Get your patient on Perforomist (Formoterol Fumarate Dihydrate)
Perforomist prior authorization resources
Most recent state uniform prior authorization forms
Perforomist patient education
Patient toolkit
Dosage & administration
DOSAGE AND ADMINISTRATION
The recommended dose of PERFOROMIST (formoterol fumarate) Inhalation Solution is one 20 mcg unit-dose vial administered twice daily (morning and evening) by nebulization. A total daily dose greater than 40 mcg is not recommended.
PERFOROMIST Inhalation Solution should be administered by the orally inhaled route via a standard jet nebulizer connected to an air compressor. The safety and efficacy of PERFOROMIST Inhalation Solution have been established in clinical trials when administered using the PARI-LC Plus ® nebulizer (with a facemask or mouthpiece) and the PRONEB ® Ultra compressor. The safety and efficacy of PERFOROMIST Inhalation Solution delivered from non-compressor based nebulizer systems have not been established.
PERFOROMIST Inhalation Solution should always be stored in the foil pouch, and only removed IMMEDIATELY BEFORE USE. Contents of any partially used container should be discarded.
If the recommended maintenance treatment regimen fails to provide the usual response, medical advice should be sought immediately, as this is often a sign of destabilization of COPD. Under these circumstances, the therapeutic regimen should be re-evaluated and additional therapeutic options should be considered.
The drug compatibility (physical and chemical), efficacy, and safety of PERFOROMIST Inhalation Solution when mixed with other drugs in a nebulizer have not been established.

By using PrescriberAI, you agree to the AI Terms of Use.
Perforomist prescribing information
INDICATIONS AND USAGE
PERFOROMIST Inhalation Solution is a long-acting beta 2 -adrenergic agonist (beta 2 -agonist) indicated for:
- Long-term, twice daily (morning and evening) administration in the maintenance treatment of bronchoconstriction in patients with chronic obstructive pulmonary disease (COPD), including chronic bronchitis and emphysema. (1.1 )
Important limitations of use:
Maintenance Treatment of COPD
PERFOROMIST (formoterol fumarate) Inhalation Solution is indicated for the long-term, twice daily (morning and evening) administration in the maintenance treatment of bronchoconstriction in patients with chronic obstructive pulmonary disease (COPD), including chronic bronchitis and emphysema.
Important Limitations of Use
PERFOROMIST Inhalation Solution is not indicated to treat acute deteriorations of chronic obstructive pulmonary disease [see WARNINGS AND PRECAUTIONS (5.2) ].
PERFOROMIST Inhalation Solution is not indicated to treat asthma. The safety and effectiveness of PERFOROMIST Inhalation Solution in asthma have not been established.
DOSAGE AND ADMINISTRATION
The recommended dose of PERFOROMIST (formoterol fumarate) Inhalation Solution is one 20 mcg unit-dose vial administered twice daily (morning and evening) by nebulization. A total daily dose greater than 40 mcg is not recommended.
PERFOROMIST Inhalation Solution should be administered by the orally inhaled route via a standard jet nebulizer connected to an air compressor. The safety and efficacy of PERFOROMIST Inhalation Solution have been established in clinical trials when administered using the PARI-LC Plus ® nebulizer (with a facemask or mouthpiece) and the PRONEB ® Ultra compressor. The safety and efficacy of PERFOROMIST Inhalation Solution delivered from non-compressor based nebulizer systems have not been established.
PERFOROMIST Inhalation Solution should always be stored in the foil pouch, and only removed IMMEDIATELY BEFORE USE. Contents of any partially used container should be discarded.
If the recommended maintenance treatment regimen fails to provide the usual response, medical advice should be sought immediately, as this is often a sign of destabilization of COPD. Under these circumstances, the therapeutic regimen should be re-evaluated and additional therapeutic options should be considered.
The drug compatibility (physical and chemical), efficacy, and safety of PERFOROMIST Inhalation Solution when mixed with other drugs in a nebulizer have not been established.
DOSAGE FORMS AND STRENGTHS
PERFOROMIST (formoterol fumarate) Inhalation Solution is supplied as a sterile solution for nebulization in low-density polyethylene unit-dose vials. Each vial contains formoterol fumarate dihydrate, USP equivalent to 20 mcg/2 mL of formoterol fumarate.
USE IN SPECIFIC POPULATIONS
Pregnancy
Risk Summary
There are limited available data with PERFOROMIST Inhalation Solution use in pregnant women to inform a drug-associated risk of adverse developmental outcomes. Beta-agonists may interfere with uterine contractility (see Clinical Considerations ) . In animal reproduction studies, oral administration of formoterol fumarate to pregnant rats and rabbits caused increased fetal malformations (rats and rabbits), decreased fetal weight (rats), and increased neonatal mortality (rats) following administration of doses that produced exposures approximately 730 to 29,000 times the MRHD on a mg/m 2 or AUC basis.These adverse effects generally occurred at large multiples of the MRHD when formoterol fumarate was administered by the oral route to achieve high systemic exposures. No effects were observed in a study with rats that received formoterol fumarate by the inhalation route at an exposure approximately 300 times the MRHD (see Data ) .
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2-4% and 15-20%, respectively.
Clinical Considerations
Labor or delivery
There are no adequate and well-controlled human studies that have studied the effects of PERFOROMIST Inhalation Solution during labor and delivery. Because of the potential for beta-agonists interference with uterine contractility, use of PERFOROMIST Inhalation Solution during labor should be restricted to those patients in whom the benefits clearly outweigh the risk.
Data
Animal Data
In embryofetal development studies with pregnant rats and rabbits dosed throughout the period of organogenesis, formoterol fumarate did not cause malformations in either species. However, for pregnant rats dosed throughout organogenesis, formoterol fumarate caused delayed fetal ossification at an exposure approximately 50 times the MRHD (on a mcg/m 2 basis with maternal oral doses of 200 mcg/kg and higher) and decreased fetal weight at an exposure approximately 1,500 times the MRHD (on a mcg/m 2 basis with maternal oral doses of 6,000 mcg/kg and above). In a pre- and post-natal development study with rats dosed during the late stage of pregnancy, formoterol fumarate caused stillbirth and neonatal mortality at an exposure approximately 1,500 times the MRHD (on a mcg/m 2 basis with maternal oral doses of 6,000 mcg/kg and above). However, no effects were observed in this study at an exposure approximately 50 times the MRHD (on a mcg/m 2 basis with a maternal oral dose of 200 mcg/kg).
In embryofetal development studies, conducted by another testing laboratory, with pregnant rats and rabbits dosed throughout the period of organogenesis, formoterol fumarate was teratogenic in both species. Umbilical hernia, a malformation, was observed in rat fetuses at exposures approximately 730 times the MRHD (on a mcg/m 2 basis with maternal oral doses of 3,000 mcg/kg/day and above). Brachygnathia, a skeletal malformation, was observed in rat fetuses at an exposure approximately 3,600 times the MRHD (on a mcg/m 2 basis with a maternal oral dose of 15,000 mcg/kg/day). In another study with rats, no teratogenic effects were observed with exposures up to approximately 300 times the MRHD (on a mcg/m 2 basis with a maternal inhalation dose of 1,200 mcg/kg/day). Subcapsular cysts on the liver were observed in rabbit fetuses at an exposure approximately 29,000 times the MRHD (on a mcg/m 2 basis with a maternal oral dose of 60,000 mcg/kg/day). No teratogenic effects were observed with exposures up to approximately 1,700 times the MRHD (on a mcg/m 2 basis with a maternal oral dose of 3,500 mcg/kg).
Lactation
Risk Summary
There are no well-controlled human studies of the use of PERFOROMIST Inhalation Solution in nursing mothers. It is not known whether formoterol fumarate is excreted in human milk, or whether there are effects on the breastfed infant or on the milk production.
In reproductive studies in rats formoterol was excreted in the milk ( see Data ) .
The developmental and health benefits of breastfeeding should be considered along with the mother`s clinical need for PERFOROMIST Inhalation Solution and any potential adverse effects on the breastfed child from PERFOROMIST Inhalation Solution or from the underlying maternal condition.
Data
In a pharmacokinetic study in rats formoterol was excreted in the milk. The amount of radioactive labelled 3 H-formoterol fumarate was less than 2% of that in the maternal plasma.
Pediatric Use
PERFOROMIST Inhalation Solution is not indicated for use in children. The safety and effectiveness of PERFOROMIST Inhalation Solution in pediatric patients have not been established. The pharmacokinetics of formoterol fumarate has not been studied in pediatric patients.
Geriatric Use
Of the 586 subjects who received PERFOROMIST Inhalation Solution in clinical studies, 284 were 65 years and over, while 89 were 75 years and over. Of the 123 subjects who received PERFOROMIST Inhalation Solution in the 12-week safety and efficacy trial, 48 (39%) were 65 years of age or older. No overall differences in safety or effectiveness were observed between these subjects and younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger adult patients, but greater sensitivity of some older individuals cannot be ruled out.
The pharmacokinetics of PERFOROMIST Inhalation Solution has not been studied in elderly subjects.
CONTRAINDICATIONS
Use of a LABA, including PERFOROMIST, without an inhaled corticosteroid is contraindicated in patients with asthma [see WARNINGS and PRECAUTIONS (5.1) ] . PERFOROMIST is not indicated for the treatment of asthma.
WARNINGS AND PRECAUTIONS
- LABA as monotherapy (without inhaled corticosteroid) for asthma increases the risk of serious asthma-related events. (5.1 )
- Do not initiate PERFOROMIST Inhalation Solution in acutely deteriorating patients. (5.2 )
- Do not use for relief of acute symptoms. Concomitant short-acting beta 2 -agonists can be used as needed for acute relief. (5.2 )
- Do not exceed the recommended dose. Excessive use of PERFOROMIST Inhalation Solution or use in conjunction with other medications containing long-acting beta 2 -agonists, can result in clinically significant cardiovascular effects, and may be fatal. (5.3 , 5.5 )
- Life-threatening paradoxical bronchospasm can occur. Discontinue PERFOROMIST Inhalation Solution immediately. (5.4 )
- Use with caution in patients with cardiovascular or convulsive disorders, thyrotoxicosis, or with sensitivity to sympathomimetic drugs. (5.6 , 5.7 )
Serious Asthma-Related Events – Hospitalizations, Intubations, Death
- The safety and efficacy of PERFOROMIST in patients with asthma have not been established. PERFOROMIST is not indicated for the treatment of asthma [see CONTRAINDICATIONS (4) ] .
- Use of long-acting beta2-adrenergic agonists (LABA) as monotherapy [without inhaled corticosteroids (ICS)] for asthma is associated with an increased risk of asthma-related death. Available data from controlled clinical trials also suggest that use of LABA as monotherapy increases the risk of asthma-related hospitalization in pediatric and adolescent patients. These findings are considered a class effect of LABA monotherapy. When LABA are used in fixed ‑ dose combination with ICS, data from large clinical trials do not show a significant increase in the risk of serious asthma-related events (hospitalizations, intubations, death) compared with ICS alone.
- A 28-week, placebo-controlled US study comparing the safety of another LABA (salmeterol) with placebo, each added to usual asthma therapy, showed an increase in asthma-related deaths in patients receiving salmeterol (13/13,176 in patients treated with salmeterol vs. 3/13,179 in patients treated with placebo; RR 4.37, 95% CI 1.25, 15.34). The increased risk of asthma-related death is considered a class effect of the long-acting beta2-adrenergic agonists, including PERFOROMIST Inhalation Solution.
- No study adequate to determine whether the rate of asthma related death is increased in patients treated with PERFOROMIST Inhalation Solution has been conducted. Clinical studies with formoterol fumarate administered as a dry powder inhaler suggested a higher incidence of serious asthma exacerbations in patients who received formoterol than in those who received placebo. The sizes of these studies were not adequate to precisely quantify the differences in serious asthma exacerbation rates between treatment groups.
- Available data do not suggest an increased risk of death with use of LABA in patients with COPD.
Deterioration of Disease and Acute Episodes
PERFOROMIST Inhalation Solution should not be initiated in patients with acutely deteriorating COPD, which may be a life-threatening condition. PERFOROMIST Inhalation Solution has not been studied in patients with acutely deteriorating COPD. The use of PERFOROMIST Inhalation Solution in this setting is inappropriate.
PERFOROMIST Inhalation Solution should not be used for the relief of acute symptoms, i.e., as rescue therapy for the treatment of acute episodes of bronchospasm. PERFOROMIST Inhalation Solution has not been studied in the relief of acute symptoms and extra doses should not be used for that purpose. Acute symptoms should be treated with an inhaled short-acting beta 2 -agonist.
When beginning PERFOROMIST Inhalation Solution, patients who have been taking inhaled, short-acting beta 2 -agonists on a regular basis (e.g., four times a day) should be instructed to discontinue the regular use of these drugs and use them only for symptomatic relief of acute respiratory symptoms. When prescribing PERFOROMIST Inhalation Solution, the healthcare provider should also prescribe an inhaled, short-acting beta 2 -agonist and instruct the patient how it should be used. Increasing inhaled beta 2 -agonist use is a signal of deteriorating disease for which prompt medical attention is indicated. COPD may deteriorate acutely over a period of hours or chronically over several days or longer. If PERFOROMIST Inhalation Solution no longer controls the symptoms of bronchoconstriction, or the patient’s inhaled, short-acting beta 2 -agonist becomes less effective or the patient needs more inhalation of short-acting beta 2 -agonist than usual, these may be markers of deterioration of disease. In this setting, a re-evaluation of the patient and the COPD treatment regimen should be undertaken at once. Increasing the daily dosage of PERFOROMIST Inhalation Solution beyond the recommended 20 mcg twice daily dose is not appropriate in this situation.
Excessive Use and Use with Other Long-Acting Beta 2 -Agonists
As with other inhaled beta 2 -adrenergic drugs, PERFOROMIST Inhalation Solution should not be used more often, at higher doses than recommended, or in conjunction with other medications containing long-acting beta 2 -agonists, as an overdose may result. Clinically significant cardiovascular effects and fatalities have been reported in association with excessive use of inhaled sympathomimetic drugs.
Paradoxical Bronchospasm
As with other inhaled beta 2 -agonists, PERFOROMIST Inhalation Solution can produce paradoxical bronchospasm that may be life-threatening. If paradoxical bronchospasm occurs, PERFOROMIST Inhalation Solution should be discontinued immediately and alternative therapy instituted.
Cardiovascular Effects
PERFOROMIST Inhalation Solution, like other beta 2 -agonists, can produce a clinically significant cardiovascular effect in some patients as measured by increases in pulse rate, systolic and/or diastolic blood pressure, and/or symptoms. If such effects occur, PERFOROMIST Inhalation Solution may need to be discontinued. In addition, beta-agonists have been reported to produce ECG changes, such as flattening of the T wave, prolongation of the QTc interval, and ST segment depression. The clinical significance of these findings is unknown. Therefore, PERFOROMIST Inhalation Solution, like other sympathomimetic amines, should be used with caution in patients with cardiovascular disorders, especially coronary insufficiency, cardiac arrhythmias, and hypertension.
Coexisting Conditions
PERFOROMIST Inhalation Solution, like other sympathomimetic amines, should be used with caution in patients with convulsive disorders or thyrotoxicosis, and in patients who are unusually responsive to sympathomimetic amines. Doses of the related beta 2 -agonist albuterol, when administered intravenously, have been reported to aggravate preexisting diabetes mellitus and ketoacidosis.
Hypokalemia and Hyperglycemia
Beta-agonist medications may produce significant hypokalemia in some patients, possibly through intracellular shunting, which has the potential to produce adverse cardiovascular effects [see CLINICAL PHARMACOLOGY (12.2) ]. The decrease in serum potassium is usually transient, not requiring supplementation. Beta-agonist medications may produce transient hyperglycemia in some patients.
Clinically significant changes in serum potassium and blood glucose were infrequent during clinical studies with long-term administration of PERFOROMIST Inhalation Solution at the recommended dose.
Immediate Hypersensitivity Reactions
Immediate hypersensitivity reactions may occur after administration of PERFOROMIST Inhalation Solution, as demonstrated by cases of anaphylactic reactions, urticaria, angioedema, rash, and bronchospasm.
ADVERSE REACTIONS
Long-acting beta 2 -adrenergic agonists, such as PERFOROMIST, as monotherapy (without an inhaled corticosteroid) for asthma increase the risk of asthma-related events. PERFOROMIST is not indicated for the treatment of asthma [see WARNINGS AND PRECAUTIONS (5.1) ] .
Beta 2 -Agonist Adverse Reaction Profile
Adverse reactions to PERFOROMIST Inhalation Solution are expected to be similar in nature to other beta 2 -adrenergic receptor agonists including: angina, hypertension or hypotension, tachycardia, arrhythmias, nervousness, headache, tremor, dry mouth, muscle cramps, palpitations, nausea, dizziness, fatigue, malaise, insomnia, hypokalemia, hyperglycemia, and metabolic acidosis.
Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Adults with COPD
The data described below reflect exposure to PERFOROMIST Inhalation Solution 20 mcg twice daily by oral inhalation in 586 patients, including 232 exposed for 6 months and 155 exposed for at least 1 year. PERFOROMIST Inhalation Solution was studied in a 12-week, placebo- and active-controlled trial (123 subjects treated with PERFOROMIST Inhalation Solution) and a 52-week, active-controlled trial (463 subjects treated with PERFOROMIST Inhalation Solution). Patients were mostly Caucasians (88%) between 40-90 years old (mean, 64 years old) and had COPD, with a mean FEV 1 of 1.33 L. Patients with significant concurrent cardiac and other medical diseases were excluded from the trials.
Table 1 shows adverse reactions from the 12-week, double-blind, placebo-controlled trial where the frequency was greater than or equal to 2% in the PERFOROMIST Inhalation Solution group and where the rate in the PERFOROMIST Inhalation Solution group exceeded the rate in the placebo group. In this trial, the frequency of patients experiencing cardiovascular adverse events was 4.1% for PERFOROMIST Inhalation Solution and 4.4% for placebo. There were no frequently occurring specific cardiovascular adverse events for PERFOROMIST Inhalation Solution (frequency greater than or equal to 1% and greater than placebo). The rate of COPD exacerbations was 4.1% for PERFOROMIST Inhalation Solution and 7.9% for placebo.
Number of patients with adverse reactions in the 12-week multiple-dose controlled clinical trial | ||||
Adverse Reaction | PERFOROMIST Inhalation Solution 20 mcg | Placebo | ||
n | (%) | n | (%) | |
Total Patients | 123 | (100) | 114 | (100) |
Diarrhea | 6 | (4.9) | 4 | (3.5) |
Nausea | 6 | (4.9) | 3 | (2.6) |
Nasopharyngitis | 4 | (3.3) | 2 | (1.8) |
Dry Mouth | 4 | (3.3) | 2 | (1.8) |
Vomiting | 3 | (2.4) | 2 | (1.8) |
Dizziness | 3 | (2.4) | 1 | (0.9) |
Insomnia | 3 | (2.4) | 0 | 0 |
Patients treated with PERFOROMIST Inhalation Solution 20 mcg twice daily in the 52-week open-label trial did not experience an increase in specific clinically significant adverse events above the number expected based on the medical condition and age of the patients.
Postmarketing Experience
The following adverse reactions have been reported during post-approval use of PERFOROMIST Inhalation Solution. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Anaphylactic reactions, urticaria, angioedema (presenting as face, lip, tongue, eye, pharyngeal, or mouth edema), rash, and bronchospasm
DRUG INTERACTIONS
- Other adrenergic drugs may potentiate effect. Use with caution. (5.3 , 7.1 )
- Xanthine derivatives, steroids, diuretics, or non-potassium sparing diuretics may potentiate hypokalemia or ECG changes. Use with caution. (5.7 , 7.2 , 7.3 )
- MAO inhibitors, tricyclic antidepressants and drugs that prolong QTc interval may potentiate effect on the cardiovascular system. Use with extreme caution. (7.4 )
- Beta-blockers may decrease effectiveness. Use with caution and only when medically necessary. (7.5 )
Adrenergic Drugs
If additional adrenergic drugs are to be administered by any route, they should be used with caution because the sympathetic effects of formoterol may be potentiated [see WARNINGS AND PRECAUTIONS (5.3 , 5.5 , 5.6 , 5.7) ].
Xanthine Derivatives, Steroids, or Diuretics
Concomitant treatment with xanthine derivatives, steroids, or diuretics may potentiate any hypokalemic effect of adrenergic agonists [see WARNINGS AND PRECAUTIONS (5.7) ].
Non-potassium Sparing Diuretics
The ECG changes and/or hypokalemia that may result from the administration of non-potassium sparing diuretics (such as loop or thiazide diuretics) can be acutely worsened by beta-agonists, especially when the recommended dose of the beta-agonist is exceeded. Although the clinical significance of these effects is not known, caution is advised in the co-administration of beta-agonists with non-potassium sparing diuretics.
MAO Inhibitors, Tricyclic Antidepressants, QTc Prolonging Drugs
Formoterol, as with other beta 2 -agonists, should be administered with extreme caution to patients being treated with monoamine oxidase inhibitors, tricyclic antidepressants, or drugs known to prolong the QTc interval because the effect of adrenergic agonists on the cardiovascular system may be potentiated by these agents. Drugs that are known to prolong the QTc interval have an increased risk of ventricular arrhythmias.
Beta-blockers
Beta-adrenergic receptor antagonists (beta-blockers) and formoterol may inhibit the effect of each other when administered concurrently. Beta-blockers not only block the therapeutic effects of beta-agonists, but may produce severe bronchospasm in COPD patients. Therefore, patients with COPD should not normally be treated with beta-blockers. However, under certain circumstances, e.g., as prophylaxis after myocardial infarction, there may be no acceptable alternatives to the use of beta-blockers in patients with COPD. In this setting, cardioselective beta-blockers could be considered, although they should be administered with caution.
DESCRIPTION
PERFOROMIST (formoterol fumarate) Inhalation Solution is supplied as 2 mL of formoterol fumarate inhalation solution packaged in a 2.5 mL single-use low-density polyethylene vial and overwrapped in a foil pouch. Each vial contains 2 mL of a clear, colorless solution composed of formoterol fumarate dihydrate, USP equivalent to 20 mcg of formoterol fumarate in an isotonic, sterile aqueous solution containing sodium chloride, pH adjusted to 5.0 with citric acid and sodium citrate.
The active component of PERFOROMIST Inhalation Solution is formoterol fumarate dihydrate, USP, a racemate. Formoterol fumarate dihydrate is a beta 2 -adrenergic bronchodilator. Its chemical name is (±)-2-hydroxy-5-[(1RS)-1-hydroxy-2-[[(1RS)-2-(4-methoxyphenyl)-1-methylethyl]-amino]ethyl]formanilide fumarate dihydrate; its structural formula is:
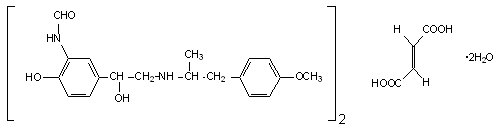
Formoterol fumarate dihydrate, USP has a molecular weight of 840.92 and its empirical formula is (C 19 H 24 N 2 O 4 ) 2 •C 4 H 4 O 4 •2H 2 O. Formoterol fumarate dihydrate, USP is a white to yellowish crystalline powder, which is freely soluble in glacial acetic acid, soluble in methanol, sparingly soluble in ethanol and isopropanol, slightly soluble in water, and practically insoluble in acetone, ethyl acetate, and diethyl ether.
PERFOROMIST Inhalation Solution does not require dilution prior to administration by nebulization. Like all other nebulized treatments, the amount delivered to the lungs will depend on patient factors and the nebulization system used and its performance.
Using the PARI-LC Plus ® nebulizer (with a facemask or mouthpiece) connected to a PRONEB ® Ultra compressor under in vitro conditions, the mean delivered dose from the mouthpiece was approximately 7.3 mcg (37% of label claim). The mean nebulizer flow rate was 4 LPM and the nebulization time was 9 minutes. PERFOROMIST Inhalation Solution should be administered from a standard jet nebulizer at adequate flow rates via a facemask or mouthpiece.
CLINICAL PHARMACOLOGY
Mechanism of Action
Formoterol fumarate is a long-acting, beta 2 -adrenergic receptor agonist (beta 2 -agonist). Inhaled formoterol fumarate acts locally in the lung as a bronchodilator. In vitro studies have shown that formoterol has more than 200-fold greater agonist activity at beta 2 -receptors than at beta 1 -receptors. Although beta 2 -receptors are the predominant adrenergic receptors in bronchial smooth muscle and beta 1 -receptors are the predominant receptors in the heart, there are also beta 2 -receptors in the human heart comprising 10% to 50% of the total beta-adrenergic receptors. The precise function of these receptors has not been established, but they raise the possibility that even highly selective beta 2 -agonists may have cardiac effects.
The pharmacologic effects of beta 2 -adrenoceptor agonist drugs, including formoterol, are at least in part attributable to stimulation of intracellular adenyl cyclase, the enzyme that catalyzes the conversion of adenosine triphosphate (ATP) to cyclic-3', 5'-adenosine monophosphate (cyclic AMP). Increased cyclic AMP levels cause relaxation of bronchial smooth muscle and inhibition of release of mediators of immediate hypersensitivity from cells, especially from mast cells.
In vitro tests show that formoterol is an inhibitor of the release of mast cell mediators, such as histamine and leukotrienes, from the human lung. Formoterol also inhibits histamine-induced plasma albumin extravasation in anesthetized guinea pigs and inhibits allergen-induced eosinophil influx in dogs with airway hyper-responsiveness. The relevance of these in vitro and animal findings to humans with COPD is unknown.
Pharmacodynamics
Systemic Safety and Pharmacokinetic / Pharmacodynamic Relationships
The major adverse effects of inhaled beta 2 -agonists occur as a result of excessive activation of the systemic beta-adrenergic receptors. The most common adverse effects in adults include skeletal muscle tremor and cramps, insomnia, tachycardia, decreases in plasma potassium, and increases in plasma glucose.
Changes in serum potassium and serum glucose were evaluated in 12 COPD patients following inhalation of single doses of PERFOROMIST Inhalation Solution containing 10, 20 and 244 mcg of formoterol fumarate (calculated on an anhydrous basis) in a crossover study. At 1 hour after treatment with formoterol fumarate inhalation solution, mean (± standard deviation) serum glucose rose 26 ± 30, 29 ± 28, and 38 ± 44 mg/dL, respectively, and was not significantly different from baseline or trough level at 24 hours post-dose. At 1 hour after dosing with formoterol fumarate inhalation solution 244 mcg, serum potassium fell by 0.68 ± 0.4 mEq/L, and was not different from baseline or trough level at 24 hours post-dose.
Linear pharmacokinetic/pharmacodynamic (PK/PD) relationships between urinary formoterol excretion and decreases in serum potassium, increases in plasma glucose, and increases in heart rate were generally observed with another inhalation formulation of formoterol fumarate and hence would be expected with PERFOROMIST Inhalation Solution also. Following single dose administration of 10-fold the recommended clinical dose of the other formoterol fumarate inhalation formulation having comparable exposure to single dose of 244 mcg of PERFOROMIST Inhalation Solution (approximately 12-fold the recommended clinical dose) in healthy subjects, the formoterol plasma concentration was found to be highly correlated with the reduction in plasma potassium concentration. Data from this study showed that maximum reductions from baseline in plasma potassium ranged from 0.55 to 1.52 mmol/L with a median maximum reduction of 1.01 mmol/L. Generally, the maximum effect on plasma potassium was noted 1 to 3 hours after peak formoterol plasma concentrations were achieved.
Electrophysiology
In the dose-ranging study of PERFOROMIST Inhalation Solution, ECG-determined heart rate increased by a mean of 6 ±3 beats per minute at 6 hours after a single dose of 244 mcg, but was back to predose level at 16-24 hours.
The effect of PERFOROMIST Inhalation Solution on heart rate and cardiac rhythm was studied in a 12-week clinical trial comparing PERFOROMIST Inhalation Solution to placebo and an active control treatment. COPD patients, including 105 patients exposed to PERFOROMIST Inhalation Solution, underwent continuous electrocardiographic (Holter) monitoring during two 24-hour periods (study baseline and after 8-12 weeks of treatment). ECGs were performed pre-dose and at 2 to 3 hours post-dose at study baseline (prior to dosing) and after 4, 8 and 12 weeks of treatment. Bazett’s and Fridericia’s methods were used to correct the QT interval for heart rate (QTcB and QTcF, respectively). The mean increase from baseline in QTcB interval over the 12-week treatment period was ≤ 4.8 msec for PERFOROMIST Inhalation Solution and ≤ 4.6 msec for placebo. The percent of patients who experienced a maximum change in QTc greater than 60 msec at any time during the 12-week treatment period was 0% and 1.8% for PERFOROMIST Inhalation Solution and placebo, respectively, based on Bazett’s correction, and 1.6% and 0.9%, respectively, based on Fridericia’s correction. Prolonged QT was reported as an adverse event in 1 (0.8%) patient treated with PERFOROMIST Inhalation Solution and 2 (1.8%) placebo patients. No occurrences of atrial fibrillation or ventricular tachycardia were observed during 24-hour Holter monitoring or reported as adverse events in patients treated with PERFOROMIST Inhalation Solution after the start of dosing. No increase in supraventricular tachycardia over placebo-treated subjects was observed. The mean increase in maximum heart rate from baseline to 8-12 weeks after the start of dosing was 0.6 beats per minute (bpm) for patients treated with PERFOROMIST Inhalation Solution twice daily compared to 1.2 bpm for placebo patients. There were no clinically meaningful differences from placebo in acute or chronic effects on heart rate, including QTcB and QTcF, or cardiac rhythm resulting from treatment with PERFOROMIST Inhalation Solution.
At an exposure from formoterol fumarate dry powder formulation comparable to approximately 12-fold the recommended dose of PERFOROMIST Inhalation Solution, a mean maximum increase of pulse rate of 26 bpm was observed 6 hours post dose in healthy subjects. This study showed that the maximum increase of mean corrected QT interval (QTc) was 25 msec when calculated using Bazett's correction and was 8 msec when calculated using Fridericia's correction. The QTc returned to baseline within 12 to 24 hours post-dose. Formoterol plasma concentrations were weakly correlated with pulse rate and increase of QTc duration. The effects on pulse rate and QTc interval are known pharmacological effects of this class of study drug and were not unexpected at this supratherapeutic formoterol fumarate inhalation dose.
Tachyphylaxis / Tolerance
Tolerance to the effects of inhaled beta-agonists can occur with regularly-scheduled, chronic use. In a placebo-controlled clinical trial in 351 adult patients with COPD, the bronchodilating effect of PERFOROMIST Inhalation Solution was determined by the FEV 1 area under the curve over 12 hours following dosing on Day 1 and after 12 weeks of treatment. The effect of PERFOROMIST Inhalation Solution did not decrease after 12 weeks of twice-daily treatment (Figures 1 and 2).
Pharmacokinetics
Information on the pharmacokinetics of formoterol (dry powder and/or inhalation solution) in plasma and/or urine is available in healthy subjects as well as patients with chronic obstructive pulmonary disease after oral inhalation of doses at and above the therapeutic dose.
Urinary excretion of unchanged formoterol was used as an indirect measure of systemic exposure. Plasma drug disposition data parallel urinary excretion, and the elimination half-lives calculated for urine and plasma are similar.
Absorption
Pharmacokinetic properties of formoterol fumarate were evaluated in 12 COPD patients following inhalation of single doses of PERFOROMIST Inhalation Solution containing 10, 20 and 244 mcg of formoterol fumarate (calculated on an anhydrous basis) and 12 mcg formoterol fumarate dry powder, through 36 hours after single-dose administration. Formoterol fumarate concentrations in plasma following the 10 and 20 mcg doses of PERFOROMIST Inhalation Solution and the 12 mcg dose of formoterol fumarate dry powder were undetectable or only detected sporadically at very low concentrations. Following a single 244 mcg dose of PERFOROMIST Inhalation Solution (approximately 12 times the recommended clinical dose), formoterol fumarate concentrations were readily measurable in plasma, exhibiting rapid absorption into plasma, and reaching a maximum drug concentration of 72 pg/mL within approximately 12 minutes of dosing.
The mean amount of formoterol excreted unchanged in 24-hour urine following single oral inhalation doses of 10, 20, and 244 mcg PERFOROMIST Inhalation Solution were found to be 109.7 ng, 349.6 ng, and 3317.5 ng, respectively. These findings indicate a near dose proportional increase in systemic exposure within the dose range tested.
When 12 mcg of a dry powder formulation of formoterol fumarate was given twice daily to COPD patients by oral inhalation for 12 weeks, the accumulation index, based on the urinary excretion of unchanged formoterol was 1.19 to 1.38. This suggests some accumulation of formoterol in plasma with multiple dosing. Although multiple-dose pharmacokinetic data is unavailable from PERFOROMIST Inhalation Solution, assumption of linear pharmacokinetics allows a reasonable prediction of minimal accumulation based on single-dose pharmacokinetics. As with many drug products for oral inhalation, it is likely that the majority of the inhaled formoterol fumarate delivered is swallowed and then absorbed from the gastrointestinal tract.
Distribution
The binding of formoterol to human plasma proteins in vitro was 61% to 64% at concentrations from 0.1 to 100 ng/mL. Binding to human serum albumin in vitro was 31% to 38% over a range of 5 to 500 ng/mL. The concentrations of formoterol used to assess the plasma protein binding were higher than those achieved in plasma following inhalation of a single 244 mcg dose of PERFOROMIST Inhalation Solution.
Metabolism
Formoterol is metabolized primarily by direct glucuronidation at either the phenolic or aliphatic hydroxyl group and O-demethylation followed by glucuronide conjugation at either phenolic hydroxyl groups. Minor pathways involve sulfate conjugation of formoterol and deformylation followed by sulfate conjugation. The most prominent pathway involves direct conjugation at the phenolic hydroxyl group. The second major pathway involves O-demethylation followed by conjugation at the phenolic 2'-hydroxyl group. In vitro studies showed that multiple drug-metabolizing enzymes catalyze glucuronidation (UGT1A1, 1A8, 1A9, 2B7 and 2B15 were the most predominant enzymes) and O-demethylation (CYP2D6, CYP2C19, CYP2C9 and CYP2A6) of formoterol. Formoterol did not inhibit CYP450 enzymes at therapeutically relevant concentrations. Some patients may be deficient in CYP2D6 or 2C19 or both. Whether a deficiency in one or both of these isozymes results in elevated systemic exposure to formoterol or systemic adverse effects has not been adequately explored.
Excretion
Following administration of single 10, 20, and 244 mcg PERFOROMIST Inhalation Solution doses (calculated on an anhydrous basis) delivered via nebulizer in 12 COPD patients, on average, about 1.1% to 1.7% of the dose was excreted in the urine as unchanged formoterol as compared to about 3.4% excreted unchanged following inhalation administration of 12 mcg of formoterol fumarate dry powder. Renal clearance of formoterol following inhalation administration of PERFOROMIST Inhalation Solution in these subjects was about 157 mL/min. Based on plasma concentrations measured following the 244 mcg dose, the mean terminal elimination half-life was determined to be 7 hours.
Gender
As reported for another formoterol fumarate inhalation formulation, upon correction for body weight, pharmacokinetics of formoterol fumarate did not differ significantly between males and females.
Geriatric, Pediatric, Hepatic/Renal Impairment
The pharmacokinetics of formoterol fumarate has not been studied in elderly and pediatric patient populations. The pharmacokinetics of formoterol fumarate has not been studied in subjects with hepatic or renal impairment.
NONCLINICAL TOXICOLOGY
Carcinogenesis, Mutagenesis, Impairment of Fertility
The carcinogenic potential of formoterol fumarate has been evaluated in 2-year drinking water and dietary studies in both rats and mice. In rats, the incidence of ovarian leiomyomas was increased at doses of 15,000 mcg/kg and above in the drinking water study and at 20,000 mcg/kg in the dietary study (AUC exposure approximately 2,300 times human exposure at the maximum recommended daily inhalation dose), but not at dietary doses up to 5,000 mcg/kg (AUC exposure approximately 570 times human exposure at the maximum recommended daily inhalation dose). In the dietary study, the incidence of benign ovarian theca-cell tumors was increased at doses of 500 mcg/kg (AUC exposure was approximately 57 times human exposure at the maximum recommended daily inhalation dose) and above. This finding was not observed in the drinking water study, nor was it seen in mice (see below).
In mice, the incidence of adrenal subcapsular adenomas and carcinomas was increased in males at doses of 69,000 mcg/kg (AUC exposure approximately 1000 times human exposure at the maximum recommended daily inhalation dose) and above in the drinking water study, but not at doses up to 50,000 mcg/kg (AUC exposure approximately 750 times human exposure at the maximum recommended daily inhalation dose) in the dietary study. The incidence of hepatocarcinomas was increased in the dietary study at doses of 20,000 and 50,000 mcg/kg in females (AUC exposures approximately 300 and 750 times human exposure at the maximum recommended daily inhalation dose, respectively) and 50,000 mcg/kg in males, but not at doses up to 5,000 mcg/kg (AUC exposure approximately 75 times human exposure at the maximum recommended daily inhalation dose). Also in the dietary study, the incidence of uterine leiomyomas and leiomyosarcomas was increased at doses of 2,000 mcg/kg (AUC exposure was approximately 30 times human exposure at the maximum recommended daily inhalation dose) and above. Increases in leiomyomas of the rodent female genital tract have been similarly demonstrated with other beta-agonist drugs.
Formoterol fumarate was not mutagenic or clastogenic in the following tests: mutagenicity tests in bacterial and mammalian cells, chromosomal analyses in mammalian cells, unscheduled DNA synthesis repair tests in rat hepatocytes and human fibroblasts, transformation assay in mammalian fibroblasts and micronucleus tests in mice and rats.
Reproduction studies in rats revealed no impairment of fertility at oral doses up to 3,000 mcg/kg (approximately 730 times the maximum recommended daily inhalation powder dose in humans on a mcg/m 2 basis).
Animal Pharmacology
Studies in laboratory animals (minipigs, rodents, and dogs) have demonstrated the occurrence of cardiac arrhythmias and sudden death (with histologic evidence of myocardial necrosis) when beta-agonists and methylxanthines are administered concurrently. The clinical significance of these findings is unknown [see DRUG INTERACTIONS, Xanthine Derivatives, Steroids, or Diuretics (7.2) ].
CLINICAL STUDIES
Adult COPD Trial
PERFOROMIST (formoterol fumarate) Inhalation Solution was evaluated in a 12-week, double-blind, placebo- and active-controlled, randomized, parallel-group, multicenter trial conducted in the United States. Of a total enrollment of 351 adults (age range: 40 to 86 years; mean age: 63 years) with COPD who had a mean pre-bronchodilator FEV 1 of 1.34 liters (44% of predicted), 237 patients were randomized to PERFOROMIST Inhalation Solution 20 mcg or placebo, administered twice daily via a PARI-LC Plus ® nebulizer with a PRONEB ® Ultra compressor. The diagnosis of COPD was based upon a prior clinical diagnosis of COPD, a smoking history (at least 10 pack-years), age (at least 40 years), and spirometry results (pre-bronchodilator baseline FEV 1 at least 30% and less than 70% of the predicted value, and the FEV 1 /FVC less than 70%). About 58% of patients had bronchodilator reversibility, defined as a 10% or greater increase in FEV 1 after inhalation of 2 actuations (180 mcg) of albuterol from a metered dose inhaler. About 86% (106) of patients treated with PERFOROMIST Inhalation Solution and 74% (84) of placebo patients completed the trial.
PERFOROMIST Inhalation Solution 20 mcg twice daily resulted in significantly greater post-dose bronchodilation (as measured by serial FEV 1 for 12 hours post-dose; the primary efficacy analysis) compared to placebo when evaluated at endpoint (week 12 for completers and last observation for dropouts). Similar results were seen on Day 1 and at subsequent timepoints during the trial.
Mean FEV 1 measurements at Day 1 (Figure 1) and at endpoint (Figure 2) are shown below.
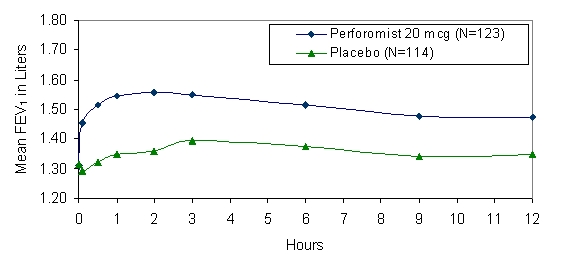
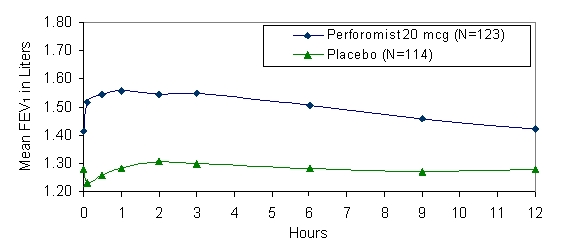
- • Figures show least-squares means adjusted for baseline FEV 1
Patients treated with PERFOROMIST Inhalation Solution used less rescue albuterol during the trial compared to patients treated with placebo.
Examination of age (≥ 65 or younger) and gender subgroups did not identify differences in response to PERFOROMIST Inhalation Solution. There were too few non-Caucasian subjects to assess differences in populations defined by race adequately.
In the 12-week study, 78% of subjects achieved a 15% increase from baseline FEV 1 following the first dose of PERFOROMIST Inhalation Solution 20 mcg. In these subjects, the median time to onset of bronchodilation, defined as 15% increase in FEV 1 , was 11.7 minutes. When defined as an increase in FEV 1 of 12% and 200 mL, the time to onset of bronchodilation was 13.1 minutes after dosing. The median time to peak bronchodilator effect was 2 hours after dosing.
HOW SUPPLIED/STORAGE AND HANDLING
PERFOROMIST (formoterol fumarate) Inhalation Solution is supplied as a 2 mL sterile solution for nebulization in 2.5 mL low-density polyethylene unit dose vials. Each vial is overwrapped in a foil pouch and supplied in cartons as listed below.
Carton of 30 individually wrapped unit dose vials, NDC 49502-605-30
Carton of 60 individually wrapped unit dose vials, NDC 49502-605-61
Storage and Handling:
Prior to dispensing to the patient : Store in a refrigerator, 2°C to 8°C (36°F to 46°F). Protect pouch from light and heat.
After dispensing to the patient: Store in a refrigerator at 2°C to 8°C (36°F to 46°F) and discard when drug expires or store at room temperature, 20°C to 25°C (68°F to 77°F) and discard if not used after 3 months. Protect pouch from light and heat.
- PERFOROMIST Inhalation Solution should only be administered via a standard jet nebulizer connected to an air compressor with an adequate airflow and equipped with a facemask or mouthpiece.
- Vial should always be stored in the foil pouch, and only removed IMMEDIATELY before use.
- Do not take by mouth.
- Contents of any partially used container should be discarded.
- Discard the container and top after use.
- Keep out of the reach of children
Mechanism of Action
Formoterol fumarate is a long-acting, beta 2 -adrenergic receptor agonist (beta 2 -agonist). Inhaled formoterol fumarate acts locally in the lung as a bronchodilator. In vitro studies have shown that formoterol has more than 200-fold greater agonist activity at beta 2 -receptors than at beta 1 -receptors. Although beta 2 -receptors are the predominant adrenergic receptors in bronchial smooth muscle and beta 1 -receptors are the predominant receptors in the heart, there are also beta 2 -receptors in the human heart comprising 10% to 50% of the total beta-adrenergic receptors. The precise function of these receptors has not been established, but they raise the possibility that even highly selective beta 2 -agonists may have cardiac effects.
The pharmacologic effects of beta 2 -adrenoceptor agonist drugs, including formoterol, are at least in part attributable to stimulation of intracellular adenyl cyclase, the enzyme that catalyzes the conversion of adenosine triphosphate (ATP) to cyclic-3', 5'-adenosine monophosphate (cyclic AMP). Increased cyclic AMP levels cause relaxation of bronchial smooth muscle and inhibition of release of mediators of immediate hypersensitivity from cells, especially from mast cells.
In vitro tests show that formoterol is an inhibitor of the release of mast cell mediators, such as histamine and leukotrienes, from the human lung. Formoterol also inhibits histamine-induced plasma albumin extravasation in anesthetized guinea pigs and inhibits allergen-induced eosinophil influx in dogs with airway hyper-responsiveness. The relevance of these in vitro and animal findings to humans with COPD is unknown.