Get your patient on Trelstar (Triptorelin Pamoate)
Trelstar prior authorization resources
Most recent state uniform prior authorization forms
Brand Resources
Trelstar patient education
Patient toolkit
Dosage & administration
2 DOSAGE AND ADMINISTRATION
TRELSTAR is administered as a single intramuscular injection in either buttock. Due to different release characteristics, the dosage strengths are not additive and must be selected based upon the desired dosing schedule. (2.1 )
Dosing Information
TRELSTAR must be administered under the supervision of a physician.
TRELSTAR is administered by a single intramuscular injection in either buttock. Dosing schedule depends on the product strength selected (Table 1). The lyophilized microgranules are to be reconstituted in sterile water. No other diluent should be used.
| Dosage | 3.75 mg | 11.25 mg | 22.5 mg |
| Recommended dose | 1 injection every 4 weeks | 1 injection every 12 weeks | 1 injection every 24 weeks |
Due to different release characteristics, the dosage strengths are not additive and must be selected based upon the desired dosing schedule.
The suspension should be administered within 2 minutes after reconstitution.
As with other drugs administered by intramuscular injection, the injection site should be alternated periodically.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
Reconstitution Instructions for TRELSTAR
Important: Please read the instructions completely and prepare the patient before you begin the injection kit activation and drug administration procedure.
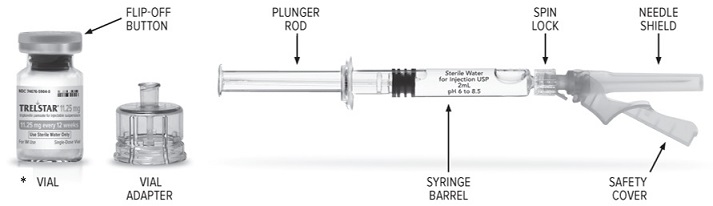
•The strength indicated on the vial in the figure above is for representative purposes only. All three strengths of the Trelstar vial have their individual strengths indicated on the label. Users will see either 3.75 mg, 11.25 mg or 22.5 mg, with the corresponding duration of treatment (4, 12 or 24 weeks respectively).
Preparation and Activation
Check that you are using the prescribed strength/dose (3.75 mg, 11.25 mg, or 22.5 mg) and that the expiry date has not passed, before preparation and activation.
Wash your hands with soap and hot water and put on gloves immediately prior to preparing the injection. Place the sealed tray on a clean, flat surface that is covered with a sterile pad or cloth. Peel the cover away from the tray and remove the injection kit components and TRELSTAR vial.
General Instructions and Recommendations
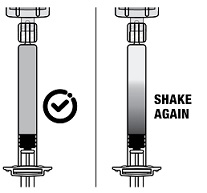
The product is a suspension of microgranules that can settle in the diluent. The final product to be administered is a suspension of microgranules with a milky, homogeneous appearance. If the product settles in the vial, shake it again to resuspend the microgranules.
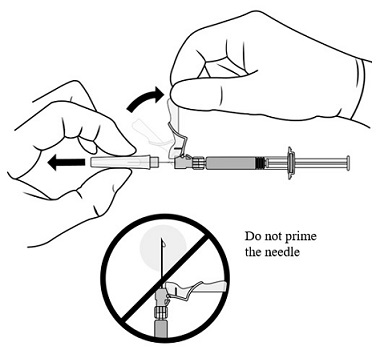
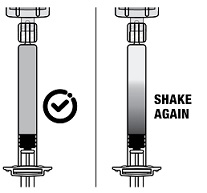
If the microgranules settle in the syringe, this will block the needle during administration. It is very important to inject the product within 2 minutes following reconstitution in the vial. If the product settles in the syringe, draw some air back into the syringe, shake it again, and expel the air (without priming the needle) before administering it.
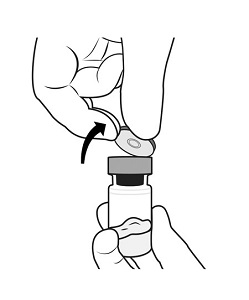 | STEP 1 – PREPARE VIAL Remove the flip-off button cap from the vial, revealing the rubber stopper. |
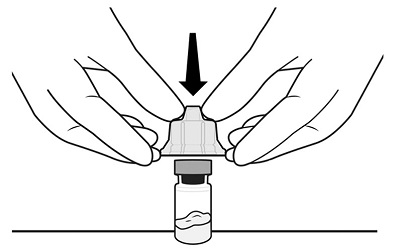 | STEP 2 – APPLY VIAL ADAPTER Peel the cover away from the blister pack containing the vial adapter. Do not remove the vial adapter from the blister pack. |
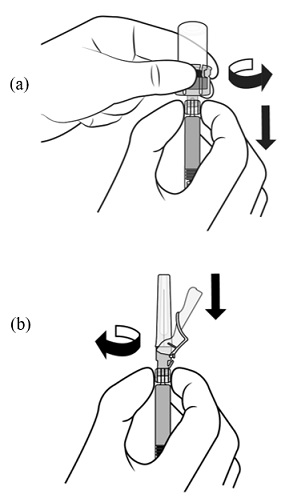
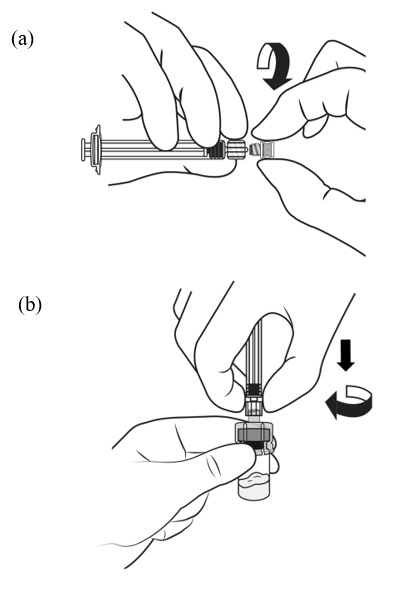 | STEP 3 – PREPARE SYRINGE AND CONNECT TO VIAL ADAPTER (a) Grasp the plastic ‘spin lock’ collar on the syringe barrel with index finger and thumb. Unscrew and discard the gray rubber cap from the syringe barrel. (b) Maintaining your grip on the spin lock, attach the syringe to the vial adapter by screwing the spin lock clockwise onto the vial adapter luer lock. Gently twist the spin lock until it stops turning to ensure a tight connection. |
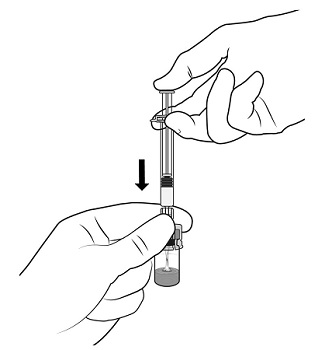 | STEP 4 – TRANSFER DILUENT TO VIAL Holding the vial and adapter with one hand, slowly push the plunger rod with the other hand and transfer all of the diluentinto the vial. |
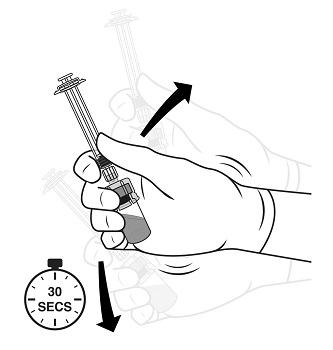 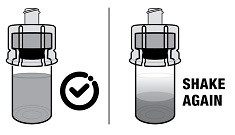 | STEP 5 – MIX TRELSTAR SUSPENSION Gripping the vial and vial adapter firmly, shake vigorously for 30 seconds to mix the contents thoroughly. This will ensure complete mixing of TRELSTAR and the sterile water diluent. Check the appearance of the suspension through the bottom of the vial. The suspension should appear homogeneous and milky. In order to avoid separation of the suspension, proceed to the next steps without delay.The product must be injected within less than 2 minutes from reconstitution.
|
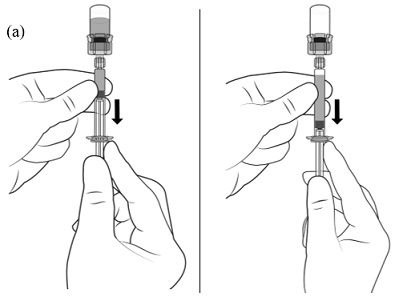 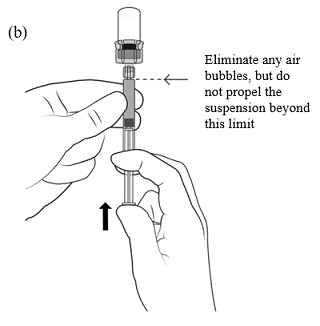  | STEP 6 – LOAD THE SYRINGE WITH TRELSTAR (a) Immediately invert the system so that the vial is at the top and the syringe is at the bottom. Pull back the plunger rod slowly to draw the reconstituted TRELSTAR into the syringe while maintaining pressure on the plunger rod to ensure it does not pull back too far. (b) Remove air bubbles by expelling air into the vial but do not propel the suspension beyond the luer lock. Note : If the product settles in the syringe, draw some air back into the syringe, shake it again, and expel the air (without priming the needle) before administering it. |
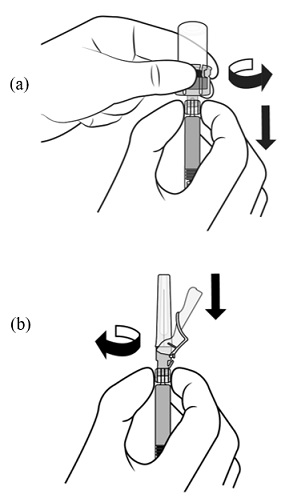 | STEP 7 – DISCONNECT VIAL ADAPTER AND CONNECT NEEDLE (a) Hold the barrel and spin lock firmly. |
 | STEP 8 – PREPARE FOR INJECTION Make sure that the patient is ready for the administration. |
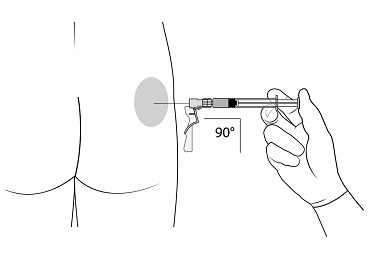 | STEP 9 – ADMINISTRATION Administer the injection by inserting the needle at a 90-degree angle into the large gluteal muscle. Ensure that the full amount of the product is injected within 10 seconds without interruption. Injection sites should be alternated. |
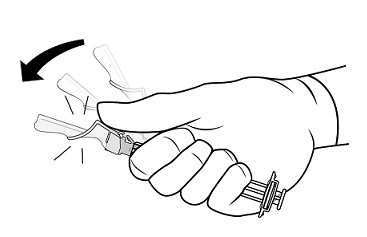 | STEP 10 – SAFETY LOCK AFTER INJECTION After administering the injection, immediately activate the safety mechanism by centering your thumb or forefinger on the textured finger pad area of the safety cover and pushing it forward over the needle until you hear or feel it lock in place. Use the one-handed technique and activate the mechanism away from yourself and others. Immediately discard the syringe into a sharps container after a single use. |

By using PrescriberAI, you agree to the AI Terms of Use.
Trelstar prescribing information
| Warnings and Precautions (5.6 ) | 09/2025 |
1 INDICATIONS AND USAGE
TRELSTAR is indicated for the treatment of advanced prostate cancer [ see Clinical Studies (14) ].
2 DOSAGE AND ADMINISTRATION
TRELSTAR is administered as a single intramuscular injection in either buttock. Due to different release characteristics, the dosage strengths are not additive and must be selected based upon the desired dosing schedule. (2.1 )
Dosing Information
TRELSTAR must be administered under the supervision of a physician.
TRELSTAR is administered by a single intramuscular injection in either buttock. Dosing schedule depends on the product strength selected (Table 1). The lyophilized microgranules are to be reconstituted in sterile water. No other diluent should be used.
| Dosage | 3.75 mg | 11.25 mg | 22.5 mg |
| Recommended dose | 1 injection every 4 weeks | 1 injection every 12 weeks | 1 injection every 24 weeks |
Due to different release characteristics, the dosage strengths are not additive and must be selected based upon the desired dosing schedule.
The suspension should be administered within 2 minutes after reconstitution.
As with other drugs administered by intramuscular injection, the injection site should be alternated periodically.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
Reconstitution Instructions for TRELSTAR
Important: Please read the instructions completely and prepare the patient before you begin the injection kit activation and drug administration procedure.
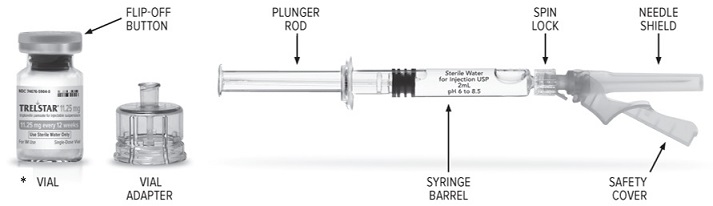
•The strength indicated on the vial in the figure above is for representative purposes only. All three strengths of the Trelstar vial have their individual strengths indicated on the label. Users will see either 3.75 mg, 11.25 mg or 22.5 mg, with the corresponding duration of treatment (4, 12 or 24 weeks respectively).
Preparation and Activation
Check that you are using the prescribed strength/dose (3.75 mg, 11.25 mg, or 22.5 mg) and that the expiry date has not passed, before preparation and activation.
Wash your hands with soap and hot water and put on gloves immediately prior to preparing the injection. Place the sealed tray on a clean, flat surface that is covered with a sterile pad or cloth. Peel the cover away from the tray and remove the injection kit components and TRELSTAR vial.
General Instructions and Recommendations
The product is a suspension of microgranules that can settle in the diluent. The final product to be administered is a suspension of microgranules with a milky, homogeneous appearance. If the product settles in the vial, shake it again to resuspend the microgranules.
If the microgranules settle in the syringe, this will block the needle during administration. It is very important to inject the product within 2 minutes following reconstitution in the vial. If the product settles in the syringe, draw some air back into the syringe, shake it again, and expel the air (without priming the needle) before administering it.
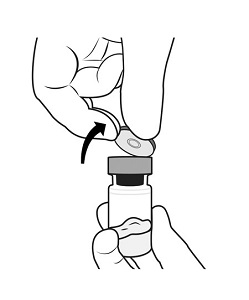 | STEP 1 – PREPARE VIAL Remove the flip-off button cap from the vial, revealing the rubber stopper. Place the vial in a standing upright position on the prepared surface. Disinfect the rubber stopper with the alcohol wipe. Discard the alcohol wipe and allow the stopper to dry. |
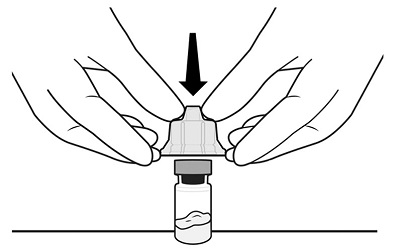 | STEP 2 – APPLY VIAL ADAPTER Peel the cover away from the blister pack containing the vial adapter. Do not remove the vial adapter from the blister pack. On a level surface, place the blister pack containing the vial adapter firmly on the vial top. Ensure the spike is centered and vertical when piercing the vial. Push down gently until you feel it snap into place. Remove the blister pack from the vial adapter. |
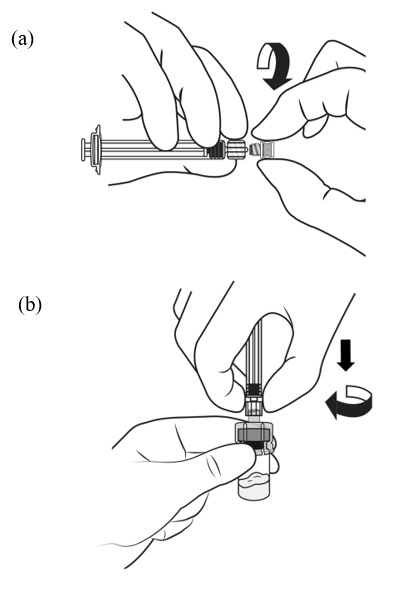 | STEP 3 – PREPARE SYRINGE AND CONNECT TO VIAL ADAPTER (a) Grasp the plastic ‘spin lock’ collar on the syringe barrel with index finger and thumb. Unscrew and discard the gray rubber cap from the syringe barrel. (b) Maintaining your grip on the spin lock, attach the syringe to the vial adapter by screwing the spin lock clockwise onto the vial adapter luer lock. Gently twist the spin lock until it stops turning to ensure a tight connection. Note: Overtightening can result in a poor connection and leakage. |
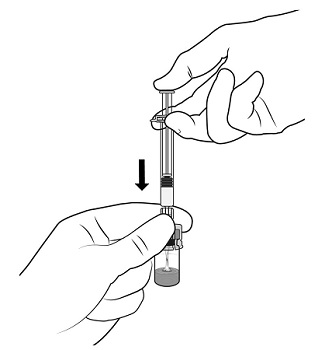 | STEP 4 – TRANSFER DILUENT TO VIAL Holding the vial and adapter with one hand, slowly push the plunger rod with the other hand and transfer all of the diluentinto the vial. |
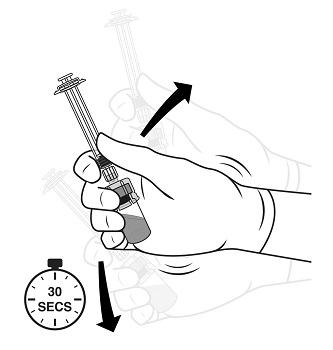 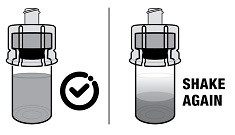 | STEP 5 – MIX TRELSTAR SUSPENSION Gripping the vial and vial adapter firmly, shake vigorously for 30 seconds to mix the contents thoroughly. This will ensure complete mixing of TRELSTAR and the sterile water diluent. Check the appearance of the suspension through the bottom of the vial. The suspension should appear homogeneous and milky. In order to avoid separation of the suspension, proceed to the next steps without delay.The product must be injected within less than 2 minutes from reconstitution. Note: If there is sedimentation in the vial, shake again. |
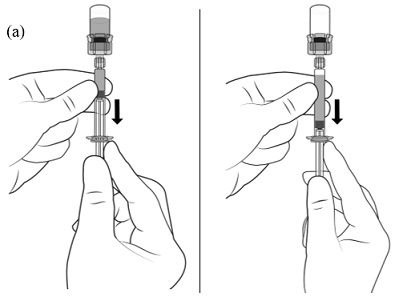 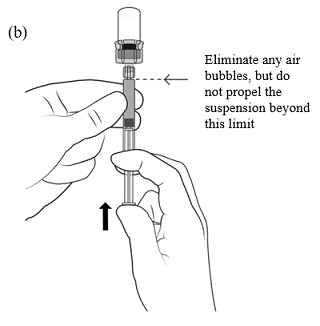  | STEP 6 – LOAD THE SYRINGE WITH TRELSTAR (a) Immediately invert the system so that the vial is at the top and the syringe is at the bottom. Pull back the plunger rod slowly to draw the reconstituted TRELSTAR into the syringe while maintaining pressure on the plunger rod to ensure it does not pull back too far. (b) Remove air bubbles by expelling air into the vial but do not propel the suspension beyond the luer lock. Note : If the product settles in the syringe, draw some air back into the syringe, shake it again, and expel the air (without priming the needle) before administering it. |
 | STEP 7 – DISCONNECT VIAL ADAPTER AND CONNECT NEEDLE (a) Hold the barrel and spin lock firmly. Hold the syringe barrel and spin lock with one hand and with the other hand turn the adapter counter-clockwise to disconnect the vial adapter and vial from the syringe. (b) Holding the syringe by the spin lock, attach the injection needle |
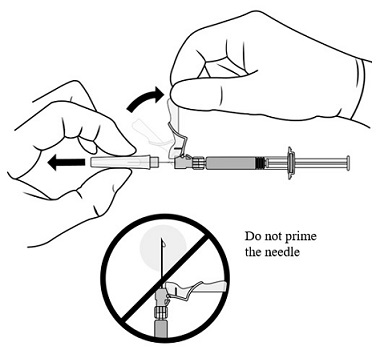 | STEP 8 – PREPARE FOR INJECTION Make sure that the patient is ready for the administration. Lift up the safety cover and remove the clear plastic needle shield by pulling it from the assembly. The safety cover should be perpendicular to the needle, with the needle facing away from you. Do not prime the needle. The syringe containing the TRELSTAR suspension is now ready for administration. The suspension should be administered immediately (less than 2 minutes) after reconstitutionto avoid excessive thickening of the suspension. |
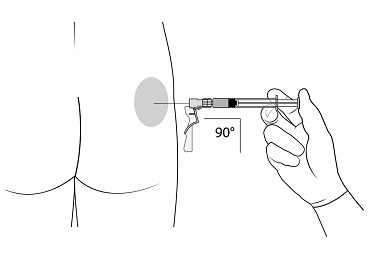 | STEP 9 – ADMINISTRATION Administer the injection by inserting the needle at a 90-degree angle into the large gluteal muscle. Ensure that the full amount of the product is injected within 10 seconds without interruption. Injection sites should be alternated. |
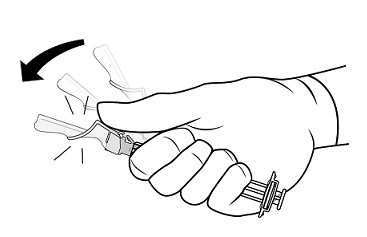 | STEP 10 – SAFETY LOCK AFTER INJECTION After administering the injection, immediately activate the safety mechanism by centering your thumb or forefinger on the textured finger pad area of the safety cover and pushing it forward over the needle until you hear or feel it lock in place. Use the one-handed technique and activate the mechanism away from yourself and others. Immediately discard the syringe into a sharps container after a single use. |
3 DOSAGE FORMS AND STRENGTHS
For injectable suspension: 3.75 mg, 11.25 mg, 22.5 mg of slightly yellow lyophilized microgranules in a single-dose vial for reconstitution with an injection kit containing one syringe filled with sterile water for injection, a vial adapter to help with reconstitution, and one needle (see figure in section 2.2).
8 USE IN SPECIFIC POPULATIONS
Females and males of reproductive potential: TRELSTAR may impair fertility. (8.3 )
Pregnancy
Risk Summary
Based on findings in animal studies and mechanism of action, TRELSTAR can cause fetal harm when administered to a pregnant woman [see Clinical Pharmacology (12.1) ] . Expected hormonal changes that occur with TRELSTAR treatment increase the risk for pregnancy loss. In animal developmental and reproductive toxicology studies, daily administration of triptorelin to pregnant rats during the period of organogenesis caused maternal toxicity and embryo-fetal toxicities, including loss of pregnancy, at doses as low as 0.2, 0.8, and 8 times the estimated human daily dose based on body surface area. Advise pregnant patients and females of reproductive potential of the potential risk to the fetus.
Data
Animal Data
Studies in pregnant rats administered triptorelin at doses of 2, 10, and 100 mcg/kg/day (approximately equivalent to 0.2, 0.8, and 8 times the estimated human daily dose based on body surface area) during the period of organogenesis demonstrated maternal toxicity and embryo-fetal toxicities. Embryo-fetal toxicities consisted of pre-implantation loss, increased resorption, and reduced mean number of viable fetuses at the high dose. Teratogenic effects were not observed in viable fetuses in rats or mice. Doses administered to mice were 2, 20, and 200 mcg/kg/day (approximately equivalent to 0.1, 0.7, and 7 times the estimated human daily dose based on body surface area).
Lactation
The safety and efficacy of TRELSTAR have not been established in females. There are no data on the presence of triptorelin in human milk, the effects of the drug on milk production, or the effects of the drug on the breastfed child. Because of the potential for serious adverse reactions in a breastfed child from TRELSTAR, a decision should be made to either discontinue breastfeeding, or discontinue the drug taking into account the importance of the drug to the mother.
Females and Males of Reproductive Potential
Infertility
Males
Based on mechanism of action, TRELSTAR may impair fertility in males of reproductive potential [see Clinical Pharmacology (12.1 )] .
Pediatric Use
The safety and effectiveness of TRELSTAR in pediatric patients have not been established.
Geriatric Use
Prostate cancer occurs primarily in an older population. Clinical studies with TRELSTAR have been conducted primarily in patients ≥ 65 years [ see Clinical Pharmacology (12.3) and Clinical Studies (14) ].
Renal Impairment
Subjects with renal impairment had higher exposure than young healthy males [ see Clinical Pharmacology (12.3) ].
Hepatic Impairment
Subjects with hepatic impairment had higher exposure than young healthy males [ see Clinical Pharmacology (12.3) ].
4 CONTRAINDICATIONS
- Known hypersensitivity to triptorelin or any other component of the product, or other GnRH agonists or GnRH. (4 )
Hypersensitivity
TRELSTAR is contraindicated in individuals with a known hypersensitivity to triptorelin or any other component of the product, or other GnRH agonists or GnRH [ see Warnings and Precautions (5.1) ].
5 WARNINGS AND PRECAUTIONS
- Hypersensitivity: Anaphylactic shock, hypersensitivity, and angioedema have been reported. In the event of a reaction, discontinue TRELSTAR and initiate appropriate medical management. (5.1 )
- Tumor Flare: Transient increase in serum testosterone levels can occur within the first few weeks of treatment. This may worsen prostate cancer and result in spinal cord compression and urinary tract obstruction. Monitor patients at risk and manage as appropriate. (5.2 )
- Metabolic Syndrome: The use of GnRH agonists may lead to an increased risk of metabolic changes such as hyperglycemia, diabetes, hyperlipidemia, and non-alcoholic fatty liver disease. Monitor for signs and symptoms of metabolic syndrome including lipids, blood glucose level and/or HbA1c and manage according to institutional guidelines. (5.3 )
- Cardiovascular Diseases: Increased risk of myocardial infarction, sudden cardiac death and stroke has been reported in men. Monitor for cardiovascular disease and manage according toto institutional guidelines. (5.4 )
- Convulsions: Convulsions have occurred in patients treated with GnRH analogs (including TRELSTAR) with or without a history of predisposing factors. Manage patients who experience convulsions according to institutional guidelines. (5.5 )
Severe Cutaneous Adverse Reactions (SCARs): SCARs have been reported in patients receiving GnRH agonists, including triptorelin products. Interrupt TRELSTAR if signs or symptoms of SCARs develop. Permanently discontinue TRELSTAR if a SCAR is confirmed. (5.6 )
Effect on QT/QTc Interval: Androgen deprivation therapy may prolong the QT interval. Consider risks and benefits. (5.7 )
- Embryo-Fetal Toxicity: TRELSTAR may cause fetal harm. (5.10 , 8.1 )
Hypersensitivity Reactions
Anaphylactic shock, hypersensitivity, and angioedema related to TRELSTAR administration have been reported. In the event of a hypersensitivity reaction, discontinue TRELSTAR immediately and administer the appropriate supportive and symptomatic care.
Tumor Flare
Initially, triptorelin (TRELSTAR), like other GnRH agonists, causes a transient increase in serum testosterone levels [ see Clinical Pharmacology (12.2) ]. As a result, worsening signs and symptoms of prostate cancer during the first weeks of treatment have been reported with GnRH agonists. Patients may experience worsening of symptoms or onset of new symptoms, including bone pain, neuropathy, hematuria, or urethral or bladder outlet obstruction.
Closely monitor patients with metastatic vertebral lesions and/or with urinary tract obstruction during the first few weeks of therapy.
Metabolic Syndrome
The use of GnRH agonists (including TRELSTAR) may lead to metabolic changes such as hyperglycemia, diabetes mellitus, and hyperlipidemia. Non-alcoholic fatty liver disease, including cirrhosis, occurred in the post-marketing setting. Hyperglycemia may represent new-onset of diabetes mellitus or worsening of glycemic control in patients with pre-existing diabetes. Monitor for changes in serum lipids, blood glucose and/or glycosylated hemoglobin (HbA1c) periodically in patients receiving TRELSTAR and manage according to institutional guidelines.
Cardiovascular Diseases
Increased risk of developing myocardial infarction, sudden cardiac death and stroke has been reported in association with the use of GnRH agonists (including TRELSTAR) in men. The risk appears low based on the reported odds ratios and should be evaluated carefully along with cardiovascular risk factors when determining a treatment for patients with prostate cancer. Monitor patients receiving TRELSTAR for symptoms and signs suggestive of development of cardiovascular disease and manage according to current institutional guidelines.
5.5 Convulsions
Convulsions have occurred in patients treated with GnRH analog (including TRELSTAR). These events included patients with risk factors for seizures such as a history of epilepsy, intracranial tumors or co-medication with other drugs known to present a risk of seizure reactions. Convulsions have also been reported in patients in the absence of known risk factors. Manage patients receiving TRELSTAR who experience convulsion according to institutional guidelines.
Severe Cutaneous Adverse Reactions
TRELSTAR can cause severe cutaneous adverse reactions (SCARs), including Stevens-Johnson syndrome/toxic epidermal necrolysis (SJS/TEN), drug reaction with eosinophilia and systemic symptoms (DRESS), and acute generalized exanthematous pustulosis (AGEP). SCARs, including SJS/TEN, DRESS, and AGEP, occurred in patients receiving TRELSTAR or other GnRH agonists; including cases with visceral involvement and/or requiring skin grafts [see Adverse Reactions (6.2 )] .
Monitor patients for the development of SCARs.
If a SCAR is suspected, interrupt TRELSTAR until the etiology of the reaction has been determined. Consultation with a dermatologist is recommended. If a SCAR is confirmed, or for other grade 4 skin reactions, permanently discontinue TRELSTAR.
Effect on QT/QTc Interval
Androgen deprivation therapy with TRELSTAR may prolong the QT/QTc interval. Providers should consider whether the benefits of androgen deprivation therapy outweigh the potential risks in patients with congenital long QT syndrome, congestive heart failure, frequent electrolyte abnormalities, and in patients taking drugs known to prolong the QT interval. Electrolyte abnormalities should be corrected. Consider periodic monitoring of electrocardiograms and electrolytes.
Laboratory Tests
Monitor serum levels of testosterone following injection of TRELSTAR. In the majority of patients, testosterone levels increased above baseline, and then declined thereafter to castrate levels (< 50 ng/dL) within four weeks [see Clinical Studies (14 ) and Adverse Reactions (6 )] .
Laboratory Test Interactions
Chronic or continuous administration of TRELSTAR in therapeutic doses results in suppression of pituitary-gonadal axis. Diagnostic tests of the pituitary-gonadal function conducted during treatment and after cessation of therapy may therefore be misleading.
Embryo-Fetal Toxicity
Based on findings from animal studies and mechanism of action, TRELSTAR can cause fetal harm when administered to a pregnant woman [Clinical Pharmacology (12.1) ] . In animal developmental and reproductive toxicology studies, daily administration of triptorelin to pregnant rats during the period of organogenesis caused maternal toxicity and embryo-fetal toxicities, including loss of pregnancy, at doses as low as 0.2, 0.8, and 8 times the estimated human daily dose based on body surface area. Advise pregnant patients and females of reproductive potential of the potential risk to the fetus [see Use in Specific Populations (8.1) ] .
6 ADVERSE REACTIONS
The following is discussed in more detail in other sections of the labeling:
Hypersensitivity Reactions [ see Warnings and Precautions (5.1 ) ]
Tumor Flare [ see Warnings and Precautions (5.2 ) ].
Metabolic Syndrome [ see Warnings and Precautions (5.3 ) ]
Cardiovascular Diseases [ see Warnings and Precautions (5.4 ) ].
Convulsions [ see Warnings and Precautions (5.5 ) ].
Severe Cutaneous Adverse Reactions [ see Warnings and Precautions (5.6 ) ].
Effect of QT/QTc Interval [ see Warnings and Precautions (5.7 ) ].
Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared with rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The safety of the three TRELSTAR formulations was evaluated in clinical trials involving patients with advanced prostate cancer. Mean testosterone levels increased above baseline during the first week following the initial injection, declining thereafter to baseline levels or below by the end of the second week of treatment. The transient increase in testosterone levels may be associated with temporary worsening of disease signs and symptoms, including bone pain, neuropathy, hematuria, and urethral or bladder outlet obstruction. Spinal cord compression with weakness or paralysis of the lower extremities have occurred [ see Warnings and Precautions (5.2) ].
Adverse reactions reported for each of the three TRELSTAR formulations in the clinical trials, are presented in Table 2, Table 3, and Table 4. The majority of adverse reactions related to TRELSTAR are a result of its pharmacological action, i.e., the induced variation in serum testosterone levels, either an increase in testosterone at the initiation of treatment, or a decrease in testosterone once castration is achieved. Local reactions at the injection site or allergic reactions may occur.
The following adverse reactions were reported to have a possible or probable relationship to therapy as described by the treating physician in at least 1% of patients receiving TRELSTAR 3.75 mg.
| Adverse Reaction s • | TRELSTAR 3.75 mg N = 140 | |
| N | % | |
| Application Site Disorders | ||
| Injection site pain | 5 | 3.6 |
| Body as a Whole | ||
| Hot flush | 82 | 58.6 |
| Pain | 3 | 2.1 |
| Leg pain | 3 | 2.1 |
| Fatigue | 3 | 2.1 |
| Cardiovascular Disorders | ||
| Hypertension | 5 | 3.6 |
| Central and Peripheral Nervous System Disorders | ||
| Headache | 7 | 5.0 |
| Dizziness | 2 | 1.4 |
| Gastrointestinal Disorders | ||
| Diarrhea | 2 | 1.4 |
| Vomiting | 3 | 2.1 |
| Musculoskeletal System Disorders | ||
| Skeletal pain | 17 | 12.1 |
| Psychiatric Disorders | ||
| Insomnia | 3 | 2.1 |
| Impotence | 10 | 7.1 |
| Emotional lability | 2 | 1.4 |
| Red Blood Cell Disorders | ||
| Anemia | 2 | 1.4 |
| Skin and Appendages Disorders | ||
| Pruritus | 2 | 1.4 |
| Urinary System Disorders | ||
| Urinary tract infection | 2 | 1.4 |
| Urinary retention | 2 | 1.4 |
• Adverse reactions for TRELSTAR 3.75 mg are coded using the WHO Adverse Reactions Terminology (WHOART)
The following adverse reactions were reported to have a possible or probable relationship to therapy as described by the treating physician in at least 1% of patients receiving TRELSTAR 11.25 mg.
| Adverse Reactions • | TRELSTAR 11.25 mg N = 174 | |
| N | % | |
| Application Site | ||
| Injection site pain | 7 | 4.0 |
| Body as a Whole | ||
| Hot flush | 127 | 73.0 |
| Leg pain | 9 | 5.2 |
| Pain | 6 | 3.4 |
| Back pain | 5 | 2.9 |
| Fatigue | 4 | 2.3 |
| Chest pain | 3 | 1.7 |
| Asthenia | 2 | 1.1 |
| Peripheral edema | 2 | 1.1 |
| Cardiovascular Disorders | ||
| Hypertension | 7 | 4.0 |
| Dependent edema | 4 | 2.3 |
| Central and Peripheral Nervous System Disorders | ||
| Headache | 12 | 6.9 |
| Dizziness | 5 | 2.9 |
| Leg cramps | 3 | 1.7 |
| Endocrine | ||
| Breast pain | 4 | 2.3 |
| Gynecomastia | 3 | 1.7 |
| Gastrointestinal Disorders | ||
| Nausea | 5 | 2.9 |
| Constipation | 3 | 1.7 |
| Dyspepsia | 3 | 1.7 |
| Diarrhea | 2 | 1.1 |
| Abdominal pain | 2 | 1.1 |
| Liver and Biliary System | ||
| Abnormal hepatic function | 2 | 1.1 |
| Metabolic and Nutritional Disorders | ||
| Edema in legs | 11 | 6.3 |
| Increased alkaline phosphatase | 3 | 1.7 |
| Musculoskeletal System Disorders | ||
| Skeletal pain | 23 | 13.2 |
| Arthralgia | 4 | 2.3 |
| Myalgia | 2 | 1.1 |
| Psychiatric Disorders | ||
| Decreased libido | 4 | 2.3 |
| Impotence | 4 | 2.3 |
| Insomnia | 3 | 1.7 |
| Anorexia | 3 | 1.7 |
| Respiratory System Disorders | ||
| Coughing | 3 | 1.7 |
| Dyspnea | 2 | 1.1 |
| Pharyngitis | 2 | 1.1 |
| Skin and Appendages | ||
| Rash | 3 | 1.7 |
| Urinary System Disorders | ||
| Dysuria | 8 | 4.6 |
| Urinary retention | 2 | 1.1 |
| Vision Disorders | ||
| Eye pain | 2 | 1.1 |
| Conjunctivitis | 2 | 1.1 |
• Adverse reactions for TRELSTAR 11.25 mg are coded using the WHO Adverse Reactions Terminology (WHOART)
The following adverse reactions occurred in at least 5% of patients receiving TRELSTAR 22.5 mg. The table includes all reactions whether or not they were ascribed to TRELSTAR by the treating physician. The table also includes the incidence of these adverse reactions that were considered by the treating physician to have a reasonable causal relationship or for which the relationship could not be assessed.
| Adverse Reactions • | TRELSTAR 22.5 mg N = 120 | |||
| Treatment-Emergent | Treatment-Related | |||
| N | % | N | % | |
| General Disorders and Administration Site Conditions | ||||
| Edema peripheral | 6 | 5.0 | 0 | 0 |
| Infections and Infestations | ||||
| Influenza | 19 | 15.8 | 0 | 0 |
| Bronchitis | 6 | 5.0 | 0 | 0 |
| Endocrine | ||||
| Diabetes Mellitus/Hyperglycemia | 6 | 5.0 | 0 | 0 |
| Musculoskeletal and Connective Tissue Disorders | ||||
| Back pain | 13 | 10.8 | 1 | 0.8 |
| Arthralgia | 9 | 7.5 | 1 | 0.8 |
| Pain in extremity | 9 | 7.5 | 1 | 0.8 |
| Nervous System Disorders | ||||
| Headache | 9 | 7.5 | 2 | 1.7 |
| Psychiatric Disorders | ||||
| Insomnia | 6 | 5.0 | 1 | 0.8 |
| Renal and Urinary Disorders | ||||
| Urinary tract infection | 14 | 11.6 | 0 | 0 |
| Urinary retention | 6 | 5.0 | 0 | 0 |
| Reproductive System and Breast Disorders | ||||
| Erectile dysfunction | 12 | 10.0 | 12 | 10.0 |
| Testicular atrophy | 9 | 7.5 | 9 | 7.5 |
| Vascular Disorders | ||||
| Hot flush | 87 | 72.5 | 86 | 71.7 |
| Hypertension | 17 | 14.2 | 1 | 0.8 |
• Adverse reactions for TRELSTAR 22.5 mg are coded using the Medical Dictionary for Regulatory Activities (MedDRA)
Changes in Laboratory Values During Treatment
The following abnormalities in laboratory values not present at baseline were observed in 10% or more of patients:
TRELSTAR 3.75 mg : There were no clinically meaningful changes in laboratory values detected during therapy.
TRELSTAR 11.25 mg : Decreased hemoglobin and RBC count and increased glucose, BUN, SGOT, SGPT, and alkaline phosphatase at the Day 253 visit.
TRELSTAR 22.5 mg : Decreased hemoglobin and increased glucose and hepatic transaminases were detected during the study. The majority of the changes were mild to moderate.
Post-marketing Experience
The following adverse reactions have been identified during post approval use of gonadotropin releasing hormone agonists. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Pituitary Apoplexy – During post-marketing surveillance, rare cases of pituitary apoplexy (a clinical syndrome secondary to infarction of the pituitary gland) have been reported after the administration of gonadotropin-releasing hormone agonists. In majority of these cases, a pituitary adenoma was diagnosed with a majority of pituitary apoplexy cases occurring within 2 weeks of the first dose, and some within the first hour. In these cases, pituitary apoplexy has presented as sudden headache, vomiting, visual changes, ophthalmoplegia, altered mental status, and sometimes cardiovascular collapse. Immediate medical attention has been required.
Cardiovascular System – cerebrovascular accident, myocardial infarction, pulmonary emboli, thromboembolic events (including deep venous thrombosis, transient ischemic attack, and thrombophlebitis)
Central/Peripheral Nervous System – convulsions
Hepatobiliary Disorder – non-alcoholic fatty liver disease
Respiratory, Thoracic, and Mediastinal Disorder – interstitial lung disease
Skin and Subcutaneous Tissue Disorders – SJS/TEN, DRESS, AGEP, dermatitis exfoliative, bullous dermatitis, and erythema multiforme.
7 DRUG INTERACTIONS
No drug-drug interaction studies involving TRELSTAR have been conducted.
Human pharmacokinetic data with triptorelin suggest that C-terminal fragments produced by tissue degradation are either degraded completely within tissues, are rapidly degraded further in plasma, or cleared by the kidneys. Therefore, hepatic microsomal enzymes are unlikely to be involved in triptorelin metabolism. However, in the absence of relevant data and as a precaution, hyperprolactinemic drugs should not be used concomitantly with TRELSTAR since hyperprolactinemia reduces the number of pituitary GnRH receptors.
11 DESCRIPTION
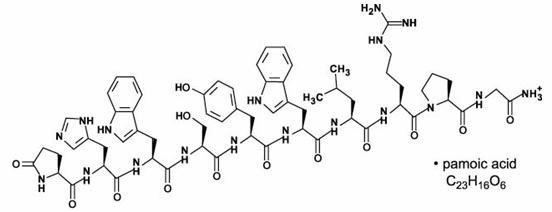
TRELSTAR is a white to slightly yellow lyophilized cake. When reconstituted, TRELSTAR has a milky appearance. It contains a pamoate salt of triptorelin, a synthetic decapeptide agonist analog of gonadotropin releasing hormone (GnRH). The chemical name of triptorelin pamoate is 5-oxo-L-prolyl-L-histidyl-L-tryptophyl-L-seryl-L-tyrosyl-D-tryptophyl-L-leucyl-L-arginyl-L-prolylglycine amide (pamoate salt). The empirical formula is C 64 H 82 N 18 O 13 · C 23 H 16 O 6 and the molecular weight is 1699.9. The structural formula is:
The TRELSTAR products are sterile, lyophilized biodegradable microgranule formulations supplied as single dose vials. Refer to Table 5 for the composition of each TRELSTAR product.
| Ingredients | TRELSTAR 3.75 mg | TRELSTAR 11.25 mg | TRELSTAR 22.5 mg |
| triptorelin pamoate (base units) | 3.75 mg | 11.25 mg | 22.5 mg |
| poly- d,l -lactide-co-glycolide | 138 mg | 120 mg | 183 mg |
| mannitol, USP | 71 mg | 74 mg | 74 mg |
| carboxymethylcellulose sodium, USP | 25 mg | 26 mg | 26 mg |
| polysorbate 80, NF | 1.7 mg | 1.7 mg | 1.7 mg |
When 2 mL sterile water is added to the vial containing TRELSTAR and mixed, a suspension is formed which is intended as an intramuscular injection. TRELSTAR is available in a vial plus a vial adapter, and a separate pre-filled syringe that contains sterile water for injection, USP, 2 mL.
12 CLINICAL PHARMACOLOGY
Mechanism of Action
Triptorelin is a synthetic decapeptide agonist analog of gonadotropin releasing hormone (GnRH). Comparative in vitro studies showed that triptorelin was 100-fold more active than native GnRH in stimulating luteinizing hormone release from monolayers of dispersed rat pituitary cells in culture and 20-fold more active than native GnRH in displacing 125 I-GnRH from pituitary receptor sites. In animal studies, triptorelin pamoate was found to have 13‑fold higher luteinizing hormone-releasing activity and 21-fold higher follicle-stimulating hormone-releasing activity compared to the native GnRH.
Pharmacodynamics
Following the first administration, there is a transient surge in circulating levels of luteinizing hormone (LH), follicle-stimulating hormone (FSH), testosterone, and estradiol [ see Adverse Reactions (6) ]. After chronic and continuous administration, usually 2 to 4 weeks after initiation of therapy, a sustained decrease in LH and FSH secretion and marked reduction of testicular steroidogenesis are observed. A reduction of serum testosterone concentration to a level typically seen in surgically castrated men is obtained. Consequently, the result is that tissues and functions that depend on these hormones for maintenance become quiescent. These effects are usually reversible after cessation of therapy.
Following a single intramuscular injection of TRELSTAR:
TRELSTAR 3.75 mg : serum testosterone levels first increased, peaking on Day 4, and declined thereafter to low levels by Week 4 in healthy male volunteers.
TRELSTAR 11.25 mg : serum testosterone levels first increased, peaking on Days 2 – 3, and declined thereafter to low levels by Weeks 3 – 4 in men with advanced prostate cancer.
TRELSTAR 22.5 mg : serum testosterone levels first increased, peaking on Day 3, and declined thereafter to low levels by Weeks 3 – 4 in men with advanced prostate cancer.
Pharmacokinetics
Results of pharmacokinetic investigations conducted in healthy men indicate that after intravenous bolus administration, triptorelin is distributed and eliminated according to a 3-compartment model and corresponding half-lives are approximately 6 minutes, 45 minutes, and 3 hours.
Absorption
Following a single intramuscular injection of TRELSTAR to patients with prostate cancer, mean peak serum concentrations of 28.4 ng/mL, 38.5 ng/mL, and 44.1 ng/mL occurred in 1 to 3 hours after the 3.75 mg, 11.25 mg, and 22.5 mg formulations, respectively.
Triptorelin did not accumulate over 9 months (3.75 mg and 11.25 mg) or 12 months (22.5 mg) of treatment.
Distribution
The volume of distribution following a single intravenous bolus dose of 0.5 mg of triptorelin peptide was 30 – 33 L in healthy male volunteers. There is no evidence that triptorelin, at clinically relevant concentrations, binds to plasma proteins.
Elimination
Metabolism
The metabolism of triptorelin in humans is unknown but is unlikely to involve hepatic microsomal enzymes (cytochrome P-450). The effect of triptorelin on the activity of other drug metabolizing enzymes is also unknown. Thus far, no metabolites of triptorelin have been identified. Pharmacokinetic data suggest that C-terminal fragments produced by tissue degradation are either completely degraded in the tissues, or rapidly degraded in plasma, or cleared by the kidneys.
Excretion
Triptorelin is eliminated by both the liver and the kidneys. Following intravenous administration of 0.5 mg triptorelin peptide to six healthy male volunteers with a creatinine clearance of 149.9 mL/min, 41.7% of the dose was excreted in urine as intact peptide with a total triptorelin clearance of 211.9 mL/min. This percentage increased to 62.3% in patients with liver disease who have a lower creatinine clearance (89.9 mL/min). It has also been observed that the nonrenal clearance of triptorelin (patient anuric, CI creat = 0) was 76.2 mL/min, thus indicating that the nonrenal elimination of triptorelin is mainly dependent on the liver.
Specific Populations
Age and Race
The effects of age and race on triptorelin pharmacokinetics have not been systematically studied. However, pharmacokinetic data obtained in young healthy male volunteers aged 20 to 22 years with an elevated creatinine clearance (approximately 150 mL/min) indicate that triptorelin was eliminated twice as fast in this young population as compared with patients with moderate renal insufficiency. This is related to the fact that triptorelin clearance is partly correlated to total creatinine clearance, which is well known to decrease with age [ see Use in Specific Populations (8.6 ) and (8.7 ) ].
Pediatric
TRELSTAR has not been evaluated in patients less than 18 years of age [ see Use in Specific Populations (8.4) ].
Hepatic and Renal Impairment
After an intravenous bolus injection of 0.5 mg triptorelin, the two distribution half-lives were unaffected by renal and hepatic impairment. However, renal insufficiency led to a decrease in total triptorelin clearance proportional to the decrease in creatinine clearance as well as increases in volume of distribution and consequently, an increase in elimination half-life (see Table 6). In subjects with hepatic insufficiency, a decrease in triptorelin clearance was more pronounced than that observed with renal insufficiency. Due to minimal increases in the volume of distribution, the elimination half-life in subjects with hepatic insufficiency was similar to subjects with renal insufficiency. Subjects with renal or hepatic impairment had 2‑ to 4-fold higher exposure (AUC values) than young healthy males [ see Use in Specific Populations (8.6 ) and (8.7 ) ].
| Group | C max (ng/mL) | AUC inf (h·ng/mL) | Cl p (mL/min) | Cl renal (mL/min) | t 1/2 (h) | Cl creat (mL/min) |
| 6 healthy male volunteers | 48.2 ±11.8 | 36.1 ±5.8 | 211.9 ±31.6 | 90.6 ±35.3 | 2.81 ±1.21 | 149.9 ±7.3 |
| 6 males with moderate renal impairment | 45.6 ±20.5 | 69.9 ±24.6 | 120.0 ±45.0 | 23.3 ±17.6 | 6.56 ±1.25 | 39.7 ±22.5 |
| 6 males with severe renal impairment | 46.5 ±14.0 | 88.0 ±18.4 | 88.6 ±19.7 | 4.3 ±2.9 | 7.65 ±1.25 | 8.9 ±6.0 |
| 6 males with liver disease | 54.1 ±5.3 | 131.9 ±18.1 | 57.8 ±8.0 | 35.9 ±5.0 | 7.58 ±1.17 | 89.9 ±15.1 |
13 NONCLINICAL TOXICOLOGY
Carcinogenesis, Mutagenesis, Impairment of Fertility
In rats, triptorelin doses of 120, 600, and 3000 mcg/kg given every 28 days (approximately 0.3, 2, and 8 times the human monthly dose based on body surface area) resulted in increased mortality with a drug treatment period of 13 – 19 months. The incidences of benign and malignant pituitary tumors and histiosarcomas were increased in a dose-related manner. No oncogenic effect was observed in mice administered triptorelin for 18 months at doses up to 6000 mcg/kg every 28 days (approximately 8 times the human monthly dose based on body surface area).
Mutagenicity studies performed with triptorelin using bacterial and mammalian systems ( in vitro Ames test and chromosomal aberration test in CHO cells and an in vivo mouse micronucleus test) provided no evidence of mutagenic potential.
After 60 days of subcutaneous treatment followed by a minimum of four estrus cycles prior to mating, triptorelin, at doses of 2, 20, and 200 mcg/kg/day in saline (approximately 0.2, 2, and 16 times the estimated human daily dose based on body surface area) or 2 monthly injections as slow release microspheres (~20 mcg/kg/day), had no effect on the fertility or general reproductive function of female rats.
No studies were conducted to assess the effect of triptorelin on male fertility.
14 CLINICAL STUDIES
TRELSTAR 3.75 mg
TRELSTAR 3.75 mg was studied in a randomized, active control trial of 277 men with advanced prostate cancer. The clinical trial population consisted of 59.9% Caucasian, 39.3% Black, and 0.8% Other. There was no difference observed with triptorelin response between racial groups. Men were between 47 and 89 years of age (mean = 71 years). Patients received either TRELSTAR 3.75 mg (N = 140) or an approved GnRH agonist monthly for 9 months. The primary efficacy endpoints were both achievement of castration by Day 29 and maintenance of castration from Day 57 through Day 253.
Castration levels of serum testosterone (≤ 1.735 nmol/L; equivalent to 50 ng/dL) in patients treated with TRELSTAR 3.75 mg were achieved at Day 29 in 125 of 137 (91.2%) patients and at Day 57 in 97.7% of patients. Maintenance of castration levels of serum testosterone from Day 57 through Day 253 was found in 96.2% of patients treated with TRELSTAR 3.75 mg.
The presence of an acute-on-chronic flare phenomenon was also studied as a secondary efficacy endpoint. Serum LH levels were measured at 2 hours after repeat TRELSTAR 3.75 mg administration on Days 85 and 169. One hundred twenty-four of the 126 evaluable patients (98.4%) on Day 85 had a serum LH level of ≤ 1.0 IU/L at 2 hours after dosing, indicating desensitization of the pituitary gonadotroph receptors.
TRELSTAR 11.25 mg
TRELSTAR 11.25 mg was studied in a randomized, active control trial of 346 men with advanced prostate cancer. The clinical trial population consisted of 48% Caucasian, 38% Black, and 15% Other. There was no difference observed with triptorelin response between racial groups. Men were between 45 and 96 years of age (mean = 71 years). Patients received either TRELSTAR 11.25 mg (N = 174) every 12 weeks for a total of up to 3 doses (maximum treatment period of 253 days) or TRELSTAR 3.75 mg (N = 172) every 28 days for a total of up to 9 doses. The primary efficacy endpoints were both achievement of castration by Day 29 and maintenance of castration from Day 57 through Day 253.
Castration levels of serum testosterone (≤ 1.735 nmol/L; equivalent to 50 ng/dL) were achieved at Day 29 in 167 of 171 (97.7%) patients treated with TRELSTAR 11.25 mg, and maintenance of castration levels of serum testosterone from Day 57 through Day 253 was found in 94.4% of patients treated with TRELSTAR 11.25 mg.
TRELSTAR 22.5 mg
TRELSTAR 22.5 mg was studied in a non-comparative trial of 120 men with advanced prostate cancer. The clinical trial population consisted of 64% Caucasian, 23% Black, and 13% Other, with a mean age of 71.1 years (range 51-93). Patients received TRELSTAR 22.5 mg (N = 120) every 24 weeks for a total of 2 doses (maximum treatment period of 337 days). The primary efficacy endpoints included achievement of castration by Day 29 and maintenance of castration from Day 57 through Day 337.
Castration levels of serum testosterone (≤ 1.735 nmol/L; equivalent to 50 ng/dL) were achieved at Day 29 in 97.5% (117 of 120) of patients treated with TRELSTAR 22.5 mg. Castration was maintained in 93.3% of patients in the period from Day 57 to Day 337.
A summary of the clinical studies for TRELSTAR is provided in Table 7.
| Product Strength | 3.75 mg | 11.25 mg | 22.5 mg |
| Number of Patients | 137 | 171 | 120 |
| Treatment Schedule | every 4 weeks | every 12 weeks | every 24 weeks |
| Duration of Study | 253 days | 253 days | 337 days |
| Castration Rate • on Day 29, % (n/N) | 91.2% (125/137) | 97.7% (167/171) | 97.5% (117/120) |
| Rate of Castration Maintenance † from Days 57 – 253, % | 96.2% | 94.4% | not applicable |
| Rate of Castration Maintenance from Days 57 – 337, % (n/N) | not applicable | not applicable | 93.3% (112/120) ‡ |
• Maintenance of castration was calculated using a frequency distribution. † Cumulative maintenance of castration was calculated using a survival analysis (Kaplan-Meier) technique. ‡ Calculation includes 5 patients who discontinued the study but who had castrate levels of testosterone prior to discontinuation.
16 HOW SUPPLIED/STORAGE AND HANDLING
TRELSTAR (triptorelin pamoate for injectable suspension) is supplied as a single dose vial with a Flip-Off cap containing sterile lyophilized triptorelin pamoate microgranules incorporated in a biodegradable copolymer of lactic and glycolic acids, with injection kit consisting of a vial adapter, a 21 gauge 1 ½” injection needle, and a pre-filled syringe containing sterile water for injection, USP, 2 mL.
TRELSTAR 3.75 mg – NDC 74676-5902-1: 3.75 mg of slightly yellow microgranules provided in a vial with a violet flip-off cap with injection kit.
TRELSTAR 11.25 mg – NDC 74676-5904-1: 11.25 mg of slightly yellow microgranules provided in a vial with a yellow green flip-off cap with injection kit.
TRELSTAR 22.5 mg – NDC 74676-5906-1: 22.5 mg of slightly yellow microgranules provided in a vial with a dark green flip-off cap with injection kit.
Storage
Store at 20-25°C (68-77°F). [See USP Controlled Room Temperature.] Do not freeze TRELSTAR.
Mechanism of Action
Triptorelin is a synthetic decapeptide agonist analog of gonadotropin releasing hormone (GnRH). Comparative in vitro studies showed that triptorelin was 100-fold more active than native GnRH in stimulating luteinizing hormone release from monolayers of dispersed rat pituitary cells in culture and 20-fold more active than native GnRH in displacing 125 I-GnRH from pituitary receptor sites. In animal studies, triptorelin pamoate was found to have 13‑fold higher luteinizing hormone-releasing activity and 21-fold higher follicle-stimulating hormone-releasing activity compared to the native GnRH.