Get your patient on Luzu (Luliconazole)
Luzu prior authorization resources
Most recent state uniform prior authorization forms
Dosage & administration
DOSAGE AND ADMINISTRATION
For topical use only. LUZU Cream, 1% is not for ophthalmic, oral, or intravaginal use.
- When treating interdigital tinea pedis, a thin layer of LUZU Cream, 1% should be applied to the affected area and approximately 1 inch of the immediate surrounding area(s) once daily for 2 weeks.
- When treating tinea cruris or tinea corporis, LUZU Cream, 1% should be applied to the affected area and approximately 1 inch of the immediate surrounding area(s) once daily for 1 week.

By using PrescriberAI, you agree to the AI Terms of Use.
Luzu prescribing information
INDICATIONS AND USAGE
LUZU (luliconazole) Cream, 1% is indicated for the topical treatment of interdigital tinea pedis, tinea cruris, and tinea corporis caused by the organisms Trichophyton rubrum and Epidermophyton floccosum .
DOSAGE AND ADMINISTRATION
For topical use only. LUZU Cream, 1% is not for ophthalmic, oral, or intravaginal use.
- When treating interdigital tinea pedis, a thin layer of LUZU Cream, 1% should be applied to the affected area and approximately 1 inch of the immediate surrounding area(s) once daily for 2 weeks.
- When treating tinea cruris or tinea corporis, LUZU Cream, 1% should be applied to the affected area and approximately 1 inch of the immediate surrounding area(s) once daily for 1 week.
DOSAGE FORMS AND STRENGTHS
Cream, 1%. Each gram of LUZU Cream, 1% contains 10 mg of luliconazole in a white cream base.
USE IN SPECIFIC POPULATIONS
Pregnancy
Risk Summary
There are no available data with LUZU Cream, 1% use in pregnant women to inform a drug-associated risk for major birth defects and miscarriage. In animal reproduction studies with pregnant rats and rabbits, there were no adverse developmental effects observed with subcutaneous administration of luliconazole during organogenesis at doses up to 3 and 24 times, respectively, the maximum recommended human dose (MRHD) [see Data] .
The background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Data
Animal Data
The animal multiples of human exposure calculations were based on daily dose body surface area (BSA) comparisons (mg/m 2 ) for the reproductive toxicology studies described in this section and in Section 13.1. The maximum recommended human dose (MRHD) was set at 8 g 1% cream per day (1.33 mg/kg/day for a 60 kg individual, which is equivalent to 49.2 mg/m 2 /day).
Systemic embryofetal development studies were conducted in rats and rabbits. Subcutaneous doses of 1, 5 and 25 mg/kg/day luliconazole were administered during the period of organogenesis (gestational days 7-17) to pregnant female rats. No treatment-related effects on maternal toxicity or malformations were noted at 25 mg/kg/day (3 times the MRHD based on BSA comparisons). Increased incidences of skeletal variation (14 th rib) were noted at 25 mg/kg/day. No treatment-related effects on skeletal variation were noted at 5 mg/kg/day (0.6 times the MRHD based on BSA comparisons).
Subcutaneous doses of 4, 20 and 100 mg/kg/day luliconazole were administered during the period of organogenesis (gestational days 6-18) to pregnant female rabbits. No treatment-related effects on maternal toxicity, embryofetal toxicity or malformations were noted at 100 mg/kg/day (24 times the MRHD based on BSA comparisons).
In a pre- and postnatal development study in rats, subcutaneous doses of 1, 5 and 25 mg/kg/day luliconazole were administered from the beginning of organogenesis (gestation day 7) through the end of lactation (lactation day 20). In the presence of maternal toxicity, embryofetal toxicity (increased prenatal pup mortality, reduced live litter sizes and increased postnatal pup mortality) was noted at 25 mg/kg/day.
No embryofetal toxicity was noted at 5 mg/kg/day (0.6 times the MRHD based on BSA comparisons). No treatment effects on postnatal development were noted at 25 mg/kg/day (3 times the MRHD based on BSA comparisons).
Lactation
Risk Summary
There is no information available on the presence of luliconazole in human milk, the effects of the drug on the breastfed infant, or the effects of the drug on milk production after topical application of LUZU Cream, 1% to women who are breastfeeding. LUZU Cream, 1% has low systemic absorption. The lack of clinical data during lactation precludes a clear determination of the risk of LUZU Cream, 1% to an infant during lactation. Therefore, the developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for LUZU Cream, 1% and any potential adverse effects on the breastfed infant from LUZU Cream, 1% or from the underlying maternal condition.
Pediatric Use
The safety and effectiveness of LUZU Cream, 1% in pediatric patients 12 to <18 years of age with tinea pedis and tinea cruris have been established by evidence from well-controlled trials in adult and pediatric subjects and a pharmacokinetic (PK) study in pediatric subjects [see Clinical Pharmacology (12.3 ) and Clinical Studies (14 )].
The safety and effectiveness of LUZU Cream, 1% in pediatric patients 2 to <18 years of age with tinea corporis have been established by evidence from a well-controlled trial in pediatric subjects [see Clinical Pharmacology (12.3 ) and Clinical Studies (14 )].
Geriatric Use
Of the total number of subjects in clinical studies of LUZU Cream, 1%, 8% were 65 and over, while 1.4% were 75 and over. No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
CONTRAINDICATIONS
None.
ADVERSE REACTIONS
The most common adverse reactions observed in clinical trials were application site reactions, which occurred in less than 1% of subjects. (6.1 )
To report SUSPECTED ADVERSE REACTIONS, contact Bausch Health US, LLC at 1-800-321-4576 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
In three Phase 3 clinical trials, 616 subjects were exposed to LUZU Cream, 1%: 305 with interdigital tinea pedis and 311 subjects with tinea cruris. Subjects with interdigital tinea pedis or tinea cruris applied LUZU Cream, 1% or vehicle cream once daily for 14 days or 7 days, respectively, to affected and adjacent areas. During clinical trials with LUZU Cream, 1%, the most common adverse reactions were application site reactions which occurred in less than 1% of subjects in both the LUZU and vehicle arms. Most adverse reactions were mild in severity.
A post-approval clinical trial was conducted in 75 subjects age 2 to <18 years old with tinea corporis. The adverse reactions in the LUZU Cream, 1% treated population were similar to the vehicle treated population.
Postmarketing Experience
The following adverse reactions have been identified during postmarketing use of luliconazole cream, 1%: contact dermatitis and cellulitis. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
DRUG INTERACTIONS
An in vivo study in adult subjects with moderate to severe interdigital tinea pedis and tinea cruris showed that LUZU Cream, 1% is mostly a weak inhibitor of CYP2C19. In a separate trial in adolescent subjects with tinea cruris, in vivo blood levels of LUZU Cream, 1%, were seen to approach those levels sufficient to show moderate inhibition of CYP2C19 [see Clinical Pharmacology (12.3 )] .
DESCRIPTION
LUZU (luliconazole) Cream, 1% contains 1% luliconazole, an azole antifungal agent, in a white cream for topical application.
Luliconazole is (2E)-2-[(4R)-4-(2,4-dichlorophenyl)-1,3-dithiolan-2-ylidene]-2-imidazol-1-ylacetonitrile. Its structural formula is:
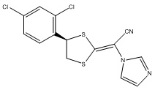
The molecular formula is C 14 H 9 Cl 2 N 3 S 2 with a molecular weight of 354.28. Luliconazole is the R enantiomer and contains one chiral center. The double bond adjacent to the dithiolane group is in the E configuration.
LUZU Cream, 1% contains 10 mg of luliconazole per gram of cream in a vehicle consisting of benzyl alcohol, butylated hydroxytoluene, cetostearyl alcohol, isopropyl myristate, medium-chain triglycerides, methylparaben, polysorbate 60, propylene glycol, purified water, and sorbitan monostearate.
CLINICAL PHARMACOLOGY
Mechanism of Action
LUZU Cream, 1% is an azole antifungal [see MICROBIOLOGY (12.4 )] .
Pharmacodynamics
At therapeutic doses, LUZU Cream, 1% is not expected to prolong QTc to any clinically relevant extent.
Pharmacokinetics
Luliconazole is the R enantiomer of a chiral molecule. The potential for interconversion between R and S enantiomers in humans has not been assessed. Information on the pharmacokinetics of luliconazole presented below refers to both R enantiomer and S enantiomer, if any, combined.
Luliconazole is >99% protein bound in plasma.
In a PK trial, 12 subjects with moderate to severe tinea pedis and 8 subjects with moderate to severe tinea cruris applied a mean daily amount of approximately 3.5 grams of LUZU Cream, 1% to the affected and surrounding areas once daily for 15 days. Plasma concentrations of luliconazole on Day 15 were measurable in all subjects and fluctuated little during the 24-hour interval. In subjects with tinea pedis, the mean ± SD of the maximum concentration (C max ) was 0.40 ± 0.76 ng/mL after the first dose and 0.93 ± 1.23 ng/mL after the final dose. The mean time to reach C max (T max ) was 16.9 ± 9.39 hours after the first dose and 5.8 ± 7.61 hours after the final dose. Exposure to luliconazole, as expressed by area under the concentration time curve (AUC 0–24 ), was 6.88 ± 14.50 ng•hr/mL after the first dose and 18.74 ± 27.05 ng•hr/mL after the final dose. In subjects with tinea cruris, the mean ± SD C max was 4.91 ± 2.51 ng/mL after the first dose and 7.36 ± 2.66 ng/mL after the final dose. The mean T max was 21.0 ± 5.55 hours after the first dose and 6.5 ± 8.25 hours after the final dose. Exposure to luliconazole, as expressed by AUC 0–24 , was 85.1 ± 43.69 ng•hr/mL after the first dose and 121.74 ± 53.36 ng•hr/mL after the final dose.
PK data of luliconazole measured in adolescent subjects (12 to <18 years of age) with moderate to severe interdigital tinea pedis or moderate to severe tinea cruris as well as in subjects 2 to <18 years of age with tinea corporis are described in Specific Populations below.
Specific Populations
PK of luliconazole was assessed in 30 adolescent subjects 12 to <18 years of age with moderate to severe interdigital tinea pedis (N=15) or moderate to severe tinea cruris (N=15). Subjects with tinea pedis applied approximately 3 grams of LUZU Cream, 1% once daily to the affected area and adjacent skin for 15 days, while subjects with tinea cruris applied LUZU Cream, 1% once daily to the affected and adjacent skin for 8 days.
Generally, the systemic exposure of luliconazole was greater in the subjects with tinea cruris than tinea pedis. In subjects with tinea pedis, the systemic concentrations of luliconazole were quantifiable in all the subjects on Day 8 and Day 15. The mean ± SD C max was 1.80 ± 1.86 ng/mL after the first dose on Day 1, and 3.93 ± 1.67 ng/mL and 3.27 ± 1.71 ng/mL on Days 8 and 15, respectively. The mean ± SD AUC 0-24 was 20.47 ± 14.47 ng•hr/mL after the first dose on Day 1, and 64.94 ± 32.47 ng•hr/mL and 60.38 ± 37.92 ng•hr/mL on Days 8 and Day 15, respectively. Like in adult subjects, the mean plasma concentrations of luliconazole in adolescent subjects on Days 8 and 15 were similar and fluctuated little during a 24-hour interval.
In subjects with moderate to severe tinea cruris, the systemic concentrations of luliconazole were quantifiable in all the subjects on Day 8. The mean ± SD C max was 9.80 ± 5.94 ng/mL after the first dose (Day 1) and 15.40 ± 13.62 ng/mL after the last dose (Day 8). The mean ± SD AUC 0-24 was 157.07 ± 92.18 ng•hr/mL and 266.06 ± 236.07 ng•hr/mL, after the first dose (Day 1) and the last dose (Day 8).
In subjects with tinea corporis, the systemic concentrations of luliconazole were assessed at pre-dose and at 6 hours post-dose on the last day of treatment following once daily treatment with LUZU Cream, 1% for 7 days. The systemic concentrations were quantifiable in all the 12 subjects and the mean ± SD daily dose of LUZU Cream, 1% was 2.84 ± 1.82 g. The mean ± SD concentrations of luliconazole at 15 minutes prior to dosing and at 6 hours post-dose on Day 7 were 4.63 ± 2.93 ng/mL and 4.84 ± 3.33 ng/mL, respectively.
Drug Interactions
Results of in vitro studies indicated that therapeutic doses of LUZU Cream, 1% did not inhibit cytochrome P450 (CYP) enzymes 1A2, 2C9 and 2D6, but can inhibit the activity of CYP2B6, 2C8, 2C19, and 3A4. The most sensitive enzyme, CYP2C19, was further evaluated in an in vivo study using omeprazole as a probe substrate in adult subjects with moderate to severe interdigital tinea pedis and tinea cruris. The results showed that LUZU Cream, 1% applied at a daily amount of approximately 4 grams increased the omeprazole systemic exposure (AUC) by approximately 30% compared to the exposure of omeprazole administered alone. LUZU Cream, 1% is considered a weak inhibitor of CYP2C19. For tinea cruris, extrapolation from both in vitro inhibition studies and in vivo data in adults to the adolescent subjects showed that in some subjects, levels of luliconazole can approach or exceed those required to be a moderate inhibitor of CYP2C19.
Results of in vitro studies indicated that therapeutic doses of LUZU Cream, 1% did not induce CYP1A2, 2B6, and 3A4.
Microbiology
Mechanism of Action
Luliconazole is an antifungal that belongs to the azole class. Although the exact mechanism of action against dermatophytes is unknown, luliconazole appears to inhibit ergosterol synthesis by inhibiting the enzyme lanosterol demethylase. Inhibition of this enzyme’s activity by azoles results in decreased amounts of ergosterol, a constituent of fungal cell membranes, and a corresponding accumulation of lanosterol.
Mechanism of Resistance
To date, a mechanism of resistance to luliconazole has not been described.
LUZU Cream, 1% has been shown to be active against most isolates of the following fungi, both in vitro and in clinical infections as described in the INDICATIONS AND USAGE section:
- Trichophyton rubrum
- Epidermophyton floccosum
NONCLINICAL TOXICOLOGY
Carcinogenesis, Mutagenesis, Impairment of Fertility
Long-term studies to evaluate the carcinogenic potential of LUZU Cream, 1% have not been conducted.
Luliconazole revealed no evidence of mutagenic or clastogenic potential based on the results of two in vitro genotoxicity tests (Ames assay and Chinese hamster lung cell chromosomal aberration assay) and one in vivo genotoxicity test (mouse bone marrow micronucleus test).
In a fertility study in rats, subcutaneous doses of 1, 5 and 25 mg/kg/day luliconazole were administered prior to and during mating and through early pregnancy. Treatment-related effects on reproductive function were noted in females (decreased live embryos and decreased corpus luteum) at 5 and 25 mg/kg/day and males (decreased sperm counts) at 25 mg/kg/day. No treatment-related effects on fertility or reproductive function were noted at 1 mg/kg/day (0.1× MRHD based on BSA comparisons).
CLINICAL STUDIES
Interdigital Tinea Pedis
The safety and efficacy of LUZU (luliconazole) Cream, 1% was evaluated in two randomized, double-blind, vehicle-controlled, multi-center clinical trials in 423 subjects with a clinical and culture-confirmed diagnosis of interdigital tinea pedis. Subjects were randomized to receive LUZU Cream, 1% or vehicle. Subjects applied either LUZU Cream, 1% or vehicle cream to the entire area of the forefeet including all interdigital web spaces and approximately 2.5 cm (1 in) of the surrounding area of the foot once daily for 14 days.
The mean age of the study population was 41 years (range 13 to 78 years); 82% were male; 53% were White and 40% were Black or African American. Signs and symptoms of tinea pedis (erythema, scaling, and pruritus), KOH exam and dermatophyte culture were assessed at baseline, end-of-treatment (Day 14), 2 and 4 weeks post-treatment.
Overall treatment success was defined as complete clearance (clinical cure and mycological cure) at 4 weeks post-treatment. LUZU Cream, 1% demonstrated complete clearance in subjects with interdigital tinea pedis. Treatment outcomes at 4 weeks post-treatment are summarized in Table 1.
| Study 1 | Study 2 | |||
|---|---|---|---|---|
| LUZU Cream, 1% N=106 n (%) | Vehicle Cream N=103 n (%) | LUZU Cream, 1% N=107 n (%) | Vehicle Cream N=107 n (%) | |
Complete Clearance Proportion of subjects who achieved both clinical cure and mycological cure | 28 (26%) | 2 (2%) | 15 (14%) | 3 (3%) |
Effective Treatment Negative KOH and culture and at most mild erythema and/or scaling and no pruritus | 51 (48%) | 10 (10%) | 35 (33%) | 16 (15%) |
Clinical Cure Absence of erythema, scaling and pruritus | 31 (29%) | 8 (8%) | 16 (15%) | 4 (4%) |
Mycological Cure Negative KOH and negative fungal culture | 66 (62%) | 18 (18%) | 60 (56%) | 29 (27%) |
Tinea Cruris
The safety and efficacy of LUZU (luliconazole) Cream, 1% was evaluated in a randomized, double-blind, vehicle-controlled, multi-center clinical trial in 256 subjects with a clinical and culture-confirmed diagnosis of tinea cruris. Subjects were randomized to receive LUZU Cream, 1% or vehicle. Subjects applied either LUZU Cream, 1% or vehicle cream to the affected area and approximately 2.5 cm (1 in) of the surrounding area once daily for 7 days.
The mean age of the study population was 40 years (range 14 to 88 years); 83% were male; 58% were White and 34% were Black or African American. Signs and symptoms of tinea cruris (erythema, scaling, and pruritus), positive KOH exam and dermatophyte culture were assessed at baseline, end-of-treatment (Day 7), 2 and 3 weeks post-treatment.
Overall treatment success was defined as complete clearance (clinical cure and mycological cure) at 3 weeks post-treatment. LUZU Cream, 1% demonstrated complete clearance in subjects with tinea cruris. Treatment outcomes at 3 weeks post-treatment are summarized in Table 2.
| LUZU Cream, 1% N=165 n (%) | Vehicle Cream N=91 n (%) | |
|---|---|---|
Complete Clearance Proportion of subjects who achieved both clinical cure and mycological cure | 35 (21%) | 4 (4%) |
Effective Treatment Negative KOH and culture and at most mild erythema and/or scaling and no pruritus | 71 (43%) | 17 (19%) |
Clinical Cure Absence of erythema, scaling and pruritus | 40 (24%) | 6 (7%) |
Mycological Cure Negative KOH and negative fungal culture | 129 (78%) | 41 (45%) |
Tinea Corporis
The safety and efficacy of LUZU (luliconazole) Cream, 1% was evaluated in a randomized, double-blind, vehicle-controlled, multi-center clinical trial in 75 subjects age 2 to <18 years old with a clinical and culture-confirmed diagnosis of tinea corporis. Subjects were randomized to receive LUZU Cream, 1% or vehicle cream. Subjects applied either LUZU Cream, 1% or vehicle cream to the affected area and approximately 2.5 cm (1 in) of the surrounding skin once daily for 7 days.
The mean age of the study population was 8 years; 72% were male; 36% were White and 64% were Black or African American. Signs and symptoms of tinea cruris (erythema, scaling, and pruritus), positive KOH exam and dermatophyte culture were assessed at baseline, end-of-treatment (Day 7), 2 and 3 weeks post-treatment.
Treatment outcomes at 3 weeks post-treatment are summarized in Table 3.
| LUZU Cream, 1% N=51 n (%) | Vehicle Cream N=14 n (%) | |
|---|---|---|
Complete Clearance Proportion of subjects who achieved both clinical cure and mycological cure | 36 (71%) | 5 (36%) |
Effective Treatment Negative KOH and culture and at most mild erythema and/or scaling and no pruritus | 39 (77%) | 8 (57%) |
Clinical Cure Absence of erythema, scaling and pruritus | 41 (80%) | 6 (43%) |
Mycological Cure Negative KOH and negative fungal culture | 41 (80%) | 8 (57%) |
HOW SUPPLIED/STORAGE AND HANDLING
LUZU (luliconazole) Cream, 1% is a white cream supplied in tubes as follows:
60 g NDC 99207-850-60
Store at 20° to 25°C (68° to 77°F); excursions permitted from 15° to 30°C (59° to 86°F) [see USP Controlled Room Temperature].
Mechanism of Action
LUZU Cream, 1% is an azole antifungal [see MICROBIOLOGY (12.4 )] .