Get your patient on Takhzyro (Lanadelumab-Flyo)
Takhzyro prior authorization resources
Most recent state uniform prior authorization forms
Brand Resources
Takhzyro patient education
Patient toolkit
Dosage & administration
DOSAGE AND ADMINISTRATION
For subcutaneous use only.
Recommended Dosage:
- Adult and pediatric patients 12 years of age and older: administer 300 mg every 2 weeks by the patient or caregiver. Dosing interval every 4 weeks may be considered in some patients. (2.1 )
- Pediatric patients 6 to less than 12 years of age: administer 150 mg every 2 weeks by a healthcare provider or caregiver. Dosing interval every 4 weeks may be considered in some patients. (2.2 )
- Pediatric patients 2 to less than 6 years of age: administer 150 mg every 4 weeks by a healthcare provider or caregiver. (2.2 )
- See Full Prescribing Information for Administration Instructions. (2.3 )
Recommended Dosage for Adult and Pediatric Patients 12 Years of Age and Older
The recommended starting dosage in adult and pediatric patients 12 years of age and older is 300 mg administered subcutaneously every 2 weeks (q2wks). A dosing interval of 300 mg every 4 weeks (q4wks) is also effective and may be considered if the patient is well-controlled (e.g., attack free) for more than 6 months.
Recommended Dosage for Pediatric Patients 2 to Less Than 12 Years of Age
Pediatric Patients 6 to Less Than 12 Years of Age
The recommended starting dosage in pediatric patients 6 to less than 12 years of age is 150 mg administered subcutaneously q2wks. A dosing interval of 150 mg q4wks may be considered if the patient is well-controlled (e.g., attack free) for more than 6 months.
Pediatric Patients 2 to Less Than 6 Years of Age
The recommended dosage in pediatric patients 2 to less than 6 years of age is 150 mg administered subcutaneously q4wks.
Preparation and Administration Instructions
TAKHZYRO is administered subcutaneously only.
TAKHZYRO is intended for administration by a healthcare provider, patient or caregiver.
The patient or caregiver should be trained in subcutaneous injection technique by a healthcare professional.
- Adult and pediatric patients 12 years of age and older: TAKHZYRO may be administered by the patient or caregiver.
- Pediatric patients 2 to less than 12 years of age: TAKHZYRO should be administered by a healthcare provider or caregiver.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. Do not use TAKHZYRO if the solution appears discolored or contains visible particles. TAKHZYRO is a clear to slightly opalescent, colorless to slightly yellow solution.
Administration Instructions for Single-Dose Prefilled Syringes
Instruct patients and/or caregiver on proper use of the TAKHZYRO prefilled syringe and assess that they are well trained in subcutaneous injection technique prior to administration by patient and/or caregiver.
Avoid vigorous agitation of the prefilled syringe.
Take the TAKHZYRO prefilled syringe out of the refrigerator 15 minutes before injecting to allow it to equilibrate to room temperature.
Using aseptic technique, inject TAKHZYRO subcutaneously into the abdomen, thigh, or upper arm.
Discard any unused portion of drug remaining in the prefilled syringe.
For detailed instructions on the preparation and administration of TAKHZYRO see Instructions for Use for either single-dose 1 mL prefilled syringe or single-dose 2 mL prefilled syringe.
Administration Instructions for Single-Dose Vial
TAKHZYRO vial is provided as a ready-to-use solution that does not require additional reconstitution or dilution for administration.
Instruct patients and/or caregivers on proper use of TAKHZYRO from a vial and assess that they are well trained in subcutaneous injection technique prior to administration by patient and/or caregiver.
Avoid vigorous agitation of the vial.
Take the TAKHZYRO vial out of the refrigerator 15 minutes before injecting to allow it to equilibrate to room temperature.
Using aseptic technique, withdraw the prescribed dose of TAKHZYRO from the vial using an 18-gauge needle. Change the needle on the syringe to a 27-gauge, ½-inch needle or other needle suitable for subcutaneous injection. Inject TAKHZYRO subcutaneously into the abdomen, thigh, or upper arm. In clinical studies, the majority of patients self-administered TAKHZYRO over 10 to 60 seconds.
TAKHZYRO should be administered within 2 hours of preparing the dosing syringe. After the dosing syringe is prepared, it can be refrigerated at 36°F to 46°F (2°C to 8°C) and must be used within 8 hours.
Discard any unused portions of drug remaining in the vial and dosing syringe.
For detailed instructions on the preparation and administration of TAKHZYRO see single-dose vial Instructions for Use .

By using PrescriberAI, you agree to the AI Terms of Use.
Takhzyro prescribing information
INDICATIONS AND USAGE
TAKHZYRO ® is indicated for prophylaxis to prevent attacks of hereditary angioedema (HAE) in adult and pediatric patients aged 2 years and older.
DOSAGE AND ADMINISTRATION
For subcutaneous use only.
Recommended Dosage:
- Adult and pediatric patients 12 years of age and older: administer 300 mg every 2 weeks by the patient or caregiver. Dosing interval every 4 weeks may be considered in some patients. (2.1 )
- Pediatric patients 6 to less than 12 years of age: administer 150 mg every 2 weeks by a healthcare provider or caregiver. Dosing interval every 4 weeks may be considered in some patients. (2.2 )
- Pediatric patients 2 to less than 6 years of age: administer 150 mg every 4 weeks by a healthcare provider or caregiver. (2.2 )
- See Full Prescribing Information for Administration Instructions. (2.3 )
Recommended Dosage for Adult and Pediatric Patients 12 Years of Age and Older
The recommended starting dosage in adult and pediatric patients 12 years of age and older is 300 mg administered subcutaneously every 2 weeks (q2wks). A dosing interval of 300 mg every 4 weeks (q4wks) is also effective and may be considered if the patient is well-controlled (e.g., attack free) for more than 6 months.
Recommended Dosage for Pediatric Patients 2 to Less Than 12 Years of Age
Pediatric Patients 6 to Less Than 12 Years of Age
The recommended starting dosage in pediatric patients 6 to less than 12 years of age is 150 mg administered subcutaneously q2wks. A dosing interval of 150 mg q4wks may be considered if the patient is well-controlled (e.g., attack free) for more than 6 months.
Pediatric Patients 2 to Less Than 6 Years of Age
The recommended dosage in pediatric patients 2 to less than 6 years of age is 150 mg administered subcutaneously q4wks.
Preparation and Administration Instructions
TAKHZYRO is administered subcutaneously only.
TAKHZYRO is intended for administration by a healthcare provider, patient or caregiver.
The patient or caregiver should be trained in subcutaneous injection technique by a healthcare professional.
- Adult and pediatric patients 12 years of age and older: TAKHZYRO may be administered by the patient or caregiver.
- Pediatric patients 2 to less than 12 years of age: TAKHZYRO should be administered by a healthcare provider or caregiver.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. Do not use TAKHZYRO if the solution appears discolored or contains visible particles. TAKHZYRO is a clear to slightly opalescent, colorless to slightly yellow solution.
Administration Instructions for Single-Dose Prefilled Syringes
Instruct patients and/or caregiver on proper use of the TAKHZYRO prefilled syringe and assess that they are well trained in subcutaneous injection technique prior to administration by patient and/or caregiver.
Avoid vigorous agitation of the prefilled syringe.
Take the TAKHZYRO prefilled syringe out of the refrigerator 15 minutes before injecting to allow it to equilibrate to room temperature.
Using aseptic technique, inject TAKHZYRO subcutaneously into the abdomen, thigh, or upper arm.
Discard any unused portion of drug remaining in the prefilled syringe.
For detailed instructions on the preparation and administration of TAKHZYRO see Instructions for Use for either single-dose 1 mL prefilled syringe or single-dose 2 mL prefilled syringe.
Administration Instructions for Single-Dose Vial
TAKHZYRO vial is provided as a ready-to-use solution that does not require additional reconstitution or dilution for administration.
Instruct patients and/or caregivers on proper use of TAKHZYRO from a vial and assess that they are well trained in subcutaneous injection technique prior to administration by patient and/or caregiver.
Avoid vigorous agitation of the vial.
Take the TAKHZYRO vial out of the refrigerator 15 minutes before injecting to allow it to equilibrate to room temperature.
Using aseptic technique, withdraw the prescribed dose of TAKHZYRO from the vial using an 18-gauge needle. Change the needle on the syringe to a 27-gauge, ½-inch needle or other needle suitable for subcutaneous injection. Inject TAKHZYRO subcutaneously into the abdomen, thigh, or upper arm. In clinical studies, the majority of patients self-administered TAKHZYRO over 10 to 60 seconds.
TAKHZYRO should be administered within 2 hours of preparing the dosing syringe. After the dosing syringe is prepared, it can be refrigerated at 36°F to 46°F (2°C to 8°C) and must be used within 8 hours.
Discard any unused portions of drug remaining in the vial and dosing syringe.
For detailed instructions on the preparation and administration of TAKHZYRO see single-dose vial Instructions for Use .
DOSAGE FORMS AND STRENGTHS
TAKHZYRO is a sterile, preservative-free, clear to slightly opalescent, colorless to slightly yellow solution available in the following presentations.
- Injection: 150 mg/1 mL (150 mg/mL) solution in a single-dose prefilled syringe
- Injection: 300 mg/2 mL (150 mg/mL) solution in a single-dose prefilled syringe
- Injection: 300 mg/2 mL (150 mg/mL) solution in a single-dose vial
USE IN SPECIFIC POPULATIONS
Pregnancy
Risk Summary
There are no available data on TAKHZYRO use in pregnant women to inform any drug associated risks. Monoclonal antibodies such as lanadelumab-flyo are transported across the placenta during the third trimester of pregnancy; therefore, potential effects on a fetus are likely to be greater during the third trimester of pregnancy. An enhanced pre-and postnatal development (ePPND) study conducted in pregnant monkeys at doses resulting in exposures of up to 33 times the exposure achieved (on an AUC basis) at the maximum recommended human dose (MRHD) revealed no evidence of harm to the developing fetus.
The background risk of major birth defects and miscarriage for the indicated population is unknown. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Data
Animal Data
In the ePPND study, pregnant cynomolgus monkeys were administered lanadelumab-flyo once weekly at subcutaneous doses resulting in up to 33 times the exposure at the MRHD (on an AUC basis with maternal subcutaneous doses up to 50 mg/kg/week) from gestation day 20, at the beginning of organogenesis, through to parturition. There were no lanadelumab-flyo-related effects on maintenance of pregnancy or parturition. Maternal lanadelumab-flyo treatment had no effects on embryo-fetal development, survival, growth, or postnatal development of offspring through 3 months of age. Lanadelumab-flyo crossed the placenta in monkeys. Offspring were exposed to lanadelumab-flyo at approximately 50% of the maternal plasma concentration out to postnatal day 21 (PND 21). Lanadelumab-flyo concentrations were approximately equivalent in maternal and offspring plasma at PND 90.
Lactation
Risk Summary
There are no data on the presence of lanadelumab-flyo in human milk, its effects on the breastfed infant, or its effects on milk production. Lanadelumab-flyo was detected in the milk of lactating cynomolgus monkeys at approximately 0.2% of the maternal plasma concentration. The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for TAKHZYRO and any potential adverse effects on the breastfed infant from TAKHZYRO or from the underlying maternal condition.
Data
Animal Data
Available pharmacokinetic data in cynomolgus monkeys have shown excretion of lanadelumab-flyo in milk at approximately 0.2% of the maternal plasma level.
Pediatric Use
The safety and effectiveness of TAKHZYRO for prophylaxis to prevent attacks of hereditary angioedema (HAE) have been established in pediatric patients 2 years of age and older.
Use of TAKHZYRO for this indication in patients 12 years of age and older was supported by a subgroup analysis by age of 10 patients aged 12 to <18 years in Trial 1 (a randomized, double-blind, placebo-controlled parallel-group study in adult and pediatric patients 12 years of age and older with HAE). Results of the subgroup analysis by age were consistent with overall study results. An additional 13 pediatric patients aged 12 to <18 years were enrolled in the open-label extension study [see Adverse Reactions (6.1) , Clinical Pharmacology (12.3) and Clinical Studies (14) ].
Use of TAKHZYRO for this indication in patients 2 to less than 12 years of age was supported by extrapolation of efficacy data from Trial 1, an adequate and well controlled study in adult and pediatric (12 to less than 18 years of age) patients, with additional pharmacokinetic analyses showing similar drug exposures between adults (>18 years of age) and pediatric patients (2 to less than 12 years of age), and safety and pharmacodynamic data from an open-label, multicenter study in pediatric patients with HAE aged 2 to less than 12 years that enrolled 21 patients (4 patients were aged 2 to less than 6 years and 17 patients were 6 to less than 12 years of age) [see Adverse Reactions (6.1) and Clinical Pharmacology (12.3) ] . The pharmacodynamic response observed in this trial for pediatric patients 2 to less than 12 years of age was similar to that seen in adult and pediatric patients 12 years of age and older [see Clinical Pharmacology (12.2) ] .
The safety and effectiveness of TAKHZYRO in pediatric patients less than 2 years of age have not been established.
Geriatric Use
The safety and effectiveness of TAKHZYRO were evaluated in a subgroup of patients (N=5) aged ≥65 years in Trial 1. Results of the subgroup analysis by age were consistent with overall study results [see Adverse Reactions (6.1) , Clinical Pharmacology (12.3) and Clinical Studies (14) ] .
CONTRAINDICATIONS
None.
WARNINGS AND PRECAUTIONS
Hypersensitivity reactions have been observed. In case of a severe hypersensitivity reaction, discontinue TAKHZYRO administration and institute appropriate treatment. (5.1 )
Hypersensitivity Reactions
Hypersensitivity reactions have been observed. In case of a severe hypersensitivity reaction, discontinue TAKHZYRO administration and institute appropriate treatment.
ADVERSE REACTIONS
The most common adverse reactions (≥10%) are injection site reactions, upper respiratory infections, headache, rash, dizziness, diarrhea, and myalgia. (6.1 )
To report SUSPECTED ADVERSE REACTIONS, contact Takeda Pharmaceuticals at 1-877-TAKEDA-7 (1-877-825-3327) or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch .
Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Adult and Pediatric Patients 12 Years of Age and Older
The safety of TAKHZYRO is primarily based on a 26-week, randomized, double-blind, parallel-group and placebo-controlled study (Trial 1) in 125 patients with Type I or II HAE. Eligible patients were also able to participate in an open-label extension study (Trial 2) up to 130 weeks. In Trial 1, a total of 84 patients with HAE aged 12 years and older received at least one dose of TAKHZYRO. Overall, 70% of patients were female and 90% of patients were Caucasian with a mean age of 41 years. The proportion of patients who discontinued study drug prematurely due to adverse events was 1.2% for TAKHZYRO-treated patients and 4.9% for placebo-treated patients. No deaths occurred in the trial.
The safety profile of TAKHZYRO was generally similar across all subgroups of patients, including analysis by age, sex, and geographic region.
Table 1 shows adverse reactions occurring in ≥10% of patients in any TAKHZYRO treatment group that also occurred at a higher rate than in the placebo treatment group in Trial 1.
| Adverse Reaction | Placebo (N=41) | TAKHZYRO | |||
|---|---|---|---|---|---|
| 150 mg q4wks (N=28) | 300 mg q4wks (N=29) | 300 mg q2wks (N=27) | Total (N=84) | ||
| n (%) | n (%) | n (%) | n (%) | n (%) | |
| N= number of patients; n =number of patients experiencing the event; q2wks = every 2 weeks; q4wks = every 4 weeks | |||||
| Injection site reactions Injection site reactions include: pain, erythema, bruising, hematoma, hemorrhage, pruritus, swelling, induration, paresthesia, reaction, warmth, edema and rash. | 14 (34) | 16 (57) | 13 (45) | 15 (56) | 44 (52) |
| Upper respiratory infection Includes upper respiratory infection, viral upper respiratory infection | 13 (32) | 3 (11) | 9 (31) | 12 (44) | 24 (29) |
| Headache Includes headache, tension headache, sinus headache | 9 (22) | 3 (11) | 6 (21) | 9 (33) | 18 (21) |
| Rash Includes rash, rash maculopapular, rash erythematous | 2(5) | 2 (7) | 3 (10) | 1 (4) | 6 (7) |
| Dizziness | 0 | 1 (4) | 3 (10) | 1 (4) | 5 (6) |
| Diarrhea | 2 (5) | 3 (11) | 0 | 1 (4) | 4 (5) |
| Myalgia | 0 | 1 (4) | 0 | 3 (11) | 4 (5) |
Injection site reactions primarily consisted mainly of pain, erythema, and bruising at the injection site. There was no meaningful difference in injection site reactions with self-administration.
Less Common Adverse Reactions
Other adverse reactions that occurred at a higher incidence in TAKHZYRO-treated patients compared to placebo include hypersensitivity (1% vs 0%), increased aspartate transaminase (2% vs 0%), and increased alanine transaminase (2% vs 0%).
Safety data from the open-label extension study, consisting of 109 rollover patients from Trial 1 and 103 non-rollover HAE patients, is consistent with controlled safety data from Trial 1.
Laboratory Abnormalities
Transaminase elevations
During the placebo-controlled treatment period in Trial 1, the number of TAKHZYRO-treated patients with maximum transaminase (ALT or AST) levels >8, >5, or >3 times the upper limit of normal (ULN) was 1 (1.2%), 0 (0%), or 3 (3.6%) respectively, compared to 0 in the placebo-treated patients. These transaminase elevations were asymptomatic and transient. No patients had elevated total bilirubin >2× ULN. One TAKHZYRO-treated patient permanently discontinued treatment due to elevated transaminases (4.1× ULN AST). None of the patients were reported to have serious adverse reactions of elevated transaminases.
Pediatric Patients 2 to Less Than 12 Years of Age
The safety of TAKHZYRO was evaluated at 150 mg/mL (150 mg q4wks for patients 2 to <6 years or 150 mg q2wks with the option for 150 mg q4wks if the patient is well-controlled for 6 months for patients 6 to <12 years) in an open-label, multicenter study with 21 patients aged 2 to less than 12 years. No new safety signals were observed in these patients.
DRUG INTERACTIONS
No dedicated drug interaction studies have been conducted [see Clinical Pharmacology (12.3) ].
Drug-Laboratory Test Interactions
Coagulation tests
TAKHZYRO can increase activated partial thromboplastin time (aPTT) due to an interaction of TAKHZYRO with the aPTT assay. The reagents used in the aPTT laboratory test initiate intrinsic coagulation through the activation of plasma kallikrein in the contact system. Inhibition of plasma kallikrein by TAKHZYRO can increase aPTT in this assay. In Trial 1, prolongation of aPTT (>1× ULN) was observed at one or more time points in 3, 9, and 11 patients treated with TAKHZYRO 150 mg q4wks, 300 mg q4wks, and 300 mg q2wks, respectively, compared to 5 placebo-treated patients. Only one patient in the 300 mg q2wks treatment group experienced transient aPTT prolongation ≥1.5x ULN which was confounded by ongoing heparin therapy. None of the increases in aPTT in patients treated with TAKHZYRO were associated with abnormal bleeding adverse events. There were no differences in INR values between treatment groups.
DESCRIPTION
Lanadelumab-flyo, a plasma kallikrein inhibitor, is a non-plasma derived, recombinant, fully human, monoclonal antibody (IgG1/κ-light chain) produced in Chinese Hamster Ovary (CHO) cells. Based on the amino acid sequence, the molecular weight of the non-glycosylated lanadelumab-flyo is 146 kDa. The calculated molecular mass of the fully reduced light chain is 23 kDa. The calculated molecular mass of the fully reduced and non-glycosylated heavy chain is 49 kDa.
TAKHZYRO (lanadelumab-flyo) injection is a sterile, preservative-free, clear to slightly opalescent, colorless to slightly yellow solution for subcutaneous use.
Each mL of ready-to-use TAKHZYRO solution contains 150 mg of lanadelumab-flyo, citric acid monohydrate (4.1 mg), L-histidine (7.8 mg), polysorbate 80 (0.1 mg), sodium chloride (5.3 mg), sodium phosphate dibasic dihydrate (5.3 mg), and Water for Injection, USP. The solution has a pH of approximately 6.0.
CLINICAL PHARMACOLOGY
Mechanism of Action
Lanadelumab-flyo is a fully human monoclonal antibody (IgG1/κ-light chain) that binds plasma kallikrein and inhibits its proteolytic activity. Plasma kallikrein is a protease that cleaves high-molecular-weight-kininogen (HMWK) to generate cleaved HMWK (cHMWK) and bradykinin, a potent vasodilator that increases vascular permeability resulting in swelling and pain associated with HAE. In patients with HAE due to C1-inhibitor (C1-INH) deficiency or dysfunction, normal regulation of plasma kallikrein activity is not present, which leads to uncontrolled increases in plasma kallikrein activity and results in angioedema attacks. Lanadelumab-flyo decreases plasma kallikrein activity to control excess bradykinin generation in patients with HAE.
Pharmacodynamics
In adult and pediatric (12 to less than 18 years) patients, concentration-dependent inhibition of plasma kallikrein, measured as reduction of cHMWK levels, was demonstrated after subcutaneous administration of TAKHZYRO 150 mg q4wks, 300 mg q4wks or 300 mg q2wks in patients with HAE.
For pediatric patients 2 to less than 6 years (150 mg q4wks) and 6 to less than 12 years (150 mg q2wks), the observed mean percent change from baseline cHMWK levels was similar to that observed in adult and pediatric (12 to less than 18 years) patients (300 mg q2wks or 300 mg q4wks).
Cardiac Electrophysiology
TAKHZYRO did not prolong the QT/QTc interval.
Pharmacokinetics
Following subcutaneous administration, the pharmacokinetics of lanadelumab-flyo was approximately dose-proportional in the therapeutic dose range in patients with HAE (Table 2). The pharmacokinetic properties and exposure (steady state) of lanadelumab-flyo in HAE patients, following subcutaneous administration of 150 mg q4wks, 300 mg q4wks and 300 mg q2wks, are provided in Table 2 . Following subcutaneous administration of TAKHZYRO, peak plasma concentrations are reached within 5 days, and terminal elimination half-life is ~ 2 weeks. The anticipated time to reach steady state concentration was approximately 70 days. At steady-state, the mean accumulation ratio is approximately 1.44, 1.42, and 2.43 for dosing regimen of 150 mg q4wks, 300 mg q4wks and 300 mg q2wks, respectively.
| Pharmacokinetic Parameters | Lanadelumab-flyo | ||
|---|---|---|---|
| 150 mg q4wks (N=28) | 300 mg q4wks (N=29) | 300 mg q2wks (N=27) | |
| CL/F: apparent clearance; Vc/F: apparent volume of distribution; AUC tau,ss : area under the curve over the dosing interval at steady-state; C max,ss : maximum concentration at steady-state; C min,ss : minimum concentration at steady state; T max : time to maximum concentration; t 1/2 terminal elimination half-life. | |||
| CL/F (L/day) | 0.667 (0.162) | 0.742 (0.239) | 0.809 (0.370) |
| Vc/F (L) | 14.1 (2.93) | 14.9 (4.45) | 16.6 (4.79) |
| AUC tau,ss (µg•day/mL) | 233 (56.6) | 441(137) | 408 (138) |
| C max,ss (µg/mL) | 12.0 (3.01) | 23.3 (7.94) | 34.4 (11.2) |
| C min,ss (µg/mL) | 4.81 (1.40) | 8.77 (2.80) | 25.4 (9.18) |
| t max (day) | 5.17 (1.09) | 5.17 (1.12) | 4.11 (0.377) |
| t 1/2 (day) | 14.9 (2.00) | 14.2 (1.89) | 15.0 (2.48) |
Specific Populations
Population pharmacokinetic analyses showed that age, gender and race did not meaningfully influence the pharmacokinetics of lanadelumab-flyo after correcting for body weight. Body weight was identified as an important covariate describing the variability of clearance and volume of distribution, resulting in higher exposure (AUC and C max ) in lighter patients. However, this difference is not considered to be clinically relevant and no dose adjustments are recommended for any of these demographics.
Pediatric Population
Based on population pharmacokinetics (PK) analyses, the geometric mean lanadelumab-flyo average concentration at steady state (C ave ) was approximately 25% higher following subcutaneous administration of TAKHZYRO 300 mg q2wks in pediatric patients 12 to less than 18 years of age than the mean C ave in adult patients under the same dosing regimen, due to lower body weight in pediatric patients. Lanadelumab-flyo exposures in pediatric patients 2 to less than 12 years of age receiving TAKHZYRO 150 mg q2wks or q4wks are comparable to those in adult patients receiving TAKHZYRO 300 mg q2wks. The geometric mean lanadelumab-flyo C ave was approximately 7% higher following subcutaneous administration of TAKHZYRO 150 mg q2wks in pediatric patients 6 to less than 12 years of age compared to the mean C ave in adult patients receiving 300 mg q2wks. The mean lanadelumab-flyo C ave was approximately 14% lower following subcutaneous administration of TAKHZYRO 150 mg q4wks in pediatric patients 2 to less than 6 years of age compared to the mean C ave in adult patients receiving 300 mg q2wks.
Renal Impairment
No dedicated studies have been conducted to evaluate the PK of lanadelumab-flyo in renal impairment patients. Based on population pharmacokinetic analysis, renal impairment (estimated GFR: 60 to 89 mL/min/1.73m 2 , [mild, N=98] and 30 to 59 mL/min/1.73m 2 , [moderate, N=9]) had no effect on the clearance or volume of distribution of lanadelumab-flyo.
Concomitant medications
The use of analgesic, antibacterial, antihistamine, anti-inflammatory and anti-rheumatic medications had no effect on clearance and volume of distribution of lanadelumab-flyo.
For breakthrough HAE attacks, use of rescue medications such as plasma-derived and recombinant C1-INH, icatibant or ecallantide had no effects on clearance and volume of distribution of lanadelumab-flyo.
Immunogenicity
The observed incidence of anti-drug antibodies is highly dependent on the sensitivity and specificity of the assay. Differences in assay methods preclude meaningful comparisons of the incidence of anti-drug antibodies in the studies described below with the incidence of anti-drug antibodies in other studies, including those of lanadelumab-flyo or of other lanadelumab products.
In Trial 1 with adult and pediatric patients 12 years of age and older, 10 (12%) lanadelumab-flyo-treated and 2 (5%) placebo-treated patients had at least 1 anti-drug antibody (ADA)-positive sample during the 26-week treatment period; antibody titers were low (range: 20 to 1280). The ADA response observed was transient in 2/10 lanadelumab-flyo and 1/2 placebo-treated patients. Pre-existing low titer antibodies were observed in 3 lanadelumab-flyo-treated patients and 1 placebo-treated patient with ADAs. Two patients receiving 150 mg q4wks had low titer antibodies classified as neutralizing.
In an open-label, multicenter study in pediatric patients 2 to less than 12 years of age, 3/20 (15%) lanadelumab-treated patients who completed the study developed ADAs during the 52-week treatment period; all of whom were in the 6 to less than 12 years age group. The ADA response observed was transient in all 3 patients. None of these patients had pre-existing antibodies. One patient had neutralizing antibodies.
The development of ADA including neutralizing antibodies against lanadelumab-flyo did not appear to adversely affect pharmacokinetics (PK), pharmacodynamics (PD), safety or clinical response.
NONCLINICAL TOXICOLOGY
Carcinogenesis, Mutagenesis, Impairment of Fertility
Animal studies have not been conducted to evaluate the carcinogenic potential of lanadelumab-flyo. Published literature supports bradykinin, which is elevated in HAE, as a pro-tumorigenic molecule. However, the malignancy risk in humans from an antibody that inhibits plasma kallikrein activity, such as lanadelumab-flyo, which lowers bradykinin levels, is currently unknown.
Male and female fertility were unaffected based upon no observed adverse histopathological findings in the reproductive organs from sexually mature cynomolgus monkeys that received lanadelumab-flyo for 13 weeks at subcutaneous doses up to 50 mg/kg/week (resulting in approximately 22 times the exposure at the MRHD on an AUC basis).
CLINICAL STUDIES
Trial 1 (NCT02586805)
The efficacy of TAKHZYRO for the prevention of angioedema attacks in patients 12 years of age and older with Type I or II HAE was demonstrated in a multicenter, randomized, double-blind, placebo-controlled parallel-group study (Trial 1).
The study included 125 adult and pediatric patients (12 years of age and older) with Type I or II HAE who experienced at least one investigator-confirmed attack per 4 weeks during the run-in period. Patients were randomized into 1 of 4 parallel treatment arms, stratified by baseline attack rate, in a 3:2:2:2 ratio (placebo, lanadelumab-flyo 150 mg q4wks, lanadelumab-flyo 300 mg q4wks, or lanadelumab-flyo 300 mg q2wks by subcutaneous injection) for the 26-week treatment period. Patients ≥18 years of age were required to discontinue other prophylactic HAE medications prior to entering the study; however, all patients were allowed to use rescue medications for treatment of breakthrough HAE attacks.
Overall, 90% of patients had Type I HAE. A history of laryngeal angioedema attacks was reported in 65% of patients and 56% were on prior long-term prophylaxis. During the study run-in period, attack rates of ≥3 attacks/month were observed in 52% of patients overall.
All TAKHZYRO treatment arms produced clinically meaningful and statistically significant reductions in the mean HAE attack rate compared to placebo across all primary and secondary endpoints in the Intent-to-Treat population (ITT) as shown in Table 3 .
| Endpoint Statistics | Placebo (N=41) | TAKHZYRO | ||
|---|---|---|---|---|
| 150 mg q4wks (N=28) | 300 mg q4wks (N=29) | 300 mg q2wks (N=27) | ||
| CI=confidence interval; LS=least squares. Note: Results are from a Poisson regression model accounting for over dispersion with fixed effects for treatment group (categorical) and normalized baseline attack rate (continuous), and the logarithm of time in days each patient was observed during the treatment period as an offset variable in the model. | ||||
| Number of HAE Attacks from Day 0 to 182 Primary efficacy endpoint. | ||||
| LS Mean (95% CI) monthly attack rate Model-based treatment period HAE attack rate (attacks/4 weeks). | 1.97 (1.64, 2.36) | 0.48 (0.31, 0.73) | 0.53 (0.36, 0.77) | 0.26 (0.14, 0.46) |
| % Reduction relative to placebo (95% CI) Calculated as the ratio of the model-based treatment period HAE attack rates (lanadelumab/placebo) minus 1 multiplied by 100. | 76 (61, 85) | 73 (59, 82) | 87 (76, 93) | |
| Adjusted p-values Adjusted p-values for multiple testing. | <0.001 | <0.001 | <0.001 | |
| Number of HAE Attacks Requiring Acute Treatment from Day 0 to 182 | ||||
| LS Mean (95% CI) monthly attack rate | 1.64 (1.34, 2.00) | 0.31 (0.18, 0.53) | 0.42 (0.28, 0.65) | 0.21 (0.11, 0.40) |
| % Reduction relative to placebo (95% CI) | 81 (66, 89) | 74 (59, 84) | 87 (75, 93) | |
| Adjusted p-values | <0.001 | <0.001 | <0.001 | |
| Number of Moderate or Severe HAE Attacks from Day 0 to 182 | ||||
| LS Mean (95% CI) monthly attack rate | 1.22 (0.97, 1.52) | 0.36 (0.22, 0.58) | 0.32 (0.20, 0.53) | 0.20 (0.11, 0.39) |
| % Reduction relative to placebo (95% CI) | 70 (50, 83) | 73 (54, 84) | 83 (67, 92) | |
| Adjusted p-values | <0.001 | <0.001 | <0.001 | |
The mean reduction in HAE attack rate was consistently higher across the TAKHZYRO treatment arms compared to placebo regardless of the baseline history of prior long-term prophylaxis, laryngeal attacks, or attack rate during the run-in period.
Additional pre-defined exploratory endpoints included the percentage of patients who were attack free for the entire 26-week treatment period and the percentage of patients achieving threshold (≥50%, ≥70%, ≥90%) reductions in HAE attack rates compared to run-in during the 26-week treatment period. A ≥50% reduction in HAE attack rate was observed in 100% of patients on 300 mg q2wks or q4wks and 89% on 150 mg q4wks compared to 32% of placebo patients. A ≥70% reduction in HAE attack rates was observed in 89%, 76%, and 79% of patients on 300 mg q2wks, 300 mg q4wks, and 150 mg q4wks, respectively, compared to 10% of placebo patients. A ≥90% reduction in HAE attack rates was observed 67%, 55%, and 64% of patients on 300 mg q2wks, 300 mg q4wks, and 150 mg q4wks, respectively, compared to 5% of placebo patients.
The percentage of attack-free patients for the entire 26-week treatment period was 44%, 31%, and 39% in the TAKHZYRO 300 mg q2wks, 300 mg q4wks, and 150 mg q4wks groups respectively, compared to 2% of placebo patients.
Trial 2 (NCT02741596)
Patients who completed Trial 1 were eligible to rollover into an open-label extension study. Rollover patients, regardless of randomization group in Trial 1, received a single dose of TAKHZYRO 300 mg at study entry and were followed until the first HAE attack occurred. All efficacy endpoints were exploratory in this uncontrolled, unblinded study. At week 4 post-dose, approximately 80% of patients who had been in the 300 mg q2wks treatment group (N=25) in Trial 1 remained attack-free. After the first HAE attack, all patients received open-label treatment with TAKHZYRO 300 mg q2wks.
HOW SUPPLIED/STORAGE AND HANDLING
How Supplied
TAKHZYRO (lanadelumab-flyo) injection is a ready-to-use, clear to slightly opalescent, colorless to slightly yellow solution supplied in the following presentations.
Single-dose prefilled syringe
- Supplied in a carton containing one single-dose prefilled syringe with a bromobutyl rubber stopper, 27-gauge, ½-inch staked needle and rigid needle cap.
- NDC 47783-645-01: 150 mg/mL prefilled syringe
- NDC 47783-646-01: 300 mg/2 mL (150 mg/mL) prefilled syringe
Single-dose vial
- Supplied in a carton containing one single-dose glass vial with chlorobutyl rubber stopper, aluminum crimp seal and polypropylene flip-off cap.
- NDC 47783-644-01: 300 mg/2 mL (150 mg/mL) vial
Storage and Handling
- Store the prefilled syringes and vials refrigerated at 36°F to 46°F (2°C to 8°C).
- Do not freeze. Do not shake.
- Keep the prefilled syringe and vial in the original carton to protect from light.
INSTRUCTIONS FOR USE
TAKHZYRO ® (tak-ZYE-roe) (lanadelumab-flyo) injection, for subcutaneous use single-dose 1 mL prefilled syringe
This Instructions for Use contains information on how to inject TAKHZYRO. Please make sure to read, understand, and follow the Instructions for Use before injecting TAKHZYRO.
A healthcare provider should show you how to prepare and inject TAKHZYRO properly before you use it for the first time. Contact your healthcare provider if you have any questions.
| Important information: | |
| |
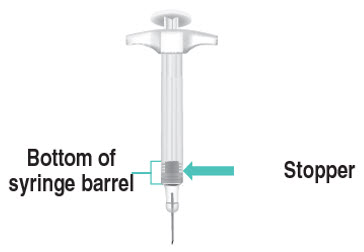
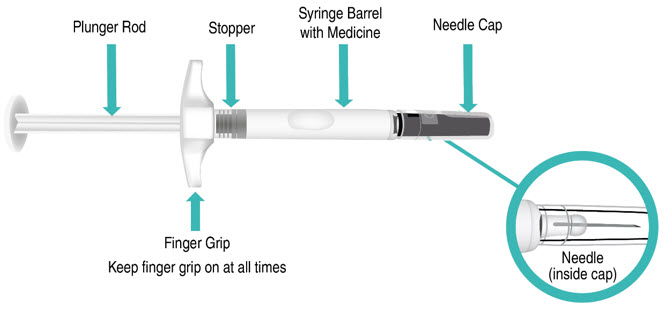 Figure A: TAKHZYRO prefilled syringe Figure A: TAKHZYRO prefilled syringe | |
| Storing TAKHZYRO: | |
|
Step 1: Prepare for your injection
| |
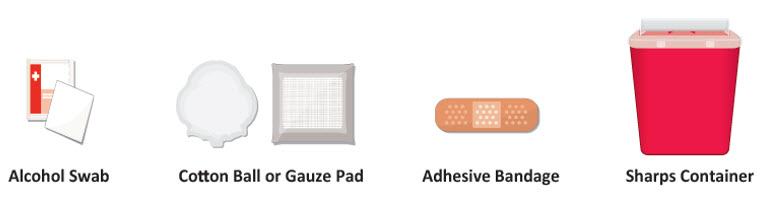 Figure B: Supplies Figure B: Supplies | |
|  |
|  Figure C: Remove prefilled syringe Figure C: Remove prefilled syringe |
| 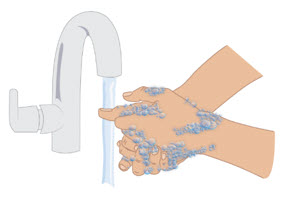 Figure D: Wash hands Figure D: Wash hands |
|  Figure E: Location of expiration date Figure E: Location of expiration date |
| 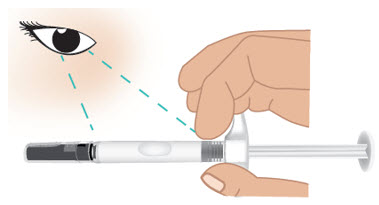 Figure F: Inspect the prefilled syringe Figure F: Inspect the prefilled syringe |
| Step 2: Select and prepare injection site | |
| 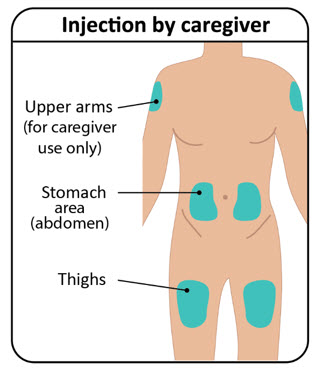 Figure G: Injection sites Figure G: Injection sites |
| 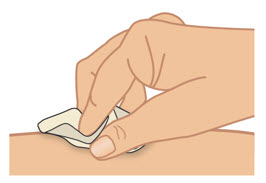 Figure H: Clean injection site Figure H: Clean injection site |
| 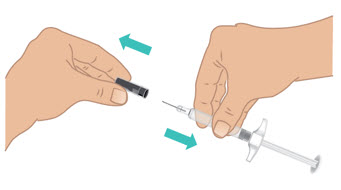 Figure I: Remove needle cap Figure I: Remove needle cap |
| |
Step 3: Inject TAKHZYRO
|  Figure J: Grip prefilled syringe Figure J: Grip prefilled syringe | |
|  Figure K: Pinch a 1-inch fold of skin Figure K: Pinch a 1-inch fold of skin | |
| 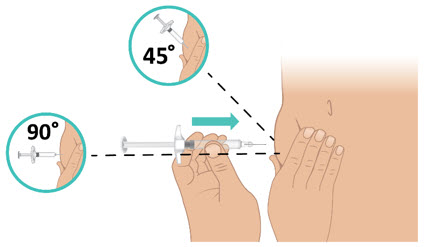 Figure L: Insert the needle Figure L: Insert the needle | |
| 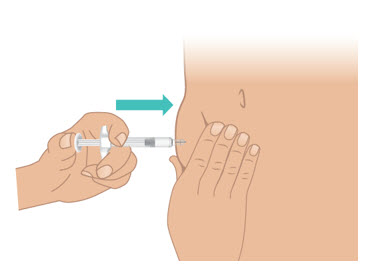 Figure M: Push the plunger rod all the way down Figure M: Push the plunger rod all the way down | |
| ||
| ||
Step 4: Throw away (dispose of) TAKHZYRO prefilled syringe
FDA-cleared sharps containers are generally available through pharmacies, medical supply companies, healthcare providers, and online. |  Figure O: Dispose in a sharps container Figure O: Dispose in a sharps container |
| |
Questions?
For product or service-related questions, call 1-877-TAKEDA-7 (1-877-825-3327) or go to www.TAKHZYRO.com .
Manufactured by: Takeda Pharmaceuticals U.S.A., Inc. Cambridge, MA 02142 U.S. License No. 1898
TAKHZYRO is a registered trademark of Dyax Corp. Takeda and  are registered trademarks of Takeda Pharmaceutical Company Limited. ©2025 Takeda Pharmaceuticals U.S.A., Inc. All rights reserved.
are registered trademarks of Takeda Pharmaceutical Company Limited. ©2025 Takeda Pharmaceuticals U.S.A., Inc. All rights reserved.
This Instructions for Use has been approved by the U.S. Food and Drug Administration.
Approved: 1/2025
Mechanism of Action
Lanadelumab-flyo is a fully human monoclonal antibody (IgG1/κ-light chain) that binds plasma kallikrein and inhibits its proteolytic activity. Plasma kallikrein is a protease that cleaves high-molecular-weight-kininogen (HMWK) to generate cleaved HMWK (cHMWK) and bradykinin, a potent vasodilator that increases vascular permeability resulting in swelling and pain associated with HAE. In patients with HAE due to C1-inhibitor (C1-INH) deficiency or dysfunction, normal regulation of plasma kallikrein activity is not present, which leads to uncontrolled increases in plasma kallikrein activity and results in angioedema attacks. Lanadelumab-flyo decreases plasma kallikrein activity to control excess bradykinin generation in patients with HAE.