 52 pediatric patients birth to less than 2 years of age that supported extrapolation from adult data [see Clinical Studies (14 )] . Adverse reactions in pediatric patients were similar to those reported in adults [see Adverse Reactions (6.1 )] . No dosage adjustment according to age is necessary in pediatric patients [see Dosage and Administration (2.1 ), Pharmacokinetics (12.3 )] . The safety of Gadoterate Meglumine Injection has not been established in preterm neonates.
No cases of NSF associated with Gadoterate Meglumine Injection or any other GBCA have been identified in pediatric patients age 6 years and younger [see Warnings and Precautions (5.2 )] . Normal estimated GFR (eGFR) is approximately 30 mL/minute/1.73 m 2 at birth and increases to adult values by 2 years of age.
Juvenile Animal Data
Single and repeat-dose toxicity studies in neonatal and juvenile rats did not reveal findings suggestive of a specific risk for use in pediatric patients including term neonates and infants.
Geriatric Use
In clinical studies of Gadoterate Meglumine Injection, 900 patients were 65 years of age and over, and 304 patients were 75 years of age and over. No overall differences in safety or efficacy were observed between these subjects and younger subjects. In general, use of Gadoterate Meglumine Injection in elderly patients should be cautious, reflecting the greater frequency of impaired renal function and concomitant disease or other drug therapy. No age-related dosage adjustment is necessary.
Renal Impairment
CONTRAINDICATIONS
History of clinically important hypersensitivity reactions to Gadoterate Meglumine Injection [see Warnings and Precautions (5.3 )] .
WARNINGS AND PRECAUTIONS
- Hypersensitivity: Anaphylactoid/anaphylactic reactions with cardiovascular, respiratory or cutaneous manifestations, ranging from mild to severe, including death, have uncommonly occurred. Monitor patients closely for need of emergency cardiorespiratory support. (5.3 )
- Gadolinium is retained for months or years in brain, bone, and other organs. (5.4 )
Risk Associated with Intrathecal Use
Intrathecal administration of GBCAs can cause serious adverse reactions including death, coma, encephalopathy, and seizures. The safety and effectiveness of Gadoterate Meglumine Injection have not been established with intrathecal use. Gadoterate Meglumine Injection is not approved for intrathecal use [see Dosage and Administration (2.1 )] .
Nephrogenic Systemic Fibrosis
GBCAs increase the risk for nephrogenic systemic fibrosis (NSF) among patients with impaired elimination of the drugs. Avoid use of gadoterate meglumine injection among these patients unless the diagnostic information is essential and not available with non-contrast MRI or other modalities. The GBCA-associated NSF risk appears highest for patients with chronic, severe kidney disease (GFR < 30 mL/min/1.73 m 2 ) as well as patients with acute kidney injury. The risk appears lower for patients with chronic, moderate kidney disease (GFR 30 - 59 mL/min/1.73 m 2 ) and little, if any, for patients with chronic, mild kidney disease (GFR 60 - 89 mL/min/1.73 m 2 ). NSF may result in fatal or debilitating fibrosis affecting the skin, muscle and internal organs. Report any diagnosis of NSF following Gadoterate Meglumine Injection administration to Slate Run Pharmaceuticals, LLC at 1-888-341-9214 or FDA (1-800-FDA-1088 or www.fda.gov/medwatch).
Screen patients for acute kidney injury and other conditions that may reduce renal function. Features of acute kidney injury consist of rapid (over hours to days) and usually reversible decrease in kidney function, commonly in the setting of surgery, severe infection, injury or drug-induced kidney toxicity. Serum creatinine levels and estimated GFR may not reliably assess renal function in the setting of acute kidney injury. For patients at risk for chronically reduced renal function (e.g., age > 60 years, diabetes mellitus or chronic hypertension), estimate the GFR through laboratory testing.
The factors that may increase the risk for NSF are repeated or higher than recommended doses of a GBCA and the degree of renal impairment at the time of exposure. Record the specific GBCA and the dose administered to a patient. For patients at highest risk for NSF, do not exceed the recommended Gadoterate Meglumine Injection dose and allow a sufficient period of time for elimination of the drug prior to re-administration. For patients receiving hemodialysis, physicians may consider the prompt initiation of hemodialysis following the administration of a GBCA in order to enhance the contrast agent’s elimination. The usefulness of hemodialysis in the prevention of NSF is unknown [see Dosage and Administration (2 ) and Clinical Pharmacology (12 )] .
Hypersensitivity Reactions
Anaphylactic and anaphylactoid reactions have been reported with Gadoterate Meglumine Injection, involving cardiovascular, respiratory, and/or cutaneous manifestations. Some patients experienced circulatory collapse and died. In most cases, initial symptoms occurred within minutes of Gadoterate Meglumine Injection administration and resolved with prompt emergency treatment [see Adverse Reactions (6 )] .
- Before Gadoterate Meglumine Injection administration, assess all patients for any history of a reaction to contrast media, bronchial asthma and/or allergic disorders. These patients may have an increased risk for a hypersensitivity reaction to Gadoterate Meglumine Injection.
- Administer Gadoterate Meglumine Injection only in situations where trained personnel and therapies are promptly available for the treatment of hypersensitivity reactions, including personnel trained in resuscitation.
- During and following Gadoterate Meglumine Injection administration, observe patients for signs and symptoms of hypersensitivity reactions.
Gadolinium Retention
Gadolinium is retained for months or years in several organs. The highest concentrations (nanomoles per gram of tissue) have been identified in the bone, followed by other organs (e.g. brain, skin, kidney, liver and spleen). The duration of retention also varies by tissue and is longest in bone. Linear GBCAs cause more retention than macrocyclic GBCAs. At equivalent doses, gadolinium retention varies among the linear agents with Omniscan (gadodiamide) and Optimark (gadoversetamide) causing greater retention than other linear agents [Eovist (gadoxetate disodium), Magnevist (gadopentetate dimeglumine), MultiHance (gadobenate dimeglumine)]. Retention is lowest and similar among the macrocyclic GBCAs [Dotarem (gadoterate meglumine), Gadavist (gadobutrol), ProHance (gadoteridol)].
Consequences of gadolinium retention in the brain have not been established. Pathologic and clinical consequences of GBCA administration and retention in skin and other organs have been established in patients with impaired renal function [see Warnings and Precautions (5.2 )] . There are rare reports of pathologic skin changes in patients with normal renal function. Adverse events involving multiple organ systems have been reported in patients with normal renal function without an established causal link to gadolinium retention [see Adverse Reactions (6.2 )] .
While clinical consequences of gadolinium retention have not been established in patients with normal renal function, certain patients might be at higher risk. These include patients requiring multiple lifetime doses, pregnant and pediatric patients, and patients with inflammatory conditions. Consider the retention characteristics of the agent when choosing a GBCA for these patients. Minimize repetitive GBCA imaging studies, particularly closely spaced studies when possible.
Acute Kidney Injury
In patients with chronically reduced renal function, acute kidney injury requiring dialysis has occurred with the use of GBCAs. The risk of acute kidney injury may increase with increasing dose of the contrast agent; administer the lowest dose necessary for adequate imaging. Screen all patients for renal impairment by obtaining a history and/or laboratory tests. Consider follow-up renal function assessments for patients with a history of renal dysfunction.
Extravasation and Injection Site Reactions
Ensure catheter and venous patency before the injection of Gadoterate Meglumine Injection. Extravasation into tissues during Gadoterate Meglumine Injection administration may result in tissue irritation [see Nonclinical Toxicology (13.2 )] .
ADVERSE REACTIONS
The following clinically significant adverse reactions are described elsewhere in the labeling:
Nephrogenic systemic fibrosis [see Warnings and Precautions (5.2 )] .
Hypersensitivity reactions [see Warnings and Precautions (5.3 )].
Gadolinium Retention [see Warnings and Precautions (5.4 )] .
Clinical Studies Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
The data described below reflect Gadoterate Meglumine Injection exposure in 2867 patients, representing 2682 adults and 185 pediatric patients. Overall, 55% of the patients were men. In clinical trials where ethnicity was recorded, the ethnic distribution was 81% Caucasian, 11% Asian, 4% Black, and 4% others. The average age was 53 years (range from < 1 week to 97 years).
Overall, 4% of patients reported at least one adverse reaction, primarily occurring immediately or within 24 hours following Gadoterate Meglumine Injection administration. Most adverse reactions were mild or moderate in severity and transient in nature.
Table 2 lists adverse reactions that occurred in ≥ 0.2% patients who received Gadoterate Meglumine Injection.
Reaction | Rate (%) n=2867 |
Nausea | 0.6% |
Headache | 0.4% |
Injection Site Pain | 0.4% |
Injection Site Coldness | 0.2% |
Rash | 0.2% |
Adverse reactions that occurred with a frequency < 0.2% in patients who received Gadoterate Meglumine Injection include: feeling cold, feeling hot, burning sensation, somnolence, pain, dizziness, dysgeusia, blood creatinine increased, hypotension, hypertension, asthenia, fatigue, injection site reactions (inflammation, extravasation, pruritus, swelling, warmth), paresthesia, pruritus, laryngeal discomfort, pain in extremity, vomiting, anxiety and palpitations.
Adverse Reactions in Pediatric Patients
During clinical trials, 185 pediatric patients (52 aged < 24 months, 33 aged 2 - 5 years, 57 aged 6 – 11 years and 43 aged 12 - 17 years) received Gadoterate Meglumine Injection. Overall, 7 pediatric patients (3.8%) reported at least one adverse reaction following Gadoterate Meglumine Injection administration. The most frequently reported adverse reaction was headache (1.1%). Most adverse events were mild in intensity and transient in nature.
Post-Marketing Experience
The following additional adverse reactions have been identified during postmarketing use of Gadoterate Meglumine Injection. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
System Organ Class | Adverse Reaction |
Cardiac Disorders | bradycardia, tachycardia, arrhythmia |
Immune System Disorders | hypersensitivity/anaphylactoid reactions including cardiac arrest, respiratory arrest, cyanosis, pharyngeal edema, laryngospasm, bronchospasm, angioedema, conjunctivitis, ocular hyperemia, eyelid edema, lacrimation increased, hyperhidrosis, urticaria |
Nervous System Disorders | coma, convulsion, syncope, presyncope, parosmia, tremor |
Musculoskeletal and Connective Tissue Disorders | muscle contracture, muscle weakness |
Gastrointestinal Disorders | diarrhea, salivary hypersecretion, acute pancreatitis with onset within 48 hours after GBCA administration |
General Disorders and Administration Site Conditions | malaise, fever Adverse events with variable onset and duration have been reported after GBCA administration [see Warnings and Precautions (5.4 )] . These include fatigue, asthenia, pain syndromes, and heterogeneous clusters of symptoms in the neurological, cutaneous, and musculoskeletal systems. |
Respiratory, Thoracic and Mediastinal Disorders | Acute respiratory distress syndrome, pulmonary edema |
Skin and Subcutaneous Tissue Disorders | NSF, in patients whose reports were confounded by the receipt of other GBCAs or in situations where receipt of other GBCAs could not be ruled out. No unconfounded cases of NSF have been reported with Gadoterate Meglumine Injection. Gadolinium-associated plaques |
Vascular Disorders | superficial phlebitis |
DRUG INTERACTIONS
Gadoterate does not interfere with serum and plasma calcium measurements determined by colorimetric assays. Specific drug interaction studies with Gadoterate Meglumine Injection have not been conducted.
DESCRIPTION
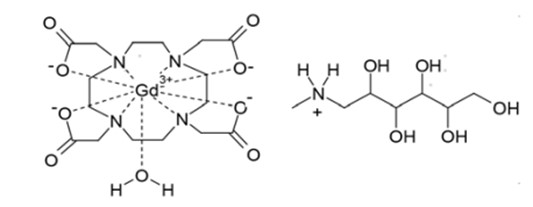
Gadoterate Meglumine Injection, USP is a paramagnetic macrocyclic ionic contrast agent administered for magnetic resonance imaging. The chemical name for gadoterate meglumine is D-glucitol, 1-deoxy-1-(methylamino)-,[1,4,7,10-tetraazacyclododecane-1,4,7,10-tetraaceto(4-)-.kappa.N1, .kappa.N4, .kappa.N7, .kappa.N10, .kappa.O1, .kappa.O4, .kappa.O7, .kappa.O10]gadolinate(1-)(1:1); it has a formula weight of 753.9 g/mol and empirical formula of C 23 H 42 O 13 N 5 Gd (anhydrous basis).
The structural formula of gadoterate meglumine in solution is as follows:
CAS Registry No. 92943-93-6
Gadoterate Meglumine Injection, USP is a sterile, nonpyrogenic, clear, colorless to yellow, aqueous solution of 0.5 mmol/mL of gadoterate meglumine, for intravenous use. No preservative is added. Each mL of Gadoterate Meglumine Injection, USP contains 376.9 mg of gadoterate meglumine, 0.25 mg of DOTA and water for injection. Gadoterate Meglumine Injection, USP has a pH of 6.5 to 8.0.
The main physiochemical properties of Gadoterate Meglumine Injection, USP are provided below:
Parameter | Value |
Density @ 20°C | 1.1753 g/cm 3 |
Viscosity @ 20°C | 3.4 mPa·s |
Viscosity @ 37°C | 2.4 mPa·s |
Osmolality | 1350 mOsm/kg water |
The thermodynamic stability constants for gadoterate (log K therm and log K cond at pH 7.4) are 25.6 and 19.3, respectively.
CLINICAL PHARMACOLOGY
Mechanism of Action
Gadoterate is a paramagnetic molecule that develops a magnetic moment when placed in a magnetic field. The magnetic moment enhances the relaxation rates of water protons in its vicinity, leading to an increase in signal intensity (brightness) of tissues.
In magnetic resonance imaging (MRI), visualization of normal and pathological tissue depends in part on variations in the radiofrequency signal intensity that occurs with:
- differences in proton density
- differences of the spin-lattice or longitudinal relaxation times (T1)
- differences in the spin-spin or transverse relaxation time (T2)
When placed in a magnetic field, gadoterate shortens the T1 and T2 relaxation times in target tissues. At recommended doses, the effect is observed with greatest sensitivity in the T1-weighted sequences.
Pharmacodynamics
Gadoterate affects proton relaxation times and consequently the MR signal, and the contrast obtained is characterized by the relaxivity of the gadoterate molecule. The relaxivity values for gadoterate are similar across the spectrum of magnetic field strengths used in clinical MRI (0.2-1.5 T).
Disruption of the blood-brain barrier or abnormal vascularity allows distribution of gadoterate in lesions such as neoplasms, abscesses, and infarcts.
Pharmacokinetics
The pharmacokinetics of total gadolinium assessed up to 48 hours following an intravenously administered 0.1 mmol/kg dose of Gadoterate Meglumine Injection in healthy adult subjects demonstrated a mean elimination half-life (reported as mean ± SD) of about 1.4 ± 0.2 hr and 2.0 ± 0.7 hr in female and male subjects, respectively. Similar pharmacokinetic profile and elimination half-life values were observed after intravenous injection of 0.1 mmol/kg of Gadoterate Meglumine Injection followed 20 minutes later by a second injection of 0.2 mmol/kg (1.7 ± 0.3 hr and 1.9 ± 0.2 hr in female and male subjects, respectively).
Distribution
The volume of distribution at steady state of total gadolinium in healthy subjects is 179 ± 26 and 211 ± 35 mL/kg in female and male subjects respectively, roughly equivalent to that of extracellular water. Gadoterate does not undergo protein binding in vitro . The extent of blood cell partitioning of gadoterate is not known.
Following GBCA administration, gadolinium is present for months or years in brain, bone, skin and other organs [see Warnings and Precautions (5.4 )] .
Metabolism
Gadoterate is not known to be metabolized.
Elimination
Following a 0.1 mmol/kg dose of Gadoterate Meglumine Injection, total gadolinium is excreted primarily in the urine with 72.9 ± 17.0% and 85.4 ± 9.7% (mean ± SD) eliminated within 48 hours, in female and male subjects, respectively. Similar values were achieved after a cumulative dose of 0.3 mmol/kg (0.1 + 0.2 mmol/kg, 20 minutes later), with 85.5 ± 13.2% and 92.0 ± 12.0% recovered in urine within 48 hrs in female and male subjects respectively.
In healthy subjects, the renal and total clearance rates of total gadolinium are comparable (1.27 ± 0.32 and 1.74 ± 0.12 mL/min/kg in females; and 1.40 ± 0.31 and 1.64 ± 0.35 mL/min/kg in males, respectively) indicating that the drug is primarily cleared through the kidneys. Within the studied dose range (0.1 to 0.3 mmol/kg), the kinetics of total gadolinium appear to be linear.
Specific Populations
Renal Impairment
A single intravenous dose of 0.1 mmol/kg of Gadoterate Meglumine Injection was administered to 8 patients (5 men and 3 women) with impaired renal function (mean serum creatinine of 498 ± 98 μmol/L in the 10-30 mL/min creatinine clearance group and 192 ± 62 μmol/L in the 30-60 mL/min creatinine clearance group). Renal impairment delayed the elimination of total gadolinium. Total clearance decreased as a function of the degree of renal impairment. The distribution volume was unaffected by the severity of renal impairment (Table 5). No changes in renal function test parameters were observed after Gadoterate Meglumine Injection. The mean cumulative urinary excretion of total gadolinium was approximately 76.9 ± 4.5% in 48 hrs in patients with moderate renal impairment, 68.4 ± 3.5% in 72 hrs in patients with severe renal impairment and 93.3 ± 4.7% in 24 hrs for subjects with normal renal function.
Population | Elimination Half-Life (hr) | Plasma Clearance (L/h/kg) | Distribution Volume (L/kg) |
Healthy volunteers | 1.6 ± 0.2 | 0.10 ± 0.01 | 0.246 ± 0.03 |
Patients with moderate renal impairment | 5.1 ± 1.0 | 0.036 ± 0.007 | 0.236 ± 0.01 |
Patients with severe renal impairment | 13.9 ± 1.2 | 0.012 ± 0.001 | 0.234 ± 0.01 |
Gadoterate was shown to be dialyzable after an IV injection of Gadoterate Meglumine Injection in 10 patients with end-stage renal failure who required hemodialysis treatment. Gd serum concentration decreased over time by 88%, 93% and 97% at 0.5 hr, 1.5 hr, and 4 hrs after start of dialysis, respectively. A second and third hemodialysis session further removed Gd. After the third dialysis, Gd serum concentration decreased by 99.7%.
Pediatric Population
The pharmacokinetics of gadoterate in pediatric patients receiving Gadoterate Meglumine Injection aged birth (term neonates) to 23 months, was investigated in an open label, multicenter study, using a population pharmacokinetics approach. A total of 45 subjects (22 males, 23 females) received a single intravenous dose of Gadoterate Meglumine Injection 0.1 mmol/kg (0.2 mL/kg). The age ranged from less than one week to 23.8 months (mean 9.9 months) and body weight ranged from 3 to 15 kg (mean 8.1 kg). Individual level of renal maturity in the study population, as expressed by eGFR ranged between 52 and 281 mL/min/1.73 m 2 and 11 patients had an eGFR below 100 mL/min/1.73 m 2 (range 52 to 95 mL/min/1.73 m 2 ).
Gadoterate concentrations obtained up to 8 hours after Gadoterate Meglumine Injection administration were best fitted using a biphasic model with linear elimination from the intravascular space. The mean clearance adjusted to body weight was estimated at 0.16 ± 0.07 L/h/kg and increased with eGFR. The estimated mean elimination half-life was 1.47 ± 0.45 hr.
The body weight adjusted clearance of gadoterate after single intravenous injection of 0.1 mmol/kg of Gadoterate Meglumine Injection in pediatric subjects aged less than 2 years was similar to that observed in healthy adults.
NONCLINICAL TOXICOLOGY
Carcinogenesis, Mutagenesis, Impairment of Fertility
Long-term animal studies have not been performed to evaluate the carcinogenic potential of gadoterate meglumine.
Gadoterate meglumine did not demonstrate mutagenic potential in in vitro bacterial reverse mutation assays (Ames test) using Salmonella typhimurium, in an in vitro chromosome aberration assay in Chinese hamster ovary cells, in an in vitro gene mutation assay in Chinese hamster lung cells, nor in an in vivo mouse micronucleus assay.
No impairment of male or female fertility and reproductive performance was observed in rats after intravenous administration of gadoterate meglumine at the maximum tested dose of 10 mmol/kg/day (16 times the maximum human dose based on surface area), given during more than 9 weeks in males and more than 4 weeks in females. Sperm counts and sperm motility were not adversely affected by treatment with the drug.
Animal Toxicology and/or Pharmacology
Local intolerance reactions, including moderate irritation associated with infiltration of inflammatory cells were observed after perivenous injection in rabbits suggesting the possibility of local irritation if the contrast medium leaks around the veins in a clinical setting [see Warnings and Precautions (5.5 )] .
Toxicity of gadoterate meglumine was evaluated in neonatal and juvenile (pre- and post-weaning) rats following a single or repeated intravenous administration at doses 1, 2, and 4 times the MHD based on BSA. Gadoterate meglumine was well tolerated at all dose levels tested and had no effect on growth, pre-weaning development, behavior and sexual maturation.
CLINICAL STUDIES
CNS Imaging
Efficacy and safety of Gadoterate Meglumine Injection were evaluated in a multi-center clinical trial (Study A) that enrolled 364 adult and 38 pediatric patients (aged ≥ 2 years) with known or suspected CNS lesions. Adults were randomized 2 to 1 to receive either Gadoterate Meglumine Injection or gadopentetate dimeglumine, each administered at a dose of 0.1 mmol/kg. All pediatric patients received Gadoterate Meglumine Injection, also at a dose of 0.1 mmol/kg. In the trial, patients first underwent a baseline (pre-contrast) MRI examination followed by the assigned GBCA administration and a post-contrast MR examination. The images (pre-contrast, post-contrast and “paired pre- and post-contrast”) were interpreted by three independent off-site readers blinded to clinical information. The primary efficacy analysis compared three patient-level visualization scores (paired images) to baseline MRI (pre-contrast images) for adults who received Gadoterate Meglumine Injection. The three primary visualization components were: contrast enhancement, border delineation and internal morphology. For each of these components there was a pre-defined scoring scale. Lesion counting (up to five per patient) was also reflected within each component’s patient-level visualization score.
Among the adult patients, 245 received Gadoterate Meglumine Injection and their data comprised the primary efficacy population. There were 114 (47%) men and 131 (53%) women with a mean age of 53 years (range 18 to 85 years), the racial and ethnic representations were 84% Caucasian, 11% Asian, 4% Black, and 1% other.
Table 6 displays a comparison of paired images (pre-and post-contrast) to pre-contrast images with respect to the proportion of patients who had paired image scores that were greater “better”, or same/worse “not better” than the pre-contrast scores and with respect to the difference in the mean patient level visualization score. Across the three readers 56% to 94% of patients had improved lesion visualization for paired images compared to pre-contrast images. Gadoterate Meglumine Injection provided a statistically significant improvement for all three primary visualization components. More lesions were seen on the paired images than the pre-contrast images.
Lesion Scores | Reader 1 | Reader 2 | Reader 3 |
n=231 | n=232 | n=237 | |
Border Delineation | |||
Better | 195 (84%) | 215 (93%) | 132 (56%) |
Not Better | 28 (12%) | 7 (3%) | 88 (37%) |
Missing | 8 (4%) | 10 (4%) | 17 (7%) |
Difference in Mean Score (b) | 2.26• | 2.89• | 1.17• |
Internal Morphology | |||
Better | 218 (94%) | 214 (93%) | 187 (79%) |
Not Better | 5 (2%) | 8 (3%) | 33 (14%) |
Missing | 8 (4%) | 10 (4%) | 17 (7%) |
Difference in Mean Score (b) | 2.74• | 2.75• | 1.54• |
Contrast Enhancement | |||
Better | 208 (90%) | 216 (93%) | 208 (88%) |
Not Better | 15 (6%) | 6 (3%) | 12 (5%) |
Missing | 8 (4%) | 10 (4%) | 17 (7%) |
Difference in Mean Score (b) | 3.09• | 3.69• | 2.92• |
(a) Better: number of patients with paired (pre-and post-contrast) score greater than the pre-contrast score, Not better: number of patients with paired score same as or worse than the pre-contrast score, Missing: number of patients with missing score
(b) Difference = paired mean score minus pre-contrast mean score
•Statistically significant improvement by paired t-test
In secondary analyses, post-contrast images were improved in comparison to pre-contrast images. Gadoterate Meglumine Injection lesion visualization scores were similar to those for gadopentetate dimeglumine. Gadoterate Meglumine Injection imaging results in the pediatric patients were also similar to those seen in adults.
In a second clinical trial (Study B), MR images were reread from 150 adult patients with known CNS lesions who had participated in previously conducted clinical trial. Gadoterate Meglumine Injection administration and image interpretation was performed in the same manner as in Study A. Similar to Study A, this trial also demonstrated improved lesion visualization with Gadoterate Meglumine Injection.
CNS Imaging in the Sub-Population of Pediatric Patients < 2 Years Old
A non-randomized study (Study C) with 28 pediatric patients under 2 years of age who were referred for contrast MRI of the CNS supported extrapolation of CNS efficacy findings from adults and older children. CNS lesions were identified in 16 of these 28 patients on paired pre- and post-contrast images compared to 15 patients on pre-contrast images alone. In the 16 patients who had identifiable lesions, the scores for the co-endpoints of lesion visualization were improved for at least one lesion on paired pre- and post-contrast images compared to pre-contrast images in 8 out of 16 (50%) patients for lesion border delineation, 8 out of 16 (50%) patients for lesion internal morphology, and 14 out of 16 (88%) patients for lesion contrast enhancement.
HOW SUPPLIED/STORAGE AND HANDLING
Gadoterate Meglumine Injection, USP is a clear, colorless to yellow solution containing 0.5 mmol/mL of gadoterate meglumine. It is supplied in vials.
- Gadoterate Meglumine Injection, USP is supplied in 10 mL vials containing 5 mL or 10 mL of solution, in 20 mL vials containing 15 mL or 20 mL of solution.
Each single dose vial is closed with a rubber stopper and sealed with an aluminum cap and the contents are sterile.
Vials are individually packaged in a box of 10, in the following configurations:
5 mL in glass vial (NDC 70436-123-31)
10 mL in glass vial (NDC 70436-123-33)
15 mL in glass vial (NDC 70436-123-34)
20 mL in glass vial (NDC 70436-123-35)
Storage
Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F) [See USP Controlled Room Temperature].
Should solidification occur in the vial because of exposure to the cold, Gadoterate Meglumine Injection, USP should be brought to room temperature before use. If allowed to stand at room temperature for a minimum of 90 minutes, Gadoterate Meglumine Injection, USP should return to a clear, colorless to yellow solution. Before use, examine the product to assure that all solids are dissolved and that the container and closure have not been damaged. Discard the vial if solids persist.
Mechanism of Action
Gadoterate is a paramagnetic molecule that develops a magnetic moment when placed in a magnetic field. The magnetic moment enhances the relaxation rates of water protons in its vicinity, leading to an increase in signal intensity (brightness) of tissues.
In magnetic resonance imaging (MRI), visualization of normal and pathological tissue depends in part on variations in the radiofrequency signal intensity that occurs with:
- differences in proton density
- differences of the spin-lattice or longitudinal relaxation times (T1)
- differences in the spin-spin or transverse relaxation time (T2)
When placed in a magnetic field, gadoterate shortens the T1 and T2 relaxation times in target tissues. At recommended doses, the effect is observed with greatest sensitivity in the T1-weighted sequences.