Modafinil
Modafinil Prescribing Information
Modafinil is indicated to improve wakefulness in adult patients with excessive sleepiness associated with narcolepsy, obstructive sleep apnea (OSA), or shift work disorder (SWD).
In OSA, modafinil is indicated to treat excessive sleepiness and not as treatment for the underlying obstruction. If continuous positive airway pressure (CPAP) is the treatment of choice for a patient, a maximal effort to treat with CPAP for an adequate period of time should be made prior to initiating and during treatment with modafinil for excessive sleepiness.
- 100 mg – capsule-shaped, white to off white, tablet, debossed with "PROVIGIL" on one side and "100 MG" on the other.
- 200 mg – capsule-shaped, white to off white, scored, tablet, debossed with "PROVIGIL" on one side and "200 MG" on the other.
Modafinil is contraindicated in patients with known hypersensitivity to modafinil or armodafinil or its inactive ingredients
Serious rash requiring hospitalization and discontinuation of treatment has been reported in association with the use of modafinil.
In clinical trials of modafinil, the incidence of rash resulting in discontinuation was approximately 0.8% (13 per 1,585) in pediatric patients (age <17 years); these rashes included 1 case of possible Stevens-Johnson Syndrome (SJS) and 1 case of apparent multi-organ hypersensitivity reaction. Several of the cases were associated with fever and other abnormalities (e.g., vomiting, leukopenia). The median time to rash that resulted in discontinuation was 13 days. No such cases were observed among 380 pediatric patients who received placebo. Modafinil is not approved for use in pediatric patients for any indication
Rare cases of serious or life-threatening rash, including SJS, Toxic Epidermal Necrolysis (TEN), and Drug Rash with Eosinophilia and Systemic Symptoms (DRESS) have been reported in adults and children in worldwide postmarketing experience. The reporting rate of TEN and SJS associated with modafinil use, which is generally accepted to be an underestimate due to underreporting, exceeds the background incidence rate. Estimates of the background incidence rate for these serious skin reactions in the general population range between 1 to 2 cases per million-person years.
There are no factors that are known to predict the risk of occurrence or the severity of rash associated with modafinil. Nearly all cases of serious rash associated with modafinil occurred within 1 to 5 weeks after treatment initiation. However, isolated cases have been reported after prolonged treatment (e.g., 3 months). Accordingly, duration of therapy cannot be relied upon as a means to predict the potential risk heralded by the first appearance of a rash.
Although benign rashes also occur with modafinil, it is not possible to reliably predict which rashes will prove to be serious. Accordingly, modafinil should be discontinued at the first sign of rash, unless the rash is clearly not drug-related. Discontinuation of treatment may not prevent a rash from becoming life-threatening or permanently disabling or disfiguring.
Angioedema and hypersensitivity (with rash, dysphagia, and bronchospasm), were observed in patients treated with armodafinil, the R enantiomer of modafinil (which is the racemic mixture). No such cases were observed in modafinil clinical trials. However, angioedema has been reported in postmarketing experience with modafinil. Patients should be advised to discontinue therapy and immediately report to their physician any signs or symptoms suggesting angioedema or anaphylaxis (e.g., swelling of face, eyes, lips, tongue or larynx; difficulty in swallowing or breathing; hoarseness).
Multi-organ hypersensitivity reactions, including at least one fatality in postmarketing experience, have occurred in close temporal association (median time to detection 13 days: range 4-33) to the initiation of modafinil.
Although there have been a limited number of reports, multi-organ hypersensitivity reactions may result in hospitalization or be life-threatening. There are no factors that are known to predict the risk of occurrence or the severity of multi-organ hypersensitivity reactions. Signs and symptoms of this disorder were diverse; however, patients typically, although not exclusively, presented with fever and rash associated with other organ system involvement. Other associated manifestations included myocarditis, hepatitis, liver function test abnormalities, hematological abnormalities (e.g., eosinophilia, leukopenia, thrombocytopenia), pruritus, and asthenia. Because multi-organ hypersensitivity is variable in its expression, other organ system symptoms and signs, not noted here, may occur.
If a multi-organ hypersensitivity reaction is suspected, modafinil should be discontinued. Although there are no case reports to indicate cross‑sensitivity with other drugs that produce this syndrome, the experience with drugs associated with multi-organ hypersensitivity would indicate this to be a possibility.
The following serious adverse reactions are described elsewhere in the labeling:
- Serious Rash, including Stevens-Johnson Syndrome [see Warnings and Precautions ()]
5.1 Serious Rash, including Stevens-Johnson SyndromeSerious rash requiring hospitalization and discontinuation of treatment has been reported in association with the use of modafinil.
In clinical trials of modafinil, the incidence of rash resulting in discontinuation was approximately 0.8% (13 per 1,585) in pediatric patients (age <17 years); these rashes included 1 case of possible Stevens-Johnson Syndrome (SJS) and 1 case of apparent multi-organ hypersensitivity reaction. Several of the cases were associated with fever and other abnormalities (e.g., vomiting, leukopenia). The median time to rash that resulted in discontinuation was 13 days. No such cases were observed among 380 pediatric patients who received placebo. Modafinil is not approved for use in pediatric patients for any indication
[see Use in Specific Populations (8.4)].Rare cases of serious or life-threatening rash, including SJS, Toxic Epidermal Necrolysis (TEN), and Drug Rash with Eosinophilia and Systemic Symptoms (DRESS) have been reported in adults and children in worldwide postmarketing experience. The reporting rate of TEN and SJS associated with modafinil use, which is generally accepted to be an underestimate due to underreporting, exceeds the background incidence rate. Estimates of the background incidence rate for these serious skin reactions in the general population range between 1 to 2 cases per million-person years.
There are no factors that are known to predict the risk of occurrence or the severity of rash associated with modafinil. Nearly all cases of serious rash associated with modafinil occurred within 1 to 5 weeks after treatment initiation. However, isolated cases have been reported after prolonged treatment (e.g., 3 months). Accordingly, duration of therapy cannot be relied upon as a means to predict the potential risk heralded by the first appearance of a rash.
Although benign rashes also occur with modafinil, it is not possible to reliably predict which rashes will prove to be serious. Accordingly, modafinil should be discontinued at the first sign of rash, unless the rash is clearly not drug-related. Discontinuation of treatment may not prevent a rash from becoming life-threatening or permanently disabling or disfiguring.
- Angioedema and Anaphylaxis Reactions [see Warnings and Precautions ()]
5.2 Angioedema and Anaphylaxis ReactionsAngioedema and hypersensitivity (with rash, dysphagia, and bronchospasm), were observed in patients treated with armodafinil, the R enantiomer of modafinil (which is the racemic mixture). No such cases were observed in modafinil clinical trials. However, angioedema has been reported in postmarketing experience with modafinil. Patients should be advised to discontinue therapy and immediately report to their physician any signs or symptoms suggesting angioedema or anaphylaxis (e.g., swelling of face, eyes, lips, tongue or larynx; difficulty in swallowing or breathing; hoarseness).
- Multi-organ Hypersensitivity Reactions [see Warnings and Precautions ()]
5.3 Multi-organ Hypersensitivity ReactionsMulti-organ hypersensitivity reactions, including at least one fatality in postmarketing experience, have occurred in close temporal association (median time to detection 13 days: range 4-33) to the initiation of modafinil.
Although there have been a limited number of reports, multi-organ hypersensitivity reactions may result in hospitalization or be life-threatening. There are no factors that are known to predict the risk of occurrence or the severity of multi-organ hypersensitivity reactions. Signs and symptoms of this disorder were diverse; however, patients typically, although not exclusively, presented with fever and rash associated with other organ system involvement. Other associated manifestations included myocarditis, hepatitis, liver function test abnormalities, hematological abnormalities (e.g., eosinophilia, leukopenia, thrombocytopenia), pruritus, and asthenia. Because multi-organ hypersensitivity is variable in its expression, other organ system symptoms and signs, not noted here, may occur.
If a multi-organ hypersensitivity reaction is suspected, modafinil should be discontinued. Although there are no case reports to indicate cross‑sensitivity with other drugs that produce this syndrome, the experience with drugs associated with multi-organ hypersensitivity would indicate this to be a possibility.
- Persistent Sleepiness [see Warnings and Precautions ()]
5.4 Persistent SleepinessPatients with abnormal levels of sleepiness who take modafinil should be advised that their level of wakefulness may not return to normal. Patients with excessive sleepiness, including those taking modafinil, should be frequently reassessed for their degree of sleepiness and, if appropriate, advised to avoid driving or any other potentially dangerous activity. Prescribers should also be aware that patients may not acknowledge sleepiness or drowsiness until directly questioned about drowsiness or sleepiness during specific activities.
- Psychiatric Symptoms [see Warnings and Precautions ()]
5.5 Psychiatric SymptomsPsychiatric adverse reactions have been reported in patients treated with modafinil.
In the adult modafinil controlled trials, psychiatric symptoms resulting in treatment discontinuation (at a frequency ≥0.3%) and reported more often in patients treated with modafinil compared to those treated with placebo were anxiety (1%), nervousness (1%), insomnia (<1%), confusion (<1%), agitation (<1%), and depression (<1%).
Postmarketing adverse reactions associated with the use of modafinil have included mania, delusions, hallucinations, suicidal ideation, and aggression, some resulting in hospitalization. Many, but not all, patients had a prior psychiatric history. One healthy male volunteer developed ideas of reference, paranoid delusions, and auditory hallucinations in association with multiple daily 600 mg doses of modafinil (three times the recommended dose) and sleep deprivation. There was no evidence of psychosis 36 hours after drug discontinuation.
Caution should be exercised when modafinil is given to patients with a history of psychosis, depression, or mania. Consideration should be given to the possible emergence or exacerbation of psychiatric symptoms in patients treated with modafinil. If psychiatric symptoms develop in association with modafinil administration, consider discontinuing modafinil.
- Effects on Ability to Drive and Use Machinery [see Warnings and Precautions ()]
5.6 Effects on Ability to Drive and Use MachineryAlthough modafinil has not been shown to produce functional impairment, any drug affecting the CNS may alter judgment, thinking or motor skills. Patients should be cautioned about operating an automobile or other hazardous machinery until it is reasonably certain that modafinil therapy will not adversely affect their ability to engage in such activities.
- Cardiovascular Events [see Warnings and Precautions ()]
5.7 Cardiovascular EventsIn modafinil clinical studies, cardiovascular adverse reactions, including chest pain, palpitations, dyspnea, and transient ischemic T-wave changes on ECG occurred in three subjects in association with mitral valve prolapse or left ventricular hypertrophy. In a Canadian clinical trial, a 35 year old obese narcoleptic male with a prior history of syncopal episodes experienced a 9-second episode of asystole after 27 days of modafinil treatment (300 mg/day in divided doses). Modafinil is not recommended in patients with a history of left ventricular hypertrophy or in patients with mitral valve prolapse who have experienced the mitral valve prolapse syndrome when previously receiving CNS stimulants. Findings suggestive of mitral valve prolapse syndrome include but are not limited to ischemic ECG changes, chest pain, or arrhythmia. If new onset of any of these findings occurs, consider cardiac evaluation. Consider increased monitoring in patients with a recent history of myocardial infarction or unstable angina.
Blood pressure monitoring in short term (≤ 3 months) controlled trials showed no clinically significant changes in mean systolic and diastolic blood pressure in patients receiving modafinil as compared to placebo. However, a retrospective analysis of the use of antihypertensive medication in these studies showed that a greater proportion of patients on modafinil required new or increased use of antihypertensive medications (2.4%) compared to patients on placebo (0.7%). The differential use was slightly larger when only studies in OSA were included, with 3.4% of patients on modafinil and 1.1% of patients on placebo requiring such alterations in the use of antihypertensive medication. Increased monitoring of heart rate and blood pressure may be appropriate in patients on modafinil. Caution should be exercised when prescribing modafinil to patients with known cardiovascular disease.
The clearance of drugs that are substrates for CYP3A4/5 (e.g., steroidal contraceptives, cyclosporine, midazolam, and triazolam) may be increased by modafinil via induction of metabolic enzymes, which results in lower systemic exposure. Dosage adjustment of these drugs should be considered when these drugs are used concomitantly with modafinil
Modafinil is a 1:1 racemic compound, whose enantiomers have different pharmacokinetics (e.g., the half-life of R-modafinil is approximately three times that of S-modafinil in adult humans). The enantiomers do not interconvert. At steady state, total exposure to R-modafinil is approximately three times that for S-modafinil. The trough concentration (Cmin,ss) of circulating modafinil after once daily dosing consists of 90% of R-modafinil and 10% of S-modafinil. The effective elimination half-life of modafinil after multiple doses is about 15 hours. The enantiomers of modafinil exhibit linear kinetics upon multiple dosing of 200-600 mg/day once daily in healthy volunteers. Apparent steady states of total modafinil and R-modafinil are reached after 2-4 days of dosing.
Modafinil is readily absorbed after oral administration, with peak plasma concentrations occurring at 2-4 hours. The bioavailability of modafinil tablets is approximately equal to that of an aqueous suspension. The absolute oral bioavailability was not determined due to the aqueous insolubility (<1 mg/mL) of modafinil, which precluded intravenous administration. Food has no effect on overall modafinil bioavailability; however, time to reach peak concentration (tmax) may be delayed by approximately one hour if taken with food.
Modafinil has an apparent volume of distribution of approximately 0.9 L/kg. In human plasma, in vitro, modafinil is moderately bound to plasma protein (approximately 60%), mainly to albumin. The potential for interactions of modafinil with highly protein-bound drugs is considered to be minimal.
The major route of elimination is metabolism (approximately 90%), primarily by the liver, with subsequent renal elimination of the metabolites. Urine alkalinization has no effect on the elimination of modafinil.
Metabolism occurs through hydrolytic deamidation, S-oxidation, aromatic ring hydroxylation, and glucuronide conjugation. Less than 10% of an administered dose is excreted as the parent compound. In a clinical study using radiolabeled modafinil, a total of 81% of the administered radioactivity was recovered in 11 days post-dose, predominantly in the urine (80% vs. 1.0% in the feces). The largest fraction of the drug in urine was modafinil acid, but at least six other metabolites were present in lower concentrations. Only two metabolites reach appreciable concentrations in plasma, i.e., modafinil acid and modafinil sulfone. In preclinical models, modafinil acid, modafinil sulfone, 2-[(diphenylmethyl)sulfonyl]acetic acid and 4-hydroxy modafinil, were inactive or did not appear to mediate the arousal effects of modafinil.
In adults, decreases in trough levels of modafinil have sometimes been observed after multiple weeks of dosing, suggesting auto-induction, but the magnitude of the decreases and the inconsistency of their occurrence suggest that their clinical significance is minimal. Significant accumulation of modafinil sulfone has been observed after multiple doses due to its long elimination half-life of 40 hours. Auto-induction of metabolizing enzymes, most importantly cytochrome P-450 CYP3A4, has also been observed in vitro after incubation of primary cultures of human hepatocytes with modafinil and in vivo after extended administration of modafinil at 400 mg/day.
A slight decrease (approximately 20%) in the oral clearance (CL/F) of modafinil was observed in a single dose study at 200 mg in 12 subjects with a mean age of 63 years (range 53 – 72 years), but the change was considered not likely to be clinically significant. In a multiple dose study (300 mg/day) in 12 patients with a mean age of 82 years (range 67 – 87 years), the mean levels of modafinil in plasma were approximately two times those historically obtained in matched younger subjects. Due to potential effects from the multiple concomitant medications with which most of the patients were being treated, the apparent difference in modafinil pharmacokinetics may not be attributable solely to the effects of aging. However, the results suggest that the clearance of modafinil may be reduced in the elderly
The pharmacokinetics of modafinil are not affected by gender.
The influence of race on the pharmacokinetics of modafinil has not been studied.
In a single dose 200 mg modafinil study, severe chronic renal failure (creatinine clearance ≤20 mL/min) did not significantly influence the pharmacokinetics of modafinil, but exposure to modafinil acid (an inactive metabolite) was increased 9-fold.
The pharmacokinetics and metabolism of modafinil were examined in patients with cirrhosis of the liver (6 men and 3 women). Three patients had stage B or B+ cirrhosis and 6 patients had stage C or C+ cirrhosis (per the Child-Pugh score criteria). Clinically 8 of 9 patients were icteric and all had ascites. In these patients, the oral clearance of modafinil was decreased by about 60% and the steady state concentration was doubled compared to normal patients
In vitro data demonstrated that modafinil weakly induces CYP1A2, CYP2B6, and possibly CYP3A activities in a concentration-related manner and that CYP2C19 activity is reversibly inhibited by modafinil. In vitro data also demonstrated that modafinil produced an apparent concentration-related suppression of expression of CYP2C9 activity. Other CYP activities did not appear to be affected by modafinil.
The existence of multiple pathways for modafinil metabolism, as well as the fact that a non-CYP-related pathway is the most rapid in metabolizing modafinil, suggest that there is a low probability of substantive effects on the overall pharmacokinetic profile of modafinil due to CYP inhibition by concomitant medications. However, due to the partial involvement of CYP3A enzymes in the metabolic elimination of modafinil, coadministration of potent inducers of CYP3A4/5 (e.g., carbamazepine, phenobarbital, rifampin) or inhibitors of CYP3A4/5 (e.g., ketoconazole, erythromycin) could alter the plasma concentrations of modafinil.
- Drugs Metabolized by CYP3A4/5
- In vitro data demonstrated that modafinil is a weak inducer of CYP3A activity in a concentration-related manner. Therefore, the blood levels and effectiveness of drugs that are substrates for CYP3A enzymes (e.g., steroidal contraceptives, cyclosporine, midazolam, and triazolam) may be reduced after initiation of concomitant treatment with modafinil[see Drug Interactions ].
- Ethinyl Estradiol - Administration of modafinil to female volunteers once daily at 200 mg/day for 7 days followed by 400 mg/day for 21 days resulted in a mean 11% decrease in mean Cmaxand 18% decrease in mean AUC0-24of ethinyl estradiol (EE2; 0.035 mg; administered orally with norgestimate). There was no apparent change in the elimination rate of ethinyl estradiol.
- Triazolam - In the drug interaction study between modafinil and ethinyl estradiol (EE2), on the same days as those for the plasma sampling for EE2pharmacokinetics, a single dose of triazolam (0.125 mg) was also administered. Mean Cmaxand AUC0-∞of triazolam were decreased by 42% and 59%, respectively, and its elimination half-life was decreased by approximately an hour after the modafinil treatment.
- Cyclosporine - One case of an interaction between modafinil and cyclosporine, a substrate of CYP3A4, has been reported in a 41 year old woman who had undergone an organ transplant. After one month of administration of 200 mg/day of modafinil, cyclosporine blood levels were decreased by 50%. The interaction was postulated to be due to the increased metabolism of cyclosporine, since no other factor expected to affect the disposition of the drug had changed.
- Midazolam - In a clinical study, concomitant administration of armodafinil 250 mg resulted in a reduction in systemic exposure to midazolam by 32% after a single oral dose (5 mg) and 17% after a single intravenous dose (2 mg).
- Quetiapine - In a separate clinical study, concomitant administration of armodafinil 250 mg with quetiapine (300 mg to 600 mg daily doses) resulted in a reduction in the mean systemic exposure of quetiapine by approximately 29%.
- Drugs Metabolized by CYP1A2
- In vitro data demonstrated that modafinil is a weak inducer of CYP1A2 in a concentration-related manner. However, in a clinical study with armodafinil using caffeine as a probe substrate, no significant effect on CYP1A2 activity was observed.
- Drugs Metabolized by CYP2B6
- In vitro data demonstrated that modafinil is a weak inducer of CYP2B6 activity in a concentration-related manner.
- Drugs Metabolized by CYP2C9
- In vitro data demonstrated that modafinil produced an apparent concentration-related suppression of expression of CYP2C9 activity suggesting that there is a potential for a metabolic interaction between modafinil and the substrates of this enzyme (e.g., S-warfarin and phenytoin)[see Drug Interactions ].
- Warfarin: Concomitant administration of modafinil with warfarin did not produce significant changes in the pharmacokinetic profiles of R- and S-warfarin. However, since only a single dose of warfarin was tested in this study, an interaction cannot be ruled out[see Drug Interactions ].
- Drugs Metabolized by CYP2C19
- In vitro data demonstrated that modafinil is a reversible inhibitor of CYP2C19 activity. CYP2C19 is also reversibly inhibited, with similar potency, by a circulating metabolite, modafinil sulfone. Although the maximum plasma concentrations of modafinil sulfone are much lower than those of parent modafinil, the combined effect of both compounds could produce sustained partial inhibition of the enzyme. Therefore, exposure to some drugs that are substrates for CYP2C19 (e.g., phenytoin, diazepam, propranolol, omeprazole, and clomipramine) may be increased when used concomitantly with modafinil[see Drug Interactions ].
- In a clinical study, concomitant administration of armodafinil 400 mg resulted in a 40% increase in exposure to omeprazole after a single oral dose (40 mg), as a result of moderate inhibition of CYP2C19 activity.
- Interactions withCNSActive Drugs
- Concomitant administration of modafinil with methylphenidate or dextroamphetamine produced no significant alterations on the pharmacokinetic profile of modafinil or either stimulant, even though the absorption of modafinil was delayed for approximately one hour.
- Concomitant modafinil or clomipramine did not alter the pharmacokinetic profile of either drug; however, one incident of increased levels of clomipramine and its active metabolite desmethylclomipramine was reported in a patient with narcolepsy during treatment with modafinil.
- CYP2C19 also provides an ancillary pathway for the metabolism of certain tricyclic antidepressants (e.g., clomipramine and desipramine) and selective serotonin reuptake inhibitors that are primarily metabolized by CYP2D6. In tricyclic-treated patients deficient in CYP2D6 (i.e., those who are poor metabolizers of debrisoquine; 7-10% of the Caucasian population; similar or lower in other populations), the amount of metabolism by CYP2C19 may be substantially increased. Modafinil may cause elevation of the levels of the tricyclics in this subset of patients[see Drug Interactions ].
- Concomitant administration of armodafinil with quetiapine reduced the systemic exposure of quetiapine.
- Interaction with P-Glycoprotein
- An in vitro study demonstrated that armodafinil is a substrate of P-glycoprotein. The impact of inhibition of P-glycoprotein is not known.
The effectiveness of steroidal contraceptives may be reduced when used with modafinil and for one month after discontinuation of therapy. Alternative or concomitant methods of contraception are recommended for patients taking steroidal contraceptives (e.g., ethinyl estradiol) when treated concomitantly with modafinil and for one month after discontinuation of modafinil treatment.
Blood levels of cyclosporine may be reduced when used with modafinil. Monitoring of circulating cyclosporine concentrations and appropriate dosage adjustment for cyclosporine should be considered when used concomitantly with modafinil.
Elimination of drugs that are substrates for CYP2C19 (e.g., phenytoin, diazepam, propranolol, omeprazole, and clomipramine) may be prolonged by modafinil via inhibition of metabolic enzymes, with resultant higher systemic exposure. In individuals deficient in the CYP2D6 enzyme, the levels of CYP2D6 substrates which have ancillary routes of elimination through CYP2C19, such as tricyclic antidepressants and selective serotonin reuptake inhibitors, may be increased by co-administration of modafinil. Dose adjustments of these drugs and other drugs that are substrates for CYP2C19 may be necessary when used concomitantly with modafinil
Modafinil is a 1:1 racemic compound, whose enantiomers have different pharmacokinetics (e.g., the half-life of R-modafinil is approximately three times that of S-modafinil in adult humans). The enantiomers do not interconvert. At steady state, total exposure to R-modafinil is approximately three times that for S-modafinil. The trough concentration (Cmin,ss) of circulating modafinil after once daily dosing consists of 90% of R-modafinil and 10% of S-modafinil. The effective elimination half-life of modafinil after multiple doses is about 15 hours. The enantiomers of modafinil exhibit linear kinetics upon multiple dosing of 200-600 mg/day once daily in healthy volunteers. Apparent steady states of total modafinil and R-modafinil are reached after 2-4 days of dosing.
Modafinil is readily absorbed after oral administration, with peak plasma concentrations occurring at 2-4 hours. The bioavailability of modafinil tablets is approximately equal to that of an aqueous suspension. The absolute oral bioavailability was not determined due to the aqueous insolubility (<1 mg/mL) of modafinil, which precluded intravenous administration. Food has no effect on overall modafinil bioavailability; however, time to reach peak concentration (tmax) may be delayed by approximately one hour if taken with food.
Modafinil has an apparent volume of distribution of approximately 0.9 L/kg. In human plasma, in vitro, modafinil is moderately bound to plasma protein (approximately 60%), mainly to albumin. The potential for interactions of modafinil with highly protein-bound drugs is considered to be minimal.
The major route of elimination is metabolism (approximately 90%), primarily by the liver, with subsequent renal elimination of the metabolites. Urine alkalinization has no effect on the elimination of modafinil.
Metabolism occurs through hydrolytic deamidation, S-oxidation, aromatic ring hydroxylation, and glucuronide conjugation. Less than 10% of an administered dose is excreted as the parent compound. In a clinical study using radiolabeled modafinil, a total of 81% of the administered radioactivity was recovered in 11 days post-dose, predominantly in the urine (80% vs. 1.0% in the feces). The largest fraction of the drug in urine was modafinil acid, but at least six other metabolites were present in lower concentrations. Only two metabolites reach appreciable concentrations in plasma, i.e., modafinil acid and modafinil sulfone. In preclinical models, modafinil acid, modafinil sulfone, 2-[(diphenylmethyl)sulfonyl]acetic acid and 4-hydroxy modafinil, were inactive or did not appear to mediate the arousal effects of modafinil.
In adults, decreases in trough levels of modafinil have sometimes been observed after multiple weeks of dosing, suggesting auto-induction, but the magnitude of the decreases and the inconsistency of their occurrence suggest that their clinical significance is minimal. Significant accumulation of modafinil sulfone has been observed after multiple doses due to its long elimination half-life of 40 hours. Auto-induction of metabolizing enzymes, most importantly cytochrome P-450 CYP3A4, has also been observed in vitro after incubation of primary cultures of human hepatocytes with modafinil and in vivo after extended administration of modafinil at 400 mg/day.
A slight decrease (approximately 20%) in the oral clearance (CL/F) of modafinil was observed in a single dose study at 200 mg in 12 subjects with a mean age of 63 years (range 53 – 72 years), but the change was considered not likely to be clinically significant. In a multiple dose study (300 mg/day) in 12 patients with a mean age of 82 years (range 67 – 87 years), the mean levels of modafinil in plasma were approximately two times those historically obtained in matched younger subjects. Due to potential effects from the multiple concomitant medications with which most of the patients were being treated, the apparent difference in modafinil pharmacokinetics may not be attributable solely to the effects of aging. However, the results suggest that the clearance of modafinil may be reduced in the elderly
The pharmacokinetics of modafinil are not affected by gender.
The influence of race on the pharmacokinetics of modafinil has not been studied.
In a single dose 200 mg modafinil study, severe chronic renal failure (creatinine clearance ≤20 mL/min) did not significantly influence the pharmacokinetics of modafinil, but exposure to modafinil acid (an inactive metabolite) was increased 9-fold.
The pharmacokinetics and metabolism of modafinil were examined in patients with cirrhosis of the liver (6 men and 3 women). Three patients had stage B or B+ cirrhosis and 6 patients had stage C or C+ cirrhosis (per the Child-Pugh score criteria). Clinically 8 of 9 patients were icteric and all had ascites. In these patients, the oral clearance of modafinil was decreased by about 60% and the steady state concentration was doubled compared to normal patients
In vitro data demonstrated that modafinil weakly induces CYP1A2, CYP2B6, and possibly CYP3A activities in a concentration-related manner and that CYP2C19 activity is reversibly inhibited by modafinil. In vitro data also demonstrated that modafinil produced an apparent concentration-related suppression of expression of CYP2C9 activity. Other CYP activities did not appear to be affected by modafinil.
The existence of multiple pathways for modafinil metabolism, as well as the fact that a non-CYP-related pathway is the most rapid in metabolizing modafinil, suggest that there is a low probability of substantive effects on the overall pharmacokinetic profile of modafinil due to CYP inhibition by concomitant medications. However, due to the partial involvement of CYP3A enzymes in the metabolic elimination of modafinil, coadministration of potent inducers of CYP3A4/5 (e.g., carbamazepine, phenobarbital, rifampin) or inhibitors of CYP3A4/5 (e.g., ketoconazole, erythromycin) could alter the plasma concentrations of modafinil.
- Drugs Metabolized by CYP3A4/5
- In vitro data demonstrated that modafinil is a weak inducer of CYP3A activity in a concentration-related manner. Therefore, the blood levels and effectiveness of drugs that are substrates for CYP3A enzymes (e.g., steroidal contraceptives, cyclosporine, midazolam, and triazolam) may be reduced after initiation of concomitant treatment with modafinil[see Drug Interactions ].
- Ethinyl Estradiol - Administration of modafinil to female volunteers once daily at 200 mg/day for 7 days followed by 400 mg/day for 21 days resulted in a mean 11% decrease in mean Cmaxand 18% decrease in mean AUC0-24of ethinyl estradiol (EE2; 0.035 mg; administered orally with norgestimate). There was no apparent change in the elimination rate of ethinyl estradiol.
- Triazolam - In the drug interaction study between modafinil and ethinyl estradiol (EE2), on the same days as those for the plasma sampling for EE2pharmacokinetics, a single dose of triazolam (0.125 mg) was also administered. Mean Cmaxand AUC0-∞of triazolam were decreased by 42% and 59%, respectively, and its elimination half-life was decreased by approximately an hour after the modafinil treatment.
- Cyclosporine - One case of an interaction between modafinil and cyclosporine, a substrate of CYP3A4, has been reported in a 41 year old woman who had undergone an organ transplant. After one month of administration of 200 mg/day of modafinil, cyclosporine blood levels were decreased by 50%. The interaction was postulated to be due to the increased metabolism of cyclosporine, since no other factor expected to affect the disposition of the drug had changed.
- Midazolam - In a clinical study, concomitant administration of armodafinil 250 mg resulted in a reduction in systemic exposure to midazolam by 32% after a single oral dose (5 mg) and 17% after a single intravenous dose (2 mg).
- Quetiapine - In a separate clinical study, concomitant administration of armodafinil 250 mg with quetiapine (300 mg to 600 mg daily doses) resulted in a reduction in the mean systemic exposure of quetiapine by approximately 29%.
- Drugs Metabolized by CYP1A2
- In vitro data demonstrated that modafinil is a weak inducer of CYP1A2 in a concentration-related manner. However, in a clinical study with armodafinil using caffeine as a probe substrate, no significant effect on CYP1A2 activity was observed.
- Drugs Metabolized by CYP2B6
- In vitro data demonstrated that modafinil is a weak inducer of CYP2B6 activity in a concentration-related manner.
- Drugs Metabolized by CYP2C9
- In vitro data demonstrated that modafinil produced an apparent concentration-related suppression of expression of CYP2C9 activity suggesting that there is a potential for a metabolic interaction between modafinil and the substrates of this enzyme (e.g., S-warfarin and phenytoin)[see Drug Interactions ].
- Warfarin: Concomitant administration of modafinil with warfarin did not produce significant changes in the pharmacokinetic profiles of R- and S-warfarin. However, since only a single dose of warfarin was tested in this study, an interaction cannot be ruled out[see Drug Interactions ].
- Drugs Metabolized by CYP2C19
- In vitro data demonstrated that modafinil is a reversible inhibitor of CYP2C19 activity. CYP2C19 is also reversibly inhibited, with similar potency, by a circulating metabolite, modafinil sulfone. Although the maximum plasma concentrations of modafinil sulfone are much lower than those of parent modafinil, the combined effect of both compounds could produce sustained partial inhibition of the enzyme. Therefore, exposure to some drugs that are substrates for CYP2C19 (e.g., phenytoin, diazepam, propranolol, omeprazole, and clomipramine) may be increased when used concomitantly with modafinil[see Drug Interactions ].
- In a clinical study, concomitant administration of armodafinil 400 mg resulted in a 40% increase in exposure to omeprazole after a single oral dose (40 mg), as a result of moderate inhibition of CYP2C19 activity.
- Interactions withCNSActive Drugs
- Concomitant administration of modafinil with methylphenidate or dextroamphetamine produced no significant alterations on the pharmacokinetic profile of modafinil or either stimulant, even though the absorption of modafinil was delayed for approximately one hour.
- Concomitant modafinil or clomipramine did not alter the pharmacokinetic profile of either drug; however, one incident of increased levels of clomipramine and its active metabolite desmethylclomipramine was reported in a patient with narcolepsy during treatment with modafinil.
- CYP2C19 also provides an ancillary pathway for the metabolism of certain tricyclic antidepressants (e.g., clomipramine and desipramine) and selective serotonin reuptake inhibitors that are primarily metabolized by CYP2D6. In tricyclic-treated patients deficient in CYP2D6 (i.e., those who are poor metabolizers of debrisoquine; 7-10% of the Caucasian population; similar or lower in other populations), the amount of metabolism by CYP2C19 may be substantially increased. Modafinil may cause elevation of the levels of the tricyclics in this subset of patients[see Drug Interactions ].
- Concomitant administration of armodafinil with quetiapine reduced the systemic exposure of quetiapine.
- Interaction with P-Glycoprotein
- An in vitro study demonstrated that armodafinil is a substrate of P-glycoprotein. The impact of inhibition of P-glycoprotein is not known.
More frequent monitoring of prothrombin times/INR should be considered whenever modafinil is coadministered with warfarin
Modafinil is a 1:1 racemic compound, whose enantiomers have different pharmacokinetics (e.g., the half-life of R-modafinil is approximately three times that of S-modafinil in adult humans). The enantiomers do not interconvert. At steady state, total exposure to R-modafinil is approximately three times that for S-modafinil. The trough concentration (Cmin,ss) of circulating modafinil after once daily dosing consists of 90% of R-modafinil and 10% of S-modafinil. The effective elimination half-life of modafinil after multiple doses is about 15 hours. The enantiomers of modafinil exhibit linear kinetics upon multiple dosing of 200-600 mg/day once daily in healthy volunteers. Apparent steady states of total modafinil and R-modafinil are reached after 2-4 days of dosing.
Modafinil is readily absorbed after oral administration, with peak plasma concentrations occurring at 2-4 hours. The bioavailability of modafinil tablets is approximately equal to that of an aqueous suspension. The absolute oral bioavailability was not determined due to the aqueous insolubility (<1 mg/mL) of modafinil, which precluded intravenous administration. Food has no effect on overall modafinil bioavailability; however, time to reach peak concentration (tmax) may be delayed by approximately one hour if taken with food.
Modafinil has an apparent volume of distribution of approximately 0.9 L/kg. In human plasma, in vitro, modafinil is moderately bound to plasma protein (approximately 60%), mainly to albumin. The potential for interactions of modafinil with highly protein-bound drugs is considered to be minimal.
The major route of elimination is metabolism (approximately 90%), primarily by the liver, with subsequent renal elimination of the metabolites. Urine alkalinization has no effect on the elimination of modafinil.
Metabolism occurs through hydrolytic deamidation, S-oxidation, aromatic ring hydroxylation, and glucuronide conjugation. Less than 10% of an administered dose is excreted as the parent compound. In a clinical study using radiolabeled modafinil, a total of 81% of the administered radioactivity was recovered in 11 days post-dose, predominantly in the urine (80% vs. 1.0% in the feces). The largest fraction of the drug in urine was modafinil acid, but at least six other metabolites were present in lower concentrations. Only two metabolites reach appreciable concentrations in plasma, i.e., modafinil acid and modafinil sulfone. In preclinical models, modafinil acid, modafinil sulfone, 2-[(diphenylmethyl)sulfonyl]acetic acid and 4-hydroxy modafinil, were inactive or did not appear to mediate the arousal effects of modafinil.
In adults, decreases in trough levels of modafinil have sometimes been observed after multiple weeks of dosing, suggesting auto-induction, but the magnitude of the decreases and the inconsistency of their occurrence suggest that their clinical significance is minimal. Significant accumulation of modafinil sulfone has been observed after multiple doses due to its long elimination half-life of 40 hours. Auto-induction of metabolizing enzymes, most importantly cytochrome P-450 CYP3A4, has also been observed in vitro after incubation of primary cultures of human hepatocytes with modafinil and in vivo after extended administration of modafinil at 400 mg/day.
A slight decrease (approximately 20%) in the oral clearance (CL/F) of modafinil was observed in a single dose study at 200 mg in 12 subjects with a mean age of 63 years (range 53 – 72 years), but the change was considered not likely to be clinically significant. In a multiple dose study (300 mg/day) in 12 patients with a mean age of 82 years (range 67 – 87 years), the mean levels of modafinil in plasma were approximately two times those historically obtained in matched younger subjects. Due to potential effects from the multiple concomitant medications with which most of the patients were being treated, the apparent difference in modafinil pharmacokinetics may not be attributable solely to the effects of aging. However, the results suggest that the clearance of modafinil may be reduced in the elderly
The pharmacokinetics of modafinil are not affected by gender.
The influence of race on the pharmacokinetics of modafinil has not been studied.
In a single dose 200 mg modafinil study, severe chronic renal failure (creatinine clearance ≤20 mL/min) did not significantly influence the pharmacokinetics of modafinil, but exposure to modafinil acid (an inactive metabolite) was increased 9-fold.
The pharmacokinetics and metabolism of modafinil were examined in patients with cirrhosis of the liver (6 men and 3 women). Three patients had stage B or B+ cirrhosis and 6 patients had stage C or C+ cirrhosis (per the Child-Pugh score criteria). Clinically 8 of 9 patients were icteric and all had ascites. In these patients, the oral clearance of modafinil was decreased by about 60% and the steady state concentration was doubled compared to normal patients
In vitro data demonstrated that modafinil weakly induces CYP1A2, CYP2B6, and possibly CYP3A activities in a concentration-related manner and that CYP2C19 activity is reversibly inhibited by modafinil. In vitro data also demonstrated that modafinil produced an apparent concentration-related suppression of expression of CYP2C9 activity. Other CYP activities did not appear to be affected by modafinil.
The existence of multiple pathways for modafinil metabolism, as well as the fact that a non-CYP-related pathway is the most rapid in metabolizing modafinil, suggest that there is a low probability of substantive effects on the overall pharmacokinetic profile of modafinil due to CYP inhibition by concomitant medications. However, due to the partial involvement of CYP3A enzymes in the metabolic elimination of modafinil, coadministration of potent inducers of CYP3A4/5 (e.g., carbamazepine, phenobarbital, rifampin) or inhibitors of CYP3A4/5 (e.g., ketoconazole, erythromycin) could alter the plasma concentrations of modafinil.
- Drugs Metabolized by CYP3A4/5
- In vitro data demonstrated that modafinil is a weak inducer of CYP3A activity in a concentration-related manner. Therefore, the blood levels and effectiveness of drugs that are substrates for CYP3A enzymes (e.g., steroidal contraceptives, cyclosporine, midazolam, and triazolam) may be reduced after initiation of concomitant treatment with modafinil[see Drug Interactions ].
- Ethinyl Estradiol - Administration of modafinil to female volunteers once daily at 200 mg/day for 7 days followed by 400 mg/day for 21 days resulted in a mean 11% decrease in mean Cmaxand 18% decrease in mean AUC0-24of ethinyl estradiol (EE2; 0.035 mg; administered orally with norgestimate). There was no apparent change in the elimination rate of ethinyl estradiol.
- Triazolam - In the drug interaction study between modafinil and ethinyl estradiol (EE2), on the same days as those for the plasma sampling for EE2pharmacokinetics, a single dose of triazolam (0.125 mg) was also administered. Mean Cmaxand AUC0-∞of triazolam were decreased by 42% and 59%, respectively, and its elimination half-life was decreased by approximately an hour after the modafinil treatment.
- Cyclosporine - One case of an interaction between modafinil and cyclosporine, a substrate of CYP3A4, has been reported in a 41 year old woman who had undergone an organ transplant. After one month of administration of 200 mg/day of modafinil, cyclosporine blood levels were decreased by 50%. The interaction was postulated to be due to the increased metabolism of cyclosporine, since no other factor expected to affect the disposition of the drug had changed.
- Midazolam - In a clinical study, concomitant administration of armodafinil 250 mg resulted in a reduction in systemic exposure to midazolam by 32% after a single oral dose (5 mg) and 17% after a single intravenous dose (2 mg).
- Quetiapine - In a separate clinical study, concomitant administration of armodafinil 250 mg with quetiapine (300 mg to 600 mg daily doses) resulted in a reduction in the mean systemic exposure of quetiapine by approximately 29%.
- Drugs Metabolized by CYP1A2
- In vitro data demonstrated that modafinil is a weak inducer of CYP1A2 in a concentration-related manner. However, in a clinical study with armodafinil using caffeine as a probe substrate, no significant effect on CYP1A2 activity was observed.
- Drugs Metabolized by CYP2B6
- In vitro data demonstrated that modafinil is a weak inducer of CYP2B6 activity in a concentration-related manner.
- Drugs Metabolized by CYP2C9
- In vitro data demonstrated that modafinil produced an apparent concentration-related suppression of expression of CYP2C9 activity suggesting that there is a potential for a metabolic interaction between modafinil and the substrates of this enzyme (e.g., S-warfarin and phenytoin)[see Drug Interactions ].
- Warfarin: Concomitant administration of modafinil with warfarin did not produce significant changes in the pharmacokinetic profiles of R- and S-warfarin. However, since only a single dose of warfarin was tested in this study, an interaction cannot be ruled out[see Drug Interactions ].
- Drugs Metabolized by CYP2C19
- In vitro data demonstrated that modafinil is a reversible inhibitor of CYP2C19 activity. CYP2C19 is also reversibly inhibited, with similar potency, by a circulating metabolite, modafinil sulfone. Although the maximum plasma concentrations of modafinil sulfone are much lower than those of parent modafinil, the combined effect of both compounds could produce sustained partial inhibition of the enzyme. Therefore, exposure to some drugs that are substrates for CYP2C19 (e.g., phenytoin, diazepam, propranolol, omeprazole, and clomipramine) may be increased when used concomitantly with modafinil[see Drug Interactions ].
- In a clinical study, concomitant administration of armodafinil 400 mg resulted in a 40% increase in exposure to omeprazole after a single oral dose (40 mg), as a result of moderate inhibition of CYP2C19 activity.
- Interactions withCNSActive Drugs
- Concomitant administration of modafinil with methylphenidate or dextroamphetamine produced no significant alterations on the pharmacokinetic profile of modafinil or either stimulant, even though the absorption of modafinil was delayed for approximately one hour.
- Concomitant modafinil or clomipramine did not alter the pharmacokinetic profile of either drug; however, one incident of increased levels of clomipramine and its active metabolite desmethylclomipramine was reported in a patient with narcolepsy during treatment with modafinil.
- CYP2C19 also provides an ancillary pathway for the metabolism of certain tricyclic antidepressants (e.g., clomipramine and desipramine) and selective serotonin reuptake inhibitors that are primarily metabolized by CYP2D6. In tricyclic-treated patients deficient in CYP2D6 (i.e., those who are poor metabolizers of debrisoquine; 7-10% of the Caucasian population; similar or lower in other populations), the amount of metabolism by CYP2C19 may be substantially increased. Modafinil may cause elevation of the levels of the tricyclics in this subset of patients[see Drug Interactions ].
- Concomitant administration of armodafinil with quetiapine reduced the systemic exposure of quetiapine.
- Interaction with P-Glycoprotein
- An in vitro study demonstrated that armodafinil is a substrate of P-glycoprotein. The impact of inhibition of P-glycoprotein is not known.
Caution should be used when concomitantly administering MAO inhibitors and modafinil.
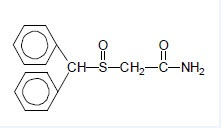
Modafinil is a wakefulness‑promoting agent for oral administration. Modafinil is a racemic compound. The chemical name for modafinil is 2‑[(diphenylmethyl)sulfinyl]acetamide. The molecular formula is C15H15NO2S and the molecular weight is 273.35.
The chemical structure is:
Modafinil is a white to off-white, crystalline powder that is practically insoluble in water and cyclohexane. It is sparingly to slightly soluble in methanol and acetone.
Modafinil tablets contain 100 mg or 200 mg of modafinil and the following inactive ingredients: croscarmellose sodium, lactose monohydrate, magnesium stearate, microcrystalline cellulose, povidone, and pregelatinized starch.