Xanax prior authorization resources
Most recent state uniform prior authorization forms
Xanax patient education
Patient toolkit
Dosage & administration
DOSAGE AND ADMINISTRATION
- Generalized Anxiety Disorder : (2.1 )
- Recommended starting oral dosage is 0.25 mg to 0.5 mg three times daily.
- Dosage may be increased, at intervals of every 3 to 4 days, to a maximum recommended daily dose of 4 mg, given in divided doses.
- Use the lowest possible effective dose and frequently assess the need for continued treatment.
- Panic Disorder : Recommended starting oral dosage is 0.5 mg three times daily. The dosage may be increased at intervals of every 3 to 4 days in increments of no more than 1 mg per day. (2.2 )
- When tapering, decrease dosage by no more than 0.5 mg every 3 days. Some patients may require an even slower dosage reduction. (2.3 , 5.2 )
- See the Full Prescribing Information for the recommended dosage in geriatric patients, patients with hepatic impairment, and with use with ritonavir. (2.4 , 2.5 , 2.6 )
Dosage in Generalized Anxiety Disorder
The recommended starting oral dosage of XANAX for the acute treatment of patients with GAD is 0.25 mg to 0.5 mg administered three times daily. Depending upon the response, the dosage may be adjusted at intervals of every 3 to 4 days. The maximum recommended dosage is 4 mg daily (in divided doses).
Use the lowest possible effective dose and frequently assess the need for continued treatment [see Warnings and Precautions (5.2) ] .
Dosage in Panic Disorder
The recommended starting oral dosage of XANAX for the treatment of PD is 0.5 mg three times daily. Depending on the response, the dosage may be increased at intervals of every 3 to 4 days in increments of no more than 1 mg per day.
Controlled trials of XANAX in the treatment of panic disorder included dosages in the range of 1 mg to 10 mg daily. The mean dosage was approximately 5 mg to 6 mg daily. Occasional patients required as much as 10 mg per day.
For patients receiving doses greater than 4 mg per day, periodic reassessment and consideration of dosage reduction is advised. In a controlled postmarketing dose-response study, patients treated with doses of XANAX greater than 4 mg per day for 3 months were able to taper to 50% of their total maintenance dose without apparent loss of clinical benefit.
The necessary duration of treatment for PD in patients responding to XANAX is unknown. After a period of extended freedom from panic attacks, a carefully supervised tapered discontinuation may be attempted, but there is evidence that this may often be difficult to accomplish without recurrence of symptoms and/or the manifestation of withdrawal phenomena [see Dosage and Administration (2.3) ] .
Discontinuation or Dosage Reduction of XANAX
To reduce the risk of withdrawal reactions, use a gradual taper to discontinue XANAX or reduce the dosage. If a patient develops withdrawal reactions, consider pausing the taper or increasing the dosage to the previous tapered dosage level. Subsequently decrease the dosage more slowly [see Warnings and Precautions (5.3) , Drug Abuse and Dependence (9.3) ] .
Reduced the dosage by no more than 0.5 mg every 3 days. Some patients may benefit from an even more gradual discontinuation. Some patients may prove resistant to all discontinuation regimens.
In a controlled postmarketing discontinuation study of panic disorder patients which compared the recommended taper schedule with a slower taper schedule, no difference was observed between the groups in the proportion of patients who tapered to zero dose; however, the slower schedule was associated with a reduction in symptoms associated with a withdrawal syndrome.
Dosage Recommendations in Geriatric Patients
In geriatric patients, the recommended starting oral dosage of XANAX is 0.25 mg, given 2 or 3 times daily. This may be gradually increased if needed and tolerated. Geriatric patients may be especially sensitive to the effects of benzodiazepines. If adverse reactions occur at the recommended starting dosage, the dosage may be reduced [see Use in Specific Populations (8.5) , Clinical Pharmacology (12.3) ] .
Dosage Recommendations in Patients with Hepatic Impairment
In patients with hepatic impairment, the recommended starting oral dosage of XANAX is 0.25 mg, given 2 or 3 times daily. This may be gradually increased if needed and tolerated. If adverse reactions occur at the recommended starting dose, the dosage may be reduced [see Use in Specific Populations (8.6) , Clinical Pharmacology (12.3) ] .
Dosage Modifications for Drug Interactions
XANAX should be reduced to half of the recommended dosage when a patient is started on ritonavir and XANAX together, or when ritonavir administered to a patient treated with XANAX. Increase the XANAX dosage to the target dose after 10 to 14 days of dosing ritonavir and XANAX together. It is not necessary to reduce XANAX dose in patients who have been taking ritonavir for more than 10 to 14 days.
XANAX is contraindicated with concomitant use of all strong CYP3A inhibitors, except ritonavir [see Contraindications (4) , Warnings and Precautions (5.5) ] .

By using PrescriberAI, you agree to the AI Terms of Use.
Xanax prescribing information
WARNING: RISKS FROM CONCOMITANT USE WITH OPIOIDS; ABUSE, MISUSE, AND ADDICTION; and DEPENDENCE AND WITHDRAWAL REACTIONS
- Concomitant use of benzodiazepines and opioids may result in profound sedation, respiratory depression, coma, and death. Reserve concomitant prescribing of these drugs for patients for whom alternative treatment options are inadequate. Limit dosages and durations to the minimum required. Follow patients for signs and symptoms of respiratory depression and sedation [see Warnings and Precautions (5.1) , Drug Interactions (7.1) ] .
- The use of benzodiazepines, including XANAX, exposes users to risks of abuse, misuse, and addiction, which can lead to overdose or death. Abuse and misuse of benzodiazepines commonly involve concomitant use of other medications, alcohol, and/or illicit substances, which is associated with an increased frequency of serious adverse outcomes. Before prescribing XANAX and throughout treatment, assess each patient’s risk for abuse, misuse, and addiction [see Warnings and Precautions (5.2) ] .
- The continued use of benzodiazepines, including XANAX, may lead to clinically significant physical dependence. The risks of dependence and withdrawal increase with longer treatment duration and higher daily dose. Abrupt discontinuation or rapid dosage reduction of XANAX after continued use may precipitate acute withdrawal reactions, which can be life-threatening. To reduce the risk of withdrawal reactions, use a gradual taper to discontinue XANAX or reduce the dosage [see Dosage and Administration (2.2) , Warnings and Precautions (5.3) ] .
Warnings and Precautions (5.8 ) 1/2023
INDICATIONS AND USAGE
XANAX is indicated for the:
- acute treatment of generalized anxiety disorder (GAD) in adults.
- treatment of panic disorder (PD), with or without agoraphobia in adults.
DOSAGE AND ADMINISTRATION
- Generalized Anxiety Disorder : (2.1 )
- Recommended starting oral dosage is 0.25 mg to 0.5 mg three times daily.
- Dosage may be increased, at intervals of every 3 to 4 days, to a maximum recommended daily dose of 4 mg, given in divided doses.
- Use the lowest possible effective dose and frequently assess the need for continued treatment.
- Panic Disorder : Recommended starting oral dosage is 0.5 mg three times daily. The dosage may be increased at intervals of every 3 to 4 days in increments of no more than 1 mg per day. (2.2 )
- When tapering, decrease dosage by no more than 0.5 mg every 3 days. Some patients may require an even slower dosage reduction. (2.3 , 5.2 )
- See the Full Prescribing Information for the recommended dosage in geriatric patients, patients with hepatic impairment, and with use with ritonavir. (2.4 , 2.5 , 2.6 )
Dosage in Generalized Anxiety Disorder
The recommended starting oral dosage of XANAX for the acute treatment of patients with GAD is 0.25 mg to 0.5 mg administered three times daily. Depending upon the response, the dosage may be adjusted at intervals of every 3 to 4 days. The maximum recommended dosage is 4 mg daily (in divided doses).
Use the lowest possible effective dose and frequently assess the need for continued treatment [see Warnings and Precautions (5.2) ] .
Dosage in Panic Disorder
The recommended starting oral dosage of XANAX for the treatment of PD is 0.5 mg three times daily. Depending on the response, the dosage may be increased at intervals of every 3 to 4 days in increments of no more than 1 mg per day.
Controlled trials of XANAX in the treatment of panic disorder included dosages in the range of 1 mg to 10 mg daily. The mean dosage was approximately 5 mg to 6 mg daily. Occasional patients required as much as 10 mg per day.
For patients receiving doses greater than 4 mg per day, periodic reassessment and consideration of dosage reduction is advised. In a controlled postmarketing dose-response study, patients treated with doses of XANAX greater than 4 mg per day for 3 months were able to taper to 50% of their total maintenance dose without apparent loss of clinical benefit.
The necessary duration of treatment for PD in patients responding to XANAX is unknown. After a period of extended freedom from panic attacks, a carefully supervised tapered discontinuation may be attempted, but there is evidence that this may often be difficult to accomplish without recurrence of symptoms and/or the manifestation of withdrawal phenomena [see Dosage and Administration (2.3) ] .
Discontinuation or Dosage Reduction of XANAX
To reduce the risk of withdrawal reactions, use a gradual taper to discontinue XANAX or reduce the dosage. If a patient develops withdrawal reactions, consider pausing the taper or increasing the dosage to the previous tapered dosage level. Subsequently decrease the dosage more slowly [see Warnings and Precautions (5.3) , Drug Abuse and Dependence (9.3) ] .
Reduced the dosage by no more than 0.5 mg every 3 days. Some patients may benefit from an even more gradual discontinuation. Some patients may prove resistant to all discontinuation regimens.
In a controlled postmarketing discontinuation study of panic disorder patients which compared the recommended taper schedule with a slower taper schedule, no difference was observed between the groups in the proportion of patients who tapered to zero dose; however, the slower schedule was associated with a reduction in symptoms associated with a withdrawal syndrome.
Dosage Recommendations in Geriatric Patients
In geriatric patients, the recommended starting oral dosage of XANAX is 0.25 mg, given 2 or 3 times daily. This may be gradually increased if needed and tolerated. Geriatric patients may be especially sensitive to the effects of benzodiazepines. If adverse reactions occur at the recommended starting dosage, the dosage may be reduced [see Use in Specific Populations (8.5) , Clinical Pharmacology (12.3) ] .
Dosage Recommendations in Patients with Hepatic Impairment
In patients with hepatic impairment, the recommended starting oral dosage of XANAX is 0.25 mg, given 2 or 3 times daily. This may be gradually increased if needed and tolerated. If adverse reactions occur at the recommended starting dose, the dosage may be reduced [see Use in Specific Populations (8.6) , Clinical Pharmacology (12.3) ] .
Dosage Modifications for Drug Interactions
XANAX should be reduced to half of the recommended dosage when a patient is started on ritonavir and XANAX together, or when ritonavir administered to a patient treated with XANAX. Increase the XANAX dosage to the target dose after 10 to 14 days of dosing ritonavir and XANAX together. It is not necessary to reduce XANAX dose in patients who have been taking ritonavir for more than 10 to 14 days.
XANAX is contraindicated with concomitant use of all strong CYP3A inhibitors, except ritonavir [see Contraindications (4) , Warnings and Precautions (5.5) ] .
DOSAGE FORMS AND STRENGTHS
XANAX tablets are available as:
- 0.25 mg: white, oval, scored, imprinted “XANAX 0.25”
- 0.5 mg: peach, oval, scored, imprinted “XANAX 0.5”
- 1 mg: blue, oval, scored, imprinted “XANAX 1.0”
- 2 mg: white, oblong, multi-scored, imprinted “XANAX ” on one side and “2” on the reverse side
USE IN SPECIFIC POPULATIONS
Lactation: Breastfeeding not recommended. (8.2 )
Pregnancy
Pregnancy Exposure Registry
There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to psychiatric medications, including XANAX, during pregnancy. Healthcare providers are encouraged to register patients by calling the National Pregnancy Registry for Psychiatric Medications at 1-866-961-2388 or visiting online at https://womensmentalhealth.org/research/pregnancyregistry/.
Risk Summary
Neonates born to mothers using benzodiazepines late in pregnancy have been reported to experience symptoms of sedation and/or neonatal withdrawal [see Warnings and Precautions (5.8) and Clinical Considerations) ] . Available data from published observational studies of pregnant women exposed to benzodiazepines do not report a clear association with benzodiazepines and major birth defects ( see Data ).
The background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated risk of major birth defects and of miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Clinical Considerations
Fetal/Neonatal adverse reactions
Benzodiazepines cross the placenta and may produce respiratory depression, hypotonia, and sedation in neonates. Monitor neonates exposed to XANAX during pregnancy or labor for signs of sedation, respiratory depression, hypotonia, and feeding problems. Monitor neonates exposed to XANAX during pregnancy for signs of withdrawal. Manage these neonates accordingly [see Warnings and Precautions (5.8) ] .
Data
Human Data
Published data from observational studies on the use of benzodiazepines during pregnancy do not report a clear association with benzodiazepines and major birth defects. Although early studies reported an increased risk of congenital malformations with diazepam and chlordiazepoxide, there was no consistent pattern noted. In addition, the majority of recent case-control and cohort studies of benzodiazepine use during pregnancy, which were adjusted for confounding exposures to alcohol, tobacco, and other medications, have not confirmed these findings.
Lactation
Risk Summary
Limited data from published literature reports the presence of alprazolam in human breast milk. There are reports of sedation, poor feeding and poor weight gain in infants exposed to benzodiazepines through breast milk. The effects of alprazolam on lactation are unknown.
Because of the potential for serious adverse reactions, including sedation and withdrawal symptoms in breastfed infants, advise patients that breastfeeding is not recommended during treatment with XANAX.
Pediatric Use
Safety and effectiveness of XANAX have not been established in pediatric patients.
Geriatric Use
XANAX-treated geriatric patients had higher plasma concentrations of alprazolam (due to reduced clearance) compared to younger adult patients receiving the same doses. Therefore, dosage reduction of XANAX is recommended in geriatric patients [see Dosage and Administration (2.4) and Clinical Pharmacology (12.3) ] .
Hepatic Impairment
Patients with alcoholic liver disease exhibit a longer elimination half-life (19.7 hours), compared to healthy subjects (11.4 hours). This may be caused by decreased clearance of alprazolam in patients with alcoholic liver disease. Dosage reduction of XANAX is recommended in patients with hepatic impairment [see Dosage and Administration (2.4) , Clinical Pharmacology (12.3) ] .
CONTRAINDICATIONS
XANAX is contraindicated in patients:
- with known hypersensitivity to alprazolam or other benzodiazepines. Angioedema has been reported [see Adverse Reactions (6.2) ] .
- taking strong cytochrome P450 3A (CYP3A) inhibitors (e.g., ketoconazole, itraconazole), except ritonavir [see Dosage and Administration (2.6) , Warnings and Precautions (5.5) , Drug Interactions (7.1) ]
WARNINGS AND PRECAUTIONS
- Effects on Driving and Operating Machinery: Patients receiving XANAX should be cautioned against operating machinery or driving a motor vehicle, as well as avoiding concomitant use of alcohol and other central nervous system (CNS) depressant drugs. (5.4 )
- Patients with Depression: Exercise caution in patients with signs or symptoms of depression. Prescribe the least number of tablets feasible to avoid intentional overdosage. (5.6 )
- Neonatal Sedation and Withdrawal Syndrome: XANAX use during pregnancy can result in neonatal sedation and/or neonatal withdrawal. (5.8 , 8.1 )
Risks from Concomitant Use with Opioids
Concomitant use of benzodiazepines, including XANAX, and opioids may result in profound sedation, respiratory depression, coma, and death. Because of these risks, reserve concomitant prescribing of these drugs in patients for whom alternative treatment options are inadequate.
Observational studies have demonstrated that concomitant use of opioid analgesics and benzodiazepines increases the risk of drug-related mortality compared to use of opioids alone. If a decision is made to prescribe XANAX concomitantly with opioids, prescribe the lowest effective dosages and minimum durations of concomitant use, and follow patients closely for signs and symptoms of respiratory depression and sedation. In patients already receiving an opioid analgesic, prescribe a lower initial dose of XANAX than indicated in the absence of an opioid and titrate based on clinical response. If an opioid is initiated in a patient already taking XANAX, prescribe a lower initial dose of the opioid and titrate based upon clinical response.
Advise both patients and caregivers about the risks of respiratory depression and sedation when XANAX is used with opioids. Advise patients not to drive or operate heavy machinery until the effects of concomitant use with the opioid have been determined [see Drug Interactions (7.1) ] .
Abuse, Misuse, and Addiction
The use of benzodiazepines, including XANAX, exposes users to the risks of abuse, misuse, and addiction, which can lead to overdose or death. Abuse and misuse of benzodiazepines often (but not always) involve the use of doses greater than the maximum recommended dosage and commonly involve concomitant use of other medications, alcohol, and/or illicit substances, which is associated with an increased frequency of serious adverse outcomes, including respiratory depression, overdose, or death [see Drug Abuse and Dependence (9.2) ] .
Before prescribing XANAX and throughout treatment, assess each patient’s risk for abuse, misuse, and addiction (e.g., using a standardized screening tool). Use of XANAX, particularly in patients at elevated risk, necessitates counseling about the risks and proper use of XANAX along with monitoring for signs and symptoms of abuse, misuse, and addiction. Prescribe the lowest effective dosage; avoid or minimize concomitant use of CNS depressants and other substances associated with abuse, misuse, and addiction (e.g., opioid analgesics, stimulants); and advise patients on the proper disposal of unused drug. If a substance use disorder is suspected, evaluate the patient and institute (or refer them for) early treatment, as appropriate.
Dependence and Withdrawal Reactions
To reduce the risk of withdrawal reactions, use a gradual taper to discontinue XANAX or reduce the dosage (a patient-specific plan should be used to taper the dose) [see Dosage and Administration (2.3) ] .
Patients at an increased risk of withdrawal adverse reactions after benzodiazepine discontinuation or rapid dosage reduction include those who take higher dosages, and those who have had longer durations of use.
Acute Withdrawal Reactions
The continued use of benzodiazepines, including XANAX, may lead to clinically significant physical dependence. Abrupt discontinuation or rapid dosage reduction of XANAX after continued use, or administration of flumazenil (a benzodiazepine antagonist) may precipitate acute withdrawal reactions, which can be life-threatening (e.g., seizures) [see Drug Abuse and Dependence (9.3) ] .
Protracted Withdrawal Syndrome
In some cases, benzodiazepine users have developed a protracted withdrawal syndrome with withdrawal symptoms lasting weeks to more than 12 months [see Drug Abuse and Dependence (9.3) ] .
Certain adverse clinical events, some life-threatening, are a direct consequence of physical dependence to XANAX. These include a spectrum of withdrawal symptoms; the most important is seizure [see Drug Abuse and Dependence (9.3)] . Even after relatively short-term use at doses of ≤4 mg/day, there is some risk of dependence. Spontaneous reporting system data suggest that the risk of dependence and its severity appear to be greater in patients treated with doses greater than 4 mg/day and for long periods (more than 12 weeks). However, in a controlled postmarketing discontinuation study of panic disorder patients who received XANAX, the duration of treatment (3 months compared to 6 months) had no effect on the ability of patients to taper to zero dose. In contrast, patients treated with doses of XANAX greater than 4 mg/day had more difficulty tapering to zero dose than those treated with less than 4 mg/day.
In a controlled clinical trial in which 63 patients were randomized to XANAX and where withdrawal symptoms were specifically sought, the following were identified as symptoms of withdrawal: heightened sensory perception, impaired concentration, dysosmia, clouded sensorium, paresthesias, muscle cramps, muscle twitch, diarrhea, blurred vision, appetite decrease, and weight loss. Other symptoms, such as anxiety and insomnia, were frequently seen during discontinuation, but it could not be determined if they were due to return of illness, rebound, or withdrawal.
Interdose Symptoms
Early morning anxiety and emergence of anxiety symptoms between doses of XANAX have been reported in patients with panic disorder taking prescribed maintenance doses. These symptoms may reflect the development of tolerance or a time interval between doses which is longer than the duration of clinical action of the administered dose. In either case, it is presumed that the prescribed dose is not sufficient to maintain plasma levels above those needed to prevent relapse, rebound, or withdrawal symptoms over the entire course of the interdosing interval.
Effects on Driving and Operating Machinery
Because of its CNS depressant effects, patients receiving XANAX should be cautioned against engaging in hazardous occupations or activities requiring complete mental alertness such as operating machinery or driving a motor vehicle. For the same reason, patients should be cautioned about the concomitant use of alcohol and other CNS depressant drugs during treatment with XANAX [see Drug Interactions (7.1) ] .
Interaction with Drugs that Inhibit Metabolism via Cytochrome P450 3A
The initial step in alprazolam metabolism is hydroxylation catalyzed by cytochrome P450 3A (CYP3A). Drugs that inhibit this metabolic pathway may have a profound effect on the clearance of alprazolam.
Strong CYP3A Inhibitors
XANAX is contraindicated in patients receiving strong inhibitors of CYP3A (such as azole antifungal agents), except ritonavir [see Contraindications (4) ] . Ketoconazole and itraconazole have been shown in vivo to increase plasma alprazolam concentrations 3.98 fold and 2.70 fold, respectively.
Dosage adjustment is necessary when XANAX and ritonavir are initiated concomitantly or when ritonavir is added to a stable dosage of XANAX [see Dosage and Administration (2.6) , Drug Interactions (7.1) ] .
Drugs demonstrated to be CYP3A inhibitors on the basis of clinical studies involving alprazolam: nefazodone, fluvoxamine, and cimetidine [see Drug Interaction (7.1) , Clinical Pharmacology (12.3) ] . Use caution and consider dose reduction of XANAX, as appropriate, during co-administration with these drugs.
Patients with Depression
Benzodiazepines may worsen depression. Panic disorder has been associated with primary and secondary major depressive disorders and increased reports of suicide among untreated patients. Consequently, appropriate precautions (e.g., limiting the total prescription size and increased monitoring for suicidal ideation) should be considered in patients with depression.
Mania
Episodes of hypomania and mania have been reported in association with the use of XANAX in patients with depression [see Adverse Reactions (6.2) ] .
Neonatal Sedation and Withdrawal Syndrome
Use of XANAX late in pregnancy can result in sedation (respiratory depression, lethargy, hypotonia) and/or withdrawal symptoms (hyperreflexia, irritability, restlessness, tremors, inconsolable crying, and feeding difficulties) in the neonate [see Use in Specific Populations (8.1) ] . Monitor neonates exposed to XANAX during pregnancy or labor for signs of sedation and monitor neonates exposed to XANAX during pregnancy for signs of withdrawal; manage these neonates accordingly.
Risk in Patients with Impaired Respiratory Function
There have been reports of death in patients with severe pulmonary disease shortly after the initiation of treatment with XANAX. Closely monitor patients with impaired respiratory function. If signs and symptoms of respiratory depression, hypoventilation, or apnea occur, discontinue XANAX.
ADVERSE REACTIONS
The following clinically significant adverse reactions are described elsewhere in the labeling:
- Risks from Concomitant Use with Opioids [see Warnings and Precautions (5.1) ]
- Abuse, Misuse, and Addiction [see Warnings and Precautions (5.2) ]
- Dependence and Withdrawal Reactions [see Warnings and Precautions (5.3) ]
- Effects on Driving and Operating Machinery [see Warnings and Precautions (5.4) ]
- Patients with Depression [see Warnings and Precautions (5.6) ]
- Neonatal Sedation and Withdrawal Syndrome [see Warnings and Precautions (5.8) ]
- Risks in Patients with Impaired Respiratory Function [see Warnings and Precautions (5.9) ]
Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The data in the two tables below are estimates of adverse reaction incidence among adult patients who participated in:
- 4-week placebo-controlled clinical studies with XANAX dosages up to 4 mg per day for the acute treatment of generalized anxiety disorder (Table 1)
- Short-term (up to 10 weeks) placebo-controlled clinical studies with XANAX dosages up to 10 mg per day for panic disorder, with or without agoraphobia (Table 2).
XANAX n=565 | Placebo n=505 | |
Nervous system disorders | ||
Drowsiness | 41% | 22% |
Light-headedness | 21% | 19% |
Dizziness | 2% | 1% |
Akathisia | 2% | 1% |
Gastrointestinal disorders | ||
Dry mouth | 15% | 13% |
Increased salivation | 4% | 2% |
Cardiovascular disorders | ||
Hypotension | 5% | 2% |
Skin and subcutaneous tissue disorders | ||
Dermatitis/allergy | 4% | 3% |
In addition to the adverse reactions (i.e., greater than 1%) enumerated in the table above for patients with generalized anxiety disorder, the following adverse reactions have been reported in association with the use of benzodiazepines: dystonia, irritability, concentration difficulties, anorexia, transient amnesia or memory impairment, loss of coordination, fatigue, seizures, sedation, slurred speech, jaundice, musculoskeletal weakness, pruritus, diplopia, dysarthria, changes in libido, menstrual irregularities, incontinence and urinary retention.
| XANAX n=1388 | Placebo n=1231 | |
|---|---|---|
Drowsiness Fatigue and Tiredness Impaired Coordination Irritability Memory Impairment Cognitive Disorder Decreased Libido Dysarthria Confusional state | 77% 49% 40% 33% 33% 29% 14% 23% 10% | 43% 42% 18% 30% 22% 21% 8% 6% 8% |
Increased libido | 8% | 4% |
Change in libido (not specified) | 7% | 6% |
Disinhibition | 3% | 2% |
Talkativeness | 2% | 1% |
Derealization | 2% | 1% |
Gastrointestinal disorders | ||
Constipation | 26% | 15% |
Increased salivation | 6% | 4% |
Skin and subcutaneous tissue disorders | ||
Rash | 11% | 8% |
Other | ||
Increased appetite | 33% | 23% |
Decreased appetite | 28% | 24% |
Weight gain | 27% | 18% |
Weight loss | 23% | 17% |
Micturition difficulties | 12% | 9% |
Menstrual disorders | 11% | 9% |
Sexual dysfunction | 7% | 4% |
Incontinence | 2% | 1% |
In addition to the reactions (i.e., greater than 1%) enumerated in the table above for patients with panic disorder, the following adverse reactions have been reported in association with the use of XANAX: seizures, hallucinations, depersonalization, taste alterations, diplopia, elevated bilirubin, elevated hepatic enzymes, and jaundice.
Adverse Reactions Reported as Reasons for Discontinuation in Treatment of Panic Disorder in Placebo-Controlled Trials
In a larger database comprised of both controlled and uncontrolled studies in which 641 patients received XANAX, discontinuation-emergent symptoms which occurred at a rate of over 5% in patients treated with XANAX and at a greater rate than the placebo-treated group are shown in Table 3.
| n=number of patients. | |
XANAX-treated Patients n=641 | |
Nervous system disorders | |
Insomnia | 29.5% |
Light-headedness | 19.3% |
Abnormal involuntary movement | 17.3% |
Headache | 17.0% |
Muscular twitching | 6.9% |
Impaired coordination | 6.6% |
Muscle tone disorders | 5.9% |
Weakness | 5.8% |
Psychiatric disorders | |
Anxiety | 19.2% |
Fatigue and Tiredness | 18.4% |
Irritability | 10.5% |
Cognitive disorder | 10.3% |
Memory impairment | 5.5% |
Depression | 5.1% |
Confusional state | 5.0% |
Gastrointestinal disorders | |
Nausea/Vomiting | 16.5% |
Diarrhea | 13.6% |
Decreased salivation | 10.6% |
Metabolism and nutrition disorders | |
Weight loss | 13.3% |
Decreased appetite | 12.8% |
Dermatological disorders | |
Sweating | 14.4% |
Cardiovascular disorders | |
Tachycardia | 12.2% |
Special Senses | |
Blurred vision | 10.0% |
There have also been reports of withdrawal seizures upon rapid decrease or abrupt discontinuation of XANAX [see Warning and Precautions (5.2) and Drug Abuse and Dependence (9.3) ] .
Paradoxical reactions such as stimulation, increased muscle spasticity, sleep disturbances, hallucinations, and other adverse behavioral effects such as agitation, rage, irritability, and aggressive or hostile behavior have been reported rarely. In many of the spontaneous case reports of adverse behavioral effects, patients were receiving other CNS drugs concomitantly and/or were described as having underlying psychiatric conditions. Should any of the above events occur, alprazolam should be discontinued. Isolated published reports involving small numbers of patients have suggested that patients who have borderline personality disorder, a prior history of violent or aggressive behavior, or alcohol or substance abuse may be at risk for such events. Instances of irritability, hostility, and intrusive thoughts have been reported during discontinuation of alprazolam in patients with posttraumatic stress disorder.
Postmarketing Experience
The following adverse reactions have been identified during postapproval use of XANAX. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Endocrine disorders: Hyperprolactinemia
General disorders and administration site conditions: Edema peripheral
Hepatobiliary disorders: Hepatitis, hepatic failure
Investigations: Liver enzyme elevations
Psychiatric disorders: Hypomania, mania
Reproductive system and breast disorders: Gynecomastia, galactorrhea
Skin and subcutaneous tissue disorders: Photosensitivity reaction, angioedema, Stevens-Johnson syndrome
DRUG INTERACTIONS
- Use with Opioids: Increase the risk of respiratory depression. (7.1 )
- Use with Other CNS Depressants: Produces additive CNS depressant effects. (7.1 )
- Use with Digoxin: Increase the risk of digoxin toxicity. (7.1 )
- Use with CYP3A Inhibitors (except ritonavir): Increase the risk of adverse reactions of alprazolam. (4 , 5.5 , 7.1 )
- Use with CYP3A Inducers: Increase the risk of reduced efficacy of alprazolam. (7.1 )
Drugs Having Clinically Important Interactions with XANAX
Table 4 includes clinically significant drug interactions with XANAX [see Clinical Pharmacology (12.3) ] .
Opioids | |
Clinical implication | The concomitant use of benzodiazepines and opioids increases the risk of respiratory depression because of actions at different receptor sites in the CNS that control respiration. Benzodiazepines interact at gamma-aminobutyric acid (GABA A ) sites and opioids interact primarily at mu receptors. When benzodiazepines and opioids are combined, the potential for benzodiazepines to significantly worsen opioid‑related respiratory depression exists. |
Prevention or management | Limit dosage and duration of concomitant use of XANAX and opioids, and monitor patients closely for respiratory depression and sedation [see Warnings and Precautions (5.1) ] . |
Examples | Morphine, buprenorphine, hydromorphone, oxymorphone, oxycodone, fentanyl, methadone, alfentanil, butorphanol, codeine, dihydrocodeine, meperidine, pentazocine, remifentanil, sufentanil, tapentadol, tramadol. |
CNS Depressants | |
Clinical implication | The benzodiazepines, including alprazolam, produce additive CNS depressant effects when coadministered with other CNS depressants. |
Prevention or management | Limit dosage and duration of XANAX during concomitant use with CNS depressants [see Warnings and Precautions (5.3) ] . |
Examples | Psychotropic medications, anticonvulsants, antihistaminics, ethanol, and other drugs which themselves produce CNS depression. |
Strong Inhibitors of CYP3A (except ritonavir) | |
Clinical implication | Concomitant use of XANAX with strong CYP3A inhibitors has a profound effect on the clearance of alprazolam, resulting in increased concentrations of alprazolam and increased risk of adverse reactions [see Clinical Pharmacology (12.3) ]. |
Prevention or management | Concomitant use of XANAX with a strong CYP3A4 inhibitor (except ritonavir) is contraindicated [see Contraindications (4) , Warnings and Precautions (5.5) ]. |
Examples | Ketoconazole, itraconazole, clarithromycin |
Moderate or Weak Inhibitors of CYP3A | |
Clinical implication | Concomitant use of XANAX with CYP3A inhibitors may increase the concentrations of XANAX, resulting in increased risk of adverse reactions of alprazolam [see Clinical Pharmacology (12.3) ]. |
Prevention or management | Avoid use and consider appropriate dose reduction when XANAX is coadministered with a moderate or weak CYP3A inhibitor [see Warnings and Precautions (5.5) ]. |
Examples | Nefazodone, fluvoxamine, cimetidine, erythromycin |
CYP3A Inducers | |
Clinical implication | Concomitant use of CYP3A inducers can increase alprazolam metabolism and therefore can decease plasma levels of alprazolam [see Clinical Pharmacology (12.3) ] . |
Prevention or management | Caution is recommended during coadministration with XANAX. |
Examples | Carbamazepine, phenytoin |
Ritonavir | |
Clinical implication | Interactions involving ritonavir and alprazolam are complex and time dependent. Short term administration of ritonavir increased alprazolam exposure due to CYP3A4 inhibition. Following long term treatment of ritonavir (>10 to 14 days), CYP3A4 induction offsets this inhibition. Alprazolam exposure was not meaningfully affected in the presence of ritonavir. |
Prevention or management | Reduce XANAX dosage when ritonavir and XANAX are initiated concomitantly, or when ritonavir is added to a regimen where XANAX is stabilized. Increase XANAX dosage to the target dosage after 10 to 14 days of dosing ritonavir and XANAX concomitantly. No dosage adjustment of XANAX is necessary in patients receiving ritonavir for more than 10 to14 days [see Dosage and Administration (2.6) ] . Concomitant use of XANAX with a strong CYP3A inhibitor, except ritonavir, is contraindicated [see Contraindications (4) , Warnings and Precautions (5.5) ]. |
Digoxin | |
Clinical implication | Increased digoxin concentrations have been reported when alprazolam was given, especially in geriatric patients (>65 years of age). |
Prevention or management | In patients on digoxin therapy, measure serum digoxin concentrations before initiating XANAX. Continue monitoring digoxin serum concentration and toxicity frequently . Reduce the digoxin dose if necessary. |
Drug/Laboratory Test Interactions
Although interactions between benzodiazepines and commonly employed clinical laboratory tests have occasionally been reported, there is no consistent pattern for a specific drug or specific test.
DESCRIPTION
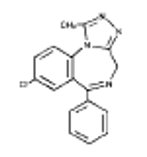
XANAX contains alprazolam which is a triazolo analog of the 1,4 benzodiazepine class of central nervous system-active compounds.
The chemical name of alprazolam is 8-Chloro-1-methyl-6-phenyl-4H-s-triazolo [4,3-α] [1,4] benzodiazepine.
The structural formula is:
Alprazolam is a white crystalline powder, which is soluble in methanol or ethanol but which has no appreciable solubility in water at physiological pH.
Each XANAX tablet, for oral administration, contains 0.25 mg, 0.5 mg, 1 mg, or 2 mg of alprazolam.
Inactive ingredients: cellulose, corn starch, docusate sodium, lactose, magnesium stearate, silicon dioxide and sodium benzoate. In addition, the 0.5 mg tablet contains FD&C Yellow No. 6 and the 1 mg tablet contains FD&C Blue No. 2.
CLINICAL PHARMACOLOGY
Mechanism of Action
Alprazolam is a 1,4 benzodiazepine. Alprazolam exerts its effect for the acute treatment of generalized anxiety disorder and panic disorder through binding to the benzodiazepine site of gamma‑aminobutyric acid-A (GABA A ) receptors in the brain and enhances GABA-mediated synaptic inhibition.
Pharmacokinetics
Plasma levels of alprazolam increase proportionally to the dose over the range of 0.5 to 3.0 mg.
Absorption
Following oral administration, peak plasma concentration of alprazolam (C max ) occurs in 1 to 2 hours post dose.
Distribution
Alprazolam is 80% bound to human serum protein, and albumin accounts for the majority of the binding.
Elimination
The mean plasma elimination half-life (T 1/2 ) of alprazolam is approximately 11.2 hours (range: 6.3 to 26.9 hours) in healthy adults.
Metabolism
Alprazolam is extensively metabolized in humans, primarily by cytochrome P450 3A4 (CYP3A4), to 2 major active metabolites in the plasma: 4-hydroxyalprazolam and α-hydroxyalprazolam. The plasma circulation levels of the two active metabolites are less than 4% of the parent. The reported relative potencies in benzodiazepine receptor binding experiments and in animal models of induced seizure inhibition are 0.20 and 0.66, respectively, for 4-hydroxyalprazolam and α-hydroxyalprazolam. The low concentrations and low potencies of 4-hydroxyalprazolam and α-hydroxyalprazolam indicate that they unlikely contribute much to the effects of alprazolam. A benzophenone derived from alprazolam is also found in humans. Their half-lives appear to be similar to that of alprazolam.
Excretion
Alprazolam and its metabolites are excreted primarily in the urine.
Specific Populations
Geriatric Patients
The mean T 1/2 of alprazolam was 16.3 hours (range: 9.0 to 26.9 hours) in healthy elderly subjects compared to 11.0 hours (range: 6.3 to -15.8 hours, n=16) in healthy younger adult subjects.
Obese Patients
The mean T 1/2 of alprazolam was 21.8 hours (range: 9.9 to 40.4 hours) in a group of obese subjects.
Patients with Hepatic Impairment
The mean T 1/2 of alprazolam was 19.7 hours (range: 5.8 to 65.3 hours) in patients with alcoholic liver disease.
Racial or Ethnic Groups
Maximal concentrations and T 1/2 of alprazolam are approximately 15% and 25% higher in Asians compared to Caucasians.
Smoking
Alprazolam concentrations may be reduced by up to 50% in smokers compared to non-smokers.
Drug Interaction Studies
In Vivo Studies
Most of the interactions that have been documented with alprazolam are with drugs that modulate CYP3A4 activity.
Compounds that are inhibitors or inducers of CYP3A would be expected to increase or decrease plasma alprazolam concentrations, respectively. Drug products that have been studied in vivo, along with their effect on increasing alprazolam AUC, are as follows: ketoconazole, 3.98 fold; itraconazole, 2.66 fold; nefazodone, 1.98 fold; fluvoxamine, 1.96 fold; and erythromycin, 1.61 fold [see Contraindications (4) , Warnings and Precautions (5.5) , Drug Interactions (7.2) ] . Other studied drugs include:
Cimetidine: Coadministration of cimetidine increased the maximum plasma concentration of alprazolam by 82%, decreased clearance by 42%, and increased T 1/2 by 16%.
Fluoxetine: Coadministration of fluoxetine with alprazolam increased the maximum plasma concentration of alprazolam by 46%, decreased clearance by 21%, increased T 1/2 by 17%, and decreased measured psychomotor performance.
Oral Contraceptives: Coadministration of oral contraceptives increased the maximum plasma concentration of alprazolam by 18%, decreased clearance by 22%, and increased T 1/2 by 29%.
Carbamazepine: The oral clearance of alprazolam (given in a 0.8 mg single dose) was increased from 0.90±0.21 mL/min/kg to 2.13±0.54 mL/min/kg and the elimination T 1/2 was shortened (from 17.1±4.9 to 7.7±1.7 hour) following administration of 300 mg per day carbamazepine for 10 days [see Drug Interactions (7.2) ] . However, the carbamazepine dose used in this study was fairly low compared to the recommended doses (1000-1200 mg per day); the effect at usual carbamazepine doses is unknown.
Ritonavir: Interactions involving HIV protease inhibitors (e.g., ritonavir) and alprazolam are complex and time dependent. Short-term low doses of ritonavir (4 doses of 200 mg) increased mean AUC of alprazolam by about 2.5-fold, and did not significantly affect C max of alprazolam. The elimination T 1/2 was prolonged (30 hours versus 13 hours). However, upon extended exposure to ritonavir (500 mg, twice daily for 10 days), CYP3A induction offset this inhibition. Alprazolam AUC and C max was reduced by 12% and 16%, respectively, in the presence of ritonavir. The elimination T 1/2 of alprazolam was not significantly changed [see Warnings and Precautions (5.5) ] .
Sertraline: A single dose of alprazolam 1 mg and steady state dose of sertraline (50 mg to 150 mg per day) did not reveal any clinically significant changes in the pharmacokinetics of alprazolam.
Imipramine and Desipramine: The steady state plasma concentrations of imipramine and desipramine have been reported to be increased an average of 31% and 20%, respectively, by the concomitant administration of XANAX in doses up to 4 mg per day.
Warfarin: Alprazolam did not affect the prothrombin or plasma warfarin levels in male volunteers administered sodium warfarin orally.
In Vitro Studies
Data from in vitro studies of alprazolam suggest a possible drug interaction of alprazolam with paroxetine. The ability of alprazolam to induce human hepatic enzyme systems has not yet been determined.
NONCLINICAL TOXICOLOGY
Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
No evidence of carcinogenic potential was observed in rats or mice administered alprazolam for 2 years at doses up to 30 and 10 mg/kg day respectively. These doses are 29 times and 4.8 times the maximum recommended human dose of 10 mg/day based on mg/m 2 body surface area, respectively.
Mutagenesis
Alprazolam was negative in the in vitro Ames bacterial reverse mutation assay and DNA Damage/Alkaline Elution Assay and in vivo rat micronucleus genetic toxicology assays.
Impairment of Fertility
Alprazolam produced no impairment of fertility in rats at doses up to 5 mg/kg per day, which is approximately 5 times the maximum recommended human dose of 10 mg per day based on mg/m 2 body surface area.
Animal Toxicology and/or Pharmacology
When rats were treated with alprazolam at oral doses of 3 mg, 10 mg, and 30 mg/kg day (3 to 29 times the maximum recommended human dose based on mg/m 2 body surface area) for 2 years, a tendency for a dose related increase in the number of cataracts was observed in females and a tendency for a dose related increase in corneal vascularization was observed in males. These lesions did not appear until after 11 months of treatment.
CLINICAL STUDIES
Generalized Anxiety Disorder
XANAX was compared to placebo in double-blind clinical studies (doses up to 4 mg per day) in patients with a diagnosis of anxiety or anxiety with associated depressive symptomatology. XANAX was significantly better than placebo at each of the evaluation periods of these 4-week studies as judged by the following psychometric instruments: Physician’s Global Impressions, Hamilton Anxiety Rating Scale, Target Symptoms, Patient’s Global Impressions, and Self-Rating Symptom Scale.
Panic Disorder
The effectiveness of XANAX in the treatment of panic disorder was studied in 3 short-term, placebo-controlled studies (up to 10 weeks) in patients with diagnoses closely corresponding to DSM-III-R criteria for panic disorder.
The average dose of XANAX was 5 mg to 6 mg per day in 2 of the studies, and the doses of XANAX were fixed at 2 mg and 6 mg per day in the third study. In all 3 studies, XANAX was superior to placebo on a variable defined as “the number of patients with zero panic attacks” (range, 37% to 83% met this criterion), as well as on a global improvement score. In 2 of the 3 studies, XANAX was superior to placebo on a variable defined as “change from baseline on the number of panic attacks per week” (range, 3.3 to 5.2), and also on a phobia rating scale. A subgroup of patients who improved on XANAX during short-term treatment in 1 of these trials was continued on an open basis up to 8 months, without apparent loss of benefit.
HOW SUPPLIED/STORAGE AND HANDLING
XANAX is supplied in the following strengths and package configurations:
Package Configuration | Tablet Strength (mg) | NDC | |
Bottles of 100 Reverse Numbered Unit dose (100) Bottles of 500 Bottles of 1000 | 0.25 mg | NDC 0009-0029-01 NDC 0009-0029-46 NDC 0009-0029-02 NDC 0009-0029-14 | white, oval, scored, imprinted “XANAX 0.25” |
Bottles of 100 Reverse Numbered Unit dose (100) Bottles of 500 Bottles of 1000 | 0.5 mg | NDC 0009-0055-01 NDC 0009-0055-46 NDC 0009-0055-03 NDC 0009-0055-15 | peach, oval, scored, imprinted “XANAX 0.5” |
Bottles of 100 Bottles of 500 Bottles of 1000 | 1 mg | NDC 0009-0090-01 NDC 0009-0090-04 NDC 0009-0090-13 | blue, oval, scored, imprinted “XANAX 1.0” |
Bottles of 100 Bottles of 500 | 2 mg | NDC 0009-0094-01 NDC 0009-0094-03 | white, oblong, multi-scored, imprinted “XANAX” on one side and “2” on the reverse side |
Store at controlled room temperature 20° to 25°C (68° to 77°F) [see USP Controlled Room Temperature].
Mechanism of Action
Alprazolam is a 1,4 benzodiazepine. Alprazolam exerts its effect for the acute treatment of generalized anxiety disorder and panic disorder through binding to the benzodiazepine site of gamma‑aminobutyric acid-A (GABA A ) receptors in the brain and enhances GABA-mediated synaptic inhibition.