Get your patient on Mirena (Levonorgestrel)
Mirena prior authorization resources
Most recent state uniform prior authorization forms
Mirena patient education
Patient toolkit
Dosage & administration
DOSAGE AND ADMINISTRATION
- Release rate of levonorgestrel (LNG) is 21 mcg/day after 24 days; this rate is reduced to about 11 mcg/day after 5 years and 7 mcg/day after 8 years. (2.1 )
- To be inserted by a trained healthcare provider using strict aseptic technique. Follow insertion instructions exactly as described. (2.2 )
- Patient should be re-examined and evaluated 4 to 6 weeks after insertion; then, yearly or more often if clinically indicated. (2.3 )
Dosing Over Time
Mirena contains 52 mg of levonorgestrel (LNG) released in vivo, at a rate of approximately 21 mcg/day after 24 days. This rate decreases progressively to approximately 11 mcg/day after 5 years and 7 mcg/day after 8 years.
For contraception, remove Mirena by the end of the eighth year and replace at the time of removal with a new Mirena if continued use is desired.
For treatment of heavy menstrual bleeding, replace Mirena by the end of the fifth year if continued use is needed because data on use in this indication beyond 5 years are limited.
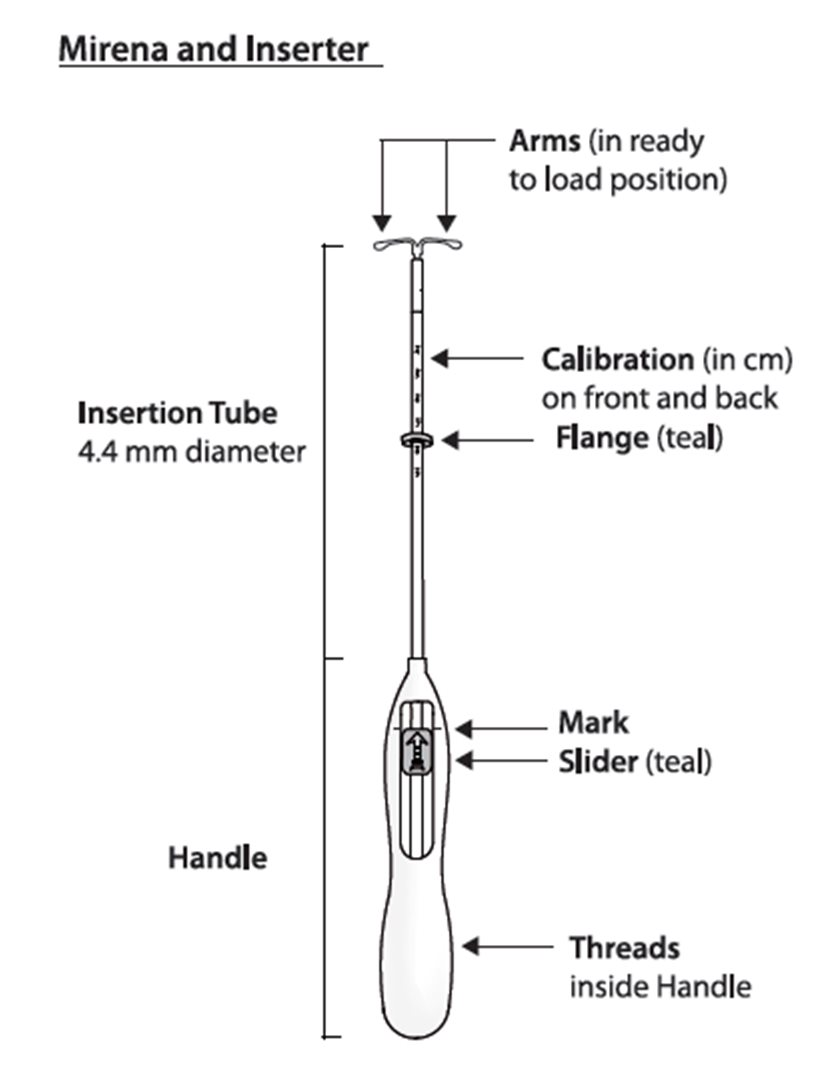
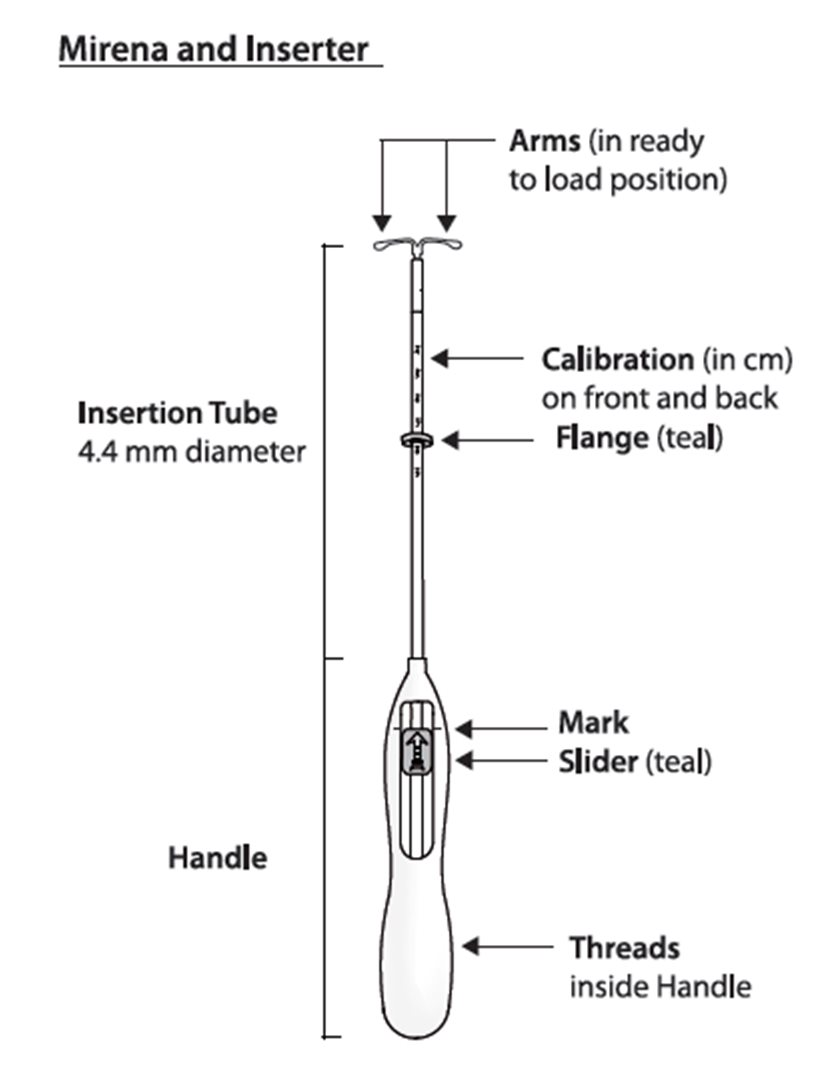
Mirena is supplied in a sterile package within an inserter that enables single-handed loading (see Figure 1). Do not open the package until required for insertion [see Description (11.2 )]. Do not use if the seal of the sterile package is broken or appears compromised. Use strict aseptic techniques throughout the insertion procedure [see Warnings and Precautions (5.3 )] .
Insertion Instructions
- Obtain a complete medical and social history to determine conditions that might influence the selection of a levonorgestrel-releasing intrauterine system (LNG IUS) for contraception . If indicated, perform a physical examination, and appropriate tests for any forms of genital or other sexually transmitted infections. [See Contraindications (4 ) and Warnings and Precautions (5.10 ).] Because irregular bleeding/spotting is common during the first months of Mirena use, exclude endometrial pathology (polyps or cancer) prior to the insertion of Mirena in women with persistent or uncharacteristic bleeding [see Warnings and Precautions (5.8 )].
- Follow the insertion instructions exactly as described to ensure proper placement and avoid premature release of Mirena from the inserter. Once released, Mirena cannot be re-loaded .
- Check expiration date of Mirena prior to initiating insertion.
- Mirena should be inserted by a trained healthcare provider. Healthcare providers should become thoroughly familiar with the insertion instructions before attempting insertion of Mirena.
- Insertion may be associated with some pain and/or bleeding or vasovagal reactions (for example, syncope, bradycardia), or with seizure, especially in patients with a predisposition to these conditions. Consider administering analgesics prior to insertion.
Timing of Insertion
Starting Mirena in women not currently using hormonal or intrauterine contraception |
|
Switching to Mirena from an oral, transdermal, or vaginal hormonal contraceptive |
|
Switching to Mirena from an injectable progestin contraceptive |
|
Switching to Mirena from a contraceptive implant or another IUS |
|
Inserting Mirena after first-trimester abortion or miscarriage |
|
Inserting Mirena after childbirth or second-trimester abortion or miscarriage | |
| |
Interval insertion following complete involution of the uterus |
|
Tools for Insertion
Note: The inserter provided with Mirena (see Figure 1) and the Insertion Procedure described in this section are not applicable for immediate insertion after childbirth or second-trimester abortion or miscarriage. For immediate insertion, remove Mirena from the inserter by first loading (see Figure 2) and then releasing (see Figure 7) Mirena from the inserter, and insert according to accepted practice.
Preparation
- Gloves
- Speculum
- Sterile uterine sound
- Sterile tenaculum
- Antiseptic solution, applicator
Procedure
- Sterile gloves
- Mirena with inserter in sealed package
- Instruments and anesthesia for paracervical block, if anticipated
- Consider having an unopened back-up Mirena available
- Sterile, sharp curved scissors
Preparation for insertion
- Exclude pregnancy and confirm that there are no other contraindications to the use of Mirena.
- With the patient comfortably in lithotomy position, do a bimanual exam to establish the size, shape and position of the uterus.
- Gently insert a speculum to visualize the cervix.
- Thoroughly cleanse the cervix and vagina with a suitable antiseptic solution.
- Prepare to sound the uterine cavity. Grasp the upper lip of the cervix with a tenaculum forceps and gently apply traction to stabilize and align the cervical canal with the uterine cavity. Perform a paracervical block if needed. If the uterus is retroverted, it may be more appropriate to grasp the lower lip of the cervix. The tenaculum should remain in position and gentle traction on the cervix should be maintained throughout the insertion procedure.
- Gently insert a uterine sound to check the patency of the cervix, measure the depth of the uterine cavity in centimeters, confirm cavity direction, and detect the presence of any uterine anomaly. If you encounter difficulty or cervical stenosis, use dilatation, and not force, to overcome resistance. If cervical dilatation is required, consider using a paracervical block.
- The uterus should sound to a depth of 6 to 10 cm. Insertion of Mirena into a uterine cavity less than 6 cm by sounding may increase the incidence of expulsion, bleeding, pain, perforation, and possibly pregnancy.
Insertion Procedure
Proceed with insertion only after completing the above steps and ascertaining that the patient is appropriate for Mirena. Ensure use of aseptic technique throughout the entire procedure .
Step 1–Opening of the package
- Open the package (Figure 1). The contents of the package are sterile.
- Using sterile gloves lift the handle of the sterile inserter and remove from the sterile package.
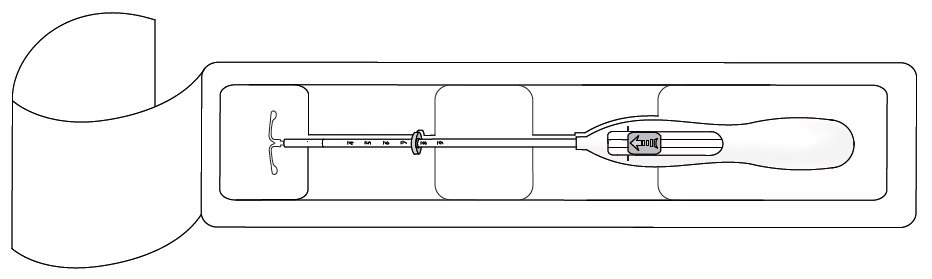
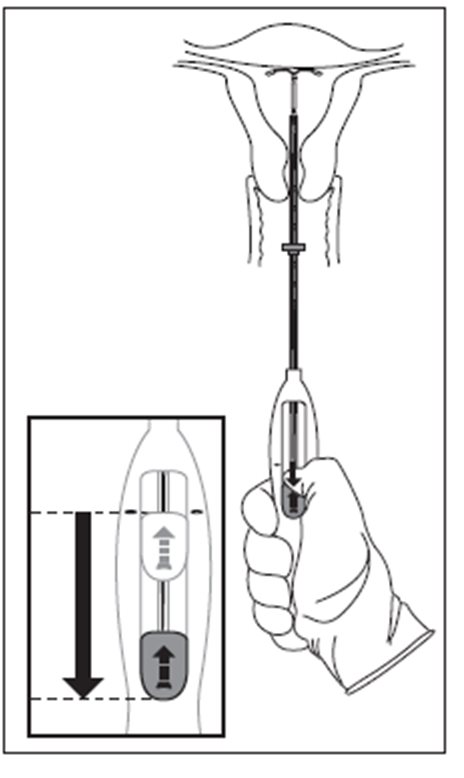
Step 2–Load Mirena into the insertion tube
- Push the slider forward as far as possible in the direction of the arrow thereby moving the insertion tube over the Mirena T-body to load Mirena into the insertion tube (Figure 2). The tips of the arms will meet to form a rounded end that extends slightly beyond the insertion tube.
- Maintain forward pressure with your thumb or forefinger on the slider. DO NOT move the slider downward at this time as this may prematurely release the threads of Mirena. Once the slider is moved below the mark, Mirena cannot be re-loaded.
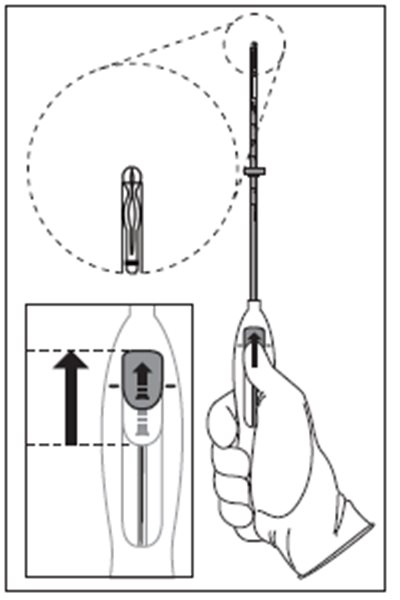
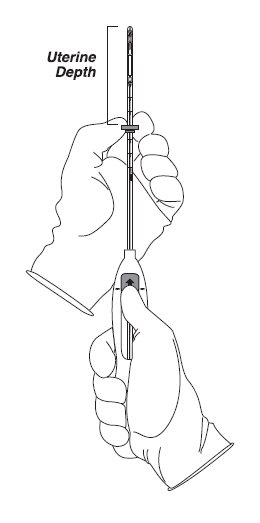
Step 3–Setting the Flange
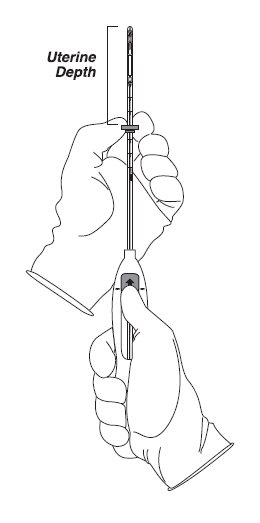
- Holding the slider in this forward position, set the upper edge of the flange to correspond to the uterine depth (in centimeters) measured during sounding (Figure 3).
Step 4–Mirena is now ready to be inserted
- Continue holding the slider in this forward position. Advance the inserter through the cervix until the flange is approximately 1.5–2 cm from the cervix and then pause (Figure 4).
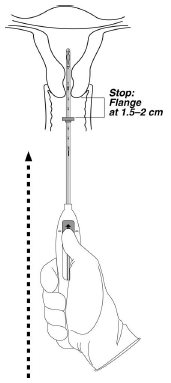
Do not force the inserter. If necessary, dilate the cervical canal.
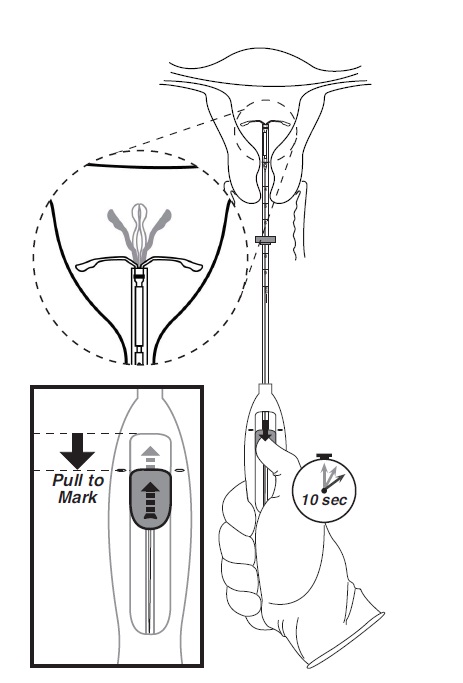
Step 5–Open the arms
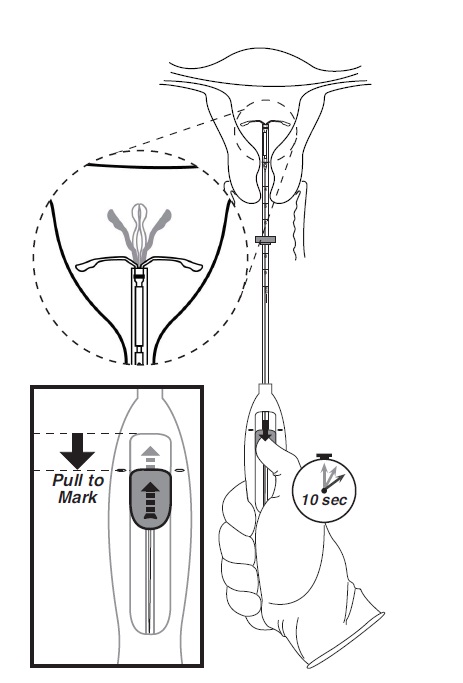
While holding the inserter steady, move the slider down to the mark to release the arms of Mirena (Figure 5). Wait 10 seconds for the horizontal arms to open completely.
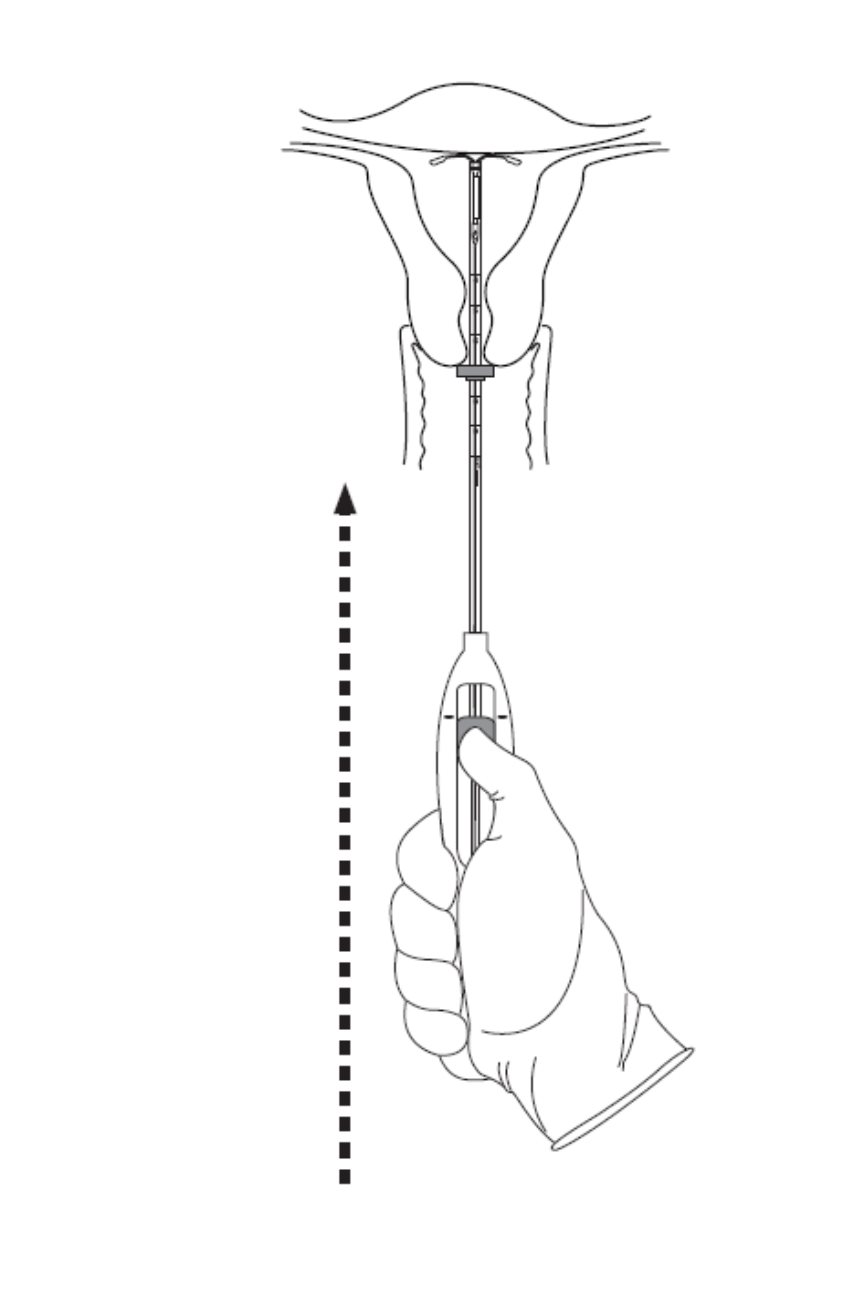
Step 6–Advance to fundal position
- Advance the inserter gently towards the fundus of the uterus until the flange touches the cervix. If you encounter fundal resistance do not continue to advance. Mirena is now in the fundal position (Figure 6). Fundal positioning of Mirena is important to prevent expulsion.
Step 7–Release Mirena and withdraw the inserter
- Holding the entire inserter firmly in place, release Mirena by moving the slider all the way down (Figure 7).
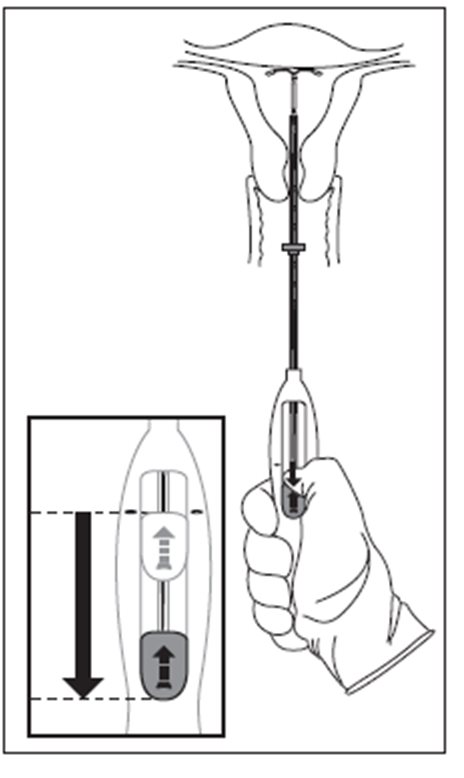
- Continue to hold the slider all the way down while you slowly and gently withdraw the inserter from the uterus.
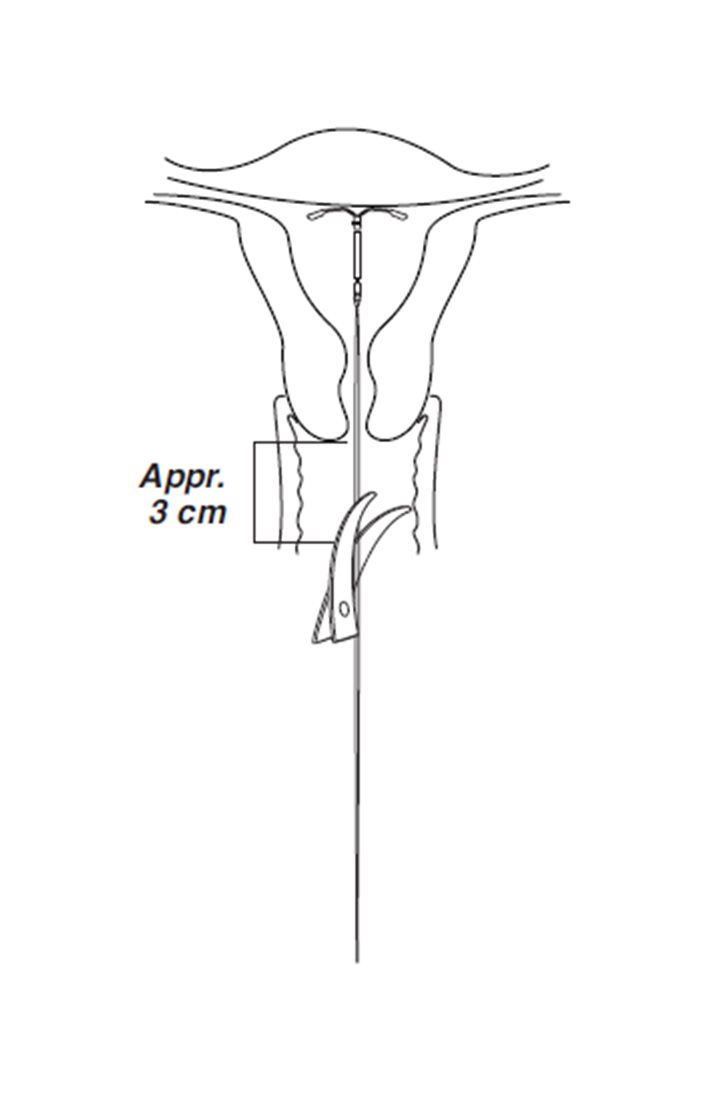
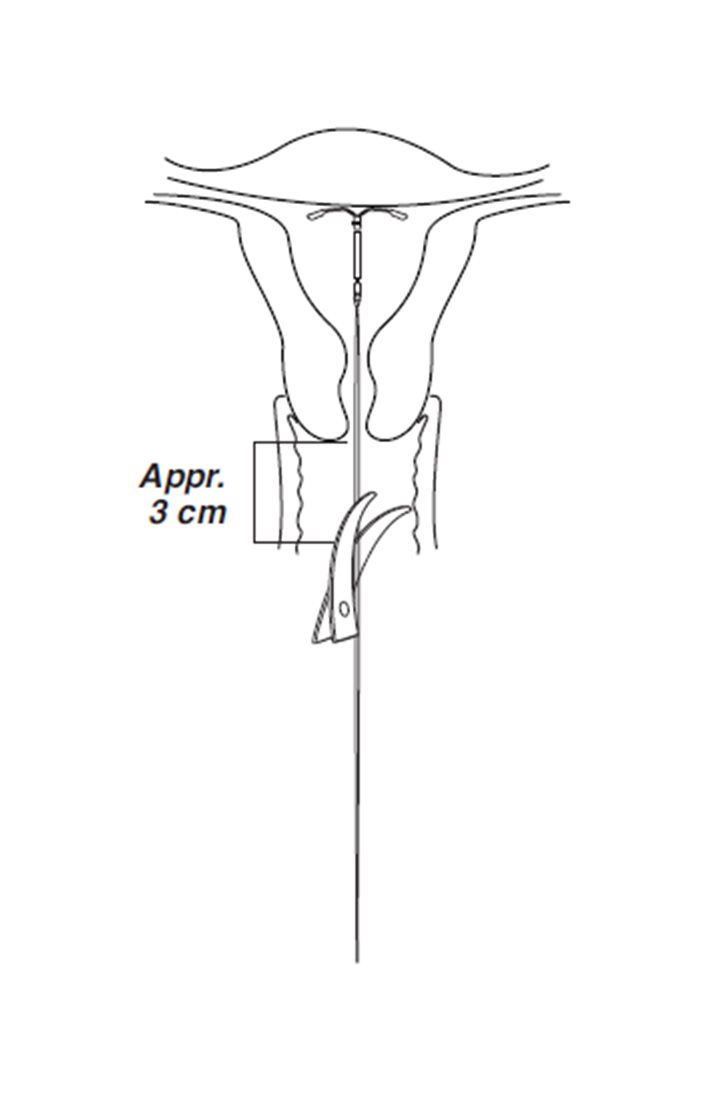
- Using a sharp, curved scissor, cut the threads perpendicular, leaving about 3 cm visible outside of the cervix [cutting threads at an angle may leave sharp ends (Figure 8)]. Do not apply tension or pull on the threads when cutting to prevent displacing Mirena.
Mirena insertion is now complete. Prescribe analgesics, if indicated. Record the Mirena lot number in the patient records.
Important information to consider during or after insertion
- If you suspect that Mirena is not in the correct position, check placement (for example, using transvaginal ultrasound). Remove Mirena if it is not positioned completely within the uterus. Do not reinsert a removed Mirena.
- If there is clinical concern, exceptional pain or bleeding during or after insertion, take appropriate steps (such as physical examination and ultrasound) immediately to exclude perforation.
Patient Follow-up
Reexamine and evaluate patients 4 to 6 weeks after insertion and once a year thereafter, or more frequently if clinically indicated.
Removal of Mirena
Timing of Removal
- For contraception, remove Mirena by the end of the eighth year and replace at the time of removal with a new Mirena if continued use is desired. Replace Mirena by the end of the fifth year if continued treatment of heavy menstrual bleeding is needed.
- If pregnancy is not desired, remove Mirena during the first 7 days of the menstrual cycle, provided the woman is still experiencing regular menses. If removal will occur at other times during the cycle, or the woman does not experience regular menses, she is at risk of pregnancy; start a new contraceptive method a week prior to removal for these women. [See Dosage and Administration (2.5 ).]
Tools for Removal
Preparation
- Gloves
- Speculum
Procedure
- Sterile forceps
Removal Procedure
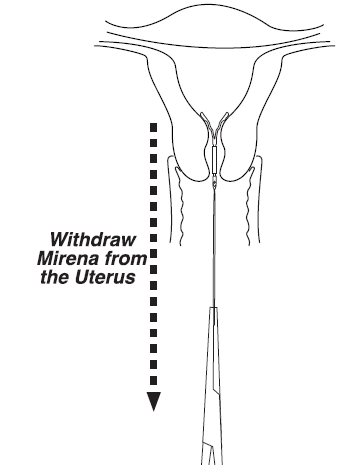
- Remove Mirena by applying gentle traction on the threads with forceps. (Figure 9).
- If the threads are not visible, determine location of Mirena by ultrasound [see Warnings and Precautions (5.10 )] .
- If Mirena is found to be in the uterine cavity on ultrasound exam, it may be removed using a narrow forceps, such as an alligator forceps. This may require dilation of the cervical canal. After removal of Mirena, examine the system to ensure that it is intact. The hormone cylinder may slide over and cover the horizontal arms, giving the appearance of missing arms. This situation generally does not require further intervention once the system is verified to be intact.
- If unable to remove with gentle traction, determine Mirena location and exclude perforation by ultrasound or other imaging [ see Warnings and Precautions (5.10 )].
- Removal may be associated with:
- pain and/or bleeding, vasovagal reactions (for example, syncope, bradycardia) or seizure, especially in patients with a predisposition to these conditions.
- breakage or embedment of Mirena in the myometrium that can make removal difficult [see Warnings and Precautions (5.5 )] . Analgesia, paracervical anesthesia, cervical dilation, alligator forceps or other grasping instrument, or hysteroscopy may be used to assist in removal.
Continuation of Contraception after Removal
- If pregnancy is not desired and if a woman wishes to continue using Mirena, a new system can be inserted immediately after removal any time during the cycle.
- If a patient with regular cycles wants to start a different contraceptive method, time removal and initiation of the new method to ensure continuous contraception. Either remove Mirena during the first 7 days of the menstrual cycle and start the new method immediately thereafter or start the new method at least 7 days prior to removing Mirena if removal is to occur at other times during the cycle.
- If a patient with irregular cycles or amenorrhea wants to start a different contraceptive method, start the new method at least 7 days before removal.

By using PrescriberAI, you agree to the AI Terms of Use.
Mirena prescribing information
INDICATIONS AND USAGE
Mirena is a progestin-containing intrauterine system (IUS) indicated for:
Contraception
Mirena is indicated for prevention of pregnancy for up to 8 years; replace after the end of the eighth year.
Heavy Menstrual Bleeding
Mirena is indicated for the treatment of heavy menstrual bleeding for up to 5 years in women who choose to use intrauterine contraception as their method of contraception; replace after the end of the fifth year if continued treatment of heavy menstrual bleeding is needed.
DOSAGE AND ADMINISTRATION
- Release rate of levonorgestrel (LNG) is 21 mcg/day after 24 days; this rate is reduced to about 11 mcg/day after 5 years and 7 mcg/day after 8 years. (2.1 )
- To be inserted by a trained healthcare provider using strict aseptic technique. Follow insertion instructions exactly as described. (2.2 )
- Patient should be re-examined and evaluated 4 to 6 weeks after insertion; then, yearly or more often if clinically indicated. (2.3 )
Dosing Over Time
Mirena contains 52 mg of levonorgestrel (LNG) released in vivo, at a rate of approximately 21 mcg/day after 24 days. This rate decreases progressively to approximately 11 mcg/day after 5 years and 7 mcg/day after 8 years.
For contraception, remove Mirena by the end of the eighth year and replace at the time of removal with a new Mirena if continued use is desired.
For treatment of heavy menstrual bleeding, replace Mirena by the end of the fifth year if continued use is needed because data on use in this indication beyond 5 years are limited.
Mirena is supplied in a sterile package within an inserter that enables single-handed loading (see Figure 1). Do not open the package until required for insertion [see Description (11.2 )]. Do not use if the seal of the sterile package is broken or appears compromised. Use strict aseptic techniques throughout the insertion procedure [see Warnings and Precautions (5.3 )] .
Insertion Instructions
- Obtain a complete medical and social history to determine conditions that might influence the selection of a levonorgestrel-releasing intrauterine system (LNG IUS) for contraception . If indicated, perform a physical examination, and appropriate tests for any forms of genital or other sexually transmitted infections. [See Contraindications (4 ) and Warnings and Precautions (5.10 ).] Because irregular bleeding/spotting is common during the first months of Mirena use, exclude endometrial pathology (polyps or cancer) prior to the insertion of Mirena in women with persistent or uncharacteristic bleeding [see Warnings and Precautions (5.8 )].
- Follow the insertion instructions exactly as described to ensure proper placement and avoid premature release of Mirena from the inserter. Once released, Mirena cannot be re-loaded .
- Check expiration date of Mirena prior to initiating insertion.
- Mirena should be inserted by a trained healthcare provider. Healthcare providers should become thoroughly familiar with the insertion instructions before attempting insertion of Mirena.
- Insertion may be associated with some pain and/or bleeding or vasovagal reactions (for example, syncope, bradycardia), or with seizure, especially in patients with a predisposition to these conditions. Consider administering analgesics prior to insertion.
Timing of Insertion
Starting Mirena in women not currently using hormonal or intrauterine contraception |
|
Switching to Mirena from an oral, transdermal, or vaginal hormonal contraceptive |
|
Switching to Mirena from an injectable progestin contraceptive |
|
Switching to Mirena from a contraceptive implant or another IUS |
|
Inserting Mirena after first-trimester abortion or miscarriage |
|
Inserting Mirena after childbirth or second-trimester abortion or miscarriage | |
| |
Interval insertion following complete involution of the uterus |
|
Tools for Insertion
Note: The inserter provided with Mirena (see Figure 1) and the Insertion Procedure described in this section are not applicable for immediate insertion after childbirth or second-trimester abortion or miscarriage. For immediate insertion, remove Mirena from the inserter by first loading (see Figure 2) and then releasing (see Figure 7) Mirena from the inserter, and insert according to accepted practice.
Preparation
- Gloves
- Speculum
- Sterile uterine sound
- Sterile tenaculum
- Antiseptic solution, applicator
Procedure
- Sterile gloves
- Mirena with inserter in sealed package
- Instruments and anesthesia for paracervical block, if anticipated
- Consider having an unopened back-up Mirena available
- Sterile, sharp curved scissors
Preparation for insertion
- Exclude pregnancy and confirm that there are no other contraindications to the use of Mirena.
- With the patient comfortably in lithotomy position, do a bimanual exam to establish the size, shape and position of the uterus.
- Gently insert a speculum to visualize the cervix.
- Thoroughly cleanse the cervix and vagina with a suitable antiseptic solution.
- Prepare to sound the uterine cavity. Grasp the upper lip of the cervix with a tenaculum forceps and gently apply traction to stabilize and align the cervical canal with the uterine cavity. Perform a paracervical block if needed. If the uterus is retroverted, it may be more appropriate to grasp the lower lip of the cervix. The tenaculum should remain in position and gentle traction on the cervix should be maintained throughout the insertion procedure.
- Gently insert a uterine sound to check the patency of the cervix, measure the depth of the uterine cavity in centimeters, confirm cavity direction, and detect the presence of any uterine anomaly. If you encounter difficulty or cervical stenosis, use dilatation, and not force, to overcome resistance. If cervical dilatation is required, consider using a paracervical block.
- The uterus should sound to a depth of 6 to 10 cm. Insertion of Mirena into a uterine cavity less than 6 cm by sounding may increase the incidence of expulsion, bleeding, pain, perforation, and possibly pregnancy.
Insertion Procedure
Proceed with insertion only after completing the above steps and ascertaining that the patient is appropriate for Mirena. Ensure use of aseptic technique throughout the entire procedure .
Step 1–Opening of the package
- Open the package (Figure 1). The contents of the package are sterile.
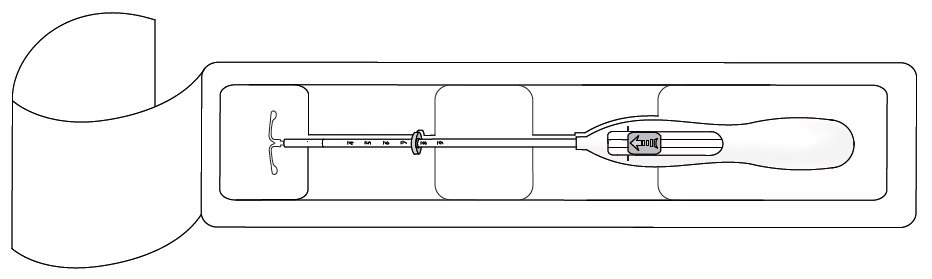
- Using sterile gloves lift the handle of the sterile inserter and remove from the sterile package.
Step 2–Load Mirena into the insertion tube
- Push the slider forward as far as possible in the direction of the arrow thereby moving the insertion tube over the Mirena T-body to load Mirena into the insertion tube (Figure 2). The tips of the arms will meet to form a rounded end that extends slightly beyond the insertion tube.
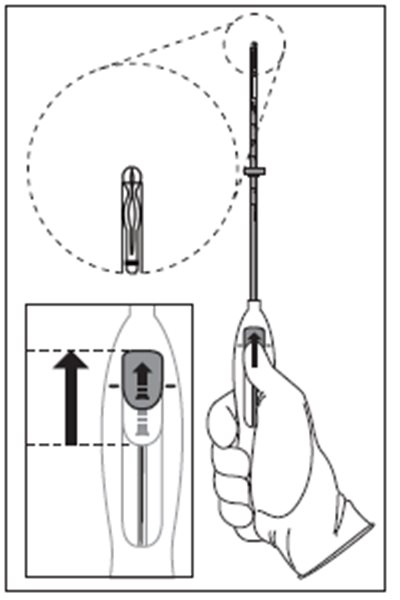
- Maintain forward pressure with your thumb or forefinger on the slider. DO NOT move the slider downward at this time as this may prematurely release the threads of Mirena. Once the slider is moved below the mark, Mirena cannot be re-loaded.
Step 3–Setting the Flange
- Holding the slider in this forward position, set the upper edge of the flange to correspond to the uterine depth (in centimeters) measured during sounding (Figure 3).
Step 4–Mirena is now ready to be inserted
- Continue holding the slider in this forward position. Advance the inserter through the cervix until the flange is approximately 1.5–2 cm from the cervix and then pause (Figure 4).
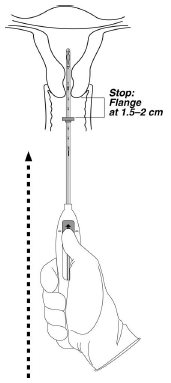
Do not force the inserter. If necessary, dilate the cervical canal.
Step 5–Open the arms
While holding the inserter steady, move the slider down to the mark to release the arms of Mirena (Figure 5). Wait 10 seconds for the horizontal arms to open completely.
Step 6–Advance to fundal position
- Advance the inserter gently towards the fundus of the uterus until the flange touches the cervix. If you encounter fundal resistance do not continue to advance. Mirena is now in the fundal position (Figure 6). Fundal positioning of Mirena is important to prevent expulsion.
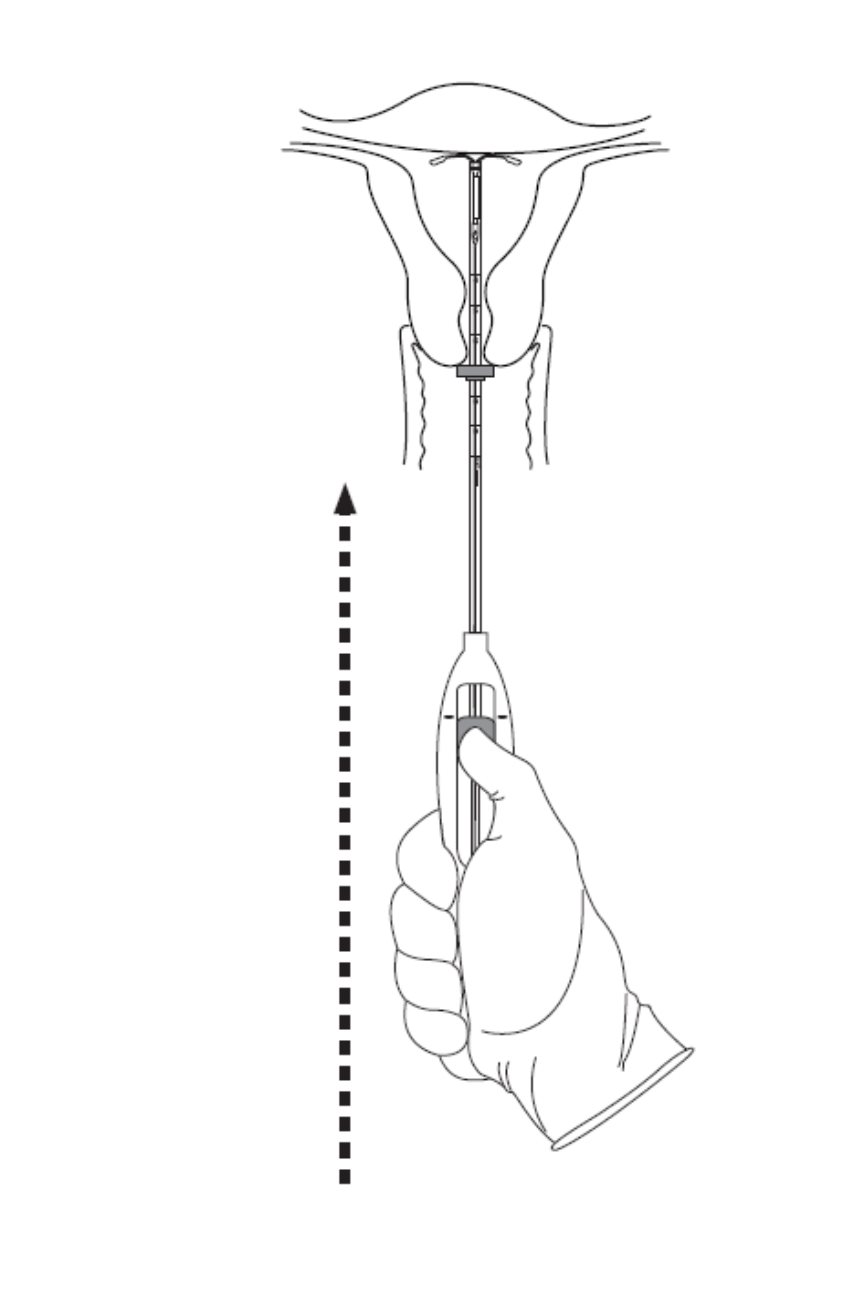
Step 7–Release Mirena and withdraw the inserter
- Holding the entire inserter firmly in place, release Mirena by moving the slider all the way down (Figure 7).
- Continue to hold the slider all the way down while you slowly and gently withdraw the inserter from the uterus.
- Using a sharp, curved scissor, cut the threads perpendicular, leaving about 3 cm visible outside of the cervix [cutting threads at an angle may leave sharp ends (Figure 8)]. Do not apply tension or pull on the threads when cutting to prevent displacing Mirena.
Mirena insertion is now complete. Prescribe analgesics, if indicated. Record the Mirena lot number in the patient records.
Important information to consider during or after insertion
- If you suspect that Mirena is not in the correct position, check placement (for example, using transvaginal ultrasound). Remove Mirena if it is not positioned completely within the uterus. Do not reinsert a removed Mirena.
- If there is clinical concern, exceptional pain or bleeding during or after insertion, take appropriate steps (such as physical examination and ultrasound) immediately to exclude perforation.
Patient Follow-up
Reexamine and evaluate patients 4 to 6 weeks after insertion and once a year thereafter, or more frequently if clinically indicated.
Removal of Mirena
Timing of Removal
- For contraception, remove Mirena by the end of the eighth year and replace at the time of removal with a new Mirena if continued use is desired. Replace Mirena by the end of the fifth year if continued treatment of heavy menstrual bleeding is needed.
- If pregnancy is not desired, remove Mirena during the first 7 days of the menstrual cycle, provided the woman is still experiencing regular menses. If removal will occur at other times during the cycle, or the woman does not experience regular menses, she is at risk of pregnancy; start a new contraceptive method a week prior to removal for these women. [See Dosage and Administration (2.5 ).]
Tools for Removal
Preparation
- Gloves
- Speculum
Procedure
- Sterile forceps
Removal Procedure
- Remove Mirena by applying gentle traction on the threads with forceps. (Figure 9).
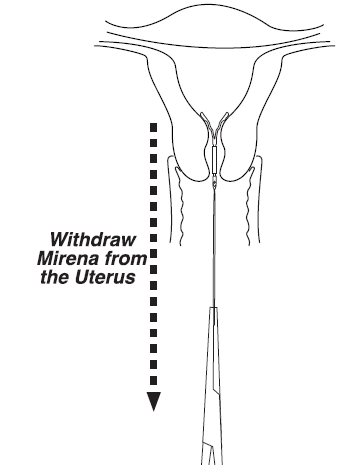
- If the threads are not visible, determine location of Mirena by ultrasound [see Warnings and Precautions (5.10 )] .
- If Mirena is found to be in the uterine cavity on ultrasound exam, it may be removed using a narrow forceps, such as an alligator forceps. This may require dilation of the cervical canal. After removal of Mirena, examine the system to ensure that it is intact. The hormone cylinder may slide over and cover the horizontal arms, giving the appearance of missing arms. This situation generally does not require further intervention once the system is verified to be intact.
- If unable to remove with gentle traction, determine Mirena location and exclude perforation by ultrasound or other imaging [ see Warnings and Precautions (5.10 )].
- Removal may be associated with:
- pain and/or bleeding, vasovagal reactions (for example, syncope, bradycardia) or seizure, especially in patients with a predisposition to these conditions.
- breakage or embedment of Mirena in the myometrium that can make removal difficult [see Warnings and Precautions (5.5 )] . Analgesia, paracervical anesthesia, cervical dilation, alligator forceps or other grasping instrument, or hysteroscopy may be used to assist in removal.
Continuation of Contraception after Removal
- If pregnancy is not desired and if a woman wishes to continue using Mirena, a new system can be inserted immediately after removal any time during the cycle.
- If a patient with regular cycles wants to start a different contraceptive method, time removal and initiation of the new method to ensure continuous contraception. Either remove Mirena during the first 7 days of the menstrual cycle and start the new method immediately thereafter or start the new method at least 7 days prior to removing Mirena if removal is to occur at other times during the cycle.
- If a patient with irregular cycles or amenorrhea wants to start a different contraceptive method, start the new method at least 7 days before removal.
DOSAGE FORMS AND STRENGTHS
Mirena is a LNG-releasing IUS (a type of intrauterine device, or IUD) consisting of a T-shaped polyethylene frame with a steroid reservoir containing a total of 52 mg LNG.
USE IN SPECIFIC POPULATIONS
Pregnancy
Risk Summary
The use of Mirena is contraindicated in pregnancy or with a suspected pregnancy and Mirena may cause adverse pregnancy outcomes [see Contraindications (4 ), Warnings and Precautions (5.1 , 5.2 )]. If a woman becomes pregnant with Mirena in place, the likelihood of ectopic pregnancy is increased and there is an increased risk of miscarriage, sepsis, premature labor, and premature delivery . Remove Mirena, if possible, if pregnancy occurs in a woman using Mirena. If Mirena cannot be removed, follow the pregnancy closely [see Warnings and Precautions (5.1 , 5.2 )] .
There have been isolated cases of virilization of the external genitalia of the female fetus following local exposure to LNG during pregnancy with an LNG IUS in place.
Lactation
Risk Summary
Published studies report the presence of LNG in human milk. Small amounts of progestins (approximately 0.1% of the total maternal doses) were detected in the breast milk of nursing mothers who used Mirena, resulting in exposure of LNG to the breastfed infants. There are no reports of adverse effects in breastfed infants with maternal use of progestin-only contraceptives. Isolated cases of decreased milk production have been reported with Mirena. The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for Mirena and any potential adverse effects on the breastfed child from Mirena or from the underlying maternal condition.
Females and Males of Reproductive Potential
Return to Fertility After Discontinuing Mirena
In two studies, return to fertility was investigated in a total of 229 women who desired pregnancy after study discontinuation and provided follow-up information. The probability to conceive within 12 months after removal of Mirena was approximately 80%.
Pediatric Use
Safety and efficacy of Mirena have been established in women of reproductive age. Efficacy is expected to be the same for postpubertal females under the age of 18 as for users 18 years and older. Use of this product before menarche is not indicated.
Geriatric Use
Mirena has not been studied in women over age 65 and is not approved for use in this population.
CONTRAINDICATIONS
The use of Mirena is contraindicated when one or more of the following conditions exist:
- Pregnancy or suspicion of pregnancy [see Warnings and Precautions (5.2 ), Use in Specific Populations (8.1 )]
- For use as post-coital contraception (emergency contraception)
- Congenital or acquired uterine anomaly including fibroids, that distorts the uterine cavity
- Acute pelvic inflammatory disease (PID) or a history of PID unless there has been a subsequent intrauterine pregnancy [see Warnings and Precautions (5.4 )]
- Postpartum endometritis or infected abortion in the past 3 months
- Known or suspected uterine or cervical malignancy
- Known or suspected breast cancer or other progestin-sensitive cancer, now or in the past
- Uterine bleeding of unknown etiology
- Untreated acute cervicitis or vaginitis, including bacterial vaginosis or other lower genital tract infections until infection is controlled
- Acute liver disease or liver tumor (benign or malignant)
- Conditions associated with increased susceptibility to pelvic infections [see Warnings and Precautions (5.4 )]
- A previously inserted intrauterine device (IUD) that has not been removed
- Hypersensitivity to any component of this product [see Adverse Reactions (6.2 ) and Description (11.1 )]
WARNINGS AND PRECAUTIONS
- Remove Mirena if pregnancy occurs with Mirena in place. If pregnancy occurs, there is increased risk of ectopic pregnancy including loss of fertility, pregnancy loss, septic abortion (including septicemia, shock and death), and premature labor and delivery. (5.1 , 5.2 )
- Group A streptococcal infection has been reported following insertion of LNG IUS; strict aseptic technique is essential during insertion. (5.3 )
- Before using Mirena, consider the risks of PID. (5.4 )
- Uterine perforation may occur and may reduce contraceptive effectiveness or require surgery. Risk is increased if inserted in lactating women and may be increased if inserted in women with fixed retroverted uteri or postpartum. (5.5)
- Partial or complete expulsion may occur, which can be unnoticed, leading to loss of contraceptive efficacy. (5.6 )
- Evaluate persistent enlarged ovarian follicles or ovarian cysts. (5.7 )
- Bleeding patterns become altered, may remain irregular and amenorrhea may ensue. (5.8 )
Risk of Ectopic Pregnancy
Evaluate women for ectopic pregnancy if they become pregnant with Mirena in place because the likelihood of a pregnancy being ectopic is increased with Mirena. Approximately one-half of pregnancies that occur with Mirena in place are likely to be ectopic. Also consider the possibility of ectopic pregnancy in the case of lower abdominal pain, especially in association with missed menses or if an amenorrheic woman starts bleeding.
The incidence of ectopic pregnancy in clinical trials with Mirena, which excluded women with a history of ectopic pregnancy, was approximately 0.1% per year. The risk of ectopic pregnancy, in women who have a history of ectopic pregnancy and use Mirena is unknown. Women with a previous history of ectopic pregnancy, tubal surgery or pelvic infection carry a higher risk of ectopic pregnancy. Ectopic pregnancy may result in loss of fertility.
Risks with Intrauterine Pregnancy
If pregnancy occurs while using Mirena, remove Mirena because leaving it in place may increase the risk of spontaneous abortion and preterm labor. Removal of Mirena or probing of the uterus may also result in spontaneous abortion. In the event of an intrauterine pregnancy with Mirena, consider the following:
Septic abortion
In patients becoming pregnant with an IUS in place, septic abortion - with septicemia, septic shock, and death - may occur.
Continuation of pregnancy
If a woman becomes pregnant with Mirena in place and if Mirena cannot be removed or the woman chooses not to have it removed, warn her that failure to remove Mirena increases the risk of miscarriage, sepsis, premature labor and premature delivery. Advise her of isolated reports of virilization of the female fetus following local exposure to LNG during pregnancy with an LNG IUS in place [see Use in Specific Populations (8.1 )]. Follow her pregnancy closely and advise her to report immediately any symptom that suggests complications of the pregnancy.
Sepsis
Severe infection or sepsis, including Group A streptococcal sepsis (GAS), have been reported following insertion of Mirena. In some cases, severe pain occurred within hours of insertion followed by sepsis within days. Because death from GAS is more likely if treatment is delayed, it is important to be aware of these rare but serious infections. Aseptic technique during insertion of Mirena is essential in order to minimize serious infections such as GAS.
Pelvic Infection
Promptly examine users with complaints of lower abdominal or pelvic pain, odorous discharge, unexplained bleeding, fever, genital lesions or sores. Remove Mirena in cases of recurrent endometritis or PID, or if an acute pelvic infection is severe or does not respond to treatment.
Pelvic Inflammatory Disease (PID)
Mirena is contraindicated in the presence of known or suspected PID or in women with a history of PID unless there has been a subsequent intrauterine pregnancy [see Contraindications (4 )]. IUDs have been associated with an increased risk of PID, most likely due to organisms being introduced into the uterus during insertion. In clinical trials, total combined upper genital infections were reported in 3.5% of Mirena users. More specifically, endometritis was reported in 2.1%, PID in 0.6%, and all other upper genital infections in ≤0.5% of women overall. These infections occurred more frequently within the first year. In a clinical trial with other IUDs 1 and a clinical trial with an IUD similar to Mirena, the highest rate occurred within the first month after insertion.
Women at increased risk for PID
PID is often associated with a sexually transmitted infection (STI), and Mirena does not protect against STI. The risk of PID is greater for women who have multiple sexual partners, and also for women whose sexual partner(s) have multiple sexual partners. Women who have had PID are at increased risk for a recurrence or re-infection. In particular, ascertain whether the woman is at increased risk of infection (for example, leukemia, acquired immune deficiency syndrome [AIDS], intravenous drug abuse).
Subclinical PID
PID may be asymptomatic but still result in tubal damage and its sequelae.
Treatment of PID
Following a diagnosis of PID, or suspected PID, bacteriologic specimens should be obtained, and antibiotic therapy should be initiated promptly. Removal of Mirena after initiation of antibiotic therapy is usually appropriate. 1
Actinomycosis
Actinomycosis has been associated with IUDs. Remove Mirena from symptomatic women and treat with antibiotics. The significance of actinomyces-like organisms on Pap smear in an asymptomatic IUD user is unknown, and so this finding alone does not always require Mirena removal and treatment. When possible, confirm a Pap smear diagnosis with cultures.
Perforation
Perforation (total or partial, including penetration/embedment of Mirena in the uterine wall or cervix) may occur most often during insertion, although the perforation may not be detected until sometime later. The incidence of perforation during clinical trials, which excluded breast-feeding women, was < 0.1%.
The risk of uterine perforation is increased in women who have recently given birth, and in women who are breastfeeding at the time of insertion. In a large postmarketing safety study conducted in the US, the risk of uterine perforation was highest when insertion occurred within ≤ 6 weeks postpartum, and also higher with breastfeeding at the time of insertion [see Adverse Reactions (6.2 )] .
The risk of perforation may be increased if Mirena is inserted when the uterus is fixed, retroverted or not completely involuted.
If perforation occurs, locate and remove Mirena. Surgery may be required. Delayed detection or removal of Mirena in case of perforation may result in migration outside the uterine cavity, adhesions, peritonitis, intestinal perforations, intestinal obstruction, abscesses and erosion of adjacent viscera. In addition, perforation may reduce contraceptive efficacy and result in pregnancy.
Expulsion
Partial or complete expulsion of Mirena may occur resulting in the loss of efficacy. Expulsion may be associated with symptoms of bleeding or pain, or it may be asymptomatic and go unnoticed. Mirena typically decreases menstrual bleeding over time; therefore, an increase of menstrual bleeding may be indicative of an expulsion. Consider further diagnostic imaging, such as x-ray, if expulsion is suspected based on ultrasound [see Warnings and Precautions (5.10)]. In clinical trials, a 4.5% expulsion rate was reported over the 5-year study duration.
The risk of expulsion is increased with insertions immediately after delivery and appears to be increased with insertion after second-trimester abortion based on limited data. In a large postmarketing safety study conducted in the US, the risk of expulsion was lower with breastfeeding status [see Adverse Reactions (6.2 )].
Remove a partially expelled Mirena. If expulsion has occurred, a new Mirena can be inserted any time the provider can be reasonably certain the woman is not pregnant.
Ovarian Cysts
Because the contraceptive effect of Mirena is mainly due to its local effects within the uterus, ovulatory cycles with follicular rupture usually occur in women of fertile age using Mirena. Ovarian cysts have been reported in approximately 8% of women using Mirena. Most cysts are asymptomatic, although some may be accompanied by pelvic pain or dyspareunia.
In most cases the ovarian cysts disappear spontaneously during two to three months observation. Evaluate persistent ovarian cysts. Surgical intervention is not usually required.
Bleeding Pattern Alterations
Mirena can alter the bleeding pattern and result in spotting, irregular bleeding, heavy bleeding, oligomenorrhea and amenorrhea. During the first 3–6 months of Mirena use, the number of bleeding and spotting days may be higher and bleeding patterns may be irregular. Thereafter the number of bleeding and spotting days usually decreases but bleeding may remain irregular. If bleeding irregularities develop during prolonged treatment, appropriate diagnostic measures should be taken to rule out endometrial pathology.
Amenorrhea develops in approximately 20% of Mirena users by one year.
If a significant change in bleeding develops during prolonged use, take appropriate diagnostic measures to rule out endometrial pathology. Consider the possibility of pregnancy if menstruation does not occur within six weeks of the onset of previous menstruation. Once pregnancy has been excluded, repeated pregnancy tests are generally not necessary in amenorrheic women unless indicated, for example, by other signs of pregnancy or by pelvic pain [see Clinical Studies (14.1 )].
In most women with heavy menstrual bleeding, the number of bleeding and spotting days may also increase during the initial months of therapy but usually decrease with continued use; the volume of blood loss per cycle progressively becomes reduced [see Clinical Studies (14.2 )].
Breast Cancer
Women who currently have or have had breast cancer, or have a suspicion of breast cancer, should not use hormonal contraception, including Mirena, because some breast cancers are hormone-sensitive [see Contraindications (4 )].
Spontaneous reports of breast cancer have been received during postmarketing experience with Mirena. Observational studies of the risk of breast cancer with use of a LNG-releasing IUS do not provide conclusive evidence of increased risk.
Clinical Considerations for Use and Removal
Use Mirena with caution after careful assessment if any of the following conditions exist, and consider removal of the system if any of them arise during use:
- Coagulopathy or use of anticoagulants
- Migraine, focal migraine with asymmetrical visual loss or other symptoms indicating transient cerebral ischemia
- Exceptionally severe headache
- Marked increase of blood pressure
- Severe arterial disease such as stroke or myocardial infarction
In addition, consider removing Mirena if any of the following conditions arise during use [see Contraindications (4 )] :
- Uterine or cervical malignancy
- Jaundice
If the threads are not visible or are significantly shortened, they may have broken or retracted into the cervical canal or uterus. Consider the possibility that the system may have been displaced (for example, expelled or perforated the uterus) [see Warnings and Precautions (5.5 , 5.6 )]. Exclude pregnancy and verify the location of Mirena, for example, by sonography, X-ray, or by gentle exploration of the cervical canal with a suitable instrument. If Mirena is displaced, remove it. A new Mirena may be inserted at that time or during the next menses if it is certain that conception has not occurred. If Mirena is in place with no evidence of perforation, no intervention is indicated.
ADVERSE REACTIONS
The following serious or otherwise important adverse reactions are discussed in elsewhere in the labeling:
- Ectopic Pregnancy [see Warnings and Precautions (5.1 )]
- Intrauterine Pregnancy [see Warnings and Precautions (5.2 )]
- Group A Streptococcal Sepsis (GAS) [see Warnings and Precautions (5.3 )]
- Pelvic Inflammatory Disease [see Warnings and Precautions (5.4 )]
- Perforation [see Warnings and Precautions (5.5 )]
- Expulsion [see Warnings and Precautions (5.6 )]
- Ovarian Cysts [see Warnings and Precautions (5.7 )]
- Bleeding Pattern Alterations [see Warnings and Precautions (5.8 )]
Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
The data provided in Table 2 reflect the experience with the use of Mirena in the adequate and well-controlled studies as well as in the supportive and uncontrolled studies for contraception and heavy menstrual bleeding (n=5,091). The data cover more than 12,101 women-years of exposure up to 5 years of use, mainly in the contraception studies (11,761 women-years). The frequencies of reported adverse drug reactions represent crude incidences.
The most common adverse reactions (≥10% users) are alterations of menstrual bleeding patterns [including unscheduled uterine bleeding (31.9%), decreased uterine bleeding (23.4%), increased scheduled uterine bleeding (11.9%), and female genital tract bleeding (3.5%)], abdominal/pelvic pain (22.6%), amenorrhea (18.4%), headache/migraine (16.3%), genital discharge (14.9%), and vulvovaginitis (10.5%). Adverse reactions reported in ≥ 5% of users are shown in Table 2.
System Organ Class | Adverse Reactions | % (N= 5,091) |
Reproductive system and breast disorders | alteration of menstrual bleeding pattern, including: unscheduled uterine bleeding decreased uterine bleeding increased scheduled uterine bleeding female genital tract bleeding | 31.9 23.4 11.9 3.5 |
amenorrhea | 18.4 | |
genital discharge | 14.9 | |
vulvovaginitis | 10.5 | |
breast pain | 8.5 | |
benign ovarian cyst and associated complications | 7.5 | |
dysmenorrhea | 6.4 | |
Gastrointestinal disorders | abdominal/pelvic pain | 22.6 |
Nervous system disorders | headache/migraine | 16.3 |
Musculoskeletal and connective tissue disorders | back pain | 7.9 |
Skin and subcutaneous tissue disorders | acne | 6.8 |
Psychiatric disorders | depression/depressive mood | 6.4 |
Other adverse reactions occurring in <5% of subjects include alopecia, (partial and complete) device expulsion, hirsutism, nausea, and PID/endometritis.
A separate study with 362 women who have used Mirena for more than 5 years showed a consistent adverse reaction profile in Years 6 through 8 as shown in Table 2. By the end of Year 8 of use, amenorrhea and infrequent bleeding are experienced by 34% and 26% of users, respectively; irregular bleeding occurs in 10%, frequent bleeding in 3%, and prolonged bleeding in 3% of users. In this study, 9% of women reported the adverse event of weight gain; it is unknown if the weight gain was caused by Mirena.
Postmarketing Experience
Adverse Reactions from Postmarketing Spontaneous Reports
The following adverse reactions have been identified during post approval use of Mirena. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
- Arterial thrombotic and venous thromboembolic events, including cases of pulmonary embolism, deep vein thrombosis and stroke
- Device breakage
- Hypersensitivity (including rash, urticaria and angioedema)
- Increased blood pressure
Reported Adverse Reactions from Postmarketing Studies
Assessment of Perforation and Expulsion of Intrauterine Devices (APEX IUD) Study
APEX IUD was a large US retrospective cohort study to assess the impact of breastfeeding and timing of postpartum IUD insertion on uterine perforation and IUD expulsion. The analyses included a total of 326,658 insertions, 30% (97,824 insertions) of which were performed in women with a delivery in the previous 12 months. For insertions performed in women who had delivered ≤ 52 weeks before IUD insertion, the majority of postpartum insertions, 57.3% (56,047 insertions) occurred between 6 and 14 weeks postpartum. Breastfeeding data were available in 94,817 insertions performed in women 52 weeks or less after delivery.
The study results indicated that the risk of uterine perforation was highest in women with IUD insertion ≤ 6 weeks postpartum. Immediate postpartum insertion (0–3 days) findings are limited due to the relatively small number of insertions occurring within this time interval. Women who were breastfeeding at the time of insertion were at 33% higher risk of perforation (adjusted hazard ratio [HR]=1.33, 95% confidence interval [CI]: 1.07–1.64) compared to women who were not breastfeeding at the time of insertion. Progressively lower risk of uterine perforation was observed in postpartum time windows beyond 6 weeks, in both breastfeeding and not breastfeeding women. Table 3 presents the uterine perforation rates for LNG IUS stratified by breastfeeding status and postpartum interval.
Breastfeeding at time of insertion | Not breastfeeding at time of insertion | |||
Postpartum interval at time of insertion | Number of events/ insertions | Uterine perforation rate per 1,000 insertions | Number of events/ insertions | Uterine perforation rate per 1,000 insertions |
0 to 3 days | 8/1,896 | 4.22 | 0/277 | 0.00 |
4 days to ≤ 6 weeks | 120/10,735 | 11.18 | 28/2,377 | 11.78 |
> 6 to ≤ 14 weeks | 268/29,677 | 9.03 | 80/12,011 | 6.66 |
> 14 to ≤ 52 weeks | 43/6,139 | 7.00 | 22/9,089 | 2.42 |
> 52 weeks or no delivery | no data available | 243/184,733 | 1.32 | |
Risk of expulsion was variable over the postpartum intervals through 52 weeks. Women who were breastfeeding were at 28% lower risk of IUD expulsion (adjusted HR=0.72, 95% CI: 0.64-0.80) compared to women who were not breastfeeding at time of insertion. Table 4 presents the IUD expulsion rates for LNG IUS stratified by breastfeeding status and postpartum interval.
Breastfeeding at time of insertion | Not breastfeeding at time of insertion | |||
Postpartum interval at time of insertion | Number of events/ insertions | Expulsion rate per 1,000 insertions | Number of events/ insertions | Expulsion rate per 1,000 insertions |
0 to 3 days | 187/1,896 | 98.63 | 12/277 | 43.32 |
4 days to ≤ 6 weeks | 185/10,735 | 17.23 | 52/2,377 | 21.88 |
> 6 to ≤ 14 weeks | 421/29,677 | 14.19 | 306/12,011 | 25.48 |
> 14 to ≤ 52 weeks | 120/6,139 | 19.55 | 273/9,089 | 30.04 |
> 52 weeks or no delivery | no data available | 5,481/184,733 | 29.67 | |
1 Expulsion includes both complete and partial expulsion
DRUG INTERACTIONS
No drug-drug interaction studies have been conducted with Mirena.
Drugs or herbal products that induce or inhibit LNG metabolizing enzymes, including CYP3A4, may decrease or increase, respectively, the serum concentrations of LNG during the use of Mirena. However, the contraceptive effect of Mirena is mediated via the direct release of LNG into the uterine cavity and is unlikely to be affected by drug interactions via enzyme induction or inhibition.
DESCRIPTION
Mirena (levonorgestrel-releasing intrauterine system) contains 52 mg of LNG, a progestin, and is intended to provide an initial release rate of LNG of approximately 21 mcg/day after 24 days.
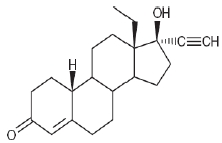
Levonorgestrel USP, (-)-13-Ethyl-17-hydroxy-18,19-dinor-17α-pregn-4-en-20-yn-3-one, the active ingredient in Mirena, has a molecular weight of 312.4, a molecular formula of C 21 H 28 O 2 , and the following structural formula:
Mirena
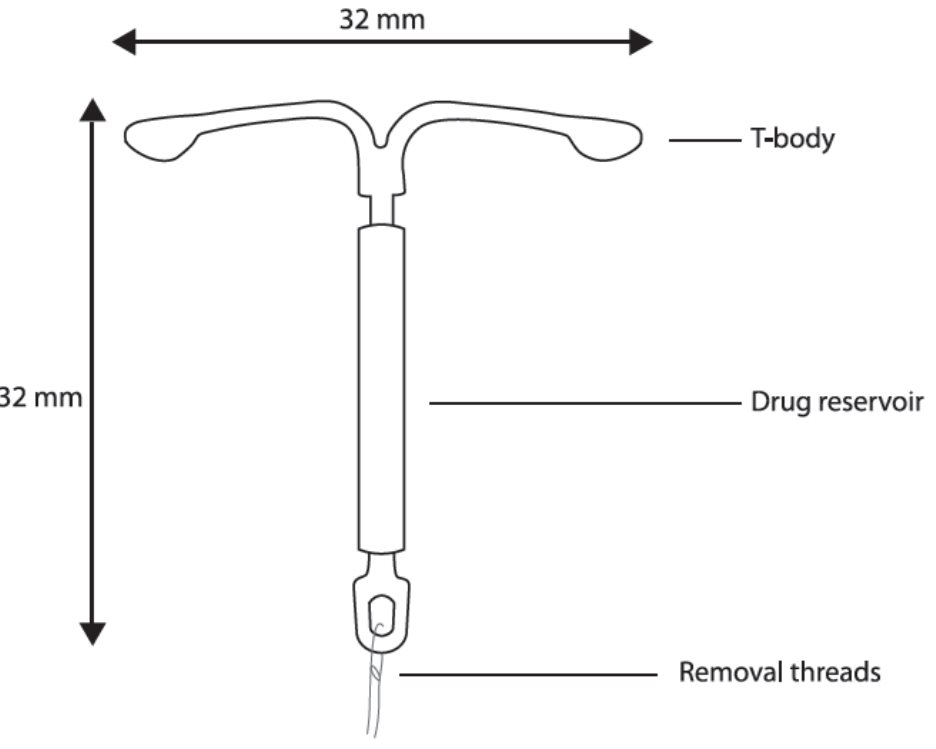
Mirena consists of a T-shaped polyethylene frame (T-body) with a steroid reservoir (hormone elastomer core) around the vertical stem. The white T-body has a loop at one end of the vertical stem and two horizontal arms at the other end. The reservoir consists of a white or almost white cylinder, made of a mixture of LNG and silicone (polydimethylsiloxane), containing a total of 52 mg LNG. The reservoir is covered by a semi-opaque silicone membrane, composed of polydimethylsiloxane and colloidal silica. The T-body is 32 mm in both the horizontal and vertical directions. The polyethylene of the T-body is compounded with barium sulfate, which makes it radiopaque. A monofilament brown polyethylene removal thread is attached to a loop at the end of the vertical stem of the T-body. The polyethylene of the removal thread contains iron oxide as a colorant (see Figure 10 ).
The components of Mirena, including its packaging, are not manufactured using natural rubber latex.
Inserter
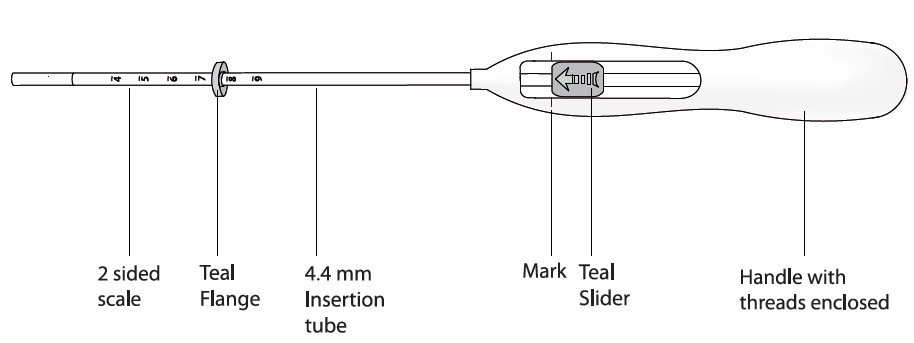
Mirena is packaged sterile within an inserter. The inserter (Figure 11), which is used for insertion of Mirena into the uterine cavity, consists of a symmetric two-sided body and slider that are integrated with flange, lock, pre-bent insertion tube and plunger. The outer diameter of the insertion tube is 4.4 mm. The vertical stem of Mirena is loaded in the insertion tube at the tip of the inserter. The arms are pre-aligned in the horizontal position. The removal threads are contained within the insertion tube and handle. Once Mirena has been placed, the inserter is discarded.
CLINICAL PHARMACOLOGY
Mechanism of Action
The local mechanism by which continuously released LNG contributes to the contraceptive effectiveness of Mirena has not been conclusively demonstrated. Studies of Mirena and similar LNG IUS prototypes have suggested several mechanisms that prevent pregnancy: thickening of cervical mucus preventing passage of sperm into the uterus, inhibition of sperm capacitation or survival, and alteration of the endometrium .
Pharmacodynamics
Mirena has mainly local progestogenic effects in the uterine cavity. The local concentrations of LNG lead to morphological changes including stromal pseudodecidualization, glandular atrophy, a leukocytic infiltration and a decrease in glandular and stromal mitoses.
Ovulation is inhibited in some women using Mirena. In a 1-year study, approximately 45% of menstrual cycles were ovulatory, and in another study after 4 years, 75% of cycles were ovulatory.
Pharmacokinetics
Absorption
Low doses of LNG are administered into the uterine cavity with the Mirena intrauterine delivery system.
Estimated in vivo release rates for different points in time are provided in Table 5.
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
After insertion of Mirena, LNG is detectable in serum/plasma after 1 hour. The maximum concentration is reached within 2 weeks after insertion and amounts to about 180 ng/L (CV 38%). In correspondence with the declining release rate, the geometric mean serum/plasma concentration of levonorgestrel declines continuously:
Time after insertion | Total LNG plasma concentrations [ng/L] (geometric CV%) |
24 days | 175 (37.6) |
2 months | 169 (37.1) |
1 year | 159 (37.4) |
3 years | 139 (37.8) |
5 years | 123 (38.2) |
8 years | 100 (39.9) |
Distribution
LNG is bound non-specifically to serum albumin and specifically to the Sex hormone-binding globulin (SHBG.) Less than 2% of the circulating LNG is present as free steroid. Levonorgestrel binds with high affinity to SHBG. Accordingly, changes in the concentration of SHBG in serum result in an increase (at higher SHBG concentrations) or in a decrease (at lower SHBG concentrations) of the total levonorgestrel concentration in serum. The concentration of SHBG declined on average by about 20% during the two months after insertion of Mirena and remained stable during thereafter, increasing only slightly until the end of the 8 years of use.
The apparent volume of distribution of LNG is reported to be approximately 1.8 L/kg.
Elimination
Following intravenous administration of 0.09 mg LNG to healthy volunteers, the total clearance of LNG is approximately 1 mL/min/kg and the elimination half-life is approximately 20 hours. Metabolic clearance rates may differ among individuals by several-fold, and this may account in part for wide individual variations in LNG concentrations seen in individuals using LNG–containing contraceptive products.
Metabolism
Following absorption, LNG is extensively metabolized. The most important metabolic pathways are the reduction of the Δ4-3-oxo group and hydroxylations at positions 2α, 1β and 16β, followed by conjugation. Significant amounts of conjugated and unconjugated 3α, 5β-tetra-hydrolevonorgestrel are also present in serum, along with much smaller amounts of 3α, 5α-tetrahydrolevonorgestrel and 16β-hydroxylevonorgestrel. CYP3A4 is the main enzyme involved in the oxidative metabolism of LNG.
Excretion
LNG and its phase I metabolites are excreted primarily as glucuronide conjugates. About 45% of LNG and its metabolites are excreted in the urine and about 32% are excreted in feces, mostly as glucuronide conjugates.
Specific Populations
Pediatric: Safety and efficacy of Mirena have been established in women of reproductive age. Use of this product before menarche is not indicated .
Geriatric: Mirena has not been studied in women over age 65 and is not currently approved for use in this population .
Race: No studies have evaluated the effect of race on the pharmacokinetics of Mirena.
Hepatic Impairment: No studies were conducted to evaluate the effect of hepatic disease on the disposition of Mirena .
Renal Impairment: No formal studies were conducted to evaluate the effect of renal disease on the disposition of Mirena.
Drug-Drug Interactions
No drug-drug interaction studies were conducted with Mirena [see Drug Interactions (7 )] .
NONCLINICAL TOXICOLOGY
Carcinogenesis, Mutagenesis, Impairment of Fertility
[See Warnings and Precautions (5.9 )]
CLINICAL STUDIES
Clinical Trials on Contraception
The safety and effectiveness of Mirena was studied in two clinical trials in Finland and Sweden. In these trials, 1,169 women 18 to 35 years of age at enrollment used Mirena for up to 5 years, for a total of 45,000 women-months of exposure. Of these, 5.6% (66) were nulliparous women. Subjects had previously been pregnant, had no history of ectopic pregnancy, had no history of pelvic inflammatory disease over the preceding 12 months, were predominantly White, and over 70% of the subjects had previously used IUDs (intrauterine devices). The reported 12-month pregnancy rates were less than or equal to 0.2 per 100 women (0.2%) and the cumulative 5-year pregnancy rate was approximately 0.7 per 100 women (0.7%).
The contraceptive efficacy of Mirena during extended use beyond 5 years was studied in the Mirena Extension Trial (NCT02985541), a multi-center, open-label, uncontrolled study conducted in the United States. The trial enrolled women 18 to 35 years of age who had been using Mirena for not less than 4.5 years and not more than 5 years at enrollment. The population consisted of 362 women using Mirena. Of these 47.2% were nulliparous. The women were predominantly White (75.4%); 14.1% of the women were Black/African American, and 2.5% were Asian; 11.3 % were Hispanic. The weight range was 38.5–163.5 kg (mean weight: 75.6 kg) and mean BMI was 27.9 kg/m 2 (range: 15.4–57.7 kg/m 2 ).
The pregnancy rate calculated as the Pearl Index (PI) was the primary efficacy endpoint used to assess contraceptive efficacy. The PI was based on 28-day equivalent exposure cycles; evaluable cycles excluded those in which back-up contraception was used unless a pregnancy occurred in that cycle. The PI for the 6th year of use based on the 1 pregnancy that occurred during Year 6 and within 7 days after Mirena removal or expulsion and 3,870 evaluable cycles was 0.34 with a 95% upper confidence limit of 1.88, and the PI for the 7th year of use based on the 1 pregnancy that occurred during Year 7 and within 7 days after Mirena removal or expulsion and 3,232 evaluable cycles was 0.40 with a 95% upper confidence limit of 2.25. The PI for the 8th year of use based on no pregnancies occurring during Year 8 and within 7 days after Mirena removal or expulsion and 2,534 evaluable cycles was 0.00 with a 95% upper confidence limit of 1.90.
The cumulative 3-year pregnancy rate for Years 6, 7 and 8 was estimated by the Kaplan-Meier method. Based on 2 pregnancies (1 in Year 6 and 1 in Year 7) and 10,216 exposure cycles, the cumulative pregnancy rate at the end of the 3-year period of extended use (Years 6, 7 and 8) was 0.68% with a 95% upper confidence limit of 2.71%.
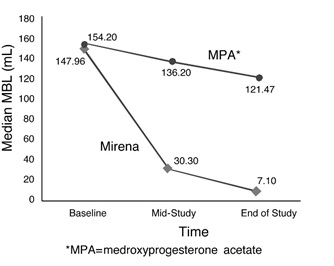
Clinical Trial on Heavy Menstrual Bleeding
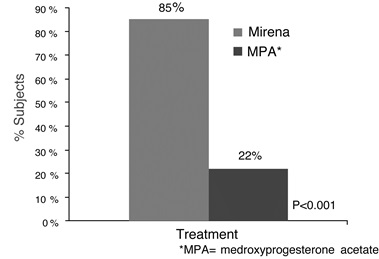
The efficacy of Mirena in the treatment of heavy menstrual bleeding was studied in a randomized, open-label, active-control, parallel-group trial comparing Mirena (n=79) to an approved therapy, medroxyprogesterone acetate (MPA) (n=81), over 6 cycles. The subjects included reproductive-aged women in good health, with no contraindications to the drug products and with confirmed heavy menstrual bleeding (≥ 80 mL menstrual blood loss [MBL]) determined using the alkaline hematin method. Excluded were women with organic or systemic conditions that may cause heavy uterine bleeding (except small fibroids, with total volume not > 5 mL). Treatment with Mirena showed a statistically significantly greater reduction in MBL (see Figure 12) and a statistically significantly greater number of subjects with successful treatment (see Figure 13). Successful treatment was defined as proportion of subjects with (1) end-of-study MBL < 80 mL and (2) a ≥ 50% decrease in MBL from baseline to end-of-study.
HOW SUPPLIED/STORAGE AND HANDLING
Mirena (levonorgestrel-releasing intrauterine system), containing a total of 52 mg LNG, is available in a carton of one sterile unit NDC# 50419-423-01.
Mirena is supplied sterile. Mirena is sterilized with ethylene oxide. Do not resterilize. For single use only. Do not use if the inner package is damaged or open. Insert before the end of the month shown on the label.
Store at 25°C (77°F); with excursions permitted between 15–30°C (59–86°F) [see USP Controlled Room Temperature].
Mechanism of Action
The local mechanism by which continuously released LNG contributes to the contraceptive effectiveness of Mirena has not been conclusively demonstrated. Studies of Mirena and similar LNG IUS prototypes have suggested several mechanisms that prevent pregnancy: thickening of cervical mucus preventing passage of sperm into the uterus, inhibition of sperm capacitation or survival, and alteration of the endometrium .